Abstract
Background
Positive communication behaviour within anaesthesia teams may decrease stress response and improve clinical performance. We aimed to evaluate the effect of positive communication during medical handover on the subsequent team-based clinical performance in a simulated critical situation. We also assessed the effect of positive communication behaviour on stress response.
Methods
This single-centre RCT involved anaesthesia teams composed of a resident and a nurse in a high-fidelity scenario of anaesthesia-related paediatric laryngospasm after a standardised handover. During the handover, similar information was provided to all teams, but positive communication behaviour was adopted only for teams in the intervention group. Primary outcome was team-based clinical performance, assessed by an independent blinded observer, using video recordings and a 0-to 100-point scenario-specific scoring tool. Three categories of tasks were considered: safety checks before the incision, diagnosis/treatment of laryngospasm, and crisis resource management/non-technical skills. Individual stress response was monitored by perceived level of stress and HR variability.
Results
The clinical performance of 64 anaesthesia professionals (grouped into 32 teams) was analysed. The mean (standard deviation) team-based performance score in the intervention group was 44 (10) points vs 35 (12) in the control group (difference: +8.4; CI95% [0.4–16.4]; P=0.04). The effects were homogeneous over the three categories of tasks. Perceived level of stress and HR variability were not significantly different between groups.
Conclusions
Positive communication behaviour between healthcare professionals during medical handover improved team-based performance in a simulation-based critical situation.
Clinical trial registration
Keywords: clinical performance, communication behaviour, high-fidelity simulation, positive communication, stress response, teamwork
Editor's key points.
-
•
Positive communication behaviour may decrease stress response and improve clinical performance.
-
•
The effect of positive communication during medical handover on team-based clinical performance and stress response was studied in a simulated critical situation (paediatric laryngospasm).
-
•
Mean team-based performance score in the positive communication intervention group was greater than in the control no-intervention group, with no significant effect on stress response.
-
•
Positive communication behaviour during medical handover improved team-based performance in a simulation-based critical situation.
Enhancing teamwork improves clinical performance and patient safety, particularly in anaesthesia.1,2 Team-based crisis management is strongly influenced by a set of social and cognitive skills grouped under the term ‘crisis resource management’.3, 4, 5 Effective communication is one of its central components,6,7 and both verbal8, 9, 10 and non-verbal11, 12, 13 aspects of communication within a team appear essential.14 Coping with stress is also fundamental for crisis management to avoid disruption of cognitive processes15 and reduction of clinical performance.16,17
Positive communication behaviour is a technique aiming to optimise both the verbal and non-verbal components of the communication process. It consists, on the verbal aspect, of using positive suggestions without any form of negation, and on the non-verbal aspect, of using a calm and slow voice; looking in the eyes; and displaying a smiling face, an open posture, and appropriate clothing.18 Positive communication behaviour is known to reduce stress response and its consequences in patients,19 but its potential benefit in healthcare professionals themselves remains to be studied.
Laryngospasm is a frequent potentially serious complication of paediatric anaesthesia.20 This critical incident is well suited for a short simulation and requires essential technical and non-technical skills.21 The primary objective of the present study was to evaluate the effect of positive communication behaviour during medical handover on subsequent team-based clinical performance in a standardised simulated scenario of anaesthesia-related paediatric laryngospasm. The secondary objective was to evaluate its effect on health professionals' acute psychological and physiological stress response.
Methods
Population and setting
This study was a prospective RCT (1:1) with two parallel arms, blinded evaluation, and a hypothesis of superiority. The protocol was preregistered on https://clinicaltrials.gov/(protocol ID: NCT03375073). Approval was obtained from the ethics committee of the French Society of Anesthesia & Intensive Care Medicine (IRB 00010254-2019-066) on May 19, 2019. The study was conducted at the medical simulation centre of the Grenoble Alpes University Hospital (Alps Research Assessment and Simulation Centre) during the 2017–8 academic year. The study followed the recommendations of the International Committee of Medical Journal Editors and the Consolidated Standards of Reporting Trials guidelines22 and its extensions for clustered trials, non-pharmacological treatment intervention, and healthcare simulation research. All subjects were volunteer professionals from the Grenoble Alpes University Hospital and gave written and informed consent to participate and to be filmed. Before the simulation, participants received a general briefing on room layout and mannequin features and limitations. Confidentiality, kindness, and the right to make mistakes were emphasised as fundamental principles of simulation learning and research. Once the scenario was completed, they received a structured debriefing. The instructor group was composed of certified anaesthetists and residents with a specific medical simulation diploma.
