Supplemental Digital Content is available in the text.
Key Words: implementation science, health services research, qualitative research, stakeholder participation, rural health, veterans
Abstract
Background:
Rapid approaches to collecting and analyzing qualitative interview data can accelerate discovery timelines and intervention development while maintaining scientific rigor. We describe the application of these methods to a program designed to improve care coordination between the Veterans Health Administration (VHA) and community providers.
Methods:
Care coordination between VHA and community providers can be challenging in rural areas. The Telehealth-based Coordination of Non-VHA Care (TECNO Care) intervention was designed to improve care coordination among VHA and community providers. To ensure contextually appropriate implementation of TECNO Care, we conducted preimplementation interviews with veterans, VHA administrators, and VHA and community providers involved in community care. Using both a rapid approach and qualitative analysis, an interviewer and 1–2 note-taker(s) conducted interviews.
Results:
Over 5 months, 18 stakeholders were interviewed and we analyzed these data to identify how best to deliver TECNO Care. Responses relevant to improving care coordination include health system characteristics; target population; metrics and outcomes; challenges with the current system; and core components. Veterans who frequently visit VHA or community providers and are referred for additional services are at risk for poor outcomes and may benefit from additional care coordination. Using these data, we designed TECNO Care to include information on VHA services and processes, assist in the timely completion of referrals, and facilitate record sharing.
Conclusion:
Rapid qualitative analysis can inform near real-time intervention development and ensure relevant content creation while setting the stage for stakeholder buy-in. Rigorous and timely analyses support the delivery of contextually appropriate, efficient, high-value patient care.
The traditional health services research pipeline has been criticized for taking too long to transform knowledge into practice.1–3 Over the timeline required to plan, conduct, and analyze a clinical trial, funding priorities may change, health care policies evolve, and newer therapies and technologies are developed.4 Therefore, we must identify methods that improve the innovation timeline without sacrificing scientific rigor.
Rapid qualitative analysis is an applied method used to obtain actionable, targeted qualitative data on a shorter timeline than traditional qualitative methods.5–8 This pragmatic method follows accepted scientific practices, is rigorous, and facilitates the collection of readily applied qualitative data.5,9,10 Compared with traditional qualitative approaches, rapid qualitative analysis does not seek to provide a theoretically rich, in-depth understanding of a concept or phenomenon. Data collection and analysis aim to identify or broaden the understanding of key mechanisms, intervention elements, salient descriptors, or facilitators and barriers of a program to address time-sensitive research questions. This method is suitable when data collection targets (eg, deliverables, selection of interviewees) and processes (eg, interview protocols) are highly structured. Thus, rapid qualitative analysis processes may be one way to shorten the traditional research timeline by quickly identifying and addressing real-world challenges in a health care system.
Health services researchers embedded within a health system may be particularly well-positioned to conduct pertinent rapid qualitative analyses. These researchers lead projects that are of importance to the health system, are familiar with key stakeholders, and can incorporate stakeholder viewpoints to ensure the relevance of research11 in a dynamic health care environment with rapidly changing policies.12,13 A shorter research timeline enables embedded researchers to meet and immediately address real-world clinical and policy demand for improved health care delivery activities.
CONTEXT: EVOLVING POLICIES IMPACT HEALTH CARE DELIVERY AND HEALTH SERVICES RESEARCH
The Veterans Access, Choice, and Accountability Act of 2014 (Choice Act) was designed to improve veterans’ access to timely, high-quality health care by expanding the availability of medical services via agreements with community providers.14 Owing in part to the Choice Act’s rapid implementation timeline,15 veterans, Veterans Health Administration (VHA) clinical providers, and community providers experienced care coordination challenges.16–19 Suboptimal care coordination between VHA and community providers has led to care fragmentation,16–20 difficulties with care tracking,20 and redundant medication prescribing.15 In mid-2019, VHA implemented the Maintaining Internal Systems and Strengthening Integrated Outside Networks Act (MISSION Act) to expand the ability of veterans to obtain community-based care as a means of receiving timely, high-quality care.21
Given changing policies, pressing health care needs, and a desire to improve the care provided to veterans, reliance upon the traditional research timeline may delay efforts to address suboptimal care coordination. Incorporating feedback from veterans, as well as VHA and community providers, on a rapid timeline during the design of an intervention may be one way to improve the “fit” and usefulness of a coordinated care intervention.
Purpose
We describe a focused methodological approach using rapid qualitative analysis that facilitated the identification of evidence-based recommendations for intervention development and implementation while maintaining scientific rigor.
