Abstract
Dental practitioners confront the highest risk of COVID-19 infection due to constant exposure to saliva, droplets, blood, and aerosols. Despite the suspension of routine dental care in many countries around the world, dental professionals perceive a moral duty to take part in the global fight against the pandemic. Therefore, dental professionals should be vigilant in defending against the transmission of the virus and as well as in the diagnosis of the disease through the oral manifestations of it. We conducted a literature review on publicly available data to outline updates on guidelines and studies of dental settings during the COVID-19 era. In this literature review, the categorization of the patients for dental treatments, protective precautions for the dental practice, considerations for dental drug prescription, and oral manifestations of the disease has been reviewed.
Keywords: Coronavirus, COVID-19, SARS-CoV-2, dentistry, pandemic
Introduction
In December 2019, Wuhan Health Commission of Hubei province of the Republic of China reported an array of 27 patients with pneumonia of obscure etiology, presenting with a constellation of symptoms such as fever, nonproductive cough, dyspnea, and bilateral ground-glass opacities with patchy shadows in computed tomography of the lungs. The patients were epidemiologically traced back into Huanan Seafood Wholesale Market, trading live species of bats, pangolins, snakes, and badgers which bolstered the hypothesis that a live animal had been the intermediary of transmitting a pathogen to the patients.[1,2] The bronchoalveolar lavage fluid of three Wuhan patients, revealed Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) as the causal factor of the disease.[3] The violent and rapid propagation of the virus through unknown mechanisms and due to population density and proximity of the live animal marketplaces made Wuhan the provenance of the animal-human interface and led to a critical juncture at which the World Health Organization declared the pandemic of coronavirus disease 2019 (COVID-19) on February 2020.[4]
The CoVs family is a class of enveloped positive-sense, single-stranded RNA viruses that are genotypically and serologically divided into four subfamilies of α, β, γ, and δ-CoVs among which α- and β-CoVs are responsible for human infections, causing respiratory, hepatic, enteric, and neurologic diseases.[5] SARS-CoV-2 as a β-CoV is evolved into two major types of L and S. It has been suggested that the S type depicts a more aggressive behavior and quicker spread whereas the L type is considered to have a relatively milder nature.[3] Human angiotensin-converting enzyme2 (ACE2) is the main host receptor of COVID-19 infection which is broadly expressed in the oral and nasal mucosa, esophagus, bronchus, lung, heart, kidney, intestinal cells, bladder, activated leukocytes, and testicular tissues, resulting in the vulnerability to multiple organ damage.[6] Among the myriad of organ involvements of COVID-19 infection, the mucosal epithelium of the upper respiratory tract is the primary site of viral replication which may proceed in the lower respiratory tract and gastrointestinal mucosa that can either lead to a mild, asymptomatic viremia or a cytokine storm initiated by the downregulation of ACE2. The latter precipitates the Acute Respiratory Distress Syndrome (ARDS) that stands out as the preeminent cause of death among COVID-19 patients.[5]
The rapid and disruptive diffusion of COVID-19 is probably associated with the easy transmission routes of the virus through respiratory droplets and contact transmission. Although primary concern has aimed attention to near-field transmissions such as hand-to-face transport from contaminated surfaces or person-to-person transmission through coughing/sneezing, recent studies are suggestive of other possible transmission routes such as aerosols, fecal-oral, and vertical transmission from mother to baby.[7,8]
In terms of the exposure risk for various working categories, dental practitioners confront the highest risk of COVID-19 infection due to constant exposure to saliva, droplets, blood, and aerosols. Therefore, inhalation of infected droplets/aerosols and direct contact with contaminated instruments or surfaces puts both dental practitioners and patients at stake.[8] Moreover, all the patients seeking dental care in the era of COVID-19 pandemic should nevertheless be considered infected regardless of the nonappearance of common clinical manifestations of the disease. The majority of the COVID-19 infected patients are either asymptomatic or represent with self-limiting, mild to medium symptoms who can be easily misinterpreted as healthy individuals.[9] Dental practitioners can also play a pivotal role in careful assessment of the patients in terms of their health status through which high-risk patients can be detected and a contagion-reduced treatment can be implemented for patients with unknown risk in emergency conditions.[8]
Concerning the aforementioned evidence, the contributory role of dentistry in the detection and assessment of initial symptoms of COVID-19 infection and providing emergency patients with a contagion-reduced environment is indisputable in the era of this pandemic outbreak. In this article, we aimed to review the challenges and perspectives of dentistry and oral and maxillofacial surgery in the upheaval of COVID-19 in terms of patient categorization for dental treatments, protective precautions in dental practice for maximal transmission control of the virus, dental drug prescription considerations, and oral manifestations of COVID-19 infection.