Work scenario
Our standardised high-fidelity simulated scenario of anaesthesia-related paediatric laryngospasm was derived from a published scenario,21 and had been repeatedly and successfully tested in our centre. It was constructed and described following the French Society of Simulation in Health (Société Francophone de Simulation en Santé) guidelines (Supplementary Appendix 1).23 It involves a two-person anaesthesia team: an anaesthesia resident and a nurse anaesthetist. Working in pairs is commonplace in France, particularly in paediatric anaesthesia. Before the scenario begins, the team receives from the senior anaesthetist a 1 min handover about the ongoing case (Table 1). After the handover, the resident and the nurse are left alone with the surgeon (played by a neutral embedded facilitator) and the anaesthetised patient (mannequin SimJunior®; Laerdal Medical, Stavanger, Norway). The senior anaesthetist remains available by telephone. After a 2 min time out, the surgeon makes the skin incision, which is immediately followed by an airway obstruction as a result of complete laryngospasm and rapid oxygen desaturation. The scenario is stopped when the anaesthesia team, once the incident is resolved, authorises the surgeon to resume the procedure.
Table 1.
Handover delivered by the senior anaesthetist to the participants.
| Control group |
Intervention group |
|
|---|---|---|
| Control communication behaviour | Positive communication behaviour | |
| Duration of handover | 1 min | |
| Information provided | 7-yr-old boy with no medical history | |
| Planned circumcision | ||
| Surgical safety checklist completed | ||
| General anaesthesia induced with sevoflurane | ||
| Airway controlled with a supraglottic device | ||
| Bilateral pudendal block + sufentanil 0.1 μg kg−1 i.v. | ||
| Surgeon about to make the incision | ||
| Non-verbal communication | ||
| Clothing | Coffee stained and poorly fitting | Clean and tight |
| Facial expression | Stressed and tired face | Calm, relaxed, and smiling face |
| Gaze orientation | Looking at the floor | Looking into the eyes |
| Posture | Closed, distant, crossed arms | Open, close, accompanying gestures |
| Voice | Fast, jerky, and sighing | Slow, regular, and grave |
| Verbal communication | ||
| Phrases | Usual, with some negative turns | Avoidance of negative turns |
| Vocabulary For example: |
Usual, with some negative words | Positive words favoured |
| ‘struggling boy’ | ‘cute, dynamic little boy’ | |
| ‘complicated’ | ‘easily’, ‘comfort’ | |
| ‘delay time’ | ‘security’ | |
| Additional comments For example: |
Made of non-positive suggestions | Made of positive suggestions |
| ‘Oh, it's you … ’ | ‘Nice to see you!’ | |
| ‘I hope everything goes well.’ | ‘It's all right. You have my full trust’. | |
| Reaction when the telephone rings | Picks up the telephone, says he has no time to talk, and then hang up. | Turns off the ringing telephone and does not answer. |
Development of the clinical performance scoring tool
A specific scoring tool was previously developed to assess team-based clinical performance in the work scenario. This tool was obtained after a four-step development method. First, the investigators composed a preliminary list of tasks, based on available literature, their experience, and the specifics of the scenario. Second, the list was revised, elaborated, and weighted by six subject-matter experts by means of a targeted modified Delphi survey. Third, the resulting provisional tool was pilot tested on a sample of simulations and improved accordingly. Fourth, the experts made an ultimate review leading to the final tool.
The final tool (Supplementary Appendix 2) consisted of 22 tasks, divided into three categories corresponding to the main pedagogical objectives of the scenario: ‘safety checks before the incision’, ‘diagnosis and treatment of laryngospasm’, and ‘crisis resource management and non-technical skills’. Each task is associated with a behaviourally anchored two- to four-level rating scale and weighted for a total of 100 points. The tool allows calculation of category-specific performance scores (0- to 18-, 0- to 42.5-, and 0- to 39.5-point scales, for safety checks before the incision, diagnosis and treatment of laryngospasm, and crisis resource management and non-technical skills, respectively), and the overall clinical performance score (0- to 100-point scale).
