Abstract
Context:
Internal derangements of temporomandibular joint (TMJ) with associated symptoms which do not respond to conservative therapies are refractory cases of temporomandibular joint dysfunction syndrome (TMD). Minimally invasive techniques like arthrocentesis and platelet rich plasma (PRP) injections are usually employed to improve TMJ symptoms and function in these cases.
Aims:
To compare PRP with arthrocentesis for evaluating the effectiveness of PRP in relieving symptoms of refractory TMJ pain dysfunction syndrome.
Setting and Design:
A clinical study was carried out on 52 patients of refractory Temporomandibular joint dysfunction syndrome. The patients were divided in two groups that is Group A - test group and Group B -control Group.
Methods and Material:
Group A consisted of 26 patients who underwent intraarticular PRP injection in TMJ and Arthrocentesis of TMJ was done in 26 patients of Group B. TMJ pain, Maximium Interincisal opening and TMJ clicking were assessed among the group as well as between the groups over a period of 6 months.
Statistical Analysis Used:
Repeated Measure ANOVA was used to compare the parameters within the groups and T test was used for group comparison at 0.05 level of significance.
Result:
There was statistically significant difference in pain intensity improvement 1 ± 0.75 versus 3.17 ± 2.13, maximum interincisal opening 39.86 ± 2.86 versus 37.59 ± 4.03 and clicking 6 versus 16 between the PRP group and arthrocentesis group at P < 0.05.
Conclusions:
Intraarticular PRP injection for the management of refractory TMD is more effective than arthrocentesis in reducing symptoms and functional improvement.
Keywords: Arthrocentesis, platelet rich plasma, temporomandibular joint, temporomandibular joint dysfunction syndrome
Introduction
The temporomandibular joint (TMJ) and related structures are mainly affected in Temporomandibular joint dysfunction syndrome (TMD) which is characterized by pain, limited mouth opening, deviation of lower jaw and joint clicking. TMD cases which do not respond to conservative therapies are refractory cases of TMD.[1,2] Arthocentesis is a method to remove inflammatory mediators from TMJ to improve TMD symptoms.[3] Platelet rich plasma (PRP) has potential healing capacity through its growth factors which can help in relieving the symptoms related to TMD.[4,5] The objective is to study the effectiveness of PRP on pain relief, maximum interincisal opening and clicking in refractory TMD cases in comparison to arthrocentesis.
Material and Methods
The study was designed on patients reporting to the department of oral and maxillofacial surgery between December 2017 to November 2019. All participants have read and signed informed consent form for the study as well as the procedures performed on them. The use of human subjects in this study was reviewed and approved by the institutional ethical committee. The study comprised of patients having TMJ pain not responding to conservative therapy like analgesic, muscle relaxants, isometric jaw exercises, soft diet, heat therapy and occlusal splint therapy. The inclusion criteria were patients having TMJ pain during function, restricted mouth opening due to TMJ dysfunction and with TMJ clicking sounds. Patients with platelet disorder or severe anemia, those on antiplatelet or anticoagulant therapy, those who have taken NSAID in last one week or undergone intraarticular injection during previous 2 months were excluded from the study. Out of 68 enrolled patients, 52 patients qualified in inclusion criteria which were randomly divided in two groups using coin toss method: Group A (test group) consisting of 26 patients, who underwent intraarticular PRP injection in TMJ and Group B (control group) consisting of 26 patients who underwent arthrocentesis of TMJ.
All PRP samples were prepared using aseptic technique; first cycle consists of centrifugation of citrated 10 ml venous blood drawn from the patient at 1800 rpm for 15 min. The second cycle consists of centrifugation of plasma rich layer harvested from 1st centrifuge at 3500 rpm for 10 min to concentrate the platelets. The PRP was finally collected in a sterile syringe for injection. The preauricular region is then prepared aseptically, a line was drawn from the middle of the tragus to outer canthus. Injection site for PRP was marked 10 mm anterior to tragus on the line and 2 mm below it. 0.6 ml of PRP was injected using 20 gauge needle into the TMJ [Figure 1]. After injection, patient was advised to open and close the mouth few times to ensure equal distribution of PRP in the superior joint space of TMJ. For arthrocentesis, two sites of entry were marked first 10 mm anterior to tragus on canthotragal line and 2 mm below it and second site of entry at 20 mm anterior to the tragus and 6 mm below the line. Totally, 50–60 ml of ringer lactate was used to perform arthrocentesis [Figure 2]. The same investigator performed both the procedures. A soft diet was advised for 1 week after intraarticular injection or arthrocentesis. Patient was advised not to take analgesic or anti-inflammatory drug to evaluate pain relief from the PRP injection or arthrocentesis.