METHODS
We conducted a 12-month project, Telehealth-based Coordination of Non-VHA Care (TECNO Care), to address the challenges of suboptimal care coordination between VHA and community providers. This project was deemed nonresearch by the local Institutional Review Board. We followed verbal informed consent procedures with all interview respondents.
Framework
The Consolidated Framework for Implementation Research (CFIR)22 guided all project activities. CFIR consists of 5 domains,22 which operationalized for our project:
Intervention characteristics, core components of a program to improve care coordination among VHA and community providers.
Inner setting, contextual features of the VHA such as the administrative structure and processes that influence health care delivery and care coordination.
Outer setting, factors outside of the VHA which impact community care and implementation of a care coordination program.
Individual characteristics, characteristics of veterans and of VHA and community providers who will implement and use the care coordination intervention.
Implementation process, actions that veterans as well as VHA and community providers take to implement the care coordination program.
We used CFIR to inform data collection methods, sampling strategy, coding, analysis, and intervention refinement so that we could develop a contextually relevant and timely intervention.
Proposed Intervention
Draft Intervention
TECNO Care was designed to leverage VHA’s telehealth infrastructure to address current problems with VHA and community care coordination. On the basis of our expertise in developing interventions,23,24 we decided early on that we would use established care coordination approaches via community care home telehealth (CCHT) to facilitate communication between veterans, VHA providers, and community providers (Fig. 1). Specifically, TECNO Care would leverage CCHT resources in that: (1) it is delivered by existing VHA CCHT clinical staff who are already trained to provide care coordination services; (2) the note templates are based on existing CCHT note formats, though tailored to focus on VHA-community care coordination; and (3) it uses existing Veterans Affairs (VA) electronic health record infrastructure for all documentation and data tracking. However, many features were left to be determined by data collected during the interviews with stakeholders. Using CFIR as a guide, we identified 6 a priori areas of interest in which to obtain information as we designed TECNO Care:
How should we identify VHA sites in which to implement TECNO Care? [Inner setting]—We identified contextual factors and the ways in which TECNO Care could supplement current VHA programs addressing care coordination.
How should we identify community sites to which to apply TECNO Care? [Outer setting]—We obtained community providers’ motivation and ability to engage with TECNO Care.
Which are the “right” patients and disease conditions for TECNO Care? [Characteristics of individuals]—We defined which veterans and/or disease states would most benefit from TECNO Care.
What are the central care coordination tasks TECNO Care should address? [Intervention characteristics]—We ensured that TECNO Care was neither duplicative nor burdensome to those who would be delivering TECNO Care.
What are potential barriers and facilitators to VHA and community provider communication for TECNO Care? [Outer setting, Inner setting]—We identified optimal strategies for communication between home telehealth nurses and community providers.
What are the right metrics to assess TECNO Care’s effectiveness? [Process]—We identified which metrics should be followed to assess the program’s impact.
FIGURE 1.
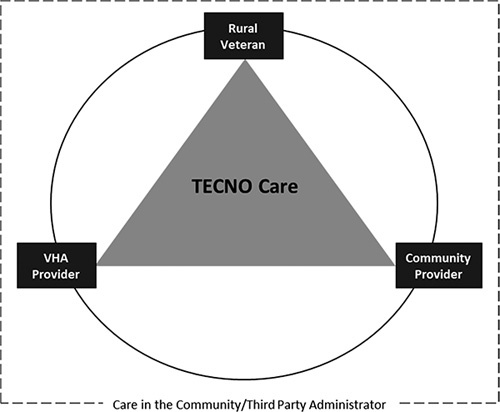
Conceptual framework of TECNO Care intervention. TECNO Care indicates Telehealth-based Coordination of Non-VHA Care; VHA, Veterans Health Administration.
Data Collection
Setting and Sample
All project activities occurred at a VHA in the Southeast US. We used a combination of purposive and snowball sampling to interview local VHA stakeholders (eg, administrators and clinicians) who either led or provided care to veterans. We used the electronic health record to identify community providers and veterans. Eligible community providers were those who had provided care to at least 10 veterans in the past year. Eligible veterans had to have obtained community care within the past year from one of the community-based providers we interviewed.
Interview Guide
Interview questions were informed by the a priori areas of interest described above. To guide question development in the interview guide, probing, and overall interview structure, we mapped interview questions to relevant CFIR domains and constructs (Table 1). Interview questions were open-ended and probes (“Tell me more,” “Please explain what you mean”) were used, as needed, to clarify interviewee responses.