Materials and Methods
The information available from the literature and the clinical management of dental patients in the era of the COVID-19 pandemic was searched for in PubMed and Google Scholar. A literature search was performed to retrieve research articles with the content of COVID-19 and dentistry, and maxillofacial surgery. No attempt to exclude any information was made, to obtain all the possible articles. Therefore, no strict inclusion and exclusion criteria were applied. High quality and relevant articles were classified into 4 categories based on their content for answering the following questions:
How should the dental patients be categorized for receiving dental treatments?
What protective precautions should be considered for dental practice during the COVID-19 outbreak?
What are the dental aspects of the drugs that are used for COVID-19 pandemic control?
What are the oral manifestations of COVID-19 infection?
Results
Categorization of the patients and case selection for dental treatments
Utilization of dental services experienced a 38% decline at the beginning of the COVID-19 outburst where the proportion of dental and oral infections increased from 51.0% to 71.9% during this era. In the meantime, the number of non-emergency patients was decreased by 70% as declared by Geu et al.[10]. Long and Corsar[11] also acknowledged a 57% decrease in daily attendances for dental abscesses while the proportion of admission-requiring abscesses increased notably from 35% to 80% which reflects the essential impress of urgent dental care during the pandemic.
Alharbi et al.[12] proposed a guideline through which dental health professionals would be able to categorize the patients to five divided groups after the meticulous screening of them in terms of COVID-19 infection: A (asymptomatic, unsuspected, unconfirmed), B (symptomatic/suspected, unconfirmed), C (stable, confirmed: mild infection with no hospitalization/oxygen therapy), D (unstable, confirmed: sever and critical cases), and E (recovered, confirmed: asymptomatic for at least 30 days after the last negative laboratory test). The authors have also classified the various dental treatments to five classes for easier decision making of the dentists by allocating each patient category to specific classes of dental treatment that can be implemented for the patients which is depicted in Table 1. According to this guideline COVID-19 infection status together with the urgency of a dental treatment leads to rationale decision making for the treatment of the patients under the premise of adequate protection measures. Although the authors suggested that full dental treatment can be implemented for recovered COVID-19 patients, Chen et al.[13] reported a case of SARS-CoV-2 reoccurrence in convalescence accentuating the active surveillance of the virus for infectivity assessment. Similarly, Loconsole et al.[14] reported the reactivation of COVID-19 in a patient after more than 30 days of the test negativity and emphasized on the fluctuant presence of the virus and possible occurrence of the false-negative results. A brief guide for interpretation of the COVID-19 viral and antibody tests is illustrated in Figure 1.
Table 1.
Categorization of dental patients and decision making for their treatment
| Dental treatment categories | Respective dental treatments | Patient groups that the treatment can be done for |
|---|---|---|
| A | Unstable maxillofacial fractures compromising the patient’s airway | All patient groups |
| Emergency | Diffuse soft tissue bacterial infection with intra/extra oral swelling compromising the patient’s airway | |
| Uncontrolled postoperative bleeding | ||
| B | Severe dental pain caused by pulpal inflammation requiring dental extraction. | A, C, and E |
| Urgent conditions capable of being managed with minimally invasive procedures, without aerosol generation | Severe dental pain from fractured vital teeth that can be managed. | |
| Dental trauma with avulsion/luxation | ||
| Surgical postoperative oseitis (dry socket) | ||
| Pericoronitis/third molar pain | ||
| Stable maxillofacial fractures requiring no intervention | ||
| Localized dental/periodontal abscesses | ||
| Defective fixed orthodontic appliances causing soft tissue laceration | ||
| C | Severe dental pain from pulpal inflammation and fractured vital tooth that needs to be managed by aerosol-generating procedures | A and E |
| Urgent conditions requiring management with invasive and/or aerosol generation | Dental trauma (avulsion/luxation) requiring aerosol-generating procedures | |
| Deboned fixed prosthesis cleaning and temporary cementation | ||
| Removable denture adjustment for oncology/radiation patients | ||
| Defective prosthesis causing soft tissue damage | ||
| Acute periodontal diseases | ||
| D | Repair/adjustment of removable dentures | - |
| Non-urgent | Asymptomatic fractured/defective restorations, fixed prosthesis, and orthodontic appliances | |
| Chronic periodontal diseases | ||
| E elective | Periodic dental and oral examinations and recall visits | - |
| Aesthetic dental procedures | ||
| Restoration/extraction of asymptomatic teeth | ||
| Routine dental cleaning | ||
| Preventive therapies | ||
| Replacement of missing teeth with fixed or removable prosthesis | ||
| Dental implant surgery | ||
| Other orthodontic procedures |
Figure 1.