Figure 1.
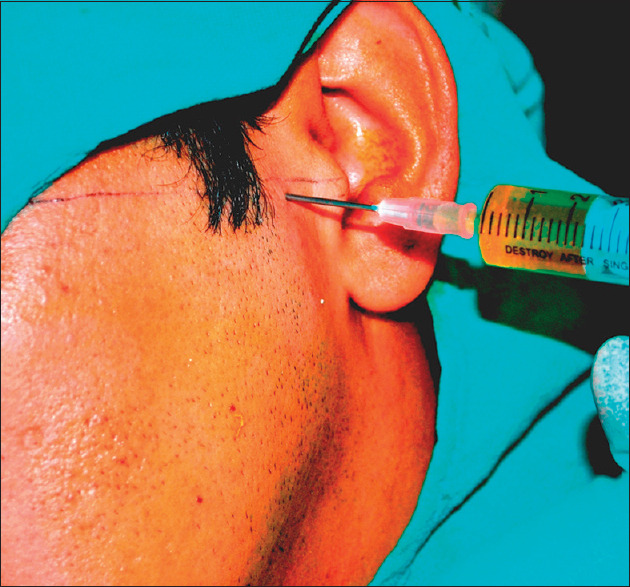
Platelet rich plasma injection in Temporomandibular Joint
Figure 2.

Arthrocentesis of Temporomandibular Joint
The assessment of TMJ pain was done using visual analogue scale which marks from 0 to 10 where 0 means no pain and 10 as worst imaginable pain. The measurement of maximum interincisal opening (MIO) was done using vernier calliper in millimetres. TMJ clicking sound was assessed by placing stethoscope over the preauricular region. All assessments were repeated by the same investigator at the follow up of 1 week, 1 month, 3 months and 6 months after the procedures. Total 8 patients were lost to follow up 4 each from both the groups. Finally, 44 patients (22 each group) underwent statistical analysis.
Statistical analysis was carried out using standard SPSS software version 17. The comparison of pain intensity, maximum interincisal opening and TMJ clicking between the groups was done using T test. Repeated Measure ANOVA was used to compare the parameters within the groups during different time periods. The level of significance was 0.05 for all statistical analysis.
Results
Total 44 patients (22 each group) were analysed after undergoing respective interventions and follow up. In present study, 60% of the patients were male in whole study population. The patient age was ranging from 15 yrs to 54 yrs with average of patients around 30.5 yrs. The patients had symptoms more in left TMJ than right side TMJ.
PRP group
Twenty-two patients treated with intraarticular PRP injection were analysed in the test group. The average age of the patient was 32.3 ± 10.4 yrs. The difference in pain (VAS) scores was statistically significant between pre-injection 5.70 ± 1.16 and 6 months post-injection 1.00 ± 0.75 at P < 0.05 [Table 1]. Even the differences in Maximum incisal opening was statistically significant (P < 0.05) between pre-injection 33.63 ± 6.68 and 6 months post-injection 39.86 ± 2.86 [Table 1]. 22 joints had clicking sound which reduced to 6 joints over a period of 6 months which was statistically significant [Table 1].
Table 1.