TABLE 1.
Provider and Veteran Interview Questions (CFIR Domain and Related Construct)23
| VHA and community providers |
| Community care experiences |
| (1) What conditions or types of patients do you think require better care coordination between VHA and community providers? [Outer setting; patient needs and resources] |
| (2) Who are the key players inside your organization that we should talk with about TECNO? [Process; engaging] |
| (a) How about more broadly in the VHA? |
| (b) How about in the community? |
| (3) What types of community care (specific referrals or services) require better care coordination between VHA and community providers? [Inner setting; relative priority] |
| (4) What specific tasks should be addressed by a program designed to improve care coordination between VHA and community care? [Inner setting; relative priority] |
| (5) How would you know if a program designed to improve care coordination between VHA and community care were effective? [Intervention characteristics; relative advantage] |
| (a) What metrics would you follow to determine success? |
| Barriers and facilitators for TECNO Care |
| (1) Tell me about how the VHA currently oversees coordination with community care. [Intervention characteristics; relative advantage] |
| (a) How do you transfer and receive clinical data? |
| (b) How does the reimbursement system work? |
| (2) How well do you think the current system of VHA/community care coordination aligns with your patients’ needs? [Outer setting; patient needs and resources] |
| (a) What works well about that system or approach? |
| (b) What could be improved? |
| (3) When you think about a telehealth-delivered program to improve coordination between VHA and community care, what factors to do you see already in place to support such a program? [Inner setting; structural characteristics] |
| (a) What factors could or should be put in place? |
| (b) How does innovative technology factor into this system? |
| Barriers and facilitators for TECNO Implementation |
| (1) What challenges do you see in implementing a program like TECNO Care into routine practice at your facility? [Inner setting; readiness for change] |
| (2) What resources would make it easier to implement a program like TECNO Care into routine practice at your facility? How does innovative technology factor into this system? [Process, planning] |
| (3) Is there anything you can share about care coordination and the Veteran’s CHOICE Act that was not discussed? |
| Veterans |
| Barriers and facilitators for TECNO Care |
| (1) When you accessed medical care outside the VHA, what worked well? What did not work well? [Outer setting; patient needs and resources] |
| (2) When you accessed community-based care, how did VHA facilitate coordinating communication between VHA and community providers? [Outer setting; patient needs and resources] |
| (a) How did you or your VHA providers ensure that your community providers had the information that they needed to give you the best possible care? |
| (b) Did you have to deal with any bills? If so, how did the billing process work? |
| (3) Are you familiar with telehealth in the VHA? Have you used it and if so, what thoughts do you have about it? [Outer setting; patient needs and resources] |
| Barriers and facilitators for TECNO Implementation |
| (1) If there were a program designed to improve care coordination between VHA and community care, what things would be most important for it to address? [Characteristics of individuals; knowledge and beliefs about the intervention] |
| (2) If there were a program designed to improve care coordination between VHA and community care, how would you know if the program were working well? [Characteristics of individuals; knowledge and beliefs about the intervention] |
| (3) What would make it easier or more difficult for you to use a program designed to improve care coordination between VHA and community care? [Characteristics of individuals; individual identification with organization] |
CFIR indicates Consolidated Framework for Implementation Research; TECNO Care, Telehealth-based Coordination of Non-VHA Care; VHA, Veterans Health Administration.
Interview Structure
The interview team consisted of an interviewer and 1–2 note-taker(s). The interviewer followed the interview guide, and the note-taker(s) simultaneously took notes in a structured format based on our 6 a priori areas. Note-takers were permitted to ask questions during the interview to obtain clarification on a concept or statement.
Analysis Plan
We used rapid qualitative analysis with purposeful data reduction activities. While interviews were recorded, they were not transcribed. Two investigators met and reviewed all notes taken by the interviewer and note-taker(s) during interviews with VHA providers, community providers, and veterans. Informed by concepts in CFIR and a priori areas, these investigators used thematic analysis and the matrix method to identify main responses across all interviews and debrief notes.25–27 Rigor and validity were established by independently coding and assigning these data in the matrix and discussions with the larger team.
