Abstract
As members of a devalued group, it is not surprising that smokers experience stigmatization and discrimination. But it is not clear if smokers react to these experiences by moving toward or away from their group membership and identity as smokers. Guided by the identity threat model of stigma (Major and O’Brien, 2005) we examined the process of stigmatization and its emotional, cognitive, attitudinal, and behavioral consequences. We experimentally examined how reading a stigmatizing newspaper article or a control article (Experiment 1) and recalling one’s experience with smoking discrimination or a control prompt (Experiment 2) affected smokers’ responses. We also examined the role of cultural contexts (U.S. vs. Denmark; only in Experiment 1) and smoking identity. In Experiment 1, we used a community sample of smokers from the U.S. (N = 111) and Denmark (N = 111). We found that reading the stigmatizing article (compared to the control) caused more rejection sensitivity (U.S. participants only) and more intentions to quit smoking (both U.S. and Danish participants) for smokers low in smoking identity. In Experiment 2, we used an online sample of 194 U.S. smokers and found that recalling instances of mistreatment made smokers more stressed, rejection sensitive, and interested in smoking cessation, when smokers appraised the stigma cue as threatening. Thus, we generally found that identity threat moved smokers toward leaving their stigmatized group (e.g., quitting smoking) rather than away from it. Our studies highlight the importance of understanding psychological process by which smokers distance themselves from their spoiled identity.
Keywords: stigma, identity threat, smoking, smoking cessation, rejection sensitivity
In the last half of the twentieth century, the cultural shift towards the denormalization of smoking in Western countries has created an environment where smoking is highly stigmatized (Brandt, 2007). But there is little scientific consensus regarding the consequences of using stigma to help smokers quit (Evans-Polce, Castaldelli-Maia, Schomerus, & Evans-Lacko, 2015). Research shows that smokers intending to quit are more likely to be successful if they are motivated by social pressures, such as stigma, than by health concerns or the cost of cigarettes (Baha & Le Faou, 2010). Smoking self-stigma is also associated with increased readiness to quit (Brown-Johnson, Cataldo, Orozco, Lisha, Hickman, & Prochaska, 2015) and longitudinal studies show that smokers’ agreement with denormalized and moralized smoking sentiments predicts quitting intentions (Hammond, Fong, Zanna, Thrasher, & Borland, 2006; Helweg-Larsen, 2014).
On the other hand, research shows that stigma can have negative consequences. In general, stigma negatively affects mental and physical health and is associated with increased levels of stress (Major & O’Brien, 2005). With respect to smoking, smokers with a high smoking identity who had their stigmatized status revealed in a mock interview (Helweg-Larsen, Sorgen, & Pisinger, 2019) or viewed a stigmatizing smoking public service announcement (Kim, Cao, & Meczkowski, 2018) decreased their interest in smoking cessation. Similarly, smokers who were reminded of their devalued status were less able to resist smoking (Cortland, Shapiro, Guzman and Ray, 2019). Thus, research on the effect of stigma on smoking behaviors has produced mixed findings. In the current study, we used the identity threat model of stigma as our theoretical foundation and examined smoking stigma experimentally to investigate not only the behavioral consequences but also the emotional, cognitive and attitudinal responses that might precede them.
The identity threat model of stigma (Major & O’Brien, 2005) has previously been used to examine weight-based identity threat (Major, Eliezer, & Rieck, 2012; Major, Hunger, Bunyan, & Miller, 2014) and smoking identity threat (Helweg-Larsen et al., 2019). The model states that people who hold a devalued social identity (a stigma) might experience stressful identity-threatening situations. For example, in the case of a smoker, identity threat arises from the individual’s awareness in a specific situation that they are perceived by others as a “smoker,” which they know is associated with a myriad of negative stereotypes, such as being regarded as “low status”, “dumb”, “addicted”, and “disgusting” (Helweg-Larsen, Tobias, & Cerban, 2010). According to the model, how people appraise the significance of those situations depends on three factors: smokers’ personal characteristics (e.g., smoking identity), the collective representations of the stigma (e.g., the role of culture in how smokers experience stigmatization), and the nature of the situational cues (e.g., specific reminders in a given situation that smokers belong to a devalued group).
Identity threat occurs when the stigma-relevant cues are perceived as potentially harmful to the person’s identity and as exceeding their personal coping resources. This threat can lead to a cascade of reactions/responses such as cognitive, emotional and behavioral reactions that serve to regulate identity-threatening experiences, such as suppressing negative emotions or compensating for negative stereotypes (Major & O’Brien, 2005). This process can cause resources to be temporarily depleted causing impaired performance in tasks of executive control (Inzlicht & Kang, 2010). Consistent with the predictions of the identity threat model, experimental research has found that stress impacts smokers so that they are less able to resist smoking, smoke more intensely, and receive greater satisfaction from smoking (McKee et al., 2011). Experiments also show that exposing smokers to stigmatizing messages caused greater cognitive depletion (Helweg-Larsen et al., 2019), and led them to downplay their smoking-related risks (Glock & Kneer, 2009) and increase their positive cognitions about smoking (Sussenbach, Fotuhi, & Oakes, 2013). Thus, research on the consequences of stigmatizing smokers include attitudinal, affective and cognitive reactions, which are associated with reduced likelihood of quitting smoking.
The identity threat model identifies personal characteristics that influence the appraisal of identity-threatening situations. Research has identified smoking identity as an important personal characteristic variable that can affect how smokers appraise their smoking stigma (Shadel & Mermelstein, 1996). Smoking identity (also referred to as smoking self-concept) refers to the extent to which people identify themselves as smokers (Shadel & Mermelstein, 1996). Greater smoking identity is associated with greater smoking frequency and failure in quitting smoking (Shadel & Cervone, 2011) and is a strong predictor of unsuccessful quit attempts (Tombor, Shahab, Brown, & West, 2013). Specifically, research shows that smokers with greater smoking identity react more strongly to an identity threat manipulation and exhibit greater cognitive depletion and self-exempting beliefs as well as less interest in quitting smoking (Helweg-Larsen et al., 2019). Therefore, we expected smoking identity to influence appraisals of identity-threatening situations such that those with a stronger smoking identity would exhibit outcomes that move them away from smoking cessation.
The identity threat model also identifies collective representations such as cultural context that might influence the appraisal of identity-threatening situations. In this study, we compared smokers from two countries—U.S. and Demark—to examine how cultural expectations about smoking influence smokers’ reactions to stigmatizing information. Understanding the effects of cultural context on smoking is vital yet often overlooked (Unger et al., 2003). The two countries are similar in terms of their market-driven economies and high individualism (Hofstede, 2001), whereas Denmark, compared to the U.S., can be characterized as more smoking-lenient with fewer tobacco control policies (Joossens & Raw, 2017), higher daily or occasional smoking prevalence (22.4% in Denmark and 14.0% in the U.S. in 2017; National Health Profile, 2017; Center for Disease Control, 2018) and more positive attitudes towards smoking (Helweg-Larsen & Nielsen, 2009; Helweg-Larsen, 2014). Consistent with these findings, Danish smokers, in comparison to U.S. smokers, more strongly oppose the stigmatization against them (Helweg-Larsen, Tobias, & Cerban, 2010). Therefore, we similarly expected Danish smokers compared to U.S. smokers to react to identity threat with stronger emotional, cognitive, attitudinal, and behavioral responses consistent with a reduced likelihood of quitting smoking.
In two studies, we experimentally investigated the effect of stigmatization (identity threat) on participants’ smoking-related emotions, attitudes, cognitions, and behaviors. We also examined how culture and smoking-identity moderated these effects. To manipulate situational cues in Experiment 1, smokers were randomly assigned to read and give a short speech about a newspaper article which described the negative social aspects of being a smoker (or having eczema in the control condition), whereas in Experiment 2, smokers recalled their own past experiences with smoking stigmatization (or with age stigmatization in the control condition). We predicted that the stigma reminders (compared to the control) would lead to greater stress, cognitive depletion (measured with a Stroop test), positive attitudes about smoking, rejection sensitivity, smoking intensity (measured with a smoking topography device before and after the stigma reminder manipulation, Study 1 only), and lower perceived risk, smoking cessation intentions, and self-efficacy. We also predicted that Danish smokers (compared to U.S. smokers; Experiment 1 only) as well as smokers with high smoking identity would react more strongly to the stigma reminder manipulations.
