Abstract
Background:
The infectious agent which has caused the COVID-19 pandemic is a coronavirus named SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). On one end of the spectrum, a patient suffering from COVID-19 may be asymptomatic or have mild symptoms, while on the other end of the spectrum, a patient may develop numerous life-threatening complications. The way a host responds to infection by SARS-CoV-2 depends on various host factors like hypertension, old age, etc., The MuLBSTA scoring system takes into account various clinical and laboratory parameters and tries to predict the mortality risk for a patient. Besides, the validation of MuLBSTA score for mortality because of COVID-19 has not been extensively studied in an Indian set-up. This study is aimed at finding the association between the MuLBSTA score and the 14-day mortality risk because of COVID-19 in Indian population.
Materials and Methods:
This study included 122 patients who were receiving treatment for SARS-CoV-2 infection at a tertiary hospital in Ranchi, Jharkhand. The disease severity (as per the ICMR guidelines), the MuLBSTA score, and the disease outcome of all patients were noted and analyzed in this study.
Results:
A strong association was seen between a MuLBSTA score of ≥12 and the 14-day mortality risk in COVID-19 patients.
Conclusion:
The MuLBSTA scoring system is an easy to calculate model, which predicts the 14-day mortality risk because of SARS-CoV-2 infection. This may help the primary care physicians in stratifying and referring the patients who have a higher chance of developing severe complications.
Keywords: 14-day mortality, COVID-19, MuLBSTA score, SARS-CoV-2
Introduction
Coronaviruses belong to a family of viruses, which have long been known to cause pneumonia in humans. The infectious agent which has caused the COVID-19 pandemic is a coronavirus named SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). It is a well-known dictum of medical science that disease manifestation and its spread depend on the interplay of the epidemiological triad, that is, host, agent, and environment. The spectrum of manifestations of COVID-19 among humans is very broad. A SARS-CoV-2 infected individual may be asymptomatic, have mild symptoms like cough, fatigue, fever, or sore throat. In extreme cases, a patient may develop life-threatening complications like acute respiratory distress syndrome (ARDS), coagulopathy, and sepsis. Extensive research works are being undertaken to understand the risk factors and protective factors that may alter the clinical outcome of the infection. In addition, many trials are underway to look for various prophylactic measures and treatment options to control this pandemic.
Various clinical prediction rules and their value for evaluation of SARS-CoV-2 infection have been proposed. For example, the mortality in community-acquired pneumonia can be predicted by CURB-65 scoring system.[1] However, whether the criteria holds true for COVID-19 is a matter of debate. Studies have suggested that the mortality rate of COVID-19 may vary from 11.7% to 28.2%.[2] This disparity in mortality rate of COVID-19 is because of a number of factors like comorbidities and the immune status of the infected individual, the health facilities available to the patient and the adopted treatment strategies.
After analyzing and establishing various high-risk factors for disease progression, a number of scores like the CALL score, HNC-LL score, MuLBSTA score, etc., have been proposed that may help healthcare workers in making clinical judgements during this COVID-19 pandemic. The MuLBSTA score is a proposed model which predicts 90-day mortality in viral pneumonia [Table 1].[3,4] Based on six parameters (multilobular infiltration, lymphopenia, bacterial co-infection, smoking history, hypertension, and age), the MuLBSTA score was found to be a strong predictor of 90-day mortality in SARS-CoV-2 infections. According to the strength of association with disease severity, different parameters have been assigned different values in this scoring system, which is tabulated below.
Table 1.
MuLBSTA scoring system
| Parameters | No | Yes |
|---|---|---|
| Multilobular involvement | 0 | +5 |
| Absolute Lymphocyte count≤0.8×109/L | 0 | +4 |
| Bacterial co-infection (Blood/Sputum) | 0 | +4 |
| Smoking History | 0 | Active smoker+3 |
| Prior smoker+2 | ||
| History of Hypertension | 0 | +2 |
| Age≥60 years | 0 | +2 |
In India, the Indian Council of Medical Research (ICMR) has defined a COVID-19 case as mild, moderate, or severe, on the basis of various clinical and radiological criteria P [Table 2]. The expected laboratory findings for each group are also mentioned in the guidelines to support the diagnosis. The treatment protocol for each category has also been elucidated clearly by ICMR to help physicians in India in managing cases.