Inter-rater reliability was studied by having the final tool applied in eight video-recorded simulations by three independent assessors. The overall intra-class correlation coefficient (ICC; two-way model, absolute agreement, single measures) was 0.85. Category-specific ICCs were 0.87, 0.90, and 0.62 for safety checks before the incision, diagnosis and treatment of laryngospasm, and crisis resource management and non-technical skills, respectively.
Study protocol
Volunteer anaesthesia residents and nurse anaesthetists, with no previous specific training on laryngospasm and unaware of the scenario, were randomly paired to form anaesthesia teams. Each team was then allocated to the intervention or control group using a stratified cluster randomisation with a 1:1 allocation ratio. Groups were stratified according to the experience of the teams. ‘Junior teams’ included a Year 2–3 resident and a second-year student nurse anaesthetist, whereas ‘experienced teams’ included a Year 4–5 resident and a nurse anaesthetist certified for less than 5 yr and not working in paediatrics. The senior anaesthetist (absent from the scenario) was the only one to know the allocation group. Group allocation was concealed by a coding system (random number sequence), the key to which was disclosed only for the final analysis.
The intervention took place during the handover period, outside the operating theatre. The teams all took over from a single actor playing the senior anaesthetist (J. Picard), who had been previously trained to follow strict rules of verbal and non-verbal communication for this handover. While he transmitted similar standardised information during a similar 1 min period, he adopted different communication behaviour depending on the allocation group. Table 1 describes in detail how the handover was carried out in the two groups. After the handover, the scenario started and was video recorded using two cameras.
Primary endpoint: clinical team-based performance
The primary endpoint was overall team-based clinical performance in the scenario, assessed by an independent observer (P-MB) blinded to group allocation using video recordings and the previously developed scoring tool. The category-specific performance scores were also calculated.
Baseline data and secondary endpoints
The duration of crisis management, from occurrence of laryngospasm to authorisation given to resume the procedure, was measured. The proportion of teams that issued a call for help in a timely manner (i.e. before SpO2 fell to <80%) was examined. Heart rate variability was recorded to assess physiological stress response in each member of the anaesthesia team. Point-by-point HR was measured and recorded by a pectoral HR monitor (Smart Sensor®; Suunto, Vantaa, Finland) connected to a dedicated mobile software (CardioMood®; CardioMood, Moscow, Russia). Sympathetic activation in response to acute stress is associated with a decrease in HR variability, and thus in standard deviation normal to normal (sdnn).24 The sdnn was calculated for each participant over six relevant consecutive periods: at subjects' arrival (during 5 min), during handover (1 min), during the pre-crisis period of the scenario (2 min), during the crisis period (from 3 to 12 min), during debriefing (from 20 to 30 min), and at discharge (5 min) (Fig. 1). Psychological stress response was monitored by perceived level of stress (PLS; on a 0–100 VAS)25 at arrival, between handover and simulation, between simulation and debriefing, and at discharge (Fig. 1). Anxiety was assessed using a validated French version26 of the State-Trait Anxiety Inventory (STAI; 20–80 points).27 The STAI distinguishes the anxiety felt at a given time (state anxiety) from anxiety as part of one's personality (trait anxiety). State anxiety was measured at subjects' arrival and discharge (Fig. 1). Trait anxiety was measured 15 days before the simulation session, as well as basal stress level, using the French version28 of the Perceived Stress Scale (from 10 to 50 points).29
Fig 1.
Timeline of conduct of the study and distribution of the measurements. D-15, 15 days before intervention; PSS, perceived stress scale; sdnn, standard deviation normal to normal; STAI-S, State-Trait Anxiety Inventory-State anxiety; STAI-T, State-Trait Anxiety Inventory-Trait anxiety.
Statistical analysis
With the assumption that the mean (standard deviation [sd]) clinical-team-based performance score would increase from 45 (10)/100 points in the control group to 55 (10)/100 points in the intervention group, a 5% α risk, a 10% β risk, and a bilateral test, the total number of teams required was 32 (16 per group). All analyses were intention to treat and all statistical tests were bilateral. Analyses were performed with Stata 15® software (Timberlake, London, UK). A P-value ≤0.05 was considered significant.