Experiment 1
Method
Participants.
To estimate the number of participants required, we used G* Power (version 3.1.9.2; Faul, Erdfelder, Lang, & Buchner, 2007) using the “ANOVA: Fixed Effects” and testing for a 3-way interaction (df = 1; 8 groups). Based on a similar manipulation used for weight stigma (Major et al., 2014) we set the effect size at ƒ2 = .20, power to .80, and alpha to .05 and found that we needed 199 participants. We recruited 240 participants (120 in each country) because we expected some participant attrition. We stopped collecting data when the desired sample size was attained, and we did not analyze data during the data collection process.
Out of the 240 total participants, data from 18 participants (9 U.S., 9 Danish) were excluded after data collection because they had personally experienced the ailment which was the topic of the control article (eczema) and were assigned to the control condition, did not meet eligibility requirements, or were unable or unwilling to fully participate in the study. No participants dropped out of the study in response to the manipulation, thus there was no differential attrition. The final sample consisted of 111 Americans and 111 Danes.
The gender distribution was similar between the two countries, with 56.8% men and 43.2% women in U.S. and 51.4% men, 46.8% women, and 1.8% non-binary in Denmark, χ2 (2) = 2.46, p = .29. Participants in the U.S. reported their race as White (82.9%), Black/African-American (11.7%), American Indian/Alaskan Native (1.8%) and other (3.6%); 3.6% identified as Hispanic. Danish participants reported their national origin (people in Denmark categorize themselves by national origin and not by race) as Danish/White (89.2%), immigrants or descendants from other Western countries (3.6%), and immigrants or descendants from non-Western countries (7.2%). See supplemental materials for more participant information.
Procedure.
Translation.
All materials were translated from English to Danish by the first author (bilingual in Danish and English) and the last author (native Danish speaker). The translations were also independently reviewed for accuracy and equivalence by another bilingual researcher.
Recruitment.
We recruited participants by distributing fliers in local shops and by posting online ads on Facebook, Instagram, Craigslist, and local neighborhood forums and newspaper. We also called referrals made by participants.
Prescreening.
We prescreened participants either via email or phone. During the pre-screening, we asked participants if they met the eligibility criteria: smoked an average of 10 or more cigarettes per day, were 18 years or older, lived in their respective countries for the past 10 years, smoked for the past 2 years, considered themselves a smoker, and had not participated in the study before. Participants were asked not to smoke 2 hr prior to the start of the study and to bring two of their own cigarettes to smoke. We paid the participants $40 to participate, $10 for being on time/not changing the appointment, and $10 for referring someone who participated in the study. Danish participants were paid corresponding amounts in Danish kroner. The study was approved by the Dickinson College Institutional Review Board.
Informed consent and initial questionnaire.
Participants read and signed a consent form. Participants then answered demographic questions, smoking behavior questions, and questions on smoking identity on a Qualtrics survey on the computer.
Smoking intensity.
Participants were asked to smoke two cigarettes through a smoking topography device (one before and one after the manipulation). We demonstrated how to attach a new mouthpiece, insert the cigarette into the device and hold the device to smoke through it. The participants were asked to relax and read a magazine while smoking each cigarette.
Stigma reminder manipulation.
After smoking the first cigarette, we asked participants to read a newspaper article (about smoking or eczema), and to prepare a speech in which they were to explain the main points of the article (e.g., why people try to hide their smoking/eczema). The participants read the article and prepared their answers for 8 min and then gave a speech for 3 min, which was video recorded. The purpose of the speech was to make sure that participant read the article and engaged with the viewpoints presented. After their speech, participants smoked their second cigarette through the smoking topography device.
Post manipulation tasks.
Participants completed a computerized Stroop test followed by additional questions on the Qualtrics survey. We then debriefed and paid participants.
Materials (listed in the order they appeared).
Smoking identity.
Smoking identity was measured using five items (Shadel and Mermelstein, 1996), such as, “Smoking is a part of my self-image.” Scale was from strongly disagree (1) to strongly agree (5). The scores were averaged such that higher scores indicated a stronger smoking identity, αU.S. = .82; αDK = .86.
Smoking intensity.
The CReSS device was chosen to measure smoking intensity because of its reliability and validity (Lee, Malson, Moolchan, Waters, & Pickworth, 2003; Perkins, Karelitz, Giedgowd, & Conklin, 2012), and because it has been used successfully in other studies as a dependent variable (Arndt et al., 2013; Fucito & Juliano, 2009; McClernon et al., 2005). See supplemental materials for further information. As expected, participants smoked with greater intensity at T1 (M = .07, SD = .82) than at T2 (M = −.07. SD = .78); t(218) = 3.10, p <. 01.
Stigma reminder manipulation.
Participants were randomly assigned to read an article (ostensibly from a major U.S. or a major Danish newspaper) explaining that smoking [or eczema] is viewed as disgusting, negatively affects interpersonal and romantic relationships, and causes difficulty in getting and keeping a job (modelled by an article used by Major et al., 2014).
Cognitive depletion.
Cognitive depletion was calculated using the Stroop test which requires participants to quickly identify the color of words in which the word itself is either congruent (e.g., the word yellow is written in yellow color) or incongruent (e.g., the word yellow is written in blue color). Participants watched a fixation target (a white cross) leading into a word on the screen after 200 ms. The word (in red, blue, yellow or green) remained on the screen until the proper color-key was pressed and the response time was measured by the software. See supplemental materials for further details. A Stroop interference score resulted from subtracting the congruent from the incongruent trial averages, with higher scores reflecting greater cognitive depletion. As expected, participants answered more quickly in congruent (M = 908.19, SD = 232.96) than incongruent (M = 1084.82, SD = 325.79) trials, t(220) = −14.90, p <.001.
Self-reported stress.
Participants report how much they felt: nervous, anxious, worried, uncomfortable and overwhelmed (Major et al., 2012) on a scale from not at all (1) to a great deal (4). Scores were averaged with higher scores indicating more stress, αU.S. = .92; αDK = .83.
Rejection sensitivity.
The smoking rejection sensitivity scale consisted of nine situations, which previous research (e.g., Helweg-Larsen et al., 2010) shows are areas of concern for some smokers, modeled on research on rejection sensitivity (Brenchley & Quinn, 2016). For example, “Imagine that you at work, and you are going outside for a smoke break. A coworker walks by and comments on the high price of cigarettes.” For each item, the participant had to answer two questions. For example, “How concerned/anxious would you be over whether your coworker was judging you because of your smoking?” from very unconcerned (1) to very concerned (4), and “I would expect that my coworker was judging me” from very unlikely (1) to very likely (4). Higher scores indicated greater rejection sensitivity, αU.S. = .88; αDK = .83.
Perceived risk.
Perceived risk was measured by asking, “Imagine you in the future smoke a pack of cigarettes every day. What then is your chance of getting lung cancer in your lifetime?” (Weinstein et al., 2007) using a scale from not at all likely (1) to extremely likely (5).
Positive cognitions about smoking.
Positive cognitions were measured using five items such as “Smoking is relaxing” using a scale from strongly disagree (1) to strongly agree (5) (Sussenbach et al., 2013); αU.S. = .77; αDK = .60.
Self-exempting beliefs.
Self-exempting beliefs were measured using 17 items from the self-exempting beliefs scale, such as “The medical evidence that smoking is harmful is exaggerated” (Oakes, Chapman, Borland, Balmford, & Trotter, 2004). The scale was from strongly disagree (1) to strongly agree (5), αU.S. = .87; αDK = .82
Smoking cessation intentions.