RESULTS
Sample and Timeline
Interviews were completed with VHA stakeholders (n=8; primary care and specialty physicians, administrators, operational leaders), community providers (n=5; primary care physicians and advanced practice providers), and veterans (n=5). Of the 5 veterans interviewed, the mean age was 70 years and 4 identified as male. We stopped interviewing new stakeholders when we achieved information saturation on care coordination.28 Interviews with VHA and community providers lasted between 20 and 25 minutes, and veteran interviews lasted between 15 and 20 minutes. All interviews were conducted over 3 months. Analyses were completed within 2 months of completion of the final interview, meaning that the entire qualitative data collection and analysis process was completed within 5 months.
Methodological Process Results
Our queries about whom to interview and rationale for conducting interviews at certain times were informed by our knowledge of VHA processes and infrastructure. We used our personal and clinical networks to initially identify VHA stakeholders to interview. We asked interviewees to suggest names of other VHA-affiliated individuals who oversaw, or were involved in, community care with whom we might speak. Interviewees were asked to send an email to individuals whose names they suggested to introduce the TECNO Care study and describe the purpose of an interview. Next, the primary investigator emailed that individual to introduce himself, further describe the study, and arrange an interview time. This approach to identifying interviewees ensured we did not “cold-contact” individuals and decreased the chances that interview requests would be ignored.
The interview process was iterative. Questions were reduced and/or changed according to responses received in prior interviews (Fig. 2). Intervention refinement began after the first interview and continued until the final interview. At each interview, after describing the emerging intervention, interviewees were asked to express how our intervention aligned with their work duties and schedule and whether the intervention, as described, addressed suboptimal care coordination. Detailed notes were taken during interviews, and debriefs were held immediately after each interview to enable the interview team to discuss common responses across interviews; identify areas upon which to gather more data, either through interviewing new stakeholders or reinterviewing stakeholders; and amend the interview guide over time to probe interviewees on emerging findings. In addition, interviewers discussed emerging patterns with the larger project team at biweekly meetings to ensure validity, rigor, and relevance to the study purpose. Discussions during the biweekly meetings served to contextualize emerging patterns and identify the need to interview additional stakeholders.
FIGURE 2.
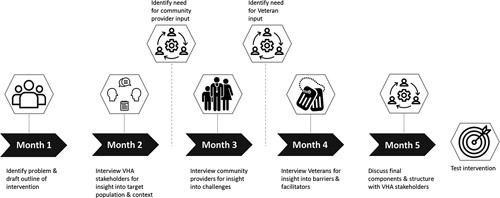
Timeline of activities from month 1 through month 5. VHA indicates Veterans Health Administration.
Responses
We identified expected and unexpected responses during analysis. Four responses were expected and addressed structural aspects of TECNO Care. Two responses were novel and addressed system-level and information needs. Due to our framework and structured questioning, these actionable findings could be directly and quickly applied to TECNO Care. We fully describe each response in Table 2 and describe how we used these findings to develop TECNO Care in Table 3.
TABLE 2.
Description of Identified Responses and Related CFIR Domain23
| Response | Description |
|---|---|
| Structural | |
| VHA context [Inner setting] | Capacity Number of clinicians to meet clinical need; limited physical space at facilities |
| Unique factors Communication among offices; differences among facilities within the VHA | |
| Veteran experience Preference for providers with knowledge of Veteran experience Convenience and continuity of care offered in VHA is a positive | |
| Medications Veterans can obtain medications at VHA pharmacies | |
| Target population [Intervention characteristics] | Illness-specific Patients with a chronic illness, frequent visits to VHA, special populations (eg, mental illness, physical therapy) or polypharmacy |
| Demographic-specific Rural veterans, veterans who obtain medications at VHA, or veterans with challenging social determinants of health | |
| Metrics and outcomes [Process] | Quality of care outcomes Strategic Analytics for Improvement and Learning (SAIL) or Healthcare Effectiveness Data and Information Set (HEDIS) Completed referrals, rehospitalizations |
| Patient-reported outcomes Satisfaction with care, access to care | |
| Core components of the intervention [Intervention characteristics] | Care coordination Facilitate referrals and medication refills and update providers about status Coordinate information sharing (medical records, laboratory/test results) among providers |
| Information sharing Provide information to community providers and veterans about VHA and community care program | |
| System-level | |
| Challenges with the current system [Inner setting] | General challenges Challenges identifying community providers in a timely fashion Confusion about community care processes Referral process for specialty care or medical services is confusing Billing procedures are not transparent |
| VHA-specific Identifying veterans who would benefit from community care is challenging Medical record sharing makes it challenging to re-engage veterans into VHA Care coordination staff are busy | |
| Information needs | |
| Additional observations [Characteristics of individuals] | Veteran-centered Provide timely and personalized care; facilitate continuity of care Provide education on telehealth and share that telehealth is supplementary to care, not a replacement |
Interview sample included: VHA stakeholders (n=8), community providers (n=5), and veterans (n=5).
