Abstract
Background:
Institutional quarantine centres were set up in all districts in Kerala as a novel strategy in the fight against novel COVID-19 virus. These were meant for returnees from affected areas, for whom home quarantine was not possible due to lack of facilities. This research aims to evaluate facilities and services of Institutional quarantine centres in Thiruvananthapuram district, Kerala state and to study profile of persons under quarantine in these centres.
Methods:
A cross-sectional study was conducted to evaluate institutional quarantine centres established in Thiruvananthapuram district of Kerala in April 2020. Evaluation was done using a checklist based on standard operating procedures for functioning of centres issued by Health department. Inspection of facilities and registers was done. Details of a subset of inmates were collected by telephonic interviews using a semi-structured questionnaire.
Results:
Two (0.41%) inmates in the centre turned positive on testing while in quarantine. Both of them were foreign returnees and were asymptomatic. There was not a single case of transmission of infection between inmates or to staff and volunteers. The adherence to infection control practices was satisfactory in all centres. One third of inmates were from listed highly affected countries and were mandatorily quarantined.
Conclusion:
Institutional quarantine centres were functioning effectively to provide quarantine facilities for high-risk individuals and thereby controlling the spread of COVID-19. Selection of facilities, staffing pattern and day to day functioning of these centres is a model which can be replicated at other COVID-19 affected areas.
Keywords: COVID-19, evaluation, institutional quarantine, institutional quarantine centres, Kerala
Introduction
The Corona virus Disease 2019 which was first reported from Wuhan city of China in December 2019 is increasing at an alarming rate with more than 19.7 million confirmed cases and 728013 deaths globally with 2215074 cases and 44386 deaths in India as on 10.08.2020.[1,2] Kerala reported the first case of India on January 30, 2020 which was an imported case from China following which there was a rise in number of cases, most of them being imported.[3] The persons from affected countries appearing to be healthy may be in the incubation period at the time of arrival. It takes on an average 5.2 days for symptoms to appear following the exposure to infection.[4] If the person interacts with the community during the incubation period, there is a chance of spread of infection to others in the community unknowingly.[5] To tackle the situation, Kerala has strengthened the surveillance and control measures against the disease. As part of control measures, the Government of Kerala advised quarantine for those who arrived in Kerala from affected countries and other states in India.
Quarantine is the restriction of movement of healthy people who are exposed to a communicable disease for preventing disease transmission in community.[6,7] Highly infectious nature of disease with asymptomatic and pre-symptomatic patients showing infectivity is a major challenge for controlling the disease.[8] The severity of disease and mortality is higher in elderly patients compared to adults which was also a concern for Kerala since elderly population constitutes 12.6% of total population of Kerala.[9] So, to prevent the transmission of infection from those who have arrived from affected countries quarantine was advised by Government of Kerala. Ensuring adherence to quarantine was the next challenge. So, to ensure successful completion of quarantine period, Institutional quarantine centres named as COVID care centres were established in the state.
An institutional quarantine centre in Kerala is a facility meant for quarantining persons who have arrived from affected countries and other states in India. Objective of these centres is to enable successful isolation and management of asymptomatic cases especially when room quarantine at their homes was not possible due to lack of facilities.[10] Standard Operating procedures for functioning of Institutional quarantine centres was issued by Government of Kerala for effective functioning of these centres. There is a need to evaluate the functioning of these centres in the pre lockdown phase and initial phase of lockdown so as to make informed decisions regarding steps to be taken for improvement of services and for planning upgradation of facilities post lock down. This study aims to evaluate the facilities and services of institutional quarantine centres in Thiruvananthapuram district of Kerala and to study the profile of persons under quarantine in these centres during pre-lock down phase and initial phase of lockdown.