Smoking cessation intentions were measured using three items from Helweg-Larsen (2014): “Do you have plans to quit smoking?” (measured on a 3-point scale from Yes, within a month (1) to No, I do not have plans to quit smoking (4), “Do you want to stop smoking?” and “Would you like to smoke less” measured on a 4-point scale from Not at all (1) to “A great deal (4). The responses in the first item were reverse scored and then responses from all items were turned into z-scores and averaged, αU.S. = .78; αDK = .77
Self-efficacy.
Self-efficacy was measured using a single item adapted from Velicer, Diclemente, Rossi, & Prochaska (1990), “How confident are you that you could quit smoking for good if you wanted to?” Participants responded on a scale from not at all (1) to extremely (5).
Results
Analytic Strategy.
We conducted a series of hierarchical regression analyses (ordinary least squares regression) using PROCESS v 3.1 macro (Hayes, 2018) in SPSS (v. 25). All analyses examined the condition (smoking stigma vs. control) x country (U.S. or Denmark) x smoking identity (variable kept continuous) for each dependent variable. We set regression parameters at 1000 bootstrap bias-corrected samples, 95% confidence intervals, and mean-centered products, to test for all effects and interactions using Model 3. We report unstandardized regression weights along with their p values and confidence intervals. Figures depict smoking identity as dichotomized at 16th and 84th percentile of the data (as recommended by Hayes, 2018). Table 1 shows all bivariate correlations, separately for each condition.
Table 1.
Bivariate Correlations among Study Variables for the Stigma Reminder and Control Conditions in Experiment 1.
| Measure | Control Condition Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stigma-Reminder Condition Mean (SD) | 2.79 (0.85) | −.07 (0.80) | 0.17 (0.13) | 2.09 (0.95) | 2.51 (0.51) | 3.47 (0.93) | 3.32 (0.74) | 2.40 (0.60) | 0.09 (0.87) | 3.14 (1.17) | |
| 1. Smoking identity | 3.14 (0.85) | -- | .03 | −.116 | .12 | .12 | −.07 | .43** | .29** | −.22* | −.44** |
| 2. Smoking intensity | −.06 (0.76) | .09 | -- | −.16 | .24 | −.08 | −.07 | .05 | .01 | .02 | .04 |
| 3. Cognitive depletion | 0.16 (0.15) | .03 | −.04 | -- | .17 | .14 | .004 | −.05 | −.01 | .10 | −.15 |
| 4. Self-reported stress | 2.11 (0.89) | .02 | −.06 | .21* | -- | .41** | .31** | −.09 | .02 | .16 | −.13 |
| 5. Rejection sensitivity | 2.45 (0.46) | .30** | −.02 | .11 | .21* | -- | .43** | .02 | .04 | .23* | −.26** |
| 6. Perceived risk | 3.49 (0.96) | .14 | −.02 | .11 | .18 | .29** | -- | .08 | −.23* | .26* | .04 |
| 7. Positive Cognitions | 3.39 (0.66) | .26** | −.09 | .02 | −.08 | .04 | −.15 | -- | .38** | −.40** | −.33** |
| 8. Self-exempting beliefs | 2.42 (0.53) | .24* | −.14 | .09 | .02 | −.13 | −.27** | .34** | -- | −.30** | −.13 |
| 9. Smoking cessation intentions | −0.10 (0.77) | .12 | .17 | −.04 | .21* | .24* | .16 | −.15 | −.17 | -- | .03 |
| 10. Self-efficacy | 2.96 (1.14) | −.21* | −.12 | −.02 | −.08 | −.11 | .01 | −.12 | −.33** | −.03 | -- |
Note.
p < .05
p < .01.
Correlations for participants in the stigma-reminder condition (N = 111–114) are presented above the diagonal and correlations for participants in the control condition (N =107–108) are presented below the diagonal. For the correlations involving the smoking intensity variable, we controlled for smoking intensity at T1. T-tests show no difference among any of the variables between the two conditions.
Smoking intensity.
Analysis of smoking intensity (T2 controlling for T1) revealed a significant interaction of smoking identity and country, b = −0.27, p < .001, 95% CI [−0.44, −0.09], such that among Americans, stronger smoking identity was associated with higher smoking intensity, b = 0.17, p = .01, 95% CI [0.04, 0.30] whereas among Danes, smoking identity was not associated with smoking intensity, b = −0.09, p = .13, 95% CI [−0.22, 0.03]. Since this interaction did not involve the manipulated variable, we did not further interpret this finding. No other effects or interactions were significant, bs = −0.08 to 0.04, ps = .34 to .96.
Cognitive depletion.
Results revealed no significant effects or interactions, bs = −0.06 to 0.02, ps = .18 to .81.
Self-reported stress.
Results showed that there was a significant effect of country, b = −.90, p < .001, 95% CI [−1.12, −0.68], such that Americans reported more stress emotions than Danes. No other effects or interactions were significant, bs = −0.11 to 0.08, ps = .22 to .88.
Rejection sensitivity.
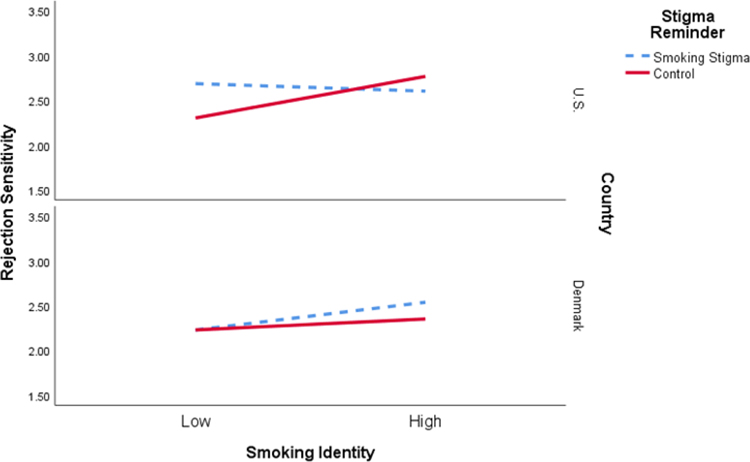
Analysis of rejection sensitivity revealed that there was a significant effect of country, b = −.25, p < .001, 95% CI [−0.37, −0.13], such that Americans reported greater rejection sensitivity than Danes. Additionally, there was a significant effect of smoking identity, b = .11, p < .001, 95% CI [0.04, 0.18], such that those who identified strongly as a smoker expressed higher rejection sensitivity. Further, there was a significant three-way interaction (see Figure 1) between stigma reminder, smoking identity, and country, b = −.41, p < .001, 95% CI [−0.69, −0.13]. Probing this interaction revealed that the three-way interaction was a result of a significant two-way interaction between stigma reminder and smoking identity in the U.S. sample and not in the Danish sample. For Danish participants, stigma reminder and smoking identity did not affect rejection sensitivity, b = −.10, p = .29. For U.S. participants stigma reminder and smoking identity interacted to affect rejection sensitivity, b = .30, p < .001, such that when smoking identity was low, participants became more rejection sensitive as a result of the stigma-reminder condition compared to the control condition, b = −.38, p < .001, 95% CI [−0.64, −0.12]. However, when smoking identity was high, participants were not affected by the stigma reminder, b = .16, p = .18, 95% CI [−0.08, 0.41]. No other effects or interactions were significant, bs = −0.10 to 0.11, ps = .12 to .94.
Figure 1.
The effect of stigma reminder on rejection sensitivity was moderated by country and smoking identity such that among U.S. participants, the stigma reminder compared to the control, led to greater rejection sensitivity, but only among smokers with a low smoking identity in Experiment 1.
Perceived risk.
There was a significant effect of country, b = −.35, p = .01, 95% CI [−0.61, −0.10], such that Americans perceived greater risk than Danes. No other effects or interactions were significant, bs = −0.20 to 0.24, ps = .11 to .94.
