Consumer-based mobile meditation applications may help women self-manage stress and other mental health symptoms, especially during the coronavirus disease (COVID-19) pandemic.
Abstract
OBJECTIVE:
To assess the effect of a consumer-based mobile meditation application (app) on wellness in outpatient obstetric and gynecology patients during the coronavirus disease 2019 (COVID-19) pandemic.
METHODS:
We conducted a randomized controlled trial at a university outpatient clinic of obstetric and gynecology patients during the COVID-19 pandemic. Women were randomly assigned to the intervention group, who was prescribed a mobile meditation app for 30 days, or the control group, which received standard care. The primary outcome was self-reported perceived stress. Secondary outcomes included self-reported depression, anxiety, sleep disturbance, and satisfaction with the meditation app. A sample size of 80 participants (40 per group) was calculated to achieve 84% power to detect a 3-point difference in the primary outcome.
RESULTS:
From April to May 2020, 101 women were randomized in the study—50 in the meditation app group and 51 in the control group. Analysis was by intention-to-treat. Most characteristics were similar between groups. Perceived stress was significantly less in the intervention group at days 14 and 30 (mean difference 4.27, 95% CI 1.30–7.24, P=.005, d=0.69 and mean difference 4.28, 95% CI 1.68–6.88, P=.002, d=0.69, respectively). Self-reported depression and anxiety were significantly less in the intervention group at days 14 and 30 (depression: P=.002 and P=.04; anxiety: P=.01, and P=.04, respectively). Sleep disturbance was significantly less in the intervention group at days 14 and 30 (P=.001 and P=.02, respectively). More than 80% of those in the intervention group reported high satisfaction with the meditation app, and 93% reported that mindfulness meditation improved their stress.
CONCLUSION:
Outpatient obstetric and gynecology patients who used the prescribed consumer-based mobile meditation app during the COVID-19 pandemic had significant reductions in perceived stress, depression, anxiety, and sleep disturbance compared with standard care.
CLINICAL TRIAL REGISTRATION:
ClinicalTrials.gov, NCT04329533.
The coronavirus disease 2019 (COVID-19) pandemic has led to health care system changes that affect obstetric and gynecology patients. This includes, but is not limited to, visitor restrictions, modifications to outpatient visits (ie, telemedicine), extended visit intervals, cancelled visits, and suspension of educational programs and group prenatal care. Experiencing a global pandemic as a pregnant patient is a unique life event that can increase stress, anxiety, and depression.1 For surgical patients, a joint statement was released on March 16, 2020, stating elective procedures should be postponed to divert health care attention and resources for this public health crisis.2 Physicians were confronted with finding new strategies to guide women through the burden of increased demands at home in addition to personal health care changes. For example, physicians could recommend more self-care (eg, home blood pressure monitoring), virtual and online support resources through public health and mental health agencies, and encourage software applications (apps) that may help self-manage stress and anxiety.1,3
Mindfulness is defined as the mental state of focusing one's awareness on the present moment without judgement.4 The effects of mindfulness meditation have been studied in pregnancy, postpartum, infertility, chronic and postoperative pelvic pain, and cancer patients with positive effects on well-being, although data are limited.5–11 Of late, mobile apps have become a popular platform to deliver mindfulness meditation. The objective of this randomized controlled trial was to assess the effect of a consumer-based mobile meditation app on perceived stress in outpatient obstetric and gynecology patients during the COVID-19 pandemic.
METHODS
We conducted a randomized controlled trial in Phoenix, Arizona, from April 14, 2020, to May 28, 2020. The Institutional Review Board at the University of Arizona College of Medicine Phoenix approved the study protocol. The trial was registered with ClinicalTrials.gov (registration number NCT04329533) and was conducted in accordance with the protocol. Included in the study were English-speaking women aged 18 years and older who were established patients of our clinic. Eligibility criteria for the obstetric patients was a confirmed pregnancy between 14 and 34 weeks of gestation; for the gynecology patients, it was a surgical procedure that was delayed or cancelled due to the COVID-19 pandemic. Women with the inability to regularly access a smart device or who already used the meditation app Calm were not eligible to participate in the study. After patients were identified, they were invited to participate in the study by telephone call from study personnel (R.B.S), and all participants provided electronic informed consent.