Materials and Methods
A cross-sectional study was conducted to evaluate institutional quarantine centres established in Thiruvananthapuram district of Kerala and to study the profile of persons under quarantine in these centres. Purpose of evaluation was to give feedback and to generate suggestions for improvement, as preparedness for the next phase of the epidemic. Evaluation was done during the month of April 2020 by a team of doctors from the Department of Community Medicine, Government Medical College, Thiruvananthapuram, with concurrence from the district health administration and clearance from the Human Ethics Committee of the institution. Team adhered to infection control practices by wearing masks, practicing social distancing and using hand sanitizers while doing evaluation. Out of the seven centres initially started in Thiruvananthapuram district, five centres were functioning at the time of evaluation and all these five centres were evaluated. Evaluation was done using a checklist based on standard operating procedures for functioning of Institutional quarantine Centres issued by the Department of Health and Family Welfare, Govt of Kerala. Inspection of facilities and registers was done. Inmates, health staff and health care volunteers of these centres were interviewed. Data regarding COVID-19 test status of inmates was analysed. The demographic profile, country/region from where arrived and date of quarantine were obtained from the registers maintained in the centres. A semi-structured questionnaire was used to collect information from a subset of inmates. Details on co-morbidities, infection control practices, rating of services received and complaints if any were collected using telephonic interviews from them. Data was entered into Microsoft excel and analysed using SPSS 26.0 (IBM SPSS Statistics Released 2018/11/30. SPSS for Windows, Trial Version 26.0.) The data collected was consolidated and described using appropriate measures of central tendency or proportions. The ethics clearance was obtained from Human Ethics Committee, Government Medical College, Thiruvananthapuram (HEC.No. 03/21/2020/MCT). Permission letter to conduct institutional evaluation was obtained from the District Medical Officer, Health. Informed verbal consent was recorded for telephonic interviews. Confidentiality was maintained and all data collected were used for the purpose of this study only.
Results
Institutional quarantine centres in Thiruvananthapuram, the capital city of Kerala state was functioning in Training centres of Government Departments, University Hostels and a private sector convention centre. Among the five centres evaluated, one was located in coastal area, three were in the centre of the city and one in the periphery. It was run by Thiruvananthapuram Corporation authorities with support from Health Department, Police Department, various other Government departments, NGOs, Self-help groups like Kudumbasree and Volunteers. Average of 100 inmates were admitted during a week's time in each of these centres. Standard Operating procedures issued by the Department of Health and Family Welfare; Govt of Kerala were followed by all centres even though some deficiencies were there in some centres in certain aspects.
Facilities were sufficient to provide bath attached single rooms to all inmates in two of the centres. High-risk individuals were provided with separate bath attached rooms while low risk individuals were allowed to share rooms in two centres. Quarantine was ensured by allocating bathrooms in the common pool to individuals to avoid sharing in those centres. In the initial days due to lack of facilities there was sharing of rooms in one centre which was closed immediately following identification and reporting of risk of transmission of infection by health authorities. With limited availability of facilities, providing single bath attached rooms to all inmates was a challenge. Electricity and water supply were uninterrupted in all these centres.
Medical officers and Health Inspectors were appointed as charge officers in all these facilities. Junior Health Inspectors (JHI), posted round the clock, were running the facilities. Service of doctors was also available round the clock. Services offered by volunteers was a unique factor contributing to effective functioning of these facilities. Smooth running of the facility was affected in centres where volunteers registered were less in number. There was a shortage of security personnel in all centres.
Medicines were not routinely procured by the centres. Some centres had patients with chronic diseases on medicines. For those patients and for minor ailments, medicines were arranged appropriately with the help of volunteers. Uninterrupted supply of masks, PPE and sanitisers was ensured by district health authorities. Other essential supplies like soaps, bed sheets and disinfectants were supplied by the corporation authorities, NGOs and Volunteers. Food and bottled drinking water were supplied by Thiruvananthapuram Corporation from Community Kitchen/Kudumbasree.
Cleaning services were provided by staff from the corporation office. In some centres this arrangement was inadequate to maintain standards. Sometimes, rooms and allotted bathrooms were cleaned only when the inmate vacated. Clothes were washed by inmates themselves. Bedsheet and pillow cover were provided by the corporation and given as per the demand from inmates. Bed sheet was either burned or taken back by the person itself. Waste was collected by corporation authorities for disposal on a daily basis. System for waste segregation in colour-coded bags was present in only some centres. There was a need for cleaning services to be entrusted to specially trained personnel in the context of such a highly infectious disease.
There was not a single case of transmission of infection between inmates or to staff and volunteers. This reflects the effectiveness of infection control systems in place. Health staff gave strict instructions regarding infection control practices to all inmates at time of admission. Soap for handwashing and masks were provided to all. But use of masks by inmates was variable. Health staff and volunteers were using masks and gloves appropriately. PPE kits were given for cleaning staff. Hand sanitizer was made available at the registration desk. IEC materials on infection control were displayed in all centres in the common areas. Sodium hypochlorite solution was used for cleaning. Disinfection of facility was done regularly by Corporation staff in some centres.
Maintenance of registers and documentation were satisfactory. A register was maintained by Junior Health Inspector (JHI) at the registration desk. Name, address, contact number, age, sex, country/region, and date of arrival were recorded in the register. In some centres' registers were not updated systematically. A common format was not there for all centres. Symptom checklist for screening was not used at the registration desk. Persons developing symptoms were shifted to General hospital in an ambulance for testing. On interviewing inmates, it was found that some were symptomatic, but were not referred to hospitals as their initial test results were negative. Initial negative results had given a false sense of security both to staff and inmates.