Positive cognitions about smoking.
There was a significant effect of country, b = .29, p < .001, 95% CI [0.12, 0.46], such that Americans had fewer positive cognitions about smoking than Danes. There was also a significant effect of smoking identity, b = .29, p < .001, 95% CI [0.19, 0.39], such that those with lower smoking identity had fewer positive cognition about smoking. No other effects or interactions were significant, bs = −0.18 to −0.01, ps = .09 to .65.
Self-exempting beliefs.
There was a significant effect of smoking identity, b = .18, p < .001, 95% CI [0.10, 0.27], such that those with lower smoking identity had fewer self-exempting beliefs. Additionally, there was a marginally significant interaction between country and smoking identity, b = −.16, p = .06, 95% CI [−0.33, 0.01], such that among Americans, greater smoking identity was associated with higher self-exempting beliefs, b = 0.26, p < .001, 95% CI [0.14, 0.39] whereas among Danes, smoking identity was not associated with self-exempting beliefs, b = 0.10, p = .09, 95% CI [−0.02, 0.22]. However, since this interaction did not involve the manipulated variable, we did not further interpret this finding. No other effects or interactions were significant, bs = −0.06 to 0.18, ps = .15 to .78.
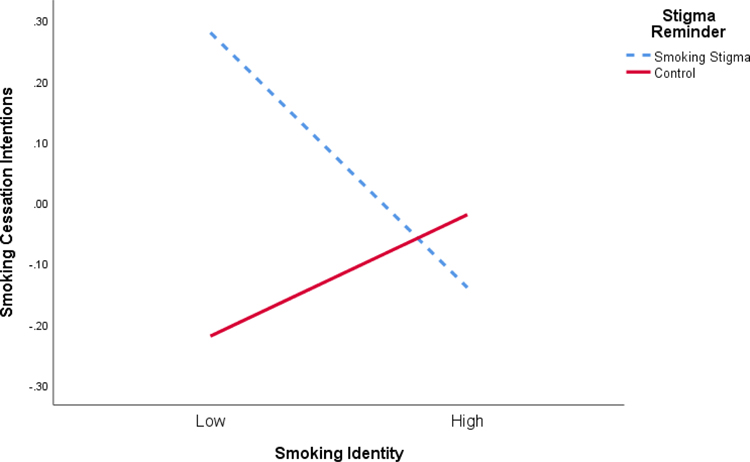
Smoking cessation intentions.
There was a significant interaction of stigma reminder and smoking identity on smoking cessation intentions, b = .35, p = .001, 95% CI [0.09, 0.60]. Probing the interaction revealed (see Figure 2) that when smoking identity was low, the stigma reminder (compared to the control) increased participants’ intentions to quit smoking, b = −.50, p < .001, 95% CI [−0.83, −0.17], whereas there were no effects when smoking identity was medium, b = −.16, p = .16, 95% CI [−0.38, 0.06] or high, b = .12, p = .44, 95% CI [−0.18, 0.42]. No other effects were significant, bs = −0.27 to 0.19, ps = .13 to .30.
Figure 2.
The effect of stigma reminder on smoking cessation intentions was moderated by smoking identity such that when reminded of their stigma, participants with a lower smoking identity had higher intentions to quit in Experiment 1.
Self-efficacy.
There was a significant effect of smoking identity, b = −.29, p < .001, 95% CI [−0.42, −0.15], such that those with lower smoking identity had higher self-efficacy. No other effects or interactions were significant, bs = −0.26 to 0.19, ps = .09 to .93.
Discussion
Based on previous research (Helweg-Larsen et al., 2019), we predicted that smoking stigma reminders (compared to a control) would lead participants to report higher levels of stress, be more cognitively depleted, hold more positive attitudes about smoking, be more rejection sensitive, smoke with a greater intensity, and report lower perceived risk, cessation intentions, and self-efficacy. We also predicted that these effects would differ according to the participants’ country and smoking identity, such that participants from the U.S. and those high in smoking identity would react more strongly to the stigma reminder. Consistent with the predictions, we found that the stigma reminder affected participants such that they became more rejection sensitive (only U.S. participants) but participants also reported greater intentions to quit smoking (both U.S. and Danish participants; but only among low smoking identity participants). We will discuss the cross-cultural effects in the general discussion.
Putting this unexpected result in perspective, identity threat may lead to different outcomes depending on the specific stigma or stigmatized group. For example, in a study using a similar manipulation but focusing on overweight college students, Major et al. (2014) found that after reading the stigmatizing article (compared to a control article), self-perceived overweight women consumed more calories and had lower diet self-efficacy. However, in our study, reading the stigmatizing article did not lead smokers to smoke with a greater intensity (a behavioral measure of consumption in the context of smoking) or lower their self-efficacy for quitting smoking. Both studies found that reading the article was associated with more rejection sensitivity but not greater stress.
The identity threat model of stigma specifies that the stigma cue (manipulation) needs to elicit identity threat, which occurs when stigma is appraised as both exceeding perceived coping resources and pertaining to one’s social identity, to yield observable outcomes (Major & O’Brien, 2005). It is possible that our participants were either experienced copers or just did not think the examples of stigma (in hiring, romantic relationship, etc.) pertained to them personally. The video-recorded prompts did not ask about their personal experiences thus a content analysis could not reveal information about whether they actually experienced identity threat.
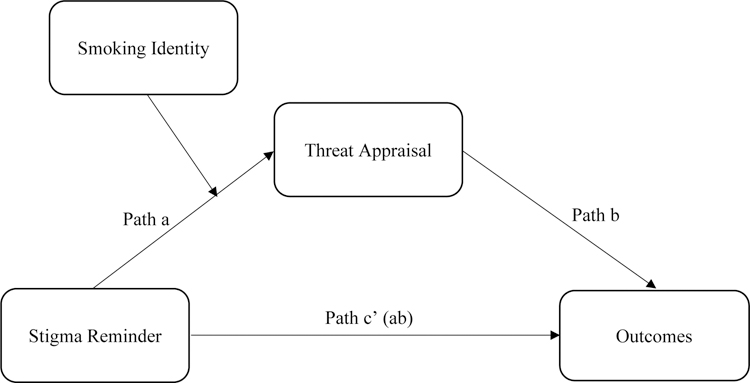
Therefore, we designed the manipulation in Experiment 2 so that participants could directly report the degree of threat they felt. We asked smokers to describe a specific stigmatizing event (smoking or age-related) that they had personally experienced and then asked if they appraised that event as threating. In this mediated moderation model (see Figure 3) we expected the stigma reminder manipulation (smoking vs. age-related) would affect smoking-related outcomes via the mediator (threat appraisal). We decided to stick to our initial predictions (since we were unsure of whether reading the smoking article in Experiment 1 had, in fact, generated threat) and therefore expected that smoking stigma would lead to increased stress, cognitive depletion, positive attitudes about smoking, rejection sensitivity, and decreased risk perceptions, smoking cessation intentions and self-efficacy, via threat appraisals. Similarly, we stuck to our initial prediction that a stronger smoking identity would intensify this pattern. Because country (U.S. vs Denmark) did not play a significant role in Experiment 1, we only used smokers from the U.S. in Experiment 2.
Figure 3.
The hypothesized moderated-mediation model of the effect of stigma reminder on outcomes, specifically stress, cognitive depletion, positive cognitions about smoking, perceived risk, self-exempting beliefs, rejection sensitivity, smoking cessation intentions and self-efficacy in Experiment 2.
Experiment 2
Method
Participants.