After completing the electronic informed consent, participants completed a baseline (day 0) survey including three validated questionnaires on perceived stress, depression, anxiety, and sleep disturbance. After baseline assessments, participants were randomized to either the intervention group, who were prescribed the mindfulness meditation app Calm for 30 days, or the control group, who received standard care. The University of Arizona College of Medicine research staff produced the computer-generated simple randomization scheme. Randomization allocation ratio was one-to-one. A password-protected randomization database, Research Electronic Data Capture (REDCap), was used for randomization allocation as well as data collection and management. The password-protected database, Qualtrics, was used for participant questionnaires.
Patients in the intervention group were provided information on how to download and use the mobile app Calm. Verbal and written encouragement was given to use the mobile app 70 minutes per week, preferably 10 minutes per day, for a total of 30 days. Patients could use any of the components of the mobile app they chose (eg, mindfulness meditation, sleep stories, nature sounds). Participants were encouraged to use the “daily Calm,” a 10-minute guided meditation unique to each day; however, this was not required. Participants in the control group continued with their standard obstetric or gynecology care for 30 days. At the conclusion of the study period, the control group received access to the mobile app Calm for 30 days.
At three specified study time periods (days 0, 14, and 30), patients completed self-reported psychological assessments. The primary study outcome was perceived stress difference between groups over the 30-day study period and was measured using Cohen's 10-item Perceived Stress Scale.12 The Perceived Stress Scale score ranges from 0 to 40 (0–13=low stress, 14–26=moderate stress, 27–40=high stress). Secondary study outcomes included the perceived stress difference mid-study (day 14) and other self-reported psychological measures of depression, anxiety, and sleep disturbance, which were measured using Zigmond's 14-item Hospital Anxiety and Depression Scale13 and the 8-item PROMIS (Patient-Reported Outcomes Measurement Information System) Sleep Disturbance Short Form.14 The Hospital Anxiety and Depression score ranges from 0 to 21 individually for anxiety and depression (0–7=normal, 8–10=borderline abnormal, 11–21=abnormal). The PROMIS Sleep Disturbance Short Form score ranges from 29 to 77 (less than 55=none to slight, 55–59.9=mild, 60–69.9=moderate, 70 and over=severe). Electronic reminders were generated for patients who did not complete the day 14 and 30 assessments, followed by reminder phone calls for the day 30 assessments.
For participants in the intervention group, satisfaction with the meditation app was assessed by questionnaire at the end of the 30-day study period. A 5-point Likert scale was used to evaluate overall satisfaction and ease of use with the app. The effect the app had on participants’ stress and sleep were assessed with a 4-point Likert scale, and perception of positive change to their mental health, physical health, stress, anxiety, and sleep were assessed with binary questions (yes or no). Frequency of app use was self-reported on the final questionnaire. All patients were assessed on their perceptions of the COVID-19 pandemic before and after the study, including personal risk of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19; ability to prevent infection; level of worry for personal, family member, and community infection; and the effect COVID-19 has had on their stress, mental health, and physical health. Electronic medical records were reviewed for demographic data, baseline characteristics, pregnancy course for the obstetric patients, and preoperative course for the gynecology patients.
We powered the study to detect a clinically significant mean difference of 3 points in the perceived stress score. The power calculation used the normal approximation method assuming a pooled standard deviation of 0.5 and the test statistic used was the two-sided Fisher's exact test with an a priori significance level of 0.05. A sample size of 80 participants (40 per group) was calculated to achieve 84% power. To allow for a 20% attrition rate, we planned to enroll 100 participants. Categorical variables were examined using the Chi squared test and two-sided Fisher's exact test. The Student's t test was used to determine differences in continuous variables. Secondary analyses compared differences by group and by time interactions using repeated analysis of variance tests. A significance level of 0.05 was used for all tests. Effect sizes were quantified using Cohen's d with values greater than 0.50 suggesting moderate effect and values 0.21 to 0.50 suggesting modest effect. Intention-to-treat and per protocol analyses were both performed; however, intention-to-treat is reported. Data were summarized using SAS 9.4. Results were reported following the CONSORT (Consolidated Standards of Reporting Trials) statement.15
RESULTS
From April 14, 2020, to May 28, 2020, we screened 263 women for inclusion in the study (132 pregnant patients, 131 gynecology patients with delayed or cancelled surgeries). A total of 101 patients were consented for participation and randomized, 50 in the meditation app group and 51 in the control group (Fig. 1). Eleven women discontinued participation after the baseline psychological assessments for unknown reasons, seven in the intervention group and four in the control group; baseline responses were used as their day 30 responses. One participant did not complete the baseline perceived stress assessment; day 14 responses were used as day 0. Thirty-one women did not complete the mid-study (day 14) assessments, 19 in the intervention group and 12 in the control group.