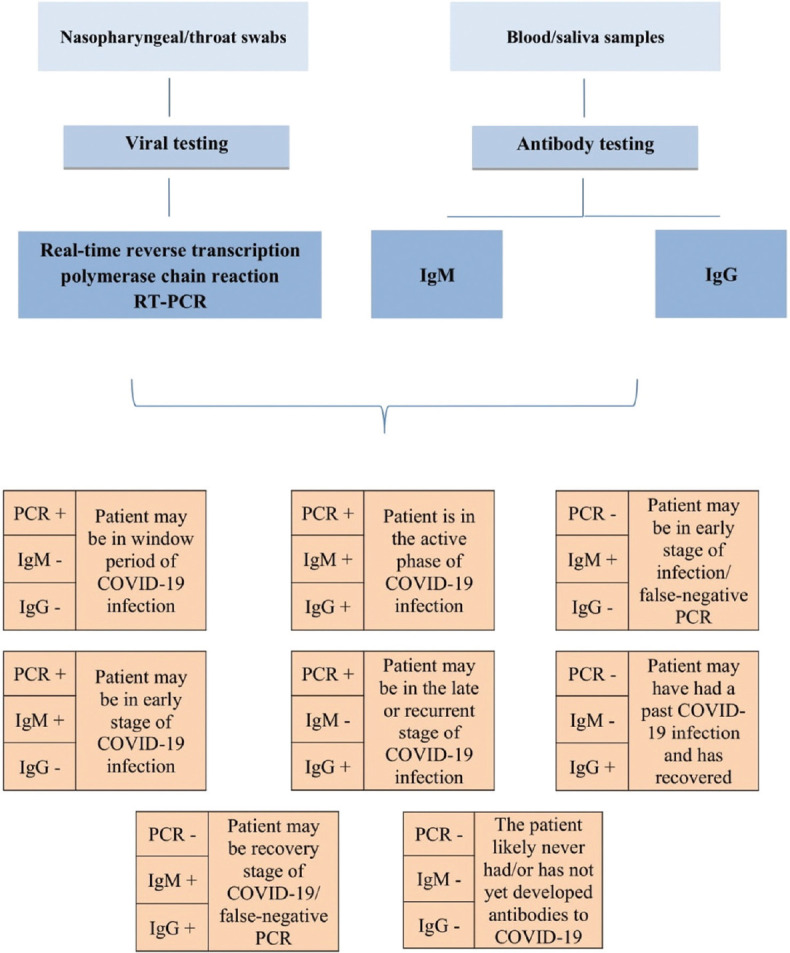
Interpretation of COVID-19 viral and antibody test results[15,16]
Protective precautions in the dental setting
Patient screening
Dental practitioners are advised to utilize telephonic pretriage for initial assessment of the patients by asking 3 pertinent questions including any recent travel history to any areas with a high incidence of COVID-19, any exposures to a person with suspected/known COVID-19 infection, and presence of any symptoms of the disease.[17] The positive response of the patients to any of the questions should be followed by deferring the dental appointment for up to 2 weeks and thus self-quarantining at home as suggested by Meng et al.[18] Therewith, body temperature and the presence of suspect symptoms should be assessed and registered at the dental office appointment.[19]
Waiting area
Parhizkar et al.[20] suggested a minimum of 6 feet distance between patients from one another/dental personnel in a sufficiently ventilated waiting room and emphasized on providing the patients with surgical face mask and hand sanitizer. GE et al.[21] suggested instructing the patients to cover their nose and mouth with a tissue or their elbows when sneezing or coughing followed by immediate disposing of the tissue and hand disinfection. However, they supposed that the 1-meter spatial distancing of the patients is adequate.
