Abstract
Background:
In the wake of the Covid-19 Pandemic, parts of the public health system at increased risk of reduced efficiency include healthcare services for women and children. This in turn could reverse all the progress achieved over the years in reducing maternal and child mortality. In this study, an attempt has been made to assess the indirect effect of the pandemic on maternal and child health services in public health facilities.
Methods:
Data pertaining to maternal and child health services being provided under specific Government programmes, were collected from public health facilities of District Sant Kabir Nagar in Uttar Pradesh, India. Comparative analysis of the data from the pandemic phase with data from the year 2019 was done to determine the impact on services.
Results:
Reduced coverage across all maternal and child health interventions was observed in the study. There was an overall decrease of 2.26 % in number of institutional deliveries. Antenatal care services were the worst affected with 22.91% decline. Immunization services were also dramatically decreased by more than 20%.
Conclusion:
The response of the public healthcare delivery system to the Covid-19 Pandemic is negatively affecting both the provision and utilization of maternal and child healthcare services. It is deterrent to the progress achieved in maternal and child health parameters over the years. Better response strategies should be put in place to minimize lag in service deliwvery.
Keywords: Child health services, COVID-19, maternal health services, pandemic, SARS CoV2
Introduction
Maternal and child healthcare services are of paramount importance for public healthcare delivery systems, especially in low- and middle-income countries. Thousands of women in India die every year due to pregnancy and childbirth-related complications while a significant number of children suffer from vaccine-preventable diseases.[1,2] Current maternal mortality ratio (MMR) in India is 113 per 100000 live births whereas in Uttar Pradesh it is even higher than the national average at 197 per 100000 live births.[3] The infant mortality rate (IMR) in India is 32 per 1000 live births and still higher in Uttar Pradesh at 43 per 1000 live births.[4] Well-designed, proper and timely availability of antenatal care (ANC) services, delivery services, and postpartum care along with infant care and mandatory immunizations form a circle of improved maternal and child health. Disruption at any step might lead to adverse outcomes. In the purview of the aforesaid situation, the Government of India launched the Reproductive, Maternal, Neonatal, and Child Health with Adolescent Health Program (RMNCH + A) in 2013, previously called Reproductive and Child Health (RCH), which is essentially meant to focus on the major causes of maternal and child deaths as well as delays in accessibility and utilization of services.[5] It appropriately directs the efforts of the health workforce towards the most disadvantaged groups and vulnerable populations in ensuring a “continuum of care” through various life stages. Various maternal and child health schemes were rolled out under the umbrella of RMNCH+A.[6] Government schemes encompassing free entitlements and services to pregnant women and infants, aim at inculcating the habit of availing antenatal and postnatal care, instilling awareness towards improving maternal and child health as well as dwindling the MMR and IMR in the country.
The ongoing coronavirus disease (COVID-19) pandemic has challenged the resilience of the most effective health systems of the world. It has emerged as a threat to global public health, forcing countries to go into complete self-imposed lockdowns.[7] It has disrupted the continuum of care and compelled the healthcare systems to prioritize the services rendered by them.[8] Owing to the pandemic, healthcare workers, equipment, and facilities have been transposed to cope with the rising number of patients having COVID-19. Nosocomial COVID-19 infections have further reduced the health workforce.[9] Public health programs meant to deliver RMNCH+services (e.g., vaccinations, free ANC, etc.) were either paused or reduced in scale. The pandemic caused major impediments in the pharmaceutical and medical supply chain globally. Although mortality rates for COVID-19 appear to be low in children and women of reproductive age,[10,11] these groups might be affected out of proportions due to disarrayed routine health services, particularly in low-income and middle-income countries (LMICs) like India. The fear of contracting the virus at health facilities, lack of trust in the health system, and misinformation about the source of the disease are creating breeding grounds that may reverse the progress achieved in maternal and child health indicators. Public health measures, if not customized to country-specific scenarios, may lead to harm that is arguably greater than the fatal effects of a pandemic that were meant to be avoided. Understanding the effects of the measures taken to curb a pandemic on maternal and child health and ensuring that essential health services are maintained while containing the pandemic, is the real challenge emanating from this situation. National programs should continue dispensing core maternal and child services deemed essential to save lives, even while posed with the risk of COVID-19 transmission.