The mean age of the inmates was 37.3 (±13.8) years. More than three-fourth of study participants were males. Available data on travel history showed that most of them had arrived from Dubai and other gulf countries. More than one third of inmates were mandatorily quarantined because of travel history from affected foreign countries. The demographic and epidemiological profile of the study subjects is summarized in Table 1. Two inmates tested positive for the disease while they were in quarantine and both of them were shifted in an ambulance, to COVID isolation unit of Government Medical College Thiruvananthapuram, which was the designated COVID hospital for the district. Both of them were foreign returnees and were asymptomatic. Most of the admissions to institutional quarantine centres were during the last week of March, immediately before lockdown was announced. The pattern of admission to Institutional quarantine centre is shown in Figure 1.
Table 1.
Demographic and epidemiological profile
| Characteristics | Study population n (%) |
|---|---|
| Age group (n=482) | |
| 1-17 years | 19 (3.9) |
| 18-40 years | 282 (58.6) |
| 41-60 years | 156 (32.3) |
| >60 years | 25 (5.2) |
| Gender (n=482) | |
| Male | 415 (86.1) |
| Female | 67 (13.9) |
| Travel history in the last one month (n=250) | |
| Dubai | 47 (19) |
| Other gulf countries | 34 (14) |
| European countries | 22 (9) |
| Other Asian countries | 9 (3) |
| USA | 3 (1) |
| Australia | 4 (2) |
| Other states in India | 97 ((39) |
| Other districts in Kerala | 34 (13) |
| Reasons for Quarantine (n=326) | |
| Mandatory Quarantine | 118 (36.2) |
| Travel from other states | 85 (26) |
| Fishermen | 77 (23.6) |
| Railway employee | 19 (5.8) |
| Travel from other districts | 11 (3.4) |
| Accompanied COVID-19 patient | 4 (1.2) |
| Symptoms | 4 (1.2) |
| Institutional quarantine Centre staff | 2 (0.6) |
| Ambulance driver | 2 (0.6) |
| Destitutes | 2 (0.6) |
| No facility at home | 1 (0.3) |
| Airport worker | 1 (0.3) |
Figure 1.
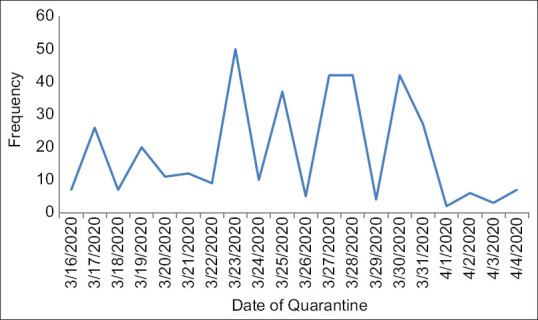
Pattern of admission in Institutional quarantine centres
Among the 50 inmates interviewed, 2 (4%) had diabetes mellitus, 2 (4%) had hypertension and 2 (4%) had both diabetes and hypertension. More than one third (40%) of the inmates could not be sent home since they had an elderly relative and did not have enough facilities to ensure strict home quarantine. Symptoms were reported by 4 (8%) out of 50 inmates. All four had breathlessness and two of them had fever. Swab was taken from 33 (66%) study subjects for testing and all of them were found to be negative. All inmates reported that practice of social distancing, frequency of handwashing and usage of masks increased after arriving in the Institutional quarantine centre. 46 (92%) out of 50 inmates were satisfied with the services provided in the Institutional quarantine centres. 37 (74%) subjects didn't report any complaint. Out of 13 persons who had complaints, 8 (62%) reported about the absence in variety of food choices, three reported lack of proper cleanliness of toilets and two reported both the complaints. Poor mental wellbeing was self-reported by 6 (12%) study participants.
Discussion
Institutional quarantine centre was a major public health measure taken as part of the state's response to the pandemic. Influx of expatriates and highly infectious nature of disease was a huge challenge for controlling the disease in Kerala.[11,12] In such a situation for getting things under control, Government of Kerala introduced institutional quarantine by establishing Institutional quarantine centres.