Hand hygiene
Hand washing plays a pivotal role in COVID-19 prevention.[18] As suggested by Peng et al.,[22] thorough hand washing is crucial when coming into contact with patients, surfaces, and equipment and touching nose, mouth, and eyes with contaminated hands has been restrictedly avoided. Soap and alcohol-based hand rubs (ABHR) are equally effective cleansers. However, handwashing with soap and water is capable of eliminating dirt, body fluids, blood, and any other visible hand contamination whereas ABHRs are appropriate sanitizers for hands that are not visibly soil.[21]
Pre-procedural mouth rinse
Despite the efficacy of chlorhexidine in the reduction of colony-forming units in dental aerosol, its effectiveness in eliminating COVID-19 is a matter of conjecture.[21,23] Farzan and Firoozi[24] stated that Povidone-iodine (PVP-I) gargle/mouthwash is the only promising and approved substance for eliminating coronaviruses. In a recent study, Kirk-Bayley et al.[25] advocated the application of PVP-I nasal sprays together with povidone-iodine mouthwash for minimizing COVID-19 transmission through virus expectoration in the form of aerosols.
3.2.5 Personal protective equipment (PPE)
Concerning the transmission of the virus through airborne droplets in the dental setting, utilization of protective equipment such as gloves, facial masks, long-sleeved water-resistant gowns, shoe cover, eyewear and face shields is of utmost importance in the era of COVID-19.[8]
Although surgical masks protect mucous membranes of the nose and mouth for droplet spatter, they do not ensure full protection against inhalation of airborne transmissive agents as declared by the Centers for Disease Control and Prevention (CDC). Yet, the patients should be asked to re-don their face covering with a surgical mask after the dental treatment completion when they leave the treatment area as well as when they enter the dental office.[26] Working in close contact with patients necessitates utilizing particulate respirators such as filtering face piece (FFP) level 2/3 or N95.[8] Utilization of the protective safety glasses and face shields is mandatory when performing an aerosol-generating procedure as COVID-19 is capable of transmitting through human conjunctival epithelium.[27]
Contaminated air filtering
Two types of commonly used devices can be utilized for filtering the contaminated air within the dental office area: high-volume evacuator (HVE) and high-efficacy particulate arrestor (HEPA). HVE is a rather inexpensive device, capable of reducing the contamination of the operating site by 90% at 2.83 m3 per minute. However, this device should be held at a specific distance from the aerosol-generating instrument (6–15 mm) for proper operation. On the other hand, HEPA is an expensive air filtration device that can remove 99.97% of 0.3 μm particles.[21] Recent guidelines suggested by the CDC proposed the utilization of portable HEPA air filtration units during aerosol-generating procedures.[26] With 6 air changes per hour (ACH), a time gap of 46 minutes is required between patients for 99.9% removal of airborne contaminants by efficacy. As the 6–15 ACH has been frequently cited for patient-care areas, a range of 18–46 minutes of time gap is demanded between patient's appointments.[28]
Surface disinfection
Although coronaviruses are proven to persist on inanimate surfaces for up to 9 days, they are noticeably vulnerable to surface disinfectants containing 62–71% ethanol, 0.5% hydrogen peroxide, and 0.1% (0.1 g/L) sodium hypochlorite within 1 minute.[29]
The protective precautions for COVID-19 infection control in the dental setting are presented in Table 2.
Table 2.