The distribution of quantitative variable was studied by examining graphic representations (frequency histograms and QQ plots) and using Shapiro–Wilk's test. Data were then expressed as mean (sd) or median [25th to 75th percentiles], as appropriate. Student's t-test was used to compare team-based clinical performance scores between groups. Results were expressed in terms of absolute differences in scores and their 95% confidence intervals (95% CIs). Duration of crisis management was compared using Wilcoxon's test because of an extreme variable. Raw data from the pectoral HR monitor were recovered and analysed independently (none of the CardioMood software analyses were used). RR outliers presumed to be attributable to artifact were graphically eliminated blindly from the randomisation group and before any statistical analysis. The effect of intervention on sdnn and PLS over time was analysed using linear mixed-effects regressions.
Results
Study population
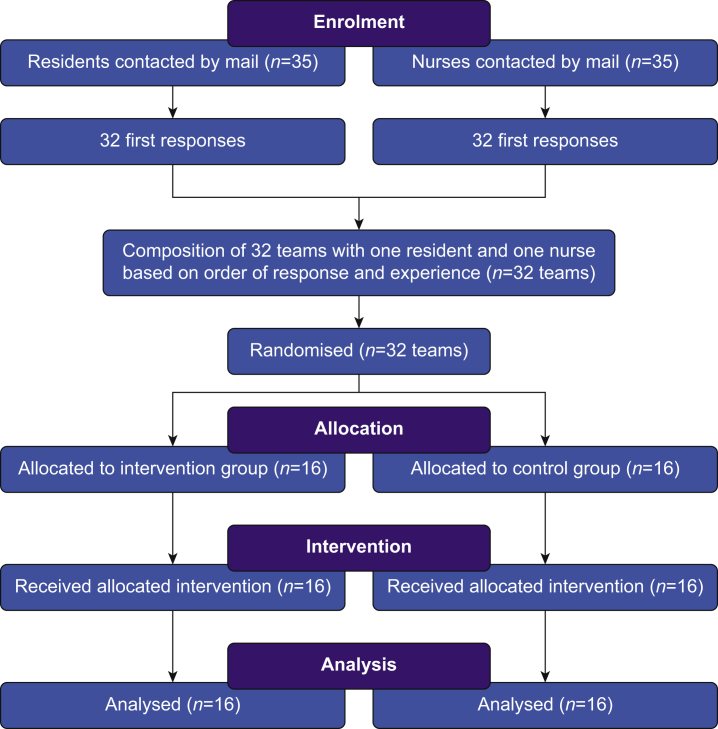
Between November 2017 and March 2018, 32 volunteer anaesthesia teams (64 subjects: 32 anaesthesia residents and 32 nurse anaesthetists) were enrolled and included in the analysis (16 pairs in each group; Fig. 2). Group characteristics and baseline stress levels are provided in Table 2. Participants were age 31 yr on average, 40% were women, and median [Q1–Q3] baseline state-anxiety score was 38 [33–45] (20–80 scale).
Fig 2.
Flow diagram. Based on Consolidated Standards of Reporting Trials guidelines.
Table 2.
Participant characteristics and baseline information.
| Control group |
Intervention group |
|||
|---|---|---|---|---|
| Resident (n=16) | Nurse (n=16) | Resident (n=16) | Nurse (n=16) | |
| Age (yr) | 29 [27–30] | 33 [30–38] | 29 [27–30] | 29 [29–34] |
| Experience (yr) | 4 [3–4]∗ | 2 [1–4]† | 4 [3–5]∗ | 2 [1–3]† |
| Women | 5 (31) | 6 (37) | 7 (44) | 7 (44) |
| Basal stress at D-15 | ||||
| STAI-T (20–80) | 42 [35–48] | 38 [33–46] | 37 [33–44] | 34 [31–44] |
| PSS (10–50) | 37 [31–40] | 32 [29–41] | 34 [30–38] | 27 [24–37] |
| Stress status at arrival | ||||
| STAI-S (20–80) | 36 [31–43] | 34 [30–39] | 35 [31–41] | 30 [25–33] |
| PLS (0–100 VAS) | 50 [35–56] | 35 [25–51] | 36 [28–50] | 46 [22–56] |
| sdnn (ms) |
63 [41–78] |
63 [53–77] |
65 [58–77] |
59 [44–65] |
|
Team (n=16) |
Team (n=16) |
|||
| Junior teams‡ | 7 (44) | 6 (38) | ||
| Previous work together | 4 (25) | 5 (31) | ||
| Mixed team (female–male) | 7 (44) | 8 (50) | ||
Data are median [Q1–Q3] or n (%). D-15, 15 days before intervention; PLS, perceived level of stress; PSS, perceived stress scale; sdnn, standard deviation normal to normal; STAI-S, State-Trait Anxiety Inventory-State anxiety; STAI-T, State-Trait Anxiety Inventory-Trait anxiety.