Table 2.
Classification of a COVID-19 case (as per Clinical Management Protocol by ICMR)
| MILD | MODERATE | SEVERE | |
|---|---|---|---|
| Clinical Criteria | |||
| Oxygen saturation (SPO2) | >94% in Room Air | 90-94% in Room Air | <90% in Room Air |
| Respiratory rate (RR) | <24/min | 24-30 | >30 |
| No pneumonia | Pneumonia + | Pneumonia ++ | |
| CT Chest Criteria | |||
| Normal or<25% | 25%-75% | 75% to 100% | |
| Grade I | Grade II/III | Grade IV |
The guidelines advice management of mild COVID-19 cases at COVID Care Centre, First Referral Units (FRUs), Community Health Centre (CHC), sub-district and district hospitals. The moderate to severe cases are to be managed in Dedicated COVID Health Centre (DCHC) or District hospital or Medical College hospitals.
MuLBSTA scoring system helps to predict mortality by using simple and easily accessible parameters. So, it may help primary care physicians, who have very limited resources at their disposal, in stratifying and referring the patients to a facility where they can be managed properly. For every patient, the score is calculated by adding the values of all parameters. A score of more than or equal to 12 is associated with higher 90-day mortality.[4,5]
A recent study by Rong Xu et al. has shown MuLBSTA scoring system to be a good model for predicting mortality and risk stratification of the patients.[6]
Another study by Garcia Clement MM. et al. showed that MuLBSTA score was better at predicting the need for ICU admissions than other prognostic scores such as PSI-PORT and CURB-65.[7]
This study is aimed at finding the usefulness of the MuLBSTA scoring system in Indian patients suffering from COVID-19 by finding its association with the 14-day mortality risk.
Methods
This single-centre, observational, retrospective study was done at a tertiary health care facility in Ranchi, Jharkhand. All real-time RT-PCR confirmed cases of COVID-19 at the COVID care centre, Rajendra Institute of Medical Sciences (RIMS), Ranchi from July 15, 2020 to August 10, 2020 were included in the study. Ethical and institutional clearance was taken from concerned authorities. Simple random sampling was done and 125 patients were selected and analyzed for clinical, radiological, and laboratory data. Proper consent from all the participants was taken. Outcomes of the illness were followed up until August 18, 2020. Three patients were lost to follow-up and hence were excluded from this study.
The study was approved by the RIMS Ethical Committee and the written informed consent, to be included in the study, was taken from the patients at the time of admission to the COVID Care Centre.
The detailed history related to the age of the patient, chief complaints at the time of admission, smoking history, and history of hypertension was taken. Blood samples were withdrawn and then sent for culture and laboratory analysis to look for lymphopenia and bacterial co-infection. Sputum cultures were also sent to find the evidence of bacterial co-infection. At the time of admission, the respiratory rate and the oxygen saturation in room air was noted. Computed tomography of chest was then carried out for each patient within 3 days of admission. This was done to check for signs of pneumonia and the number of lung lobules involved. All the data was compiled and patients were then grouped into mild, moderate, and severe cases, as per the ICMR guidelines. The MuLBSTA score for each patient was also calculated. The data thus collected was fed into the computers and after proper validation, checked for errors, compiled and analyzed with the help of SPSS 26 software for Windows. The Chi-square test was applied for categorical data to check the significance of the proposed hypothesis.
Results
122 SARS-CoV-2 infected patients were observed in this study. The mean age of the group was 44.16 years (range 11–85 years). 69 patients (56.6%) were male while 53 patients (43.4%) were females.
When the patients were grouped as per the ICMR guidelines for COVID-19, the symptoms of 72 patients (58.1%) in the study were severe while 28 patients (22.6%) were moderate. 22 patients (17.7%) were either asymptomatic or presented with mild symptoms.
The results of Chi square analysis between various parameters of MuLBSTA score and the severity of the disease is tabulated below [Table 3].
Table 3.