CFIR indicates Consolidated Framework for Implementation Research; VHA, Veterans Health Administration.
TABLE 3.
TECNO Care Components and Structure
| Month and Activity | |||||
|---|---|---|---|---|---|
| Month 1 | Month 2 | Month 3 | Month 4 | Month 5 | |
| Area of Interest | Draft Intervention | VHA Interviews | Community Interviews | Veteran Interviews | Impact on Final Intervention |
| Fit in VHA | Area of interest How should we identify VHA and community sites in which to implement TECNO Care? | Finding High need for clinicians in the community and at VHA to meet the needs of veterans | Finding Challenges exist with record sharing, obtaining and completing referrals | Finding Veterans satisfied with providers, but have challenges with billing and medications | Outcome Involve stakeholders in implementation to ensure TECNO Care is a value add and contextually relevant as use of community care will increase TECNO Care can ensure community care processes are seamless |
| Action TECNO Care fits a need at VHA and can assist with care coordination for veterans | Action Community providers are unaware of how community care and/or VHA works | Action Veterans like the convenience and continuity of care offered in VHA | |||
| Question remaining What are the experiences of community providers with community care? | Question remaining What are the experiences of veterans using community care? | ||||
| Population | Area of interest Which are the “right” patients and disease conditions for TECNO Care? | Finding High-risk veterans with frequent visits or special populations (ie, rural, mental illness) are at risk for poor outcomes | Finding Community providers suggested veterans with polypharmacy and/or who need specialty services | Finding Veterans want care that addresses their medical needs completed in a timely fashion | Outcome Focus on high-risk veterans (eg, multiple comorbidities, polypharmacy, challenging social determinants of health) and those veterans who need referrals to specialty care, tests, or procedures Complete referrals and activities in a timely fashion and “close the loop” among all parties involved |
| Action TECNO Care may be most beneficial for high-risk veterans with many visits to providers | Action TECNO Care may be most beneficial for veterans who need referrals to other services | Action TECNO Care should facilitate the completion of referrals and medical care in a timely fashion | |||
| Question remaining What characteristics of veterans do community providers feel would benefit most from TECNO Care? | Question remaining What are the experiences of veterans with referrals and obtaining care in the community? | ||||
| Implementation process | Area of interest What are key barriers and facilitators to VHA and community provider communication for TECNO Care? | Finding There are opportunities to integrate TECNO Care into existing workflows using existing staffing, but staff effort is limited | Finding Minimal, if any, information is provided to community providers about VHA processes and how to use VHA services | Finding There is perceived discontinuity in communication between VHA and community providers | Outcome Examine person-time and effort for TECNO Care interventionist to determine how much time is needed for completion of TECNO Care Obtain feedback from VHA and community providers and Veteran during implementation to help identify problems |
| Action Design TECNO Care to be delivered in a way that complements existing care coordination efforts and with the minimal dose possible to facilitate coordination | Action Ensure that community providers are given tangible resources and information about who can address their questions | Action Consider what Veteran-specific care information can be shared from VHA to community providers to reduce asking veterans repeated questions | |||
| Question remaining What key pieces of information should be universally communicated to community providers about VHA? | Question remaining What is the best approach and timing for disseminating resources to community providers? | ||||
| Outcomes | Area of interest What are the right metrics to follow in assessing TECNO Care’s effectiveness? | Finding Outcome metrics (eg, SAIL, HEDIS) are important to VHA in determining operations | Finding Completion of referrals and obtaining information on the Veteran is challenging | Finding Veterans find obtaining information about community providers and test results challenging | Outcome Number of referrals and referral completion rate, health outcomes, hospitalizations Examine community provider and Veteran satisfaction with TECNO Care and care in the community program |
| Action Use patient-reported outcomes and metrics that are valuable to VHA stakeholders | Action Include a metric to assess referral completion and quality of record sharing | Action Examine patient-reported outcomes and satisfaction with community providers | |||
| Question remaining What outcomes and metrics are important to community providers? | Question remaining Are veterans satisfied with the care they receive from community providers? | ||||
| Interventionist and content delivered | Area of interest What are the central care coordination tasks TECNO Care should address? | Finding Timeliness of referrals and follow-up to understand when/which referrals have been completed Help identify providers in the community | Finding Information from the VHA can be delayed or incomplete Medication (re)fills and formulary information is particularly problematic | Finding It is disconcerting when VHA and community providers share incongruent information about resources and processes | Outcome Knowledge of VHA and community resources available to assist the Veteran Share information on VHA processes and procedures Serve as a point of contact for questions Educate veterans and community providers on VHA pharmacy procedures |
| Action Develop an approach to quickly identify veterans and/or referrals that need additional support | Action Provide resources and information about how to connect with VHA for Veteran-specific questions | Action Provide resources and information about how to connect with VHA for specific questions | |||
| Question remaining Can we predict “at-risk” referrals that should be prioritized for TECNO Care? | Question remaining What mode of delivery is most suitable to provide information about VHA processes? | ||||
HEDIS indicates Healthcare Effectiveness Data and Information Set; SAIL, Strategic Analytics for Improvement and Learning; TECNO Care, Telehealth-based Coordination of Non-VHA Care; VHA, Veterans Health Administration.