Since the beginning of residency.
Since the beginning of the nurse anaesthetist school.
Junior teams: a Year 2–3 resident and a second-year student nurse anaesthetist (experienced teams: a Year 4–5 resident and a certified nurse anaesthetist).
Primary outcome
Team-based clinical performance scores of the intervention and control groups are displayed in Fig. 3. Mean (sd) overall performance score in the intervention group (positive communication behaviour during handover) was 44 (10)/100 points vs 35 (12)/100 points in the control group (P=0.04; +8.4/100 points; 95% CI [0.4–16.4]). The effects were homogeneous over the three categories of tasks.
Fig 3.
(a) Overall and (b) category-specific team-based clinical performance scores. Box plots show, from bottom to top, minimum, 25th percentile (Q1), median, 75th percentile (Q3), and maximum values. Outliers (shown as points) are defined by values below Q1–1.5∗[Q1–Q3] or above Q3+1.5∗[Q1–Q3].
Secondary outcomes
The median durations of crisis management were 7 [6–8] and 8 [6–8] min in the intervention and control groups, respectively (P=0.6). A call for help was issued in a timely manner by 5/16 and 3/16 teams in the intervention and control groups, respectively (P=0.7). Psychological and physiological stress responses were lower in the intervention group, but no significant differences over time were shown in linear regression (PLS: –6 points; 95% CI [–13 to 2]; P=0.13; and sdnn: +4 ms; 95% CI [–3 to 10]; P=0.28; Fig. 4). Median PLS after handover was 44 [28–54]/100 in the intervention group vs 50 [43–60]/100 in the control group (–6 points; 95% CI [–13 to 1]; P=0.09). Median sdnn during crisis period was 58 [45–70] ms in the intervention group vs 52 [40–68] ms in the control group (+7 ms; 95% CI [–1 to 14]; P=0.09). Median state anxiety at discharge was 28 [26–30] in the intervention group and 30 [24–34] in the control group (P=0.29).
Fig 4.
(a) Psychological and (b) physiological stress response over time. Data presented in difference from basal values; sdnn in milliseconds; VAS on a scale of 100 points. Each point is represented with 25th percentile, median, and 75th percentile. sdnn, standard deviation normal to normal.
Discussion
In this randomised controlled simulation trial, positive communication behaviour between healthcare professionals during handover improved subsequent team-based clinical team-based performance in a subsequent simulated anaesthesia crisis. Although the category-specific performance scores were not significantly improved, all categories of expected tasks appear to have been affected homogeneously.
Other studies found concordant results on the strong implications of social interactions within healthcare teams on the clinical performance. Positive communication within professionals can be learned and may improve collegiality and teamwork.30 Gratitude has also been shown to improve both technical and non-technical clinical performance.31 In contrast, other research teams focused on the effect of negative communication behaviours, which might be very frequent.32 Incivility between healthcare professionals may harm clinical performance in critical anaesthesia situations.33 Similarly, patient or medical expert rudeness may have adverse consequences on both individual and team diagnostic and treatment performance.34,35
Positive communication behaviour during handover tended to decrease the overall psychological and physiological stress response (not statistically significant). Of note, handover causes an increase in stress response regardless of the communication behaviour. However, the subsequent crisis was associated with a decreased physiological stress response (sdnn increased) in the intervention group, whereas it increased (sdnn decreased) in the control group. The overall absence of significant effect of the intervention in linear regression analysis may be attributable to a lack of power (our data showed high inter- and intra-individual variabilities in PLS and sdnn). Another hypothesis is that rather than leading to an absolute decrease in stress response, positive communication behaviour may lead to a shift from negative to positive stress, promoting a sense of self-confidence, security, and social support amongst health professionals.15
Our study presents methodological strengths. The simulations were multi-professional, immersive, and realistic. Residual anxiety at discharge was low, suggesting that debriefing was effective, and the subjects' psychological safety was respected.36 Clinical performance was blindly assessed by an independent assessor using video recordings and a scenario-specific scoring tool. This tool encompasses both technical and non-technical skills, and provides a primary outcome that reflects clinical performance in a holistic manner. Evidence for its validity arises from its specific content (previous development process involving independent subject-matter experts and pilot test) and internal structure (inter-rater reliability previously confirmed after application in a sample of simulations). Of note, inter-rater reliability was only moderate (ICC=0.62) for the crisis resource management and non-technical skills category, which is consistent with reference tools currently in use.37
Our study suffers from several limitations. It was a single-centre study involving a small number of participants, and the protocol did not include a qualitative analysis. Mechanisms of action of positive communication could therefore not be explored in detail. Multicentre RCTs would partly bridge the gap, but mixed methods studies, including qualitative approaches, would probably be the most appropriate.38 Second, a delicate issue was the communication behaviour adopted during handover for the control group: our objective was indeed to show the benefit of positive communication behaviour, and not the drawback of negative communication behaviour. The communication behaviour of the senior anaesthetist with the control group was therefore intentionally close to real situations of fatigue or high stress, but without falling into caricature. Finally, this critical anaesthesia incident occurring just after handover was a somewhat contrived situation, and our findings cannot be extended to all possible critical situations in actual clinical practice.