Fig. 1. CONSORT (Consolidated Standards of Reporting Trials) flowchart of patient recruitment and participation.
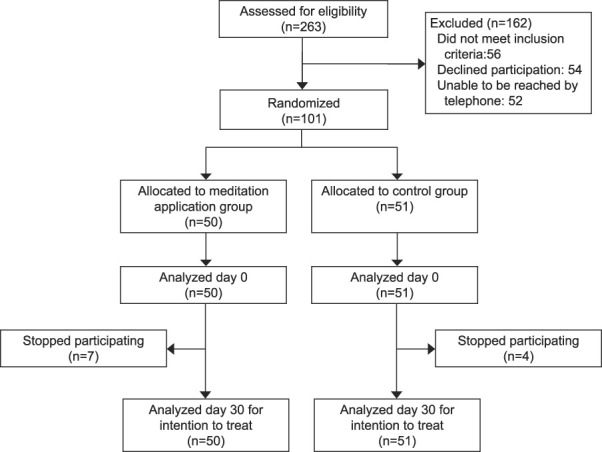
Smith. Mindfulness Effects During COVID-19. Obstet Gynecol 2021.
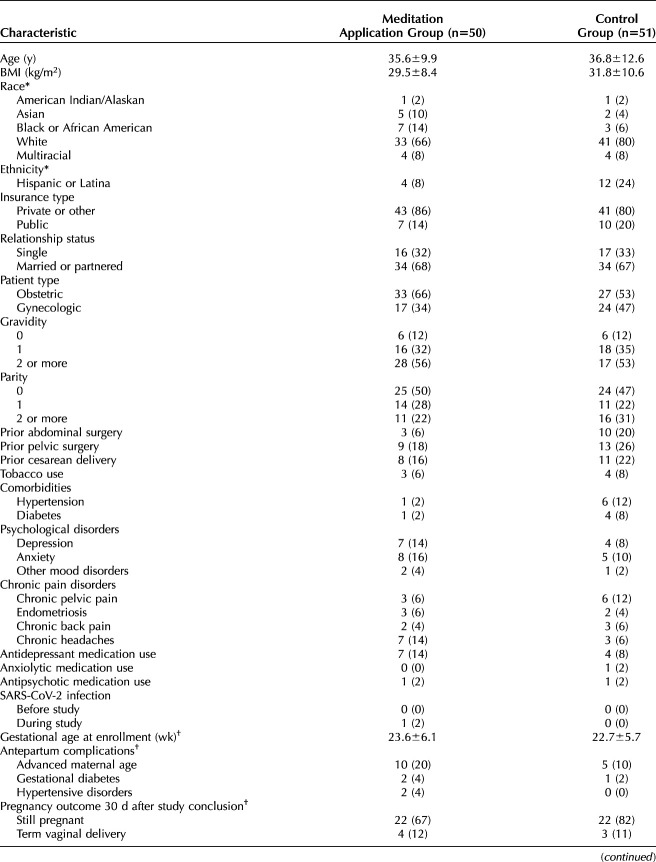
Demographic and baseline characteristics were similar between groups (Table 1). Pregnancy characteristics and outcomes were comparable between groups for the obstetric patients. Preoperative characteristics for the gynecology patients were similar between groups. A majority of patients had a previously scheduled minimally invasive hysterectomy that was delayed for at least the 30-day study period. No patients had previously received a laboratory diagnosis of SARS-CoV-2 infection before study enrollment; one patient in the intervention group had a confirmed SARS-CoV-2 infection during the study.
Table 1.