Effects of Platelet Rich Plasma on Temporomandibular Joint symptoms
| Parameter | Baseline | 1 week | 1 month | 3 month | 6 month | One way repeated Annova (F ratio) | Inference |
|---|---|---|---|---|---|---|---|
| Pain score (VAS) | 5.70±1.16 | 4.21±1.52 | 3.18±2.01 | 1.96±1.73 | 1.00±0.75 | 77.24 | Statistically significant |
| Maximal interincisal opening | 33.63±6.68 | 35.45±5.75 | 37.5±4.03 | 39.4±2.73 | 39.86±2.86 | 19.34 | Statistically significant |
| TMJ clicking | 22 | 21±0.21) | 15±0.47 | 11±0.51 | 6±0.4 | 13.92 | Statistically significant |
Arthrocentesis group
22 patients treated with TMJ arthrocentesis were analysed in the control group. The average age of the patient was 29.00 ± 8.3 yrs. The difference in pain (VAS) scores was statistically significant between pre-injection 6.25 ± 1.07 and 6 months post-injection 3.17 ± 2.13 [Table 2]. Even the differences in Maximum incisal opening was statistically significant between pre-injection 30.45 ± 3.50 and 6 months post-injection 37.59 ± 4.03 [Table 2]. 22 joints had clicking sound which reduced to 16 joints over a period of 6 months which was statistically not significant [Table 2].
Table 2.
Effects of Arthrocentesis on Temporomandibular Joint symptoms
| Parameters | Baseline | 1 week | 1 month | 3 months | 6 months | One-way repeated Annova (F ratio) | Inference |
|---|---|---|---|---|---|---|---|
| Pain score (VAS) | 6.25±1.07 | 4.2±0.92 | 3.16±1.47 | 3.21±1.92 | 3.17±2.13 | 35.35 | Statistically significant |
| Maximal interincisal opening | 30.45±3.50 | 35.22±3.67 | 37±3.30 | 37.40±4.00 | 37.59±4.03 | 79.72 | Statistically significant |
| TMJ clicking | 22 | 17±0.42 | 17±0.42 | 15±0.47 | 16±0.45 | 2.06 | Statistically not significant |
Group comparison
There was statistically significant difference with respect to improvement in pain intensity (1.00 versus 3.17) between the PRP and arthrocentesis groups (p < 0.05) [Table 3]. The difference in maximum interincisal opening (39.86 versus 37.59) was also statistically significant between the groups at P < 0.05 [Table 3]. There was statistically significant difference in TMJ clicking between the PRP and arthrocentesis groups (6 versus 16 out of 22) at P < 0.05 [Table 3].
Table 3.
Comparison of effects of Platelet Rich Plasma and Arthrocentesis groups on Temporomandibular Joint symptoms
| Parameters | Platelet Rich Plasma Group | Arthrocentesis Group | t-test for 2 independent groups | P | Inference |
|---|---|---|---|---|---|
| Pain score (VAS) | 1.00±0.75 | 3.17±2.13 | 4.49 | 0.00005 | Statistically significant |
| Maximal interincisal opening | 39.86±2.86 | 37.59±4.03 | 2.15 | 0.05 | Statistically significant |
| TMJ clicking | 6±0.4 | 16±0.45 | 3.30 | 0.001 | Statistically significant |
Discussion
Temporomandibular joint dysfunction syndrome is a progressive disorder which clinically may start with any of the symptoms like pain, reduced maximum interincisal opening or clicking. The disease may progress to disc displacement with or without reduction and osteoarthritis at a later stage. The progression of the disease depends on the condition of articular disc, retrodiscal tissue and muscular disharmony of mandible elevator and depressors especially lateral pterygoid muscle having attachment to the articular disc.[1] TMJ pain is a result of alteration in intraarticular pressure of the joint, changes in the synovial fluid or the damage of the retrodiscal tissue.[6,7] The conservative treatment modalities like counseling, hot or cold fomentation, isometric exercises, occlusal splint therapy, jaw physiotherapy, pharmacotherapy etc., should be considered as a first choice therapy in initial stages of the disease because of their negligible side effects.[8] In advance stages of the disease, degenerative or osteoarthritic changes occur in the joint. Minimally invasive and surgical treatment modalities should be considered respectively depending upon the stage of disease progression. It was found in several studies that there is higher prevalence of clinical signs in females than males. Female sex can be considered as one of the risk factor for development of TMD.[9] But in this study, male patients formed 60% of the study population.