Conclusions
Positive communication behaviour between healthcare professionals during medical handover may improve clinical team performance during a subsequent critical care situation. Our findings call for further evaluations to confirm this positive effect and to study the underlying mechanisms. Given its obvious safety, positive communication behaviour should be used in daily medical handover. Efforts and resources must be devoted to promoting its wide teaching and implementation, including by simulation, as we and others have shown to be effective.39
Authors' contributions
Study design: BB, J-NE, J-LB, PA, J. Picard
Participant recruitment: BB, J-NE, VL
Randomisation: J. Picard
Data acquisition: BB, J-NE, P-MB, VL, J. Picard
Interpretation of results: BB, J-NE, J. Piot, RW, J-LB, PA, J. Picard
Statistical analyses: HT
Writing first draft of paper: BB, J-NE, J-LB, J. Picard
Critical revision of paper for important intellectual content: J. Piot, RW, P-MB, PA
Final approval of the version to be published and agreement to be accountable for all aspects of the work, thereby ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: all authors
Acknowledgements
The authors thank P. Lafont and P. Romegoux for precious help in conducting the study, the Alps Research Assessment and Simulation Centre of the Grenoble Alpes University Hospital, and the CRNA School of the Grenoble Alpes University Hospital for their logistical support. The authors also thank the six experts who helped develop the scoring tool: C. Buleon, C. Dadure, M. Lilot, P. Roulleau, G. Savoldelli, and I. Tanoubi, and the residents and nurses for their participation.
Handling editor: Hugh C Hemmings Jr
Footnotes
This article is accompanied by an editorial: Normalising good communication in hospital teams by Weller & Webster, Br J Anaesth 2021:126:758–760, doi: 10.1016/j.bja.2020.12.036
Prior presentation: Annual Conference of the French Society of Anaesthesia and Intensive Care, September 2019, Paris, France.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.bja.2020.12.011.
Declarations of interest
The authors declare that they have no conflicts of interest.