Characteristics of the Study Participants
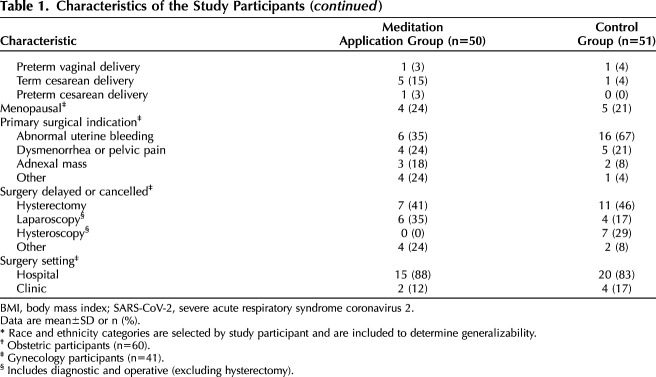
Perceived stress significantly decreased over the 30-day study period in the intervention group compared with the control group (mean difference 4.28, 95% CI 1.68–6.88, P=.002, Table 2). A significant decrease in perceived stress was also seen mid-study (day 14) in the intervention group (mean difference 4.27, 95% CI 1.30–7.24, P=.005). Perceived stress mean scores decreased in both groups with significantly greater reduction in the intervention group at day 14 and day 30 (Fig. 2). Self-reported depression was significantly less in the intervention group at days 14 and 30 (mean difference 2.27, 95% CI 0.85–3.69, P=.002 and mean difference 1.36, 95% CI 0.04–2.68, P=.04, respectively). Self-reported anxiety at days 14 and 30 was significantly less in the intervention group (mean difference 2.65, 95% CI 0.63–4.67, P=.01 and mean difference 1.89, 95% CI 0.06–3.72, P=.04, respectively). The intervention group had significantly less self-reported sleep disturbance at days 14 and 30 (mean difference 5.40, 95% CI 2.25–8.56, P=.001 and mean difference 3.16, 95% CI 0.44–5.88, P=.02, respectively). Differences by group allocation and by study time period were independently associated with the change in perceived stress as there was no significant group by time interaction found (P=.17). There were no differences between groups at baseline (day 0) for perceived stress, depression, anxiety, or sleep disturbance. Effect sizes calculated for group differences showed moderate effect in perceived stress at days 14 and 30 (d=0.69 and d=0.69, respectively). Moderate effect was seen in depression, anxiety and sleep disturbance at day 14 (d=0.77, d=0.63, and d=0.82, respectively). Modest effect was seen in depression, anxiety, and sleep disturbance at day 30 (d=0.43, d=0.43, and d=0.48). A separate per-protocol analysis for all outcomes showed no significant differences from the intention-to-treat analysis.
Table 2.
Self-Reported Psychological Measures of Participants in the Meditation and Control Groups
Fig. 2. Effect of meditation application on perceived stress mean scores at three specified study time periods.
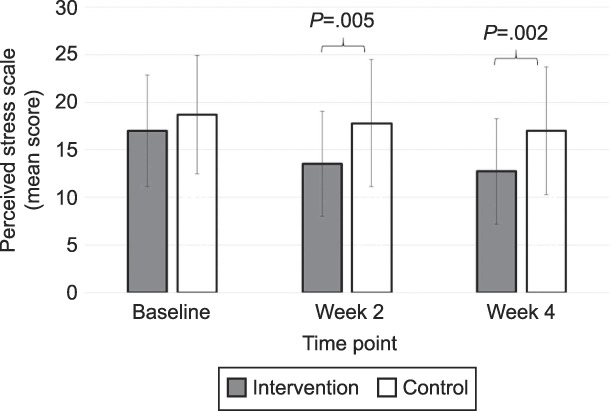
Smith. Mindfulness Effects During COVID-19. Obstet Gynecol 2021.
Subgroup analysis revealed no within-group differences at any timepoint, whether the participant was an obstetric or a gynecology patient. A comparison of the obstetric participants alone (n=60) indicated no differences at baseline for perceived stress, depression, anxiety, or sleep disturbance. The obstetric intervention group reported significantly less stress compared with the control group at day 30 (12.7±4.8 vs 17.2±6.1, P=.004). Although perceived stress scores were lower in the intervention group at day 14, they did not reach statistical significance (13.9±5.4 vs 17.8±6.7, P=.054). Depression and sleep disturbance were significantly less in the obstetric intervention group at day 14 (4.0±2.7 vs 6.8±3.2, P=.004 and 15.0±5.2 vs 21.0±6.7, P=.003, respectively). Depression and sleep disturbance at day 30 and anxiety at days 14 and 30 were less in the obstetric intervention group but did not reach statistical significance. A comparison of the gynecology participants alone (n=41) indicated that all outcomes were less in the intervention group compared with the control group at days 14 and 30; however, none reached statistical significance except the intervention group reported significantly less sleep disturbance at day 30 (15.3±6.3 vs 20.6±7.4, P=.03).