Chi-square analysis of various parameters of MuLBSTA scoring system with the severity of disease
| Parameters | Chi-square, Χ2 (2, n=122) |
|---|---|
| Multilobular involvement | 66.716,P<0.01 |
| Absolute Lymphocyte count≤0.8×109/L | 12.542,P=0.02 |
| Bacterial co-infection (Blood/Sputum) | 14.929,P=0.01 |
| Smoking History | 12.772,P=0.01 |
| History of Hypertension | 20.373,P<0.01 |
| Age ≥60 years | 10.910,P=0.04 |
Nine patients (7.3%) in this study had a MuLBSTA score of ≥12, out of which 5 patients died within 14 days of admission. Only 6 patients out of 113 patients (91.1%), who had a MuLBSTA score of <12 died within 14 days of admission [Figure 1].
Figure 1.
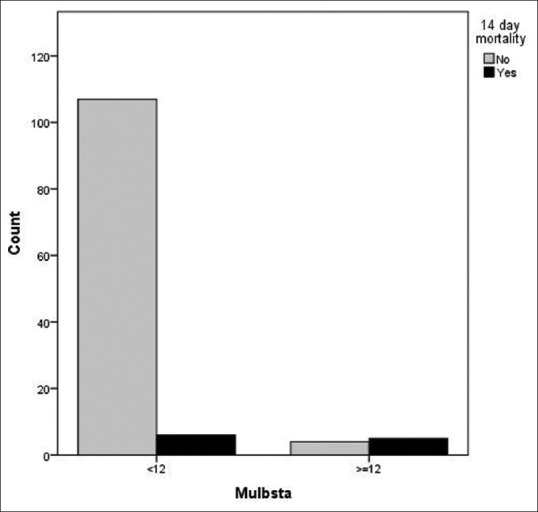
Bar diagram showing association between 14-day mortality and MuLBSTA scoring system
On Chi-square analysis between MuLBSTA score (<12 and ≥12) and the 14-day mortality risk, the following results were obtained.
χ2 (1, N = 122) = 25.655, P < 0.01
On calculating Odds ratio (OR) and relative risk (RR), so as to find the association between the 14-day mortality risk and the MuLBSTA score, the following results were inferred.
OR = 22.29 (CI = 95%), RR = 10.46
This means that, when compared to a patient with a MuLBSTA score of <12, the relative risk of a patient dying within 14 days is 10.46 times higher if his MuLBSTA score is ≥12. Also, the odds of a patient who died within 14 days of admission and having a MuLBSTA score of ≥12 is 22.29.
Discussion
COVID-19 presentations in an individual depend on a number of factors. Increased risk of death because of SARS-CoV-2 infection is commonly seen in smokers, older population, patients with cardiovascular diseases, diabetes, chronic respiratory diseases, hypertension, cancer, or obesity.[8,9,10] It becomes extremely important to determine the prognosis of a disease when so many factors are at play. MuLBSTA scoring system is one such tool that may help a physician in this decision-making.
A meta-analysis by MANNU et al. suggested that multi-lobar involvement in a community-acquired pneumonia is associated with significantly higher chances of mortality.[11] A strong association between lymphopenia and severe COVID-19 cases, more so in younger patients, has also been noted in a few studies.[12] Another study by Huttner et al. in Italy, which included 16,654 patients expired because of severe SARS-CoV-2 infection, have found that around 11% patients had either bacterial or fungal co-infection.[13] Many compelling evidences suggest that SARS-CoV-2 utilizes angiotensin-converting-enzyme-2 receptor, or ACE2-R as its receptor. Since smoking alters the expression of ACE2-R in an individual, association of smoking with mortality because of COVID-19 becomes very likely.[14] Another meta-analysis involving 611,583 subjects have suggested that the older population, aged >60 years, had a much higher chance of dying with SARS-CoV-2 infection, when compared to a younger population.[15] The MuLBSTA score takes into account all these factors and based on the strength of association of various parameters with mortality, it predicts the mortality risk for an infected patient.
A majority of patients (58.1%) included in our study had severe SARS-CoV-2 infection. Almost one-fourth patients (22.6%) had moderate illness while only 17.7% patients were either asymptomatic or had minor symptoms. When classified on the basis of the MuLBSTA scoring system, about 93% patients had a score of <12, while only about 7% patients in the study had a MuLBSTA score of ≥12. When the 14-day mortality risk was compared in both the groups, a strong association of the same was seen in patients with ≥12 MuLBSTA score.
Despite our best efforts, this study had some limitations which can be enumerated as:
Small sample size meant an increased chance of large sampling error.