Effectiveness of quarantine as a community containment strategy is evident from 2003 global SARS outbreak.[13] Even though home quarantine may be the preferred one by the persons, ensuring adherence and completion of quarantine is difficult. Designated institutional quarantine facilities serve the purpose in these situations. For effective functioning of these centres, Government should establish mechanisms for enforcement and provision of essential facilities which is a resource intensive task. This study provides evidence regarding the functioning of Institutional quarantine centres established in Thiruvananthapuram district, the advantages of this strategy, disadvantages and the areas which need improvement.
Published literature shows establishment of facilities with same objective during previous outbreaks like Observation units for ensuring quarantine for asymptomatic contacts during the Ebola outbreak in Nigeria.[14] Similarly Ebola community care centres for successful isolation of cases was also established during that time apart from Ebola treatment centres.[15] Such kind of community-based centres for successful quarantine and isolation was found to be successful during outbreaks. In our setting Institutional quarantine centres were started in established buildings like hostels, convention centres or training institutes. Similarly, evidence suggests use of hotels, construction work sites and universities for quarantine during SARS outbreak in China in 2003.[16] Even though the recommendation was to provide bath attached single rooms, sharing of rooms and bathrooms was there because of resource constraints. Well ventilated rooms were provided to the inmates as per the instructions in the Standard Operating Procedures of the state health department.[10] The centres were functioning with adequate staff except for the shortage of healthcare volunteers in some centres. More number of healthcare volunteers in the centres can ease the functioning and reduce the burden on health care staff. Security personnel and support from police is also a need since violation of quarantine was an issue in some centres.
Food and water were provided under the leadership of the Corporation without any interruption. Studies report a similar pattern where the food is provided by community health workers under the leadership of Municipality during the SARS outbreak.[16] Cleaning services were not adequate with no proper waste segregation and disposal system in most of the centres in contrast to the cleaning and disinfection practices practiced in observation units in Ebola outbreak.[14] Health staff, Volunteers and cleaning staff were using PPE appropriately. Most of the studies report adequate usage of PPE by health care staff in quarantine centres during such outbreaks.[14,16] Sodium hypochlorite solution was used for cleaning as per the national and state guidelines.[17] Mechanisms for ensuring cleanliness and disinfection of facilities should be improved with the support of LSGD.
Systematic screening should be compulsorily done before admission to prevent overcrowding and transmission of infection within the facility. Initial negative results should not be a reason for leniency.[18] Staff and inmates should be made aware of the possibility of a false negative result in the immediate post exposure period. Any person who turns symptomatic irrespective of his test result should be isolated. Strict quarantine for 14 days should be followed by all. Till date, no instance of spread of infection within the facility is reported. Two inmates have got COVID-19 positive result and were under strict quarantine in the centre. Hence there was no risk of spread.
Most of the inmates were adult males as majority of them were either employed or went in search for better job opportunities in other countries. Most of them had travel history, with 48% arriving from other affected countries. Interviewing a subset of inmates showed that 40% of them had elderly at their homes which shows the need for quarantine in designated facilities. If the number of cases increases exponentially in the coming days reverse quarantine may be a better strategy.[19] Some of the inmates reported poor mental well-being during the quarantine period. Many studies during the Ebola and SARS outbreak also reported the same and people suffered from anxiety and depression.[20,21] Studies among quarantined children and adolescents also reported psychological problems.[22] Psychological support services and actions directed towards the well-being of inmates should be strengthened. The system should also address their apprehension on return to home.
Similar to Fangcang shelter hospitals in China, for treating asymptomatic and mild cases Corona First Line Treatment Centres (CFLTC) were established in Kerala.[23] Institutional quarantine centres and CFLTC are now functional in every panchayath in the state. The Medical Officer of Primary Health Centre is in charge of these centres. The findings from this study helps primary care physician to run institutional quarantine centres effectively by filling the identified gaps. It also serves as a model for facility level preparedness at primary level as a response to pandemic which includes infrastructure assessment, equipment, supplies, documentation, health worker safety, patient care, biomedical waste management and disinfection at facility, health information, communication, documentation, monitoring and reporting. The experience with functioning, staff pattern, infection control practices, screening and documentation in institutional quarantine centres can be employed in COVID First Line Treatment Centres which is also managed by primary care physician. The effective functioning of these centres during outbreak suggests that they could be replicated in future public health emergencies also.
Summary
Institutional quarantine centres, the novel strategy established for fighting novel disease were found to be functioning effectively in providing quarantine facilities at primary level of care. The staff pattern, infection control practices, infrastructure, supplies, health information and monitoring in these centres were found to be satisfactory. There was not a single case of transmission of infection between inmates or to staff and volunteers. The functioning of these centres serves as a model which can be replicated in future pandemics as well.