As India veers from the shock of large-scale lockdowns to a gradual return to normalcy, the transition is bound to be slow. The new normal will be very different from the past as we are fighting a pathogen that could well be with us for a long time to come or may never leave. With this in mind, this study intends to quantify the potential impact of the COVID-19 pandemic on maternal and child health services in the state of Uttar Pradesh, India. An analytical study helps in making informed decisions. In this study, we add to the existing knowledge base by estimating the indirect effects of the COVID-19 pandemic on maternal and child health services. While at almost 3 to 4 months into the pandemic, pragmatic and calculable estimates provide a reference point for decision-makers and primary care physicians currently contemplating strategies of response.
Materials and Methods
The state of Uttar Pradesh is the most populous state of the country and has 75 districts.[12] This study was conducted in the district of Sant Kabir Nagar which is situated in the eastern part of the state. District Sant Kabir Nagar has nine community development blocks with six community health centers and three block-level primary health centers.[13] Four major programs of the Government of India providing services in maternal and child health were selected to analyze the overall impact of the COVID-19 pandemic on RMNCH+A services. The selected programs about maternal health are Janani Suraksha Yojana – a monetary incentive-based program to promote institutional deliveries;[14] Janani Shishu Suraksha Karyakram (JSSK) – wherein free entitlements are provided to beneficiaries including free normal delivery and cesarean section, free transport from home to health facility, interfacility transport in case of referral, free drop back from health facility to home after delivery, free diet during the hospital stay, and free provision of blood transfusion;[15] and Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA) – which ensures at least one antenatal check-up for all pregnant women in their 2nd/3rd trimester by a physician/specialist including identification and line listing of high-risk pregnancies based on obstetric/medical history along with pertinent birth planning and complication preparedness at a predesignated government health facility.[16] For evaluation of child health services, the program selected was JSSK which provides free treatment, free transport, free diet, and free provision of blood transfusion to sick infants up to 1 year of age in addition to the aforementioned services to pregnant women;[15] and universal immunization program (UIP). After obtaining due permission from the Chief Medical Officer of District Sant Kabir Nagar, data collection was done from all community and block-level primary health centers. Ethical approval was obtained from the Institutional Ethics Committee of Uttar Pradesh University of Medical Sciences (Ethical approval date 06-07-2020).
Data related to maternal healthcare services were obtained from multiple sources. Data regarding institutional deliveries and free entitlements of JSSK (number of pregnant women provided with free diet, number of pregnant women who availed free transport services from home to health facility, interfacility referral services, and free drop back from health facility to home) were collected from labor room of the health facilities. Data related to immunization services (under UIP) and ANC services that were provided to beneficiaries at an outreach session on village health and nutrition day (VHND) were collected from block program management units (BPMU's) of each facility, which is responsible for compilation of these data at the block level. For services provided under PMSMA, data were collected from antenatal clinics. Data about treatment and investigations of pregnant women and sick infants were obtained from the registers of admission and laboratories at the health facilities. Data were collected for the pandemic period, from March to June 2020, and compared with data for the same period from the year 2019.
The data thus collected were entered into a Microsoft Excel spreadsheet and analyzed using IBM Statistical Package for the Social Sciences (SPSS) version 24.0.
Results
Institutional deliveries
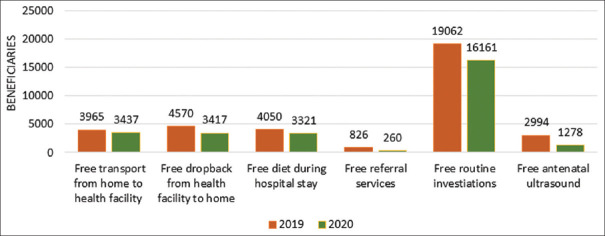
A decline of 2.26%, in several institutional deliveries, was observed during the pandemic period. Though there was an increase in March 2020, in comparison to March 2019, there was a continuous downward trend during the three subsequent months [Figure 1].