Protective precautions in dental practice for control of COVID-19 transmission
| Patient screening | Telephonic pretriage: 1. History of recent travel to high COVID-19 incidence areas 2. Exposure to known/suspected COVID-19 infected person 3. Presence of COVID-19 infection symptoms |
| Triage in dental office: all of the questions of the tele-screening should be asked together with body temperature registration preferably with a contact-free forehead thermometer. | |
| Waiting area | The waiting room should be sufficiently ventilated with natural ventilation, 60 L/s per patient |
| Patients must be provided with facial masks and sanitizing gel before entry to the dental office. Mask wearing should be obligatory for the patients, anyone accompanying them, and the personnel. | |
| Cough instruction etiquette should be posted at the entrance of the waiting room. | |
| Patients should keep a distance of 1-2 meters from each other/personnel. | |
| Magazines, toys, and any other object that can not be disinfected should be removed from waiting areas. | |
| Overlapping appointments and the number of waiting patients should be minimized in the waiting area. | |
| Hand hygiene | Soap: if the hands are visibly soiled with dirt, blood, or body fluids |
| 70-90% alcohol-based hand rubs (ABHRs): if the hands are not visibly soiled | |
| 5 hand washings protocol for at least 1 minute: before touching a patient or performing aseptic procedures and after touching a patient, exposure to body fluid, and touching a patient’s surroundings (2 before and 3 after). | |
| Pre-procedural mouth rinse | 1 min mouth rinse with 0.2-1.0% Povidone-iodine (PVP-I) or 1% hydrogen peroxide mouthwash/gargle (application of povidone-iodine nasal spray is also suggested for maximal prevention of COVID-19 for both patients and healthcare workers) |
| Personal protective equipment (PPE) | Face masks: |
| Surgical mask: should be provided and obligatory for all the patients, visitors, and personnel. Patients should be asked to re-don face covering after the completion of the dental treatment. | |
| N95 respirator: should be donned when performing an aerosol-generating procedure (using high-speed handpiece, air-water syringe, and ultrasonic scaler) | |
| European Standard Filtering Face Piece 2 (EU FFP2): same indications as N95 respirator | |
| EU FFP3 respirator: should be donned when performing emergency dental treatment for COVID-19 suspected patients. | |
| Face shields & protective eyewear: | |
| Eye protection should be guaranteed with the use of protective safety eyewear and face shields. | |
| The eye protection should be removed by grabbing the strap and pulling upwards and away from the head. The front of the eye protection should never be touched. | |
| Removal/filter of contaminated air | Utilization of a portable high-efficacy particulate arrestor (HEPA) air filtration should be considered. |
| Careful checking of the HEPA filters should be considered as they can become the source for re-entering of the microbes to the air. | |
| Based on the air changes per hour (ACH), an average time gap of 18-46 minutes is needed between patient’s appointments. | |
| Surface disinfection | Disinfection of the dental operatory should be initiated 15 minutes after completion of the treatment. |
| Surfaces should be thoroughly wiped out after each dental appointment with surface disinfectants containing 62-71% ethanol, 0.5% hydrogen peroxide, and 0.1% (0.1 g/L) sodium hypochlorite with particular attention to the operating area and door handles for at least 1 min | |
| The utilization of sanitizing tunnels has not been recommended due to unknown efficacy and risk of skin, eye, or respiratory irritation caused by its chemicals. | |
| Utilization of pesticidal devices such as high-intensity UV radiation, LED blue light, and ultrasonic devices as surface disinfection alternatives are not confirmed in terms of efficacy, safety, or circumstances of usage. | |
| Protective safety glasses, face shields, blood pressure cuffs, and thermometers should be disinfected with 70% ethyl alcohol after each use |
Considerations of drug prescription in dentistry practice
Analgesics
As the outburst of COVID-19 resulted in the limitation of dental practice to emergency treatments, patients with dental pain were compelled to rely on supportive therapy by analgesics and non-steroidal anti-inflammatory drugs (NSAIDs) administration for the alleviation of their pain. On the other hand, the mainstay treatment of mild-moderate COVID-19 patients is the analgesic supportive, antipyretic therapy which has to do with the administration of analgesics such as ibuprofen.[30] However, the exacerbation of the symptoms of COVID-19 patients followed by ibuprofen administration cast attention on the possible unfavorable effects of the drug.[31] Theoretically, the capability of ibuprofen in increasing the ACE2 bioavailability and interference with the immune system supported the enhancement of COVID-19 infection.[30,32] Although no strong epidemiological evidence supported this pharmacological theory, dentists should keep a watchful eye on updates. Therefore, prescription of paracetamol or acetaminophen as the first-line drugs for dental pain relief is suggested as a cautious solution.[30,32]
Azithromycin
Azithromycin is the empiric medication for odontogenic infection in penicillin-allergic patients and is a favorable antibiotic for the management of respiratory infections in children.[30] Despite the efficacy of a combined regimen of azithromycin and hydroxychloroquine in a few reports, no strong evidence has supported the alleged efficacy and safety of this regimen. Considering the shift of dental services to emergency treatments and therefore a possible increase in antibiotic prescription, dentists should be vigilant in prescribing azithromycin especially in countries with a high toll of COVID-19 patients to decrease the risk of antibiotics resistance and side effects. Amoxicillin or clindamycin are appropriate alternatives for azithromycin in the era of COVID-19 pandemic.[30,32]