Structural Aspects
Structural aspects focused on discrete characteristics of VHA, the target population, metrics, and TECNO Care core components. When asked about VHA characteristics, respondents described the capacity of VHA to provide care and medication management, structural characteristics of VHA, and how veterans experience care within VHA and the community. One VHA provider described current care coordination processes, “For certain medical and surgical specialties, care coordination is not a need … as comprehensive authorization tends to cover a good amount … for other instances or diagnoses, it is more of a one-and-done type of authorization.” Another VHA provider commented, “we could look at where the biggest problem areas are in terms of volume of patients waiting a long time to receive community care services, in many cases, it has less to do with the patient population themselves, and more to do with the supply of providers for that specific disease condition.”
In regard to target population characteristics, respondents described disease-specific and demographic factors that influence VHA and community care coordination. When asked which patients are at risk for poor care coordination, one VHA provider first described the benefit of the VHA patient-aligned care team (PACT) in the context of patients who have complex health care needs (eg, comorbidities, polypharmacy, specialized care needs). He then stated, “[We should focus on] patients we send out to the community for primary care. If [a patient] gets primary care in the VA they have PACT … a whole team who can help coordinate the care and then send [the patient] to specialists. If you are out in the community, [patients] don’t have that.”
We queried respondents about metrics or outcomes that would ensure TECNO Care is providing relevant care coordination data to VHA stakeholders. One VHA provider described how access was important, “it is not just true access, meaning what percentage of our patients have visits within 30 days of their desired day. It is also patient perceptions of access.” Another VHA stakeholder stated examining the quality of care is important and described current challenges, “we want to make sure our patients are getting high-quality care … [describes metrics used in VHA], but I don’t know [these same statistics] for our providers in the community.”
Respondents commented on the core components of TECNO Care such as the specific aspects of care coordination on which to focus and where to allocate resources to ensure successful care coordination. In a second interview with a VHA provider, we reviewed what we learned from other interviews and described how TECNO Care could align with current VHA processes. The VHA provider stated, “That is the goal of trying to use the resources we have to have to focus on those conditions and those patients.” In addition, we described TECNO Care in interviews with community providers. In response to hearing about how TECNO Care would assist in care coordination, one community provider stated, “That is probably the biggest thing, just the outside referrals, I think that is the biggest need.”
System-level Challenges
Respondents described challenges with the current system, which included general lack of knowledge about community care and the referral process. One community provider stated, “I would say the number one challenge is referrals … it is confusing in regards to what we need authorizations for and what we do not need authorizations for.” Veterans echoed challenges experienced by community providers with referrals to receiving additional specialty care. When asked how to overcome challenges with community care, one Veteran stated, “accessing medical records, [community providers] … should have access to my past medical records.” Overall, veterans described obtaining community care was a positive experience because the providers were close and convenient.
Information Needs
We identified, additional observations, such as the need for timely information pertaining to care coordination processes and how to integrate this care with VHA care. One Veteran stated, “the [community provider] needs the same access that the VA primary care would provide [the patient] as far as setting up appointments [for referrals].” Overall, Veteran interviews were critical in refining the intervention to ensure that TECNO Care was beneficial to veterans as well as VHA and community providers.