Funding
Institutional funding
Appendix ASupplementary data
The following are the supplementary data related to this article:
Multimedia component 1
Multimedia component 2
References
- 1.Gaba D.M. Anaesthesiology as a model for patient safety in health care. BMJ. 2000;320:785–788. doi: 10.1136/bmj.320.7237.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flin R., Patey R., Glavin R., Maran N. Anaesthetists’ non-technical skills. Br J Anaesth. 2010;105:38–44. doi: 10.1093/bja/aeq134. [DOI] [PubMed] [Google Scholar]
- 3.Flin R. Identifying and training non-technical skills for teams in acute medicine. Qual Saf Health Care. 2004;13:i80–i84. doi: 10.1136/qshc.2004.009993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper S., Wakelam A. Leadership of resuscitation teams: ‘lighthouse leadership.’. Resuscitation. 1999;42:27–45. doi: 10.1016/s0300-9572(99)00080-5. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez Castelao E., Russo S.G., Cremer S. Positive impact of crisis resource management training on no-flow time and team member verbalisations during simulated cardiopulmonary resuscitation: a randomised controlled trial. Resuscitation. 2011;82:1338–1343. doi: 10.1016/j.resuscitation.2011.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Nagpal K., Arora S., Vats A. Failures in communication and information transfer across the surgical care pathway: interview study. BMJ Qual Saf. 2012;21:843–849. doi: 10.1136/bmjqs-2012-000886. [DOI] [PubMed] [Google Scholar]
- 7.Gillespie B.M., Chaboyer W., Fairweather N. Factors that influence the expected length of operation: results of a prospective study. BMJ Qual Saf. 2012;21:3–12. doi: 10.1136/bmjqs-2011-000169. [DOI] [PubMed] [Google Scholar]
- 8.Miller D., Crandall C., Washington C., McLaughlin S. Improving teamwork and communication in trauma care through in situ simulations. Acad Emerg Med. 2012;19:608–612. doi: 10.1111/j.1553-2712.2012.01354.x. [DOI] [PubMed] [Google Scholar]
- 9.Woloshynowych M., Davis R., Brown R., Vincent C. Communication patterns in a UK emergency department. Ann Emerg Med. 2007;50:407–413. doi: 10.1016/j.annemergmed.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Bergs E.A.G., Rutten F.L.P.A., Tadros T., Krijnen P., Schipper I.B. Communication during trauma resuscitation: do we know what is happening? Injury. 2005;36:905–911. doi: 10.1016/j.injury.2004.12.047. [DOI] [PubMed] [Google Scholar]
- 11.Moore A., Butt D., Ellis-Clarke J., Cartmill J. Linguistic analysis of verbal and non-verbal communication in the operating room. ANZ J Surg. 2010;80:925–929. doi: 10.1111/j.1445-2197.2010.05531.x. [DOI] [PubMed] [Google Scholar]
- 12.Smith A.F., Mishra K. Interaction between anaesthetists, their patients, and the anaesthesia team. Br J Anaesth. 2010;105:60–68. doi: 10.1093/bja/aeq132. [DOI] [PubMed] [Google Scholar]
- 13.Ruusuvuori J. Looking means listening: coordinating displays of engagement in doctor–patient interaction. Soc Sci Med. 2001;52:1093–1108. doi: 10.1016/s0277-9536(00)00227-6. [DOI] [PubMed] [Google Scholar]
- 14.Härgestam M., Hultin M., Brulin C., Jacobsson M. Trauma team leaders’ non-verbal communication: video registration during trauma team training. Scand J Trauma Resusc Emerg Med. 2016;24:37. doi: 10.1186/s13049-016-0230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LeBlanc V.R. The effects of acute stress on performance: implications for health professions education. Acad Med. 2009;84:S25–S33. doi: 10.1097/ACM.0b013e3181b37b8f. [DOI] [PubMed] [Google Scholar]
- 16.Hunziker S., Laschinger L., Portmann-Schwarz S., Semmer N.K., Tschan F., Marsch S. Perceived stress and team performance during a simulated resuscitation. Intensive Care Med. 2011;37:1473–1479. doi: 10.1007/s00134-011-2277-2. [DOI] [PubMed] [Google Scholar]
- 17.Harvey A., Bandiera G., Nathens A.B., LeBlanc V.R. Impact of stress on resident performance in simulated trauma scenarios. J Trauma Acute Care Surg. 2012;72:497–503. doi: 10.1097/ta.0b013e31821f84be. [DOI] [PubMed] [Google Scholar]
- 18.Bernard F., Musellec H. Arnette Edition; Paris: 2013. La Communication Dans Le Soin: hypnose Médicale et Techniques Relationnelles. [Google Scholar]