Chloroquine
Chloroquine attracted a lot of attention in the early outburst of COVID-19 with regard to its inhibitory effect on SARS-CoV-2 viral replication and its subsequent clinical efficacy. Chloroquines together with antiviral drugs such as remdesivir have demonstrated a remarkable efficacy and safety for the control of COVID-19 infection and therefore many countries have faced severe shortages of the drug. This is of paramount importance for the dentists to consider the influence of the drug shortage on chloroquine-dependent dental patients such as systematic lupus erythematosus (SLE) and Sjogren's syndrome patients with oral manifestations. Moreover, dentists should be acquainted with possible oral complications of chloroquine administration such as melanotic pigmentation and lichenoid reaction of the oral mucosa.[30]
Oral manifestations of COVID-19 infection
The presence of the COVID-19 genome in the saliva of the majority of the patients indicates potential infection of the salivary glands which makes saliva a dependable and comfortable alternative to naso/oropharyngeal for sampling.[33] Taste or/and olfactory disorders are common oral manifestations of COVID-19 as the virus penetrates taste buds of the tongue via ACE2 receptors. Therefore, dentists should be aware of any alterations in taste in forms of dysgeusia and burning mouth syndrome as they might be representative of respiratory diagnostic manifestation of COVID-19 infection.
Discussion
The role of dental practitioners in preventing the transmission of COVID-19 is pivotal. Despite the suspension of routine dental care in many countries around the world, dental professionals perceive a moral duty to take part in the global fight against the pandemic. Additionally, dentists can also contribute to the initial diagnosis of the disease as it may represent with oral manifestations. Many aspects of the dental profession such as financial and psychological dimensions are at stake. Therefore, dentists need to be vigilant in the updated data, guidelines, and protocols that are related to their profession.
Conclusions
In light of the protective precautions for the dental practice, dentists can perform safe dental treatment for the patients in the era of COVID-19 pandemic. Dentists should be able to categorize the patients based on their health status and treatment demands to make a moral and beneficial decision. Moreover, oral manifestations of COVID-19 turn dentists to frontiers in the diagnosis of the disease. As COVID-19 patients may represent asymptomatic or medically unexplained symptoms, a thorough screening of the patients in terms of specific or non-specific symptoms of infection and following protective precautions is of utmost importance in dental practice.
Author's contribution
Dr. F. R, Dr. M. Kh, and Dr. Gh. Sh contributed to the design and implementation of the research, and the writing of the manuscript. All authors have approved the final article.
Ethical approval
Not applicable
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak? J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. doi: 10.1016/j.jaut. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Pneumonia of unknown aetiology in Wuhan, China: Potential for international spread via commercial air travel? J Travel Med. 2020;27:taaa008. doi: 10.1093/jtm/taaa008. doi: 10.1093/jtm/taaa008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–74. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kakodkar P, Kaka N, Baig MN. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19) Cureus. 2020;12:e7560. doi: 10.7759/cureus.7560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, epidemiology, pathogenesis, and control of covid-19. Viruses. 2020;12:372. doi: 10.3390/v12040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Magrone T, Magrone M, Jirillo E. Focus on receptors for coronaviruses with special reference to angiotensin-converting enzyme 2 as a potential drug target-A perspective. Endocr Metab Immune Disord Drug Targets. 2020;20:807–11. doi: 10.2174/1871530320666200427112902. [DOI] [PubMed] [Google Scholar]
- 7.Anderson EL, Turnham P, Griffin JR, Clarke CC. Consideration of the aerosol transmission for COVID-19 and public health. Risk Anal. 2020;40:902–7. doi: 10.1111/risa.13500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Izzetti R, Nisi M, Gabriele M, Graziani F. COVID-19 transmission in dental practice: Brief review of preventive measures in Italy. J Dent Res. 2020;99:1030–38. doi: 10.1177/0022034520920580. [DOI] [PubMed] [Google Scholar]
- 9.Rothe C, Schunk M, Sothmann P, Bretzel G, Froeschl G, Wallrauch C, et al. Transmission of 2019-NCOV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–1. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guo H, Zhou Y, Liu X, Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 2020 doi: 10.1016/j.jds.2020.02.002. doi: 10.1016/j.jds.2020.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Long L, Corsar K. The COVID-19 effect: Number of patients presenting to The Mid Yorkshire Hospitals OMFS team with dental infections before and during The COVID-19 outbreak. Br J Oral Maxillofac Surg. 2020;58:713–4. doi: 10.1016/j.bjoms.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alharbi A, Alharbi S, Alqaidi S. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- research that is available on the COVID-19 resource centre-including this Guidelines for dental care provisi 2020 [Google Scholar]
- 13.Chen D, Xu W, Lei Z, Huang Z, Liu J, Gao Z, et al. Recurrence of positive SARS-CoV-2 RNA in COVID-19: A case report. Int J Infect Dis. 2020;93:297–9. doi: 10.1016/j.ijid.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Loconsole D, Passerini F, Palmieri VO, Centrone F, Sallustio A, Pugliese S, et al. Recurrence of COVID-19 after recovery: A case report from Italy? Infection. 2020:1–3. doi: 10.1007/s15010-020-01444-1. doi: 10.1007/s15010-020-01444-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Testing for COVID-19 | CDC n.d. [Last accessed on 2020 May 24]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html .