DISCUSSION
The processes to develop TECNO Care facilitated the design of a contextually relevant and timely intervention to address suboptimal coordination between VHA and community providers. Moreover, rapid qualitative analysis facilitated the refinement of the intervention components to ensure alignment with the overall study purpose and VHA goals. Our research team leveraged our expertise in intervention development and conduct at VHA as well as our knowledge of the importance of stakeholder buy-in to the success and adoption of any program in determining our research approach. By interviewing veterans and VHA and community providers, we obtained key insights into challenges experienced in care coordination, and we began to build engagement and buy-in for our work to improve care coordination. In a search of published, peer-reviewed literature describing the rapid analysis, we identified the use of rapid analysis in process and summative evaluations of programs. However, we did not locate literature on the use rapid qualitative analysis in intervention development similar to the methods described in this manuscript. Our use of rapid qualitative analysis in intervention development adds to the literature because our rigorous and valid approach was guided by the CFIR framework, clearly articulated a priori areas of interest, targeted selection of key stakeholders to interview, continuous stakeholder feedback, immediate debriefs following each interview and routine research team discussions.
Rapid qualitative analysis is one way to develop contextually relevant interventions to time-sensitive problems and reduce research waste. Half of the research completed is never published, has avoidable design flaws, or does not align with health systems’ priorities.1 Once evidence is established, only one third of studies are implemented.2,3 Much of this delay relates to current research funding processes and traditional methodological approaches. The use of qualitative methods throughout the research process can bridge the research-to-practice gap by ensuring the “fit” of the research within the local context.5,6,29,30 Qualitative methods can help researchers develop interventions or programs, identify effective components within those interventions or programs, and determine when, how, where, and for whom the interventions or programs are most successful.29,31 Qualitative data can help ensure that the intervention provides a relative advantage over current practice, is feasible to implement, leverages the health system or community’s strengths, and is contextually appropriate.32,33 However, in a rapidly changing health care environment, traditional methods are not often equally rapid and thus become unsuitable as these traditional qualitative research methods may incompatible with rapidly changing health care delivery needs.5,6,32
Rapid qualitative analysis in the context of a framework-guided approach and a priori areas of interest facilitated the development of actionable evidence faster than traditional qualitative methods. For example, using operationalized definitions of CFIR domains and a priori areas of interest, we were able to capture the needs of the various stakeholders on a timeline that ensured that findings were still relevant when data collection ended. Our analytic approach, with targeted sampling and more structured questions, quickly identified challenges to care coordination and developed a useful, evidence-informed intervention that aligned with the Office of Rural Health VHA priorities. Importantly, we meaningfully refined our questions over time based upon CFIR domains; these changes occurred because we were explicit in the information we desired in our a priori areas of interest.
Our use of researchers familiar with the VHA enabled us to prioritize questions during the interviews to obtain targeted and actionable information on care coordination processes. Rapid approaches are pragmatic, follow accepted scientific practices, are rigorous, can be done in teams, and can use researchers and resources already within the health care system to focus the collection and analysis of data. However, challenges exist to using rapid qualitative analysis, as this method necessitates a clear understanding of the funder/stakeholder’s priorities, a grasp of the phenomenon of interest, and a need for less exploratory qualitative findings.
Innovative research methods that leverage the inherent strengths of qualitative approaches and data can inform the design, implementation, processes, feasibility, and acceptability of health services and implementation science research and interventions34; however, the use of in-depth qualitative research methods may not be appropriate, or equitable, for projects with shorter timelines, limited resources, and/or a need for more targeted data collection to refine interventions. For instance, qualitative research methods such as semistructured interviews or focus groups with key stakeholders, or observations of stakeholders, provide valuable insight into current values, priorities, and contextual factors that can influence or hinder an intervention. Obtaining stakeholder insight is critical to the success of efforts pertaining to data collection, analysis, and research resources.
Our rigorous and efficient analysis practices helped us align the intervention with current practice and VHA’s stated goals to improve care coordination. TECNO Care is currently being implemented at 3 VHA sites, and a future manuscript will describe outcomes (ie, care continuity, unique veterans served) and implementation data (eg, encounters completed, stakeholder and veteran interviews). Overall, rapid approaches, when guided by a framework and a priori areas of interest, can bridge the gap between the lengthy traditional research pipeline and the need for contextually relevant, timely solutions to current health care challenges,9 and they can be used in multiple settings and contexts, as long as the use of the method aligns with the research question and overall study purpose.5,9
Limitations
Several considerations of our approach should be acknowledged. First, all community providers were located in one geographic region of the state. Second, we interviewed veterans who had received care from 3 of the 5 community-based providers we interviewed. Due to our rapid timeline, and because our community providers and veteran interviewees expressed similar challenges with obtaining and/or providing community care, we did not pursue interviewing additional community providers and veterans. Future work should include additional input from diverse VHA and community providers, veterans, and veteran caregivers.