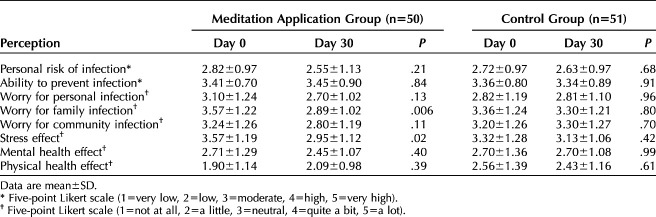
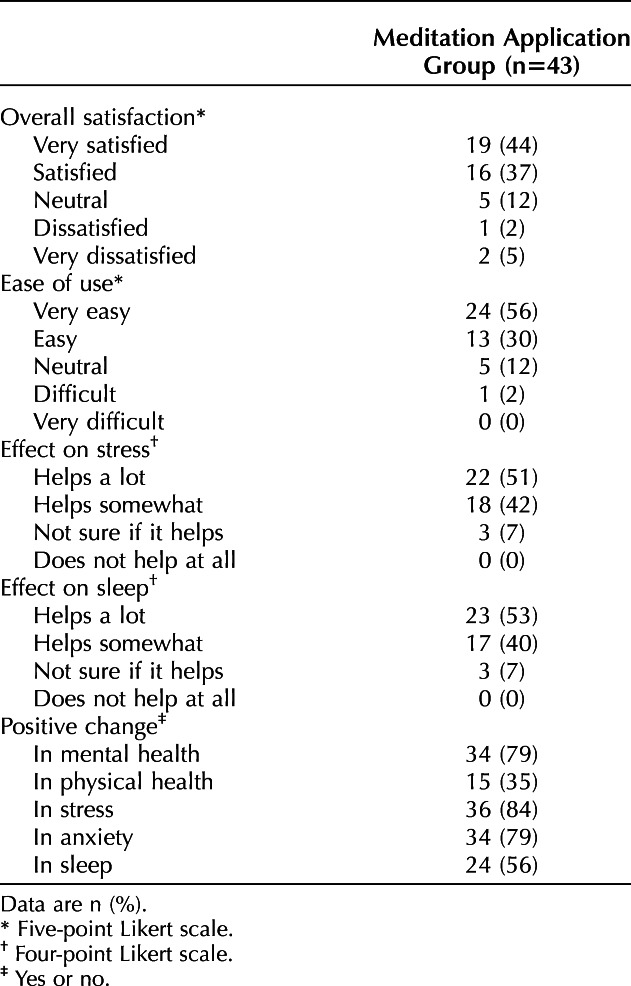
Satisfaction with the Calm app was high with a majority of participants (81%) rating very satisfied or satisfied at the end of the 30-day study period (Table 3). The app was self-reported as being easy or very easy to use for a majority of patients (86%). The self-reported positive effects on patients' stress and sleep were high, with no women selecting that the mobile app did not help at all and 7% selecting that they were not sure whether it helped with stress or sleep. The majority of patients perceived a positive change in their mental health, stress level, anxiety level, and sleep after 30 days of using the app. However, the majority of patients did not perceive a positive change to their physical health after the study. In regard to self-reported app use, 37% of patients used the app five times or greater per week and 37% of patients used the app three to four times per week, with the remainder reporting they used the app two times or fewer per week.
Table 3.
Participant Satisfaction With Meditation Application at Day 30
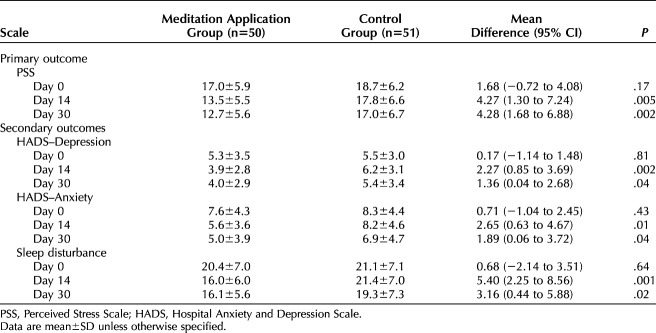
Self-reported perceptions of the COVID-19 pandemic over the 30-day study period were comparable for all participants regardless of group in regard to personal risk of infection, ability to prevent infection, worry for personal infection, and worry for community infection (Table 4). Participants in both groups did not perceive a significant change in the effect of the pandemic on their mental health or physical health over the 30-day study. Worry for family infection significantly decreased over the study period in the intervention group (P=.006) and did not significantly change in the control group. The self-reported effect of the COVID-19 pandemic on participants' stress level significantly decreased over the 30-day study in the intervention group (P=.02) and did not significantly change in the control group. This difference in stress effect over time was significantly greater in the intervention group as compared with the control group (mean difference 0.53, 95% CI 0.09–0.96, P=.02).