Conclusion
Strategic planning and coordinated effort of various departments under leadership of State and District authorities combined with dedication and hard work of health staff and volunteers have resulted in successful setting up of Institutional quarantine Centres. These centres are functioning effectively to provide quarantine facilities for high-risk individuals and thereby containing the spread of COVID-19 in Kerala. Evaluation of these centres in pre lock down and initial phase of lockdown period has generated evidence for planning and modifying strategies in running Institutional quarantine Centres more effectively in post lock down phase. This model devised by state of Kerala can be adopted by other states and countries in controlling this Pandemic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Coronavirus Disease (COVID-19) Situation Reports [Internet] cited 2020 Jun 23. Available from: https://www.who.int/emergencies/diseasesovelcoronavirus-2019/situation-reports .
- 2.#IndiaFightsCorona COVID-19 [Internet]. MyGov.in. 2020. cited 2020 Jun 23. Available from: https://mygov.in/covid-19/
- 3.COVID 19 Kerala – dhs [Internet] cited 2020 May 07. Available from: https://dhs.kerala.gov.in/public-health-2019-n-corona-virus/
- 4.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li P, Fu JB, Li KF, Liu JN, Wang HL, Liu LJ, et al. Transmission of COVID-19 in the terminal stage of incubation period: A familial cluster. Int J Infect Dis. 2020;96:452–3. doi: 10.1016/j.ijid.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Quarantine and Isolation | Quarantine | CDC [Internet] 2019. cited 2020 May 08. Available from: https://www.cdc.gov/quarantine/index.html .
- 7.Gensini GF, Yacoub MH, Conti AA. The concept of quarantine in history: From plague to SARS. J Infect. 2004;49:257–61. doi: 10.1016/j.jinf.2004.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ye F, Xu S, Rong Z, Xu R, Liu X, Deng P, et al. Delivery of infection from asymptomatic carriers of COVID-19 in a familial cluster. Int J Infect Dis. 2020;94:133–8. doi: 10.1016/j.ijid.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu K, Chen Y, Lin R, Han K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect. 2020;80:e14–8. doi: 10.1016/j.jinf.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.COVID-19- Advisory for admission to Institutional quarantine centre-dhs [Internet] cited 2020 May 08. Available from: http://dhs.kerala.gov.in/wp-con .
- 11.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72314 cases from the Chinese Center for disease control and prevention. JAMA. 2020;323:1239–42. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 12.Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (covid-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020;172:577–82. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.SARS | Guidance | Management of Contacts of Cases in Community Containment | CDC [Internet] 2019. cited 2020 May 12. Available from: https://www.cdc.gov/sars/guidance/d-quarantine/management.html .
- 14.Grigg C, Waziri NE, Olayinka AT, Vertefeuille JF. Use of group quarantine in ebola control — Nigeria, 2014. MMWR Morb Mortal Wkly Rep. 2015;64:124. [PMC free article] [PubMed] [Google Scholar]
- 15.Kucharski AJ, Camacho A, Checchi F, Waldman R, Grais RF, Cabrol JC, et al. Evaluation of the benefits and risks of introducing ebola community care centers, Sierra Leone. Emerg Infect Dis. 2015;21:393–9. doi: 10.3201/eid2103.141892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pang X, Zhu Z, Xu F, Guo J, Gong X, Liu D, et al. Evaluation of control measures implemented in the severe acute respiratory syndrome outbreak in Beijing, 2003. JAMA. 2003;290:3215–21. doi: 10.1001/jama.290.24.3215. [DOI] [PubMed] [Google Scholar]
- 17.90542653311584546120quartineguidelines.pdf [Internet] cited 2020 May 12. Available from: https://www.mohfw.gov.in/pdf/90542653311584546120quartineguidelines.pdf .
- 18.CDC. Coronavirus Disease 2019 (COVID-19) [Internet]. Centers for Disease Control and Prevention. 2020. cited 2020 May 12. Available from: https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html .
- 19.Langford T. Medical center considers reverse quarantine as possible ebola prevention [Internet] The Texas Tribune. 2014. cited 2020 May 13. Available from: https://www.texastribune.org/2014/08/12/baylor-college-medicineconsiders-reverse-quarantine/
- 20.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–20. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reynolds Dl, Garay JR, Deamond Sl, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008;136:997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saurabh K, Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to Covid-19 pandemic. Indian J Pediatr. 2020;87:1–5. doi: 10.1007/s12098-020-03347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen S, Zhang Z, Yang J, Wang J, Zhai X, Bärnighausen T, et al. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet. 2020;395:1305–14. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