The MuLBSTA scoring system is used to predict 90-day mortality. However, we could only find an association of the MuLBSTA scoring system with the 14-day mortality risk, due to limitation of resources.
The study was single-centred and retrospective. Hence, the intrinsic bias associated with this study design could not be avoided.
Conclusion
SARS-CoV-2 infection may have protean manifestations in a population. Clinical classification of a patient based on the severity (as per the ICMR protocol for COVID-19) may help a physician in proper management of a case. However, it gives little idea about the prognosis of the disease. COVID-19 is a rapidly evolving subject. Many scores have been proposed to predict the mortality risk associated with SARS-CoV-2 infection. The MuLBSTA score is one such, easy to calculate, score which predicts the 90-day mortality risk. A score of ≥12 is associated with poorer outcome. In our setup, the MuLBSTA scoring system seems to be a reliable predictor of the 14-day mortality risk in patients suffering from COVID-19. So, it may help primary care physicians in triaging and proper referral, thus helping in proper management of COVID-19 cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: An international derivation and validation study. Thorax. 2003;58:377–82. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:934–43. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guo L, Wei D, Zhang X, Wu Y, Li Q, Zhou M, et al. Clinical features predicting mortality risk in patients with viral pneumonia: The MuLBSTA score. Front Microbiol. 2019;10:2752. doi: 10.3389/fmicb.2019.02752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steinberg E, Balakrishna A, Habboushe J, Shawl A, Lee J. Calculated decisions: COVID-19 calculators during extreme resource-limited situations. Emerg Med Pract. 2020;22:CD1–CD5. PMID: 32259419. [PubMed] [Google Scholar]
- 6.Xu R, Hou K, Zhang K, Xu H, Zhang N, Fu H, et al. Performance of two risk-stratification models in hospitalized patients with Coronavirus disease. Front Med (Lausanne) 2020;7:518. doi: 10.3389/fmed.2020.00518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.García Clemente MM, Herrero Huertas J, Fernández Fernández A, De La Escosura Muñoz C, Enríquez Rodríguez AI, Pérez Martínez L, Gómez Mañas S, Iscar Urrutia M, López González FJ, Madrid Carbajal CJ, Bedate Díaz P, Arias Guillén M, Bailón Cuadrado C, Hermida Valverde T. Assessment of risk scores in Covid-19. Int J Clin Pract. 2020:e13705. doi: 10.1111/ijcp.13705. doi: 10.1111/ijcp.13705. Epub ahead of print. PMID: 32931634. [DOI] [PubMed] [Google Scholar]
- 8.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–42. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 9.Huang R, Zhu L, Xue L, et al. Clinical findings of patients with coronavirus disease 2019 in Jiangsu Province, China: A retrospective, multi-center study. PLoS Negl Trop Dis. 2020;14:e0008280. doi: 10.1371/journal.pntd.0008280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 Novel Coronavirus infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mannu GS, Loke YK, Curtain JP, Pelpola KN, Myint PK. Prognosis of multilobar pneumonia in community acquired pneumonia: A systematic review and meta-analysis. Eur J Intern Med. 2013;24:857–63. doi: 10.1016/j.ejim.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 12.Huang I, Pranata R. Lymphopenia in severe corona virus disease-2019(COVID-19): Systematic review and meta-analysis. J Intensive Care. 2020;8:36. doi: 10.1186/s40560-020-00453-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huttner B, Catho G, Pano-Pardo JR, Pulcini C, Schouten J. COVID-19: Don't neglect antimicrobial stewardship principles! Clin Microbiol Infect. 2020;26:808–10. doi: 10.1016/j.cmi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang S, Wang J, Liu F, Liu J, Cao G, Yang C, et al. COVID-19 patients with hypertension have more severe disease: A multicentre retrospective observational study. Hypertens Res. 2020;43:824–31. doi: 10.1038/s41440-020-0485-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bonanad C, Gracia-Blas S, Tarazona-Santabalbina F, Sanchis J, Bertomeu-González V, Fácila L, et al. The effect of age on mortality in patients with COVID-19: A meta-analysis with 611,583 subjects. J Am Med Dir Assoc. 2020;21:915–8. doi: 10.1016/j.jamda.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]