Figure 1.
Institutional deliveries (March to June 2019 and 2020)
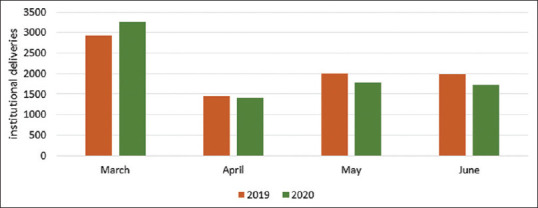
Services under JSSK
During the year 2019, 47.45% of institutional deliveries availed the free transport services from home to healthcare facility whereas 54.69% of women delivering in a public health facility were benefitted from free drop-back after delivery. Out of the total pregnant women delivering in a public healthcare facility, 48.47% were provided with a free diet during their hospital stay. Free referral services were utilized by 9.89% of total women delivering in a government facility. Free of cost routine investigations were done for 19,062 women and free ultrasound for 2994 women.
A declining trend in numbers was observed during the same months in the year 2020. Several women availing free transport services from home to healthcare facility was 42.08% whereas 41.84% availed free drop back post institutional delivery. Free diet during hospital stay was provided to 40.66% of women and only 3.18% of women utilized free referral services in a public health facility. About 16,161 women benefitted from free routine investigations and only 1278 underwent free routine ultrasound [Figure 2].
Figure 2.
Maternal health services under JSSK (March to June 2019 and 2020)
In the year 2019, during the study period, 1421 sick infants received free treatment at a government health facility, 75 sick infants were provided with free transport from home to the healthcare facility, and 120 infants were provided with free conveyance after treatment. Referral services were availed for 126 sick infants. However, in 2020, during the same period, the number of sick infants receiving free treatment dropped down to 769. Free transport services, from home to healthcare facility were provided to 93 sick infants and from hospital to home to 93 infants post treatment. Several sick infants for whom referral services were availed, however, increased to 165.
Services under PMSMA
During the study period in the year 2019, a total of 1436 women received ANC under PMSMA, out of which 800 women received ANC for the first time in the 2nd or 3rd trimester and 443 left-out pregnant women received PMSMA services. ANC services were provided by a general physician to 1281 pregnant women and by an obstetrics and gynecology specialist to 355 pregnant women. As and when needed, as part of routine investigations, 1395 pregnant women were tested for hemoglobin, 1196 were tested for blood group, 1339 were tested for urine albumin, 852 were screened for gestational diabetes mellitus, 1267 women tested for HIV, and 1002 tested for syphilis under PMSMA. A total of 218 high-risk pregnancies were identified, as part of PMSMA services.
The aforesaid numbers fell considerably during the same period in the year 2020. The total number of women who received ANC under PMSMA was 1107, out of which 489 received it for the first time in the 2nd or 3rd trimester. Left-out pregnant women who received ANC services were 577. An obstetrics and gynecology specialist provided ANC to 197 women whereas 1021 women were attended by a general physician. Under PMSMA, 1100 pregnant women were tested for hemoglobin, 1030 were tested for blood group, 1043 were tested for urine albumin, 874 were screened for gestational diabetes, 977 were tested for HIV, and 977 were tested for syphilis, as a part of routine investigations. Several high-risk pregnancies identified were 147.
Immunization services
Immunization services also experienced a declining trend during the study period in 2020 compared to the same in 2019. Several children vaccinated with Bacille Calmette Guerin (BCG) fell by 12.24%. Oral polio vaccine (OPV), pentavalent, and rotavirus vaccines which are administered together at 6 weeks, 10 weeks, and 14 weeks to an infant, were reported with a drop of 24.57%. Measles-Rubella (MR) 1st dose vaccine which is instituted at 9–12 months witnessed a drop of 27.96% whereas Japanese Encephalitis (JE) vaccine 1st dose was administered at the same time fell by 28.28%. MR 2nd dose vaccine experienced an even greater decline of 31.56% along with a similar fall in the JE 2nd dose vaccine which dropped by 30.69%. Tetanus and Diphtheria (TD) vaccine institutions dropped by 20.76% [Figure 3].