The study was posted on Prolific Academic, an online crowdsourcing platform, and a total of 340 participants attempted to take the study. Of these, 82 did not consent or were ineligible to participate (because they were not of U.S. nationality, did not smoke 10 or more cigarettes a day, or were attempting to take the study using a phone/tablet). Additionally, 50 participants started but did not complete the study. We found no evidence of differential attrition in that the number of people who dropped out after seeing the manipulation were about the same (7 in the experimental condition and 10 in the control condition), χ2 (1) = 0.97, p = 0.33. Of the remaining 208 participants, we deleted data from 14 participants because they wrote about events that did not follow the prompt (e.g., they wrote about a friend’s experiences instead of their own, wrote about smoking discrimination in the age condition, etc.).
Of the final sample containing 194 participants, 56.2% were female and 43.8% were male. Participants reported their race as White (95.9%), Black/African-American (2.1%), American Indian/Alaskan Native (0.5%), Asian (1.0%) and other (0.5%); 3.1% identified as Hispanic. The average age of the participants was 42.1 years (SD = 12.02, range: 20–71), and they smoked an average of 20.5 cigarettes a day (SD = 7.75, range: 10–60).
Because this was a new manipulation, we did not calculate a sample size a priori, but instead aimed to get as many participants as we could (given our eligibility criteria). After data collection (we did not analyze data during the data collection process), we calculated a sensitivity power analysis in G*Power (version 3.1.9.2) to examine the minimum effect size that the sample of 194 would be able to detect (with alpha at .05 and power at .80). Because a model of “moderated mediation” is not available as an option, we selected “linear multiple regression, fixed model, R2 increase” with 1 tested predictor and 4 total predictors. The result was an effect size of f2=.04 suggesting that the study was adequately powered to detect a small effect size.
Procedure.
Participants were recruited through Prolific Academic by making the study available to potential participants who had indicated that their nationality was American and that they smoked more than 10 cigarettes a day. We also asked participants to not use their phones/tablets because one of our measures required a keyboard and flash player. Participants completed the study in 23 min (on average) and were paid the equivalent of $6.75 per hour. The study was approved by the Dickinson College Institutional Review Board.
In Qualtrics, participants read the informed consent form and if they agreed to participate, we checked that they were eligible. Eligible participants then answered questions about their background, smoking habits, and smoking identity before being randomly assigned to either the smoking stigma condition or the control condition. After completing the manipulation task, they reported the degree of threat and were then asked to complete an online version of the Stroop test twice and report their scores on Qualtrics. Participants then completed additional measures on Qualtrics before being asked to go to a smoking cessation website to look at their page before returning to Qualtrics. In Qualtrics, they answered questions about the webpage they visited and about their smoking cessation intentions. We then debriefed participants and thanked them for their time.
Materials (listed in the order they appeared).
Smoking identity.
Smoking identity was measured using the same 5-item scale as in Experiment 1, α = .82.
Stigma reminder manipulation.
We piloted tested these instructions with 10 participants (who did not participate in the current study) to make sure everyone understood the task and were able to write 50 words about prompt. We made minor adjustments in the wording based on the pilot testing. Participants were randomly assigned to a smoking stigma condition or a control (age) condition in which they were asked to describe a specific event or situation in which they personally experienced mistreatment because of their smoking or age. The exact wording is in the supplemental materials.
Threat appraisal.
We assessed threat appraisal using five items adapted from The Primary Appraisal of Identity Threat (PAIT) scale (Berjot, Girault-Lidvan, & Gillet, 2012). The items asked participants to rate how much they felt judged, attacked, inferior, and threatened as well as how well they were able to cope with the situation they had described earlier (5-point scale from not at all to a great deal). Scores from the coping item were reverse coded and averaged with scores from the other four items to produce a threat appraisal score, α = .85.
Cognitive depletion.
Participants took an online Stroop test (http://cognitivefun.net/test/2) and copied their scores into Qualtrics. They completed it twice and we only used the second scores. Participants showed the expected effect of answering more quickly in congruent (M = 1051.55, SD = 390.49) than incongruent (M = 1295.65, SD = 466.46) trials, t(184) = −9.48, p <.001. The Stroop score was calculated by subtracting the congruent from the incongruent times; higher scores indicated more cognitive depletion.
Measures from Experiment 1.
We measured stress (α = .90), rejection sensitivity (α = .76), perceived risk (single item), positive cognitions (α = .64), self-exempting beliefs (α = .86), smoking cessation intentions (α = .78) and self-efficacy (single item). For the self-exempting beliefs scale we used only 8 of the 17 items (2 from each of the 4 domains the scale covers) and for the rejection sensitivity scale we used only 8 of the 18 items pertaining to four situations.
Time spent viewing a smoking cessation webpage.
Participants were told that a link on the next Qualtrics page would open a webpage (https://smokefree.gov/) and that we wanted them to look at the page for as long as they liked (adapted from Landau, Cameron, Arndt, Hamilton, Swanson, & Bultmann, 2019). Qualtrics measured how long the participants spent looking at the webpage (M = 57 s, SD = 69 s, range = 2–471 s). The number of seconds they spent on the webpage was log-transformed to reduce positive skew. There were no outliers (e.g., no scores outside of 3 SD). A longer time spent viewing the webpage indicated greater interest in smoking cessation.
Interest in cessation tools.
Interest in cessation tools from the webpage as assessed by asking (using a 5-point scale from strongly disagree to strongly agree) three questions such as “I would like to learn more about topics related to quitting,” (Landau et al., 2019), α = .88.
Results
Analysis strategy.
In PROCESS we used Model 7 for the moderated mediation analysis and Model 4 for simple mediation. Table 2 shows the bivariate correlations.
Table 2.
Bivariate Correlations among Study Variables for the Stigma Reminder and Control Conditions in Experiment 2.
| Measure | Control Condition Mean (SD) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stigma-Reminder Condition Mean (SD) | 3.20 (0.84) | 3.42 (0.99) | −0.10 (0.09) | 1.99 (0.85) | 2.53 (0.54) | 3.45 (0.98) | 3.43 (0.71) | 2.63 (0.81) | 1.54 (0.43) | 3.27 (1.17) | −0.01 (0.81) | 2.71 (1.13) | |
| 1. Smoking identity | 3.01 (0.87) | -- | .22* | −.01 | .15 | .07 | .14 | .42** | .23* | −.07 | .02 | −.13 | −.02 |
| 2. Threat appraisal | 3.09 (1.08) | .02 | -- | .12 | .23* | .24* | .05 | .20* | .18 | .02 | .37** | .15 | −.07 |
| 3. Cognitive depletion | −0.09 (0.06) | .04 | −.19 | -- | .10 | .09 | .07 | .13 | −.08 | −.03 | .03 | −.03 | −.10 |
| 4. Self-reported stress | 1.83 (0.83) | .27* | .44** | −.05 | -- | .26** | −.08 | .10 | .15 | −.03 | .18 | .02 | −.23* |
| 5. Rejection sensitivity | 2.42 (0.58) | .04 | .12 | −.08 | .30* | -- | .10 | −.12 | −.19 | .09 | .42** | .32** | −.14 |
| 6. Perceived risk | 3.17 (0.99) | −.14 | −.09 | −.02 | .01 | .30** | -- | −.15 | .29** | .002 | .02 | .12 | −.10 |
| 7. Positive cognitions | 3.27 (0.72) | .50** | .04 | −.04 | −.02 | −.23* | −.33** | -- | .30** | −.27** | −.17 | −.33** | .14 |
| 8. Self-exempting beliefs | 2.45 (0.87) | .34** | .10 | −.12 | −.05 | −.31** | −.42** | .53** | -- | .02 | −.12 | −.37** | .10 |
| 9. Time spent viewing webpage | 1.53 (0.47) | .02 | −.03 | −.09 | .02 | −.07 | −.03 | −.21* | .01 | -- | .18 | −.02 | −.10 |
| 10. Interest in cessation tools | 3.23 (1.18) | −.02 | .04 | .03 | .14 | .30** | .03 | −.31** | −.38** | .16 | -- | .56** | .02 |
| 11. Smoking cessation intentions | 0.01 (0.90) | −.17 | −.04 | .11 | .20 | .39** | .22* | −.34** | −.55** | .09 | .55** | -- | .05 |
| 12. Self-efficacy | 2.53 (1.19) | −.15 | .01 | −.01 | .08 | −.01 | −.07 | .07 | .11 | −.01 | −.02 | .11 | -- |
Note.
p < .05
p < .01.