Arthrocentesis is widely recognized as first line of minimally invasive treatment modalities in refractory cases of TMD. Arthrocentesis is the process of lavage of the superior joint space of TMJ usually with ringer lactate to remove the inflammatory mediators. It mechanically breaks down the disc adhesions within the joint due to hydrostatic pressure created during the procedure.[3,10] The pain relief in arthrocentesis is because of removal of inflammatory mediators of pain like cytokines and interleukins. This pain relief leads to improvement of mouth opening. Arthrocentesis also breaks adhesions between condylar head, mandibular fossa and articular disc which improves clicking.[11] Arthrocentesis removes the catabolic substances from the joint preventing further progression of TMD. The intraarticular pain relief may induce relaxation of the muscles around the joint providing relief to the muscular pain component of TMD.[12] This study has also shown improvement in TMJ pain, maximum interincisal opening and TMJ clicking following arthrocentesis.
Intraarticular administration of drugs like morphine, corticosteroids, long acting local anesthetic agents, low or high molecular hyaluronic acid have been done in TMD cases with different success rates. Different protocols of drug administration have been tried from single to multiple sessions. In one such study, out of six different intraarticular drug administration protocols, no statistical difference in treatment outcome variables was found.[13] Brennan administered intraarticular morphine infusion after arthrocentesis in temporomandibular joint pain dysfunction syndrome found that 90% of the patient had pain relief even after 1 yr. They recommended arthrocentesis as effective and minimally invasive technique for TMJ pain relief along the use of morphine for long term pain relief.[11] Hyaluronic acid has been compared with PRP in TMJ osteoarthritis in which PRP showed better result at long term follow up.[14]
PRP is derived from whole blood by centrifugation to get a concentrate of platelet rich plasma protein layer above the red blood cell layer. PRP has almost five times higher platelet concentration than whole blood. It provides simple and economic way to obtain growth factors. PRP is rich in growth factors like platelet derived growth factors, transforming growth factors, insulin like growth factors, fibroblast growth factors, vascular endothelial growth factors, endostatins, platelet factor 4, angiopoietins & thrombosponding etc.[15] PRP had been used in different parts of the body and different fields of medicine and dentistry like orthopaedics, spinal infusion, maxillofacial surgery, aesthetic surgery, hair growth stimulation etc.[12,16] PRP injection leads to functional recovery of a particular area like TMJ by regenerating the structures. PRP also have anabolic effect on synviocytes which leads to restoration of hyaluronic acid levels in the joint thereby enhancing cartilage production and joint lubrication.[17] The pain reduction after PRP injection is due to release of protease activated receptor 4 peptides which has analgesic and anti-inflammatory effect.[17] The PRP injection have dual effect of both simulating the inflammatory response as well as has inhibitory effect on excessive inflammation which in-turn has positive effect on tissue healing.[18,19] PRP helps to maintain the integrity of the joint cartilage and enhances articular cartilage repair thereby facilitating joint movement.[12]
Moon et al. found statistically significant improvement in TMJ pain and maximum incisal opening but the improvement in TMJ sounds were not statistically significant when PRP used for intraarticular injection.[16] Pihut et al. concluded that patients of temporomandibular joint dysfunction had reduced pain intensity after intra-articular injections of platelet-rich plasma into the temporomandibular joints.[6] Zhao et al. in meta-analysis found that PRP injections are beneficial in temporomandibular osteoarthritis for pain relief and function improvement of TMJ. It was also concluded that sample size and gender composition play important role in determining the efficacy of PRP.[20] Hassan et concluded that on comparing the parameters between PRP and Arthrocentesis groups, the difference was statistically insignificant. The improvement in pain relief was better in the PRP group but the improvement in TMJ clicking was better in arthrocentesis group.[17] Hanci et al. shown that in comparison to Arthrocentesis group, the reduction in pain intensity and TMJ clicking was statistically significant in the PRP group. But the difference in maximum incisal opening between the two groups was not statistically significant.[12] Long et al. observed that the improvement in maximum interincisal opening and pain intensity was better in PRP group when compared to chitosan group in patients of Temporomandibular joint osteoarthritis. But the improvement in TMJ sounds was comparable.[21] Alafifi et al. concluded that the improvement in TMJ pain was similar in both the PRP and arthrocentesis groups. Whereas improvement in Maximum mouth opening and clicking was better in arthrocentesis group.[22] Rajput et al. suggested that improvement in TMJ pain was better in Arthrocentesis group whereas the improvement in lateral movement and joint sound was better in PRP group.[23]
In present study, there was improvement in all the three parameters i.e., pain intensity, TMJ clicking and maximum interincisal opening in PRP group which was statistically significant. In arthrocentesis group, the improvement in pain intensity and maximum interincisal opening was statistically significant but TMJ clicking improvement was not statistically significant. On comparing PRP and arthrocentesis group, the improvement in pain intensity, maximum interincisal opening and TMJ clicking of the PRP group was more than the arthrocentesis group which was statistically significant. This study will help the primary care physicians to identify the refractory cases of temporomandibular joint dysfunction syndrome. Also they can help the patients to understand that the refractory TMD can be managed with minimal intervention i.e., injection of Platelet rich plasma in temporomandibular joint.