Table 4.
Self-Reported Perceptions of the Coronavirus Disease 2019 (COVID-19) Pandemic
One participant delivered before viability at 22 weeks of gestation during the 30-day study period; otherwise, all obstetric patients remained pregnant at completion of the study. No participants reported an adverse event or unintended effect of the study.
DISCUSSION
The results of our 101-patient randomized controlled trial indicate that self-reported stress was significantly less after 14 and 30 days of using a prescribed consumer-based mobile meditation application during the COVID-19 pandemic as compared with standard care. Differences did exist for self-reported depression, anxiety, and sleep disturbance over time with use of the mobile meditation app.
The COVID-19 pandemic has significantly affected both the physical and mental health of many women in the United States and worldwide. However, little is known about the psychological effect on our obstetric and gynecology patients, and how best to respond to the associated mental health issues that arise during the pandemic. A survey study in pregnant women reported the effect of the COVID-19 pandemic as severe on their psychological health with two-thirds reporting higher than normal anxiety.16 A multicenter study of pregnant women in China reported significantly higher rates of depression and thoughts of self-harm after the declaration of the COVID-19 pandemic.17 Pregnant women are already a vulnerable group for mental health disorders with increased prevalence of depression and anxiety.18,19 During a public health crisis such as the COVID-19 pandemic, negative effects on mental health and wellness are exacerbated with concern for the fetus. Regarding gynecology patients, the psychological effect of a cancelled surgery due to a public health crisis is also unknown. Adverse psychological effects including increased anxiety have been reported outside of gynecology when surgeries are abruptly cancelled.20,21
Mindfulness meditation as an approach to self-manage stress has been shown to benefit overall well-being.22 In pregnant women, mindfulness meditation reduces stress and depression with effects up to six months postpartum.5,6 Additionally, pregnant women with a history of depression benefit from mindfulness meditation to prevent recurrence of depression.23 Mindfulness meditation has been studied in gynecologic populations including infertility, chronic pain, and painful bladder syndrome showing improved stress, depression, and quality of life in these populations.7–10 Early investigations exist for the use of mindfulness meditation in postoperative pain after hysterectomy with positive effects.10 Our study is an important contribution to this limited body of literature and suggests improved mental health and well-being with mindfulness meditation.
During this unprecedented time of the COVID-19 pandemic, our clinic sought alternative ways to mitigate the presumed psychological effect the pandemic would have on our patients. In collaboration with Calm, Inc, we provided this low risk wellness intervention. Although our study focused on a specific meditation app during an unusual time, we highlight the need to address mental health and wellness in our patient population. The positive effects of the app on participant wellness supports the routine recommendation of wellness apps such as Calm to be used in obstetric and gynecology clinics outside of the COVID-19 pandemic to enhance patients' well-being and address mental health.
We acknowledge several limitations of our study. First, by including obstetric and gynecology patients, the population was heterogeneous. Experiencing pregnancy during a pandemic with stress for anticipated delivery may differ from stress of a cancelled surgery. Interpretation of our results is limited as one type of stress may be more amenable to mindfulness meditation compared with the other. Although a subanalysis of obstetric and gynecology patients was performed, the small sample size has limited statistical power. Justification for the combined cohort was the short enrollment period that elective surgeries were cancelled at our institution. Additionally, the participants had overall low baseline stress, were from a single institution, and were evaluated during a global pandemic, so results may not be generalizable. There was significant regional variation in the COVID-19 effect, and, at the time of our study, Arizona had not yet reached its peak infection rates, which affects the external validity of our study. Participants were presented with general information about the intervention before electing to enroll in the study, which may result in recruitment bias to patients interested in mobile wellness apps. Final limitations include use of the meditation app was self-reported, lack of follow-up after 30 days, and a high study refusal rate without data on refusers. Strengths of our study include the randomized study design that was adequately powered for the primary outcome and all psychological assessments were previously validated questionnaires.