- 16.Xie J, Ding C, Li J, Wang Y, Guo H, Lu Z, et al. Characteristics of patients with coronavirus disease (COVID-19) confirmed using an IgM-IgG antibody test. J Med Virol. 2020 doi: 10.1002/jmv.25930. doi: 10.1002/jmv. 25930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ather A, Patel B, Ruparel NB, Diogenes A, Hargreaves KM. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. J Endod. 2020;46:584–95. doi: 10.1016/j.joen.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–7. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li ZY, Meng LY. [The prevention and control of a new coronavirus infection in department of stomatology] Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;55:E001. doi: 10.3760/cma.j.issn.1002-0098.2020.0001. [DOI] [PubMed] [Google Scholar]
- 20.Parhizkar A, Shamszadeh S, Mardani M, Asgary S. Dental considerations after the outbreak of 2019 novel coronavirus disease: A review of literature. Arch Clin Infect Dis. 2020 In Press. doi: 10.5812/archcid. 103257. [Google Scholar]
- 21.Ge Z, Yang L, Xia J, Fu X, Zhang Y. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B. 2020;21:361–8. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fallahi HR, Keyhan SO, Zandian D, Kim S, Cheshmi B. Being a front-line dentist during the Covid-19 pandemic: A literature review. Maxillofac Plast Reconstr Surg. 2020;42:12. doi: 10.1186/s40902-020-00256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farzan A, Firoozi Parsa. Common mouthwashes for pre-procedural rinsing in dental practice: Which one is appropriate for eliminating coronaviruses? A mini literature review. Regen Reconstr Restor. 2020;5:2. [Google Scholar]
- 25.Kirk-Bayley J, Challacombe S, Sunkaraneni V, Combes J. The use of povidone iodine nasal spray and mouthwash during the current COVID-19 pandemic may protect healthcare workers and reduce cross infection. SSRN Electron J. 2020 doi: 10.2139/ssrn. 3563092. [Google Scholar]
- 26.Guidance for Dental Settings | CDC n.d. [Last accessed on 2020 May 22]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dentalsettings.html .
- 27.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Air | Appendix | Environmental Guidelines | Guidelines Library | Infection Control | CDC n.d. [Last accessed on 2020 May 22]. Available from: https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html#tableb1 .
- 29.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–51. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Odeh ND, Babkair H, Abu-Hammad S, Borzangy S, Abu-Hammad A, Abu-Hammad O. COVID-19: Present and future challenges for dental practice. Int J Environ Res Public Heal. 2020;17:3151. doi: 10.3390/ijerph17093151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sodhi M, Etminan M. Safety of ibuprofen in patients with COVID-19: Causal or confounded.? Chest. 2020;158:55–6. doi: 10.1016/j.chest.2020.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baghizadeh Fini M. What dentists need to know about COVID-19? Oral Oncol. 2020;105:104741. doi: 10.1016/j.oraloncology.2020.104741. doi: 10.1016/j.oraloncology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vinayachandran D, Balasubramanian S. Salivary diagnostics in COVID-19: Future research implications. J Dent Sci. 2020;15:364–6. [Google Scholar]