Figure 3.
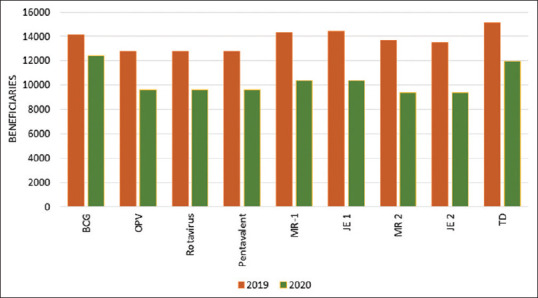
Immunization services (March to June 2019 and 2020)
Discussion
Ever since the first case of COVID-19 was reported, in the last week of February 2020, in the state of Uttar Pradesh, a continuous decline in maternal and child healthcare services has been observed. The worst affected were ANC services provided under PMSMA with a decline of 22.91% along with a 38.88% decrease in ANC during the 2nd and 3rd trimester while ANC by physician decreased by 20.30% and by a specialist by 44.51%. Laboratory services provided to pregnant women revealed a similar trend. Institutional delivery declined by 2.26% during the study period. These findings are similar to a study conducted by Sochas et al. in Sierra Leone to assess the impact of the Ebola epidemic on maternal and neonatal health in which a decline of 22% was reported in ANC services and 8% in facility delivery.[17] There was a significant reduction in the number of pregnant women availing of services under various entitlements of JSSK. A downward trend was observed among sick infants availing services under JSSK but the number of sick infants utilizing free transport from home to health facility increased by 24% and interfacility transport in case of referral by 30.95%. This can be attributed to movement restrictions that reduce physical access, in addition to reduced transport availability and the real or presumed threat of prosecution on being found at a public place without permission.[18] The use of free transport provided by the health facility thus becomes the main mode of movement. These findings are similar to a statistical modeling study by Roberton et al., which used the “Lives saved tool” (LiST) to predict the indirect effects of COVID-19 on maternal and child mortality due to underutilization of services in low- and middle-income countries.[18,19]
There has been a dramatic reduction in immunization services during the pandemic, whereby more than a 20% decrease was observed for all vaccines except for BCG. For BCG the reduction observed was 12.24%, which might be attributed to the fact that it is administered at birth in case of institutional deliveries in a public health facility as well as at VHND sessions. Similar results were reported by Rukmini who evaluated reports of the National Health Mission (NHM) to estimate the disruption of healthcare services in rural India.[19,20]
Conclusion
The COVID-19 pandemic and the response of the healthcare delivery system are affecting and disrupting both the provision and utilization of RMNCH services. These disruptions in maternal and child health services may be due to restrictions imposed by the government on population movements like the creation of containment zones, reassignment of health workers, equipment and facilities to cater to COVID-19 patients, and concerns over contracting the infection while availing these services in public health facilities. This scenario will ultimately result in an increase in maternal and child mortality rates along with the enhancement of other problems like increased pregnancy-related complications, malnutrition among children, etc., The pandemic is far from over, for, there is no specific treatment or vaccine for severe acute respiratory syndrome coronavirus 2 (SARS CoV2), till date. Keeping this in mind the government should plan to provide provisions for comprehensive maternal and child healthcare services along with the treatment of patients infected with SARS CoV2. Measures, to allay apprehensions of getting exposed to the infection while availing care at a public health facility and reinvigorating the demand for routine care among the general public, should be formulated with utmost exigency.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.UNICEF. Maternal health [Internet]. Unicef.org. 2020. cited 2020 Jul 22. Available from: https://www.unicef.org/india/what-we-do/maternal-health .
- 2.World Bank. Number of maternal deaths-India | Data [Internet]. Figure 3: Immunization services (March to June 2019 and 2020) Data.worldbank.org. 2020. cited 2020 Jul 22. Available from: https://data.worldbank.org/indicator/SH.MMR.DTHS?locations=IN .