AUTHORS' DATA SHARING STATEMENT
Will individual participant data be available (including data dictionaries)? Yes.
What data in particular will be shared? All de-identified participant data collected.
What other documents will be available? Study protocol.
When will data be available (start and end dates)? Data will become immediately available upon publication of the manuscript and ending 3 years after publication.
By what access criteria will data be shared (including with whom, for what types of analyses, and by what mechanism)? Data will be available to lead investigators with sound research proposals following appropriate institutional review board approval by password-protected files.
Footnotes
Calm, Inc donated 30-day gift codes to access the mobile application, Calm, for the study participants. Calm, Inc did not otherwise have involvement in the study. No financial compensation was received for this study.
Financial Disclosure: Dr. Mourad reports conflict unrelated to this work with Applied Medical and Intuitive Surgical as a consultant. Dr. Huberty reports conflict related to this work as a consultant for Calm, Inc in the role of Director of Science and Director of Scientific Advisory Board. Dr. Huberty conducts investigator-initiated research that utilizes the Calm application, however, Calm, Inc does not financially support her research. Dr. Huberty is paid for her consultation on an as-needed basis, however, her role is to ensure the quality of Calm's science and she has no specific obligations to the company. Dr. Huberty receives no financial incentives (eg, stocks) related to the growth or success of the company. The other authors did not report any potential conflicts of interest.
Presented at the American College of Obstetricians and Gynecologists’ Annual Clinical and Scientific Meeting, held virtually, April 30–May 3, 2021.
The authors thank our colleagues from Calm, Inc for providing the mobile meditation application to the study participants. The authors also thank Megan Puzia, MS, Breanne Laird, MS, and Elisa Martinez, MBA, for their assistance with study protocol and survey development.
The authors have confirmed compliance with the journal's requirements for authorship.
Peer reviews and author correspondence are available at http://links.lww.com/AOG/C290.
Contributor Information
Nichole D. Mahnert, Email: nichole.mahnert@gmail.com.
Janet Foote, Email: jfoote@arizona.edu.
Kelley T. Saunders, Email: Kelley.saunders@bannerhealth.com.
Jamal Mourad, Email: swwcjm@icloud.com.
Jennifer Huberty, Email: Jennifer.Huberty@asu.edu.
REFERENCES
- 1.Jago CA, Singh SS, Moretti F. Coronavirus disease 2019 (COVID-19) and pregnancy: combating isolation to improve outcomes. Obstet Gynecol 2020;136:33–6. doi: 10.1097/aog.0000000000003946 [DOI] [PubMed] [Google Scholar]
- 2.American College of Obstetricians and Gynecologists. Joint statement on elective surgeries. Accessed March 16, 2020. Available at: https://www.acog.org/news/news-releases/2020/03/joint-statement-on-elective-surgeries [Google Scholar]
- 3.Onwuzurike C, Meadows AR, Nour NM. Examining inequities associated with changes in obstetric and gynecologic care delivery during the coronavirus disease 2019 (COVID-19) pandemic. Obstet Gynecol 2020;136:37–41. doi: 10.1097/aog.0000000000003933 [DOI] [PubMed] [Google Scholar]
- 4.Huberty J, Green J, Glissmann C, Larkey L, Puzia M, Lee C. Efficacy of the mindfulness meditation mobile app “Calm” to reduce stress among college students: randomized controlled trial. J Med Internet Res 2019;21:e14273. doi: 10.2196/14273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan WL, Gau ML, Lee TY, Jou HJ, Liu CY, Wen TK. Mindfulness-based programme on the psychological health of pregnant women. Women and Birth 2019;32:e102–9. doi: 10.1016/j.wombi.2018.04.018 [DOI] [PubMed] [Google Scholar]
- 6.Pan WL, Chang CW, Chen SM, Gau ML. Assessing the effectiveness of mindfulness-based programs on mental health during pregnancy and early motherhood - a randomized control trial. BMC Pregnancy Childbirth 2019;19:1–8. doi: 10.1186/s12884-019-2503-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nery SF, Paiva SPC, Vieira ÉL, Barbosa AB, Sant'Anna EM, Casalechi M, et al. Mindfulness-based program for stress reduction in infertile women: randomized controlled trial. Stress Heal 2019;35:49–58. doi: 10.1002/smi.2839 [DOI] [PubMed] [Google Scholar]