Correlations for participants in the stigma-reminder condition (Ns = 103–104) are presented above the diagonal and correlations for participants in the control condition (Ns =82–90) are presented below the diagonal. T-tests show no difference among any of the variables between the two conditions.
Moderated mediation model.
We examined the full model (see Figure 3) and found that the moderated mediation model (index of moderated mediation in PROCESS) was not significant for any of the dependent variables. That is, smoking identity did not moderate the mediational path from stigma reminder to any of the dependent variables through threat appraisals, bs = −.0642 to .0008, SEs = .0017 to .0507.
Mediation model.
We examined a revised model without the moderating effects of smoking identity, such that the effects of stigma reminder on the dependent variables were mediated by threat. First, participants in the smoking-stigma condition perceived more threat appraisal than those in the control condition, b = −.33, p = .03, 95% CI [−0.62, −0.03]. That is, people rated their personal experiences as more threatening when they pertained to smoking stigma than age stigma. More importantly, threat appraisal mediated the effect of stigma reminder on stress, such that those who were in the smoking condition were more threatened than those in the control condition, and this threat was associated with greater stress, b = −.09, SE = .04, 95% CI [−0.18, −0.01], greater rejection sensitivity, b = −.03, SE = .02, 95% CI [−0.08, −0.001], and more interest in cessation tools, b = −.03, SE = .02, 95% CI [−0.08, −0.001]. There was no direct effect of stigma reminder on these three dependent variables [bs = −.04 to −.07, ps = .36 to .81] but there was a direct effect of stigma reminder on perceived risk such that those in the smoking condition (compared to the control) reported greater perceived risk, b = −.29, SE = .14, p = .04, 95% CI [−0.57, −0.01], but the indirect path was not significant, b = .01, SE = .03, 95% CI [−0.05, 0.07]. No other results were significant (bs = −.14 −.08).
Discussion
The results were generally consistent with the Experiment 1 results. We found that the smoking stigma reminder (compared to the control) lead participants to experience greater stress, rejection sensitivity, and interest in smoking cessation tools, when participants perceived their smoking-stigma recollections as threatening. These results were not moderated by smoking identity. We also found that the smoking reminder had a direct effect on perceived risk such that smokers who recalled a smoking (as opposed to an age) discriminatory event thought they were at a greater risk of getting lung cancer. Increased smoking risk is generally associated with greater interest in quitting (Fotuhi et al., 2013). Thus, as expected we found that the smoking-stigma cue (when it was seen as threatening) led to stress and rejection sensitivity, but contrary to our hypothesis, and generally consistent with the results of Experiment 1, we found that (threatening) stigma cues lead to interest in smoking cessation. Regardless of perceived threat, smoking stigma (compared to the control) was associated with greater perceived personal risk. In sum, again, stigma caused smokers to move toward rather than away from smoking cessation.
This experiment made several important contributions research on smoking and identity threat. First, we developed a manipulation that allows for the measurement of threat by having participants recall their own experiences of discrimination. We showed that smokers were able to think of a smoking-related (or age-related) stigmatizing event they had experienced in their own lives and that they were able to rate these personal recollections for degree of threat. This manipulation could be used in other studies to examine threat related to stigma in domains other than smoking. Second, we found that the effects of stigma reminder on the outcome variables goes through the mediated pathway of threat, or simply, the stigma reminder needs to be appraised as threatening to affect outcomes (perceived risk was the only exception to this pattern). Finally, we found evidence for quitting interest via the interest in cessation tools variable which highlights the importance of using a variety of measures to investigate cessation interest.
General Discussion
In Experiment 1, we found that reminding smokers of their stigmatized identity made people who did not strongly identify as smokers more rejection sensitive (U.S. only) and more willing to quit smoking (both U.S. and Denmark). In Experiment 2, we found that reminding smokers of their stigmatized identity made them more stressed, rejection sensitive, and interested in tools to aid smoking cessation, when the smokers appraised the reminder as threatening. We also found that the smoking manipulation directly increased perceived risk; smoking identity did not affect the pattern of these results. Thus, in both studies, identity threat moved smokers toward leaving their stigmatized group (e.g., toward smoking cessation).
These findings bring new perspectives to the identity threat model of stigma (Major & O’Brien, 2005). First, they highlight the importance of directly assessing how threatening (if at all) participants perceive various identity-related situations or experiences. We found only one direct effect in Experiment 2 suggesting that people can think of discriminatory events but they only lead to changes in emotions and behaviors, when such events are assessed as threatening. Second, we found no evidence for “cascading effects” (e.g., a host of cognitive, affective, attitudinal and behavioral effects of identity threat) as suggested by Major and O’Brien (2005), a finding consistent with research on identity threat among overweight participants (Major et al., 2014). Of course, the observed effects are just as important; we found that smokers, in response to identity threatening experiences, feel stressed and rejection sensitive as well as increase their interest in quitting.
Although the identity threat model of stigma does not specify the direction of outcomes as a result of identity threat, the literature on stigma suggests that identity threat results in poorer mental and physical health outcomes (Major & O’Brien, 2005). In fact, Helweg-Larsen et al. (2019) found that stigmatizing smokers led them towards cognitive and attitudinal reactions that indicated less interest in quitting, whereas the current results show that stigmatizing smokers led them to have reactions that indicate greater interest in quitting. This suggests that the exact task or information by which stigma-reminder is presented clearly matters. In the current study, the tasks involved reading a newspaper article describing the stigma that smokers experience (Experiment 1) or asking participants to recall their own stigmatizing experiences (Experiment 2), whereas in Helweg-Larsen et al. (2019) the task outed participants as smokers in an evaluation-rich situation (a mock job interview). Revealing a stigmatized identity in a context where most smokers wish to conceal it (e.g., a job interview) is clearly different than thinking about one’s own or other smokers’ experience with mistreatment. Research has shown that individuals with stigmatizing identities can cope with discrimination by concealing their identity and some, like those who have high rejection sensitivity, specially benefit from concealing their stigmatized identity (Quinn, 2018). Therefore, a context in which a concealed stigmatized identity is made visible might cause smokers to become less interested in quitting as a result of the anticipation of stigma, whereas a context in which individuals are reminded of the various stigmatizing experiences of smokers might be stressful, but will lead to interest leaving the devalued group (e.g., in quitting).
According to the identity threat model of stigma, cultural context determines reactions to stigma, thus, we examined smokers from a smoking lenient (Denmark) and smoking prohibitive (U.S.) countries. We found that consistent with prior research (Helweg-Larsen, 2014; Helweg-Larsen et al., 2019) overall Americans were more stressed, had greater rejection sensitivity, perceived greater risks of smoking, and held fewer positive cognitions about smoking than Danes. This cultural context likely contributed to Americans but not Danes becoming more rejection sensitive in the stigma manipulation condition compared to the control condition. However, Americans and Danes did not differ in their intentions to quit. Future studies should examine the role of other cultural contexts that differ in smoking leniency to examine the effects of smoking stigma.
Our study also brings new insights to an important variable—rejection sensitivity. For the current study, we developed a new scale of rejection sensitivity which correlated with stress, smoking cessation intentions, interest in cessation tools, threat, and risk (see Tables 1 and 2) and changed in response to both experimental manipulations. Past research has associated rejection sensitivity with psychological distress, poorer physical well-being, and increased illness symptoms (Brenchley & Quinn, 2016), and has suggested that it could be a key contributor to the negative effects of weight-based identity threat (Blodorn et al., 2016). Therefore, we suggest that rejection sensitivity warrants further examination in the domain of smoking stigma. Future research should also examine other personal characteristics such as internalized smoking stigma (Brown-Johnson et al., 2015) and shame (Kim, Cao, & Meczkowski, 2018).