Conclusions
Intraarticular PRP injection is technically more simple and effective method of management of refractory TMD than arthrocentesis. PRP provides better TMJ pain relief along with improved jaw function resulting in increased maximum interincisal opening and decreased TMJ clicking than arthrocentesis.
Key Messages
Arthrocentesis and PRP therapy are usually employed in management of temporomandibular joint dysfunction syndrome. PRP therapy was found more effective than arthrocentesis in relieving refractory TMD symptoms in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wright EF, North SL. Management and treatment of temporomandibular disorders: A clinical perspective. J Man Manip Ther. 2009;17:247–54. doi: 10.1179/106698109791352184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wieckiewicz M, Boening K, Wiland P, Shiau YY, Paradowska-Stolarz A. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J Headache Pain. 2015;16:1–12. doi: 10.1186/s10194-015-0586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nitzan DW, Dolwik MF, Martinez GA. Temporomandibular joint arthrocentesis: A simplified treatment for severe, limited mouth opening. J Oral Maxillofac Surg. 1991;49:1163–7. doi: 10.1016/0278-2391(91)90409-f. [DOI] [PubMed] [Google Scholar]
- 4.Asfaha S, Cenac N, Houle S, Altier C, Papez MD, Nguyen C, et al. Protease-activated receptor-4: A novel mechanism of inflamatory pain modulation. Br J Pharmacol. 2007;150:176–85. doi: 10.1038/sj.bjp.0706975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sharma SM, Thakar D. The clinical efficacy of autologous concentrated platelets in treatment of tmj disorders-a pilot study. Nitte Uni J Health Sci. 2014;4:70–4. [Google Scholar]
- 6.Pihut M, Szuta M, Ferendiuk E, Wieckiewicz DZ. Evaluation of pain regression in patients with TMJ dysfunction treated by intra-articular platelet rich plasma injsctions: A prelimnary report. BioMed Res Int. 2014;3:1–7. doi: 10.1155/2014/132369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishimura M, Segami N, Kanevama K, Sato J, Fujimura K. Comparison of cytokine level in synovial fluid between successful & unsuccessful cases in arthrocentesis of temporomandibular joint. J Oral Maxillofac Surg. 2004;62:284–7. doi: 10.1016/j.joms.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 8.Gupta S, Sharma AK, Purohit J, Goyal R, Malviya Y, Jain S. Comparison between intraarticular platelet-rich plasma injection versus hydrocortisone with local anesthetic injections in temporomandibular disorders: A double-blind study. Natl J Maxillofac Surg. 2018;9:205–8. doi: 10.4103/njms.NJMS_69_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Botelho A, De Arruda Veiga M. Influence of sex on temporomandibular disdorder pain: A review of occurance and development. Braz J Oral Sci. 2008;7:1631–7. [Google Scholar]
- 10.Dimitroulis G, Dolwick MF, Martinez A. temporomandibular joint arthrocentesis and lavage for the treatment of closed lock: A follow up study. Br J oral Maxillofac Surg. 1995;33:23–7. doi: 10.1016/0266-4356(95)90081-0. [DOI] [PubMed] [Google Scholar]