- 8.Ball EF, Nur Shafina Muhammad Sharizan E, Franklin G, Rogozińska E. Does mindfulness meditation improve chronic pain? A systematic review. Curr Opin Obstet Gynecol 2017;29:359–66. doi: 10.1097/gco.0000000000000417 [DOI] [PubMed] [Google Scholar]
- 9.Kanter G, Komesu YM, Qaedan F, Jeppson PC, Dunivan GC, Cichowski SB, et al. Mindfulness-based stress reduction as a novel treatment for interstitial cystitis/bladder pain syndrome: a randomized controlled trial. Int Urogynecol J 2016;27:1705–11. doi: 10.1007/s00192-016-3022-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weston E, Raker C, Huang D, Parker A, Robison K, Mathews C. The association between mindfulness and postoperative pain: a prospective cohort study of gynecologic oncology patients undergoing minimally invasive hysterectomy. J Minim Invasive Gynecol 2019;27:1119–26. doi: 10.1016/j.jmig.2019.08.021 [DOI] [PubMed] [Google Scholar]
- 11.Huberty J, Eckert R, Larkey L, Kurka J, Rodríguez De Jesús S, Yoo W, et al. Smartphone-based meditation for myeloproliferative neoplasm patients: feasibility study to inform future trials. J Med Internet Res 2019;21:e12662. doi: 10.2196/12662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Heal Soc Behav 1983;24:385–96. doi: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- 13.Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716 [DOI] [PubMed] [Google Scholar]
- 14.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measures Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item bank: 2005-2008. J Clin Epidemiol 2010;63:1179–94. doi: 10.1016/j.jclinepi.2010.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulz K, Altman D, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Obstet Gynecol 2010;115:1063–70. doi: 10.1097/aog.0b013e3181d9d421 [DOI] [PubMed] [Google Scholar]
- 16.Saccone G, Florio A, Aiello F, Venturella R, De Angelis MC, Locci M, et al. Psychological impact of coronavirus disease 2019 in pregnant women. Am J Obstet Gynecol 2020;223:293–5. doi: 10.1016/j.ajog.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Y, Zhang C, Liu H, Duan C, Li C, Fan J, et al. Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China. Am J Obstet Gynecol 2020;223:240.e1–9. doi: 10.1016/j.ajog.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Screening for perinatal depression. ACOG Committee Opinion No. 757. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;132:e208–12. doi: 10.1097/AOG.0000000000002927 [DOI] [PubMed] [Google Scholar]
- 19.Fawcett EJ, Fairbrother N, Cox ML, White IR, Fawcett JM. The prevalence of anxiety disorders during pregnancy and the postpartum period: a multivariate Bayesian meta-analysis. J Clin Psychiatry 2019;80:18r12527. doi: 10.4088/JCP.18r12527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greco F, Altieri VM, Esperto F, Mirone V, Scarpa RM. Impact of COVID-19 pandemic on health-related quality of life in uro-oncologic patients: what should we wait for? Clin Genitourin Cancer 2020. [Epub ahead of print]. doi: 10.1016/j.clgc.2020.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herrod P, Adiamah A, Boyd-Carson H, Daliya P, El-Sharkawy A, Sarmah PB, et al. Winter cancellations of elective surgical procedures in the UK: a questionnaire survey of patients on the economic and psychological impact. BMJ Open 2019;9:1–8. doi: 10.1136/bmjopen-2018-028753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eberth J, Sedlmeier P. The effects of mindfulness meditation: a meta-analysis. Mindfulness 2012;3:174–89. doi: 10.1007/s12671-012-0101-x [DOI] [Google Scholar]
- 23.Dimidjian S, Goodman SH, Felder JN, Gallop R, Brown AP, Beck A. Staying well during pregnancy and the postpartum: a pilot randomized trial of mindfulness based cognitive therapy for the prevention of depressive relapse/recurrence. J Consult Clin Psychol 2016;84:134–45. doi: 10.1037/ccp0000068 [DOI] [PMC free article] [PubMed] [Google Scholar]