In these studies, our experimental approach is valuable because it can help us identify a causal relationship and provide a controlled investigation of the effects of brief stigmatizing situations or contexts. But this approach is also a limitation because it cannot capture the accumulated effects of chronic exposure to stigma (how stigma gets “under the skin”; Chaudoir, Earnshaw, & Andel, 2013). Another limitation is that we used heavy smokers who probably have been exposed to stigma for a long time and have had time to adjust to it. Research shows that people who have longer exposure to stigma are better protected against its detrimental effects (Corrigan & Watson, 2006). Thus, inferences made from the two studies, may not generalize to smokers with less stigma exposure.
In conclusion, the findings from our study suggest that if used in the right context, stigma might be an effective tool in moving smokers toward leaving their stigmatized group (e.g., quitting smoking) rather than away from it. We do not conclude that smoking stigma (in general) is helpful to smokers, but we instead conclude that smoking stigma (in certain situations, as in our manipulation) might be helpful for smokers. By bringing attention to the context in which smoking stigma is presented or experienced, our study highlights the importance of future research to examine smoking stigma in a wide range of settings to understand the nuances of when it can be helpful for smoking cessation efforts. Public health professionals should also consider the ethics of creating more stigma overall even if it reduces smoking prevalence (Bayer, 2008; Riley, Ulrich, Hamann, & Ostroff, 2017). Smoking stigma might also create even more socioeconomic disparity as smokers with greater resources quit successfully and the remaining smokers are further marginalized and devalued (e.g., Graham, 2012). Understanding contexts of stigma will be crucial in enhancing the effectiveness of anti-smoking messages and ultimately decreasing smoking prevalence.
Supplementary Material
Acknowledgements:
We would like to thank Lia Sorgen and Sarah DiMuccio for their comments on an earlier draft of this manuscript, Study Abroad in Scandinavia https://disabroad.org/) for providing research facilities and logistical support in Copenhagen, Bridgette Rodgers for help with data management, and the following students who collected data: Meg Booth, Sophie Coates, Sam Gerhard, Bella Valeur, and Safia Sheikh. Materials are available at Open Science Framework: https://osf.io/bn7s8/.
Funding: The work was supported by the National Cancer Institute at the National Institutes of Health (R15-CA194937). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Footnotes
Declaration of Interests: The authors declare no competing interests.
References
- Arndt J, Vail KE, Cox CR, Goldenberg JL, Piasecki TM, & Gibbons FX (2013). The interactive effect of mortality reminders and tobacco craving on smoking topography. Health Psychology, 32, 525–532. doi: 10.1037/a0029201 [DOI] [PubMed] [Google Scholar]
- Aung AT, Pickworth WB, & Moolchan ET (2004). History of marijuana use and tobacco smoking topography in tobacco-dependent adolescents. Addictive Behaviors, 29, 699–706. 10.1016/j.addbeh.2004.02.012 [DOI] [PubMed] [Google Scholar]
- Baha M, & Le Faou A (2010). Smokers’ reasons for quitting in an anti-smoking social context. Public Health, 124, 225–231. doi: 10.1016/j.puhe.2010.02.011 [DOI] [PubMed] [Google Scholar]
- Bayer R (2008). Stigma and the ethics of public health: Not can we but should we. Social Science & Medicine, 67, 463–472. 10.1016/j.socscimed.2008.03.017 [DOI] [PubMed] [Google Scholar]
- Berjot S, Girault-Lidvan N, & Gillet N (2012). Appraising stigmatization and discrimination: Construction and validation of a questionnaire assessing threat and challenge appraisals to personal and social identity. Identity: An International Journal of Theory and Research, 12, 191–216. 10.1080/15283488.2012.691254 [DOI] [Google Scholar]
- Blodorn A, Major B, Hunger J, & Miller C (2016). Unpacking the psychological weight of weight stigma: A rejection-expectation pathway. Journal of Experimental Social Psychology, 63, 69–76. https://doi.org/10.1016%2Fj.jesp.2015.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt AM (2007). The cigarette century: The rise, fall and deadly persistence of the product that defined America. New York: Basic Books. [Google Scholar]
- Brenchley KJM & Quinn DM (2016). Weight-based rejection sensitivity: Scale development and implications for well-being. Body Image, 16, 79–92. 10.1016/j.bodyim.2015.11.005 [DOI] [PubMed] [Google Scholar]
- Brown-Johnson C, Cataldo J, Orozco N, Lisha N, Hickman N, & Prochaska J (2015). Validity and reliability of the internalized stigma of smoking inventory: An exploration of shame, isolation, and discrimination in smokers with mental health diagnoses. The American Journal on Addictions, 24, 410–418. doi: 10.1111/ajad.12215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2018). Current Cigarette Smoking Among Adults—United States, 2017. Morbidity and Mortality Weekly Report, 67, 1225–32, Retrieved from: https://www.cdc.gov/mmwr/volumes/67/wr/mm6744a2.htm?s_cid=mm6744a2_w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudoir S, Earnshaw V, & Andel S (2013). “Discredited” versus “discreditable”: Understanding how shared and unique stigma mechanisms affect psychological and physical health disparities. Basic & Applied Social Psychology, 35, 75–87. https://envoy.dickinson.edu:6084/10.1080/01973533.2012.746612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corrigan P, & Watson A (2006). The paradox of self-stigma and mental illness. Clinical Psychology: Science and Practice, 9, 35 53. 10.1093/clipsy.9.1.35 [DOI] [Google Scholar]
- Cortland C, Shapiro J, Guzman I, & Ray L (2019). The ironic effects of stigmatizing smoking: combining stereotype threat theory with behavioral pharmacology. Addiction. 10.1111/add.14696 [DOI] [PubMed] [Google Scholar]
- De Jesus S, Hsin A, Faulkner G, & Prapavessis H (2013). A systematic review of analysis of data reduction techniques for the CReSS smoking topography device. Journal of Smoking Cessation, 10, 12–26. doi: 10.1017/jsc.2013.31 [DOI] [Google Scholar]
- Evans-Polce R, Castaldelli-Maia J, Schomerus G, & Evans-Lacko S (2015). The downside of tobacco control? Smoking and self-stigma: A systematic review. Social Science & Medicine, 145, 26–34. 10.1016/j.socscimed.2015.09.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39, 175–191. doi: 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Fotuhi O, Fong G, Zanna M, Borland R, Yong H, & Cummings K (2013). Patterns of cognitive dissonance-reducing beliefs among smokers: A longitudinal analysis from the International Tobacco Control (ITC) Four Country Survey. Tobacco Control, 22, 52–58. 10.1136/tobaccocontrol-2011-050139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fucito LM, & Juliano LM (2009). Depression moderates smoking behavior in response to a sad mood induction. Psychology of Addictive Behaviors, 23, 546–551. doi: 10.1037/a0016529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glock S, & Kneer J (2009). Are deterrent pictures effective? The impact of warning labels on cognitive dissonance in smokers. Applied Psychology: Health & Well-Being, 1, 356–373. doi: 10.1111/j.17580854.2009.01019.x [DOI] [Google Scholar]
- Graham H (2012). Smoking, stigma and social class. Journal of Social Policy, 41, 83–99. doi: 10.1017/S004727941100033X [DOI] [Google Scholar]