- 11.Brennan PA, ilankovan V. Arthrocentesis for temporomandibular joint pain dysfunction syndrome. J Oral Maxillofac Surg. 2006;64:949–51. doi: 10.1016/j.joms.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 12.Hanci M, Karamese M, Tosun Z, Aktan TM, Duman S, Savaci N. Intra-articular platelet rich plasma injection for the treatment of temporomandibular disorders and a comparison with arthrocentesis. J Craniomaxillofac Surg. 2015;43:162–6. doi: 10.1016/j.jcms.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Manferidini D, Rancitelli D, Ferronato G, Guarda-Nardini L. Arthocentesis with or without additional drugs in temporomandibular joint inflammatory-degenerative disease: Comparison of six treatment protocols. J Oral Rehabil. 2012;39:245–51. doi: 10.1111/j.1365-2842.2011.02265.x. [DOI] [PubMed] [Google Scholar]
- 14.Hegab AF, Ali HE, Elmasry M, Khallaf MG. Platelet-rich plasma injection as an effective treatment for temporomandibular joint osteoarthritis. J Oral Maxillofac Surg. 2015;73:1706–13. doi: 10.1016/j.joms.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez AR, Sheridan P, Kupp LI. Is platelet rich plasma a perfect enhancement factor? A current review. Int J Oral Maxillofac Implants. 2003;18:93–103. [PubMed] [Google Scholar]
- 16.Moon SY, Lee ST, Ryu JW. Ultrasound guided platelet rich plasma prolotherapy for TMJ disorders. J Oral Med Pain. 2014;39:140–5. [Google Scholar]
- 17.Hassan EF, Ali TM, Abdulla NS. The clinical efficiency of platelet rich plasma in the treatment of temporomandibular disorders. Alexandria Dent J. 2016;41:226–31. [Google Scholar]
- 18.Pietrzak WS, Eppley BL. Platelet rich plasma: Biology and new technology. J Craniofac Surg. 2005;16:1043–54. doi: 10.1097/01.scs.0000186454.07097.bf. [DOI] [PubMed] [Google Scholar]
- 19.Woodall J, Jr, Tucci M, Mishra A, Asfour A, Benghuzzi H. Cellular effects of platelet rich plasma interleukin1 release from PRP treated macrophages. Biomed Sci Instrum. 2008;44:489–494. [PubMed] [Google Scholar]
- 20.Zhao K, Liu YS, Nie LS, Qian L, Nie NF, Leptihn S, et al. The influence of sample size and gender composition on the meta-analysis conclusion of platelet-rich plasma treatment for osteoarthritis. J Orthop Translat. 2020;22:34–42. doi: 10.1016/j.jot.2019.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li FL, Wu CB, Sun HJ, Zhou Q. Comparison of autologous platelet-rich plasma and chitosan in the treatment of temporomandibular joint osteoarthritis: A retrospective cohort study. J Oral Maxillofac Surg. 2020:S0278–2391. doi: 10.1016/j.joms.2020.09.016. (20) 31134-4. doi: 10.1016/j.joms. 2020.09.016. [DOI] [PubMed] [Google Scholar]
- 22.Alafifi O, Hassanien H, Taema O. Evaluation of Pain regression in patients with Temporomandibular Disc Displacement with reduction treated by Intra-Articular Platelet-Rich-Plasma injections versus Arthrocentesis. Advan Dent J. 2020;2:129–39. [Google Scholar]
- 23.Rajput A, Bansal V, Dubey P, Kapoor A. A comparative analysis of intra-articular injection of platelet-rich plasma and arthrocentesis in temporomandibular joint disorders. J Maxillofac Oral Surg. 2020:1–8. doi: 10.1007/s12663-020-01351-w. doi 101007/s12663-020-01351-w. [DOI] [PMC free article] [PubMed] [Google Scholar]