- 3.Registrar General. Sample registration system. Special bulletin on maternal mortality in India. New Delhi: Office of the Registrar General, India; 2016-18. [Google Scholar]
- 4.Registrar General. Sample Registration System. Vol. 53. New Delhi: SRS Bulletin. Office of the Registrar General, India; 2018. [Google Scholar]
- 5.Government of India. MoHFW.RMNCH+A: National Health Mission [Internet]. Nhm.gov.in. 2020. cited 2020 Jul 22. Available from: https://nhm.gov.in/index1.php?lang=1&level=1&sublinkid=794&lid=168 .
- 6.Government of India. MoHFW.RMNCH+A | National Health Portal of India [Internet]. Nhp.gov.in. 2020. cited 2020 Jul 22. Available from: https://www.nhp.gov.in/reproductive-maternal-newborn-child-and-adolesc_pg .
- 7.Singh S, Singh AK, Jain PK, Singh NP, Bajpai PK, Kharya P. Coronavirus: A threat to Global Public Health. Indian J Community Health. 2020;32:19–24. [Google Scholar]
- 8.Horton R. Offline: COVID-19 and the NHS – 'a national scandal'. Lancet. 2020;395:1022. doi: 10.1016/S0140-6736(20)30727-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kursumovic E, Lennane S, Cook TM. Deaths in healthcare workers due to COVID-19: The need for robust data and analysis. Anaesthesia. 2020;75:989–92. doi: 10.1111/anae.15116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Livingston E, Bucher K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA. 2020;323:1335–7. doi: 10.1001/jama.2020.4344. [DOI] [PubMed] [Google Scholar]
- 11.Ludvigsson JF. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatrica. 2020;109:1088–95. doi: 10.1111/apa.15270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Government of India. Ministry of Home Affairs [Internet]. Censusindia.gov.in. 2020. cited 2020 Jul 22. Available from: https://censusindia.gov.in/2011-prov-results/data_files/india/Final_PPT_2011_chapter 3.pdf .
- 13.Government of Uttar Pradesh. NIC. [Internet] 2020. cited 2020 Jul 22. Available from: https://sknagar.nic.in/subdivision-blocks/
- 14.Lim SS, Dandona L, Hoisington JA, James SL, Hogan MC, Gakidou E. India's Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: An impact evaluation. Lancet. 2010;375:2009–23. doi: 10.1016/S0140-6736(10)60744-1. [DOI] [PubMed] [Google Scholar]
- 15.Government of India. MoHFW. Janani Shishu Suraksha Karyakaram (JSSK) | National Health Portal of India [Internet]. Nhp.gov.in. 2020. cited 2020 Jul 22. Available from: https://www.nhp.gov.in/janani-shishu-surakshakaryakaram-jssk_pg .
- 16.Government of India. MoHFW. About [Internet] PMSMA. 2020. cited 2020 Jul 22. Available from: https://pmsma.nhp.gov.in/about-scheme/#about .
- 17.Sochas L, Channon AA, Nam S. Counting indirect crisis-related deaths in the context of a low-resilience health system: The case of maternal and neonatal health during the Ebola epidemic in Sierra Leone. Health Policy Plan. 2017;32(Suppl 3):iii32–9. doi: 10.1093/heapol/czx108. [DOI] [PubMed] [Google Scholar]
- 18.Ratcliffe R. Teargas, beatings and bleach: The most extreme Covid-19 lockdown controls around the world. The Guardian. 2020. Apr1. Available from: https://www.theguardian.com/global-development/2020/apr/01/extreme-coronaviruslockdown-controls-raise-fears-for-worlds-poorest .
- 19.Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, et al. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: A modelling study. Lancet Glob Health. 2020;8:e901–e8. doi: 10.1016/S2214-109X(20)30229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rukmini S. How COVID-19 response disrupted health services in rural India. Live Mint. 2020;27 [Google Scholar]