- Hammond D, Fong GT, Zanna MP, Thrasher JF, & Borland R (2006). Tobacco denormalization and industry beliefs among smokers from four countries. American Journal of Preventive Medicine, 31, 225–232. 10.1016/j.amepre.2006.04.004 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2018). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach, 2nd Edition. New York, NY: Guilford Publications [Google Scholar]
- Helweg-Larsen M, & Nielsen GA (2009). Smoking cross-culturally: Risk perceptions among young adults in Denmark and the United States. Psychology & Health, 24, 81–93. 10.1080/08870440801932656 [DOI] [PubMed] [Google Scholar]
- Helweg-Larsen M, Tobias MR, & Cerban BM (2010). Risk perception and moralization among smokers in the USA and Denmark: A qualitative approach. British Journal of Health Psychology, 15, 871–886. 10.1348/135910710X490415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helweg-Larsen M (2014). Does moralization motivate smokers to quit?: A longitudinal study of representative samples of smokers in the U.S. and Denmark. Nicotine & Tobacco Research, 10, 1379–1386. 10.1093/ntr/ntu091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helweg-Larsen M, Sorgen LJ, & Pisinger C (2019). Does it help smokers if we stigmatize them?: A test of the stigma-induced identity threat model among U.S. and Danish smokers. Social Cognition, 3, 294–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstede G (2001). Culture’s consequences (2nd Ed). Thousand Oaks, CA: Sage Publications. 10.1016/S0022-1031(03)00039-8 [DOI] [Google Scholar]
- Inzlicht M, & Kang SK (2010). Stereotype threat spillover: How coping with threats to social identity affects aggression, eating, decision making, and attention. Journal of Personality and Social Psychology, 99, 467–481. 10.1037/a0018951 [DOI] [PubMed] [Google Scholar]
- Inzlicht M, McKay L, & Aronson J (2006). Stigma as ego depletion: How being the target of prejudice affects self-control. Psychological Science, 17, 262–269. 10.1111/j.1467-9280.2006.01695.x [DOI] [PubMed] [Google Scholar]
- Joossens L, & Raw M (2017). The Tobacco Control Scale 2016 in Europe. Association of European Cancer Leagues. Retrieved from https://www.cancer.be/sites/default/files/tobacco_control_scale.pdf [Google Scholar]
- Kim J, Cao X, & Meczkowski E (2018). Does stigmatization motivate people to quit smoking? Examining the effect of stigmatizing anti-smoking campaigns on cessation intention. Health Communication, 33, 681–689. 10.1080/10410236.2017.1299275 [DOI] [PubMed] [Google Scholar]
- Landau MJ, Cameron LD, Arndt J, Hamilton WK, Swanson TJ, & Bultmann M (2019.). Beneath the surface: Abstract construal mindset receptivity to metaphors in health communications. Social Cognition, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E, Malson J, Moolchan E, Waters AJ, & Pickworth WB (2003). Smoking topography: Reliability and validity in dependent smokers. Nicotine & Tobacco Research, 5, 673–679. doi: 10.1080/1462220031000158645 [DOI] [PubMed] [Google Scholar]
- MacLeod CM (1991). Half a century of research on the Stroop effect: An integrative review. Psychological Bulletin, 109, 163–203. [DOI] [PubMed] [Google Scholar]
- Major B, & O’Brien LT (2005). The social psychology of stigma. Annual Review of Psychology. 56, 393–421. 10.1146/annurev.psych.56.091103.070137 [DOI] [PubMed] [Google Scholar]
- Major B, Eliezer D, & Rieck H (2012). The psychological weight of weight stigma. Social Psychological and Personality Science, 3, 651–658 10.1177/1948550611434400 [DOI] [Google Scholar]
- Major B, Hunger JM, Bunyan DP, & Miller CT (2014). The ironic effects of weight stigma. Journal of Experimental Social Psychology, 51, 74–80. 10.1016/j.jesp.2013.11.009 [DOI] [Google Scholar]
- McClernon FJ, Beckham JC, Mozley SL, Feldman ME, Vrana SR, & Rose JE (2005). The effects of trauma recall on smoking topography in posttraumatic stress disorder and non-posttraumatic stress disorder trauma survivors. Addictive Behaviors, 30, 247–257. doi: 10.1016/j.addbeh.2004.05.013 [DOI] [PubMed] [Google Scholar]
- McKee S, Sinha R, Weinberger A, Sofuoglu M, Harrison E, Lavery M, & Wanzer J (2010). Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. Journal of Psychopharmacology, 25, 490–502. 10.1177/0269881110376694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Profile (2017). Danskernes sundhed – Tal fra den nationale sundhedsprofil [The health of Danes – The national health profile]. Retrieved May 3, 2019 from http://danskernessundhed.dk/
- Oakes W, Chapman S, Borland R, Balmford J, & Trotter L (2004). ‘Bulletproof skeptics in life’s jungle’: Which self-exempting beliefs about smoking most predict lack of progression towards quitting? Preventive Medicine: An International Journal Devoted to Practice and Theory, 39, 776–782. 10.1016/j.ypmed.2004.03.001 [DOI] [PubMed] [Google Scholar]
- Perkins KA, Karelitz JL, Giedgowd GE, & Conklin CA (2012). The reliability of puff topography and subjective responses during ad lib smoking of a single cigarette. Nicotine & Tobacco Research, 14, 490–494. doi: 10.1093/ntr/ntr150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn DM (2018). When stigma is concealable: The costs and benefits for health. In Major B, Dovidio JF, & Link BG (Eds.), The Oxford handbook of stigma, discrimination, and health. (pp. 287–299). New York, NY: Oxford University Press. Retrieved from https://search.ebscohost.com/login.aspx?direct=true&db=psyh&AN=2017-57025-015&site=eds-live&scope=site [Google Scholar]
- Riley KE, Ulrich MR, Hamann HA, & Ostroff JS (2017). Decreasing Smoking but Increasing Stigma? Anti-tobacco Campaigns, Public Health, and Cancer Care. AMA Journal of Ethics, 19, 475–485. 10.1001/journalofethics.2017.19.5.msoc1-1705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahab L, Hammond D, O’Connor RJ, Cummings MK, Borland R, King B, & McNeill A (2008). The reliability and validity of self-reported puffing behavior: Evidence from a cross-national study. Nicotine & Tobacco Research, 10, 867–874 doi: 10.1080/14622200802027156 [DOI] [PubMed] [Google Scholar]
- Shadel WG, & Cervone D (2011). The role of the self in smoking initiation and smoking cessation: A review and blueprint for research at the intersection of social-cognition and health. Self and Identity, 10, 386–395. 10.1080/15298868.2011.557922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shadel WG, & Mermelstein R (1996). Individual differences in self-concept among smokers attempting to quit: Validation and predictive utility of measures of the smoker self-concept and abstainer self-concept. Annals of Behavioral Medicine, 18, 151–156. 10.1007/BF02883391 [DOI] [PubMed] [Google Scholar]
- Süssenbach P, Niemeier S, & Glock S (2013). Effects of and attention to graphic warning labels on cigarette packages. Psychology & Health, 28, 1192–1206. 10.1080/08870446.2013.799161 [DOI] [PubMed] [Google Scholar]
- Tombor I, Shahab L, Brown J, & West R (2013). Positive smoker identity as a barrier to quitting smoking: Findings from a national survey of smokers in England. Drug and Alcohol Dependence, 133, 740–745. 10.1016/j.drugalcdep.2013.09.001 [DOI] [PubMed] [Google Scholar]
- Unger J, Cruz T, Shakib S, Mock J, Shields A, Baezconde-Garbanati L, & ... Johnson C (2003). Exploring the cultural context of tobacco use: A transdisciplinary framework. Nicotine & Tobacco Research, 5 Suppl 1, S101–S117. 10.1080/14622200310001625546 [DOI] [PubMed] [Google Scholar]
- Velicer WF, Diclemente CC, Rossi JS, & Prochaska JO (1990). Relapse situations and self-efficacy: An integrative model. Addictive Behaviors, 15, 271–283. 10.1016/0306-4603(90)90070-e [DOI] [PubMed] [Google Scholar]
- Weinstein ND, Kwitel A, McCaul KD, Magnan RE, Gerrard M, & Gibbons FX (2007). Risk perceptions: Assessment and relationship to influenza vaccination. Health Psychology, 26, 146–151. 10.1037/0278-6133.26.2.146 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.