- 19.Kekecs Z., Varga K. Positive suggestion techniques in somatic medicine: a review of the empirical studies. Interv Med Appl Sci. 2013;5:101–111. doi: 10.1556/IMAS.5.2013.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Habre W., Disma N., Virag K. Incidence of severe critical events in pediatric anesthesia (APRICOT): a prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir Med. 2017;5:412–425. doi: 10.1016/S2213-2600(17)30116-9. [DOI] [PubMed] [Google Scholar]
- 21.Orliaguet G.A., Gall O., Savoldelli G.L., Couloigner V. Case scenario: perianesthetic management of laryngospasm in children. Anesthesiology. 2012;116:458–471. doi: 10.1097/ALN.0b013e318242aae9. [DOI] [PubMed] [Google Scholar]
- 22.Schulz K.F., Altman D.G., Moher D., CONSORT Group CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Der Sahakian G., Lecomte F., Buleon C., Guevara F., Jaffrelot M., Alinier G. 2018. Référentiel sur l’élaboration de scénarios de simulation en immersion clinique.https://sofrasims.org/wp-content/uploads/2019/10/R%C3%A9f%C3%A9rentiel-Scenario-Simulation-Sofrasims.pdf Available from: [Google Scholar]
- 24.Dobbs W.C., Fedewa M.V., MacDonald H.V. The accuracy of acquiring heart rate variability from portable devices: a systematic review and meta-analysis. Sports Med. 2019;49:417–435. doi: 10.1007/s40279-019-01061-5. [DOI] [PubMed] [Google Scholar]
- 25.Lesage F.-X., Berjot S., Deschamps F. Clinical stress assessment using a visual analogue scale. Occup Med. 2012;62:600–605. doi: 10.1093/occmed/kqs140. [DOI] [PubMed] [Google Scholar]
- 26.Spielberger C.D., Bruchon-Schweitzer M., Paulhan I. Editions du Centre de Psychologie Appliquée; Paris: 1993. Inventaire d’Anxiété état-trait forme Y (STAI-Y) [Google Scholar]
- 27.Spielberger C.D., Gorsuch R., Luschene R., Vagg P., Jacobs G. Consulting Psychologists Press; Palo Alto, CA: 1983. Manual for the state-trait anxiety inventory. [Google Scholar]
- 28.Lesage F.-X., Berjot S., Deschamps F. Psychometric properties of the French versions of the perceived stress scale. Int J Occup Med Environ Health. 2012;25:178–184. doi: 10.2478/S13382-012-0024-8. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 30.McCaffrey R., Hayes R.M., Cassell A., Miller-Reyes S., Donaldson A., Ferrell C. The effect of an educational programme on attitudes of nurses and medical residents towards the benefits of positive communication and collaboration. J Adv Nurs. 2012;68:293–301. doi: 10.1111/j.1365-2648.2011.05736.x. [DOI] [PubMed] [Google Scholar]
- 31.Riskin A., Bamberger P., Erez A. Expressions of gratitude and medical team performance. Pediatrics. 2019;143 doi: 10.1542/peds.2018-2043. [DOI] [PubMed] [Google Scholar]
- 32.Zhang S., Ma C., Meng D. Impact of workplace incivility in hospitals on the work ability, career expectations and job performance of Chinese nurses: a cross-sectional survey. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2018-021874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Katz D., Blasius K., Isaak R. Exposure to incivility hinders clinical performance in a simulated operative crisis. BMJ Qual Saf. 2019;28:750–757. doi: 10.1136/bmjqs-2019-009598. [DOI] [PubMed] [Google Scholar]
- 34.Riskin A., Erez A., Foulk T.A. Rudeness and medical team performance. Pediatrics. 2017;139 doi: 10.1542/peds.2016-2305. [DOI] [PubMed] [Google Scholar]
- 35.Riskin A., Erez A., Foulk T.A. The impact of rudeness on medical team performance: a randomized trial. Pediatrics. 2015;136:487–495. doi: 10.1542/peds.2015-1385. [DOI] [PubMed] [Google Scholar]
- 36.Evain J.N., Zoric L., Mattatia L. Residual anxiety after high fidelity simulation in anaesthesiology: an observational, prospective, pilot study. Anaesth Crit Care Pain Med. 2017;36:205–212. doi: 10.1016/j.accpm.2016.09.008. [DOI] [PubMed] [Google Scholar]
- 37.Boet S., Larrigan S., Martin L. Measuring non-technical skills of anaesthesiologists in the operating room: a systematic review of assessment tools and their measurement properties. Br J Anaesth. 2018;121:1218–1226. doi: 10.1016/j.bja.2018.07.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Webster C. Evidence and efficacy: time to think beyond the traditional randomised controlled trial in patient safety studies. Br J Anaesth. 2018;122:723–725. doi: 10.1016/j.bja.2019.02.023. [DOI] [PubMed] [Google Scholar]
- 39.Daly Guris R.J., Duarte S.S., Miller C.R., Schiavi A., Toy S. Training novice anaesthesiology trainees to speak up for patient safety. Br J Anaesth. 2019;122:767–775. doi: 10.1016/j.bja.2019.01.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1
Multimedia component 2