CONCLUSIONS
This manuscript describes how rapid qualitative analysis can elicit timely feedback to improve the fit and relevance of interventions and programs. This work illustrates: (1) the value and importance of using embedded researchers who are familiar with the health care system in which the intervention is to be used and (2) that vetting our intervention ideas with relevant stakeholders throughout intervention development helped to increase “fit” while setting the stage for stakeholder buy-in.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
ACKNOWLEDGMENTS
The authors thank Donnalee Frega, PhD, for editorial assistance and Eric Monson, PhD, for data visualization assistance.
Footnotes
Portions of this work was presented at the following conferences: VA HSR&D/QUERI National Conference, Washington, DC, from October 29 to 31, 2019 and the 12th Annual Conference on the Science of Dissemination and Implementation; Arlington, VA, from December 4 to 6, 2019.
Supported by the US Department of Veterans Affairs (VA) Office of Rural Health (VRHRC-IC #14416); the Department of Veterans Affairs Office of Academic Affiliations grant #TPH 21-000 (to A.A.L.); the Durham Center of Innovation to Accelerate Discovery and Practice Transformation grant #CIN 13-410 (to H.B.B., C.W.-C., M.J.C., A.A.L., F.A.M., L.L.Z.); HSR&D grants #16-213 (to M.J.C.), #08-027 (to H.B.B.); and the VA Office of Rural Health (to M.J.C.). Visit www.ruralhealth.va.gov to learn more. The content is solely the responsibility of the authors and does not necessarily reflect the position or policy of Duke University, the US Department of Veterans Affairs, or the US government.
H.B.B. reports receiving research funds from Sanofi, Otsuka, Johnson and Johnson, Improved Patient Outcomes, Novo Nordisk, PhRMA Foundation as well as consulting funds from Sanofi, Otsuka, Abbott, and Novartis. L.L.Z. reports receiving funding from the PhRMA Foundation and Proteus Digital Health as well as consulting funds from Novartis. A.A.L. reports receiving funding from Otsuka and the PhRMA Foundation. The remaining authors declare no conflicts of interest.
Contributor Information
Allison A. Lewinski, Email: allison.lewinski@duke.edu.
Matthew J. Crowley, Email: matthew.crowley@duke.edu.
Christopher Miller, Email: Christopher.Miller8@va.gov.
Hayden B. Bosworth, Email: boswo001@duke.edu.
George L. Jackson, Email: george.l.jackson@duke.edu.
Karen Steinhauser, Email: karen.steinhauser@duke.edu.
Courtney White-Clark, Email: Courtney.White-Clark@va.gov.
Felicia McCant, Email: Felicia.McCant@va.gov.
Leah L. Zullig, Email: leah.zullig@duke.edu.
REFERENCES
- 1.Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. 2009;374:86–89. [DOI] [PubMed] [Google Scholar]
- 2.Balas EA, Boren SA. Managing clinical knowledge for health care improvement. Yearb Med Inform. 2000;1:65–70. [PubMed] [Google Scholar]
- 3.Hanney SR, Castle-Clarke S, Grant J, et al. How long does biomedical research take? Studying the time taken between biomedical and health research and its translation into products, policy, and practice. Health Res Policy Syst. 2015;13:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer MS, Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. 2019;283:112376. [DOI] [PubMed] [Google Scholar]
- 5.Gale RC, Wu J, Erhardt T, et al. Comparison of rapid vs in-depth qualitative analytic methods from a process evaluation of academic detailing in the Veterans Health Administration. Implement Sci. 2019;14:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor B, Henshall C, Kenyon S, et al. Can rapid approaches to qualitative analysis deliver timely, valid findings to clinical leaders? A mixed methods study comparing rapid and thematic analysis. BMJ Open. 2018;8:e019993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Watkins DC. Rapid and rigorous qualitative data analysis: the “RADaR” technique for applied research. Int J Qual Methods. 2017;16:1609406917712131. [Google Scholar]
- 8.Brown-Johnson C, Safaeinili N, Zionts D, et al. The Stanford Lightning Report Method: a comparison of rapid qualitative synthesis results across four implementation evaluations. Learn Health Syst. 2020;4:e10210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamilton AB. Qualitative methods in rapid turn-around health services research. Health Services Research & Development Cyberseminar. 2013. Available at: https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=780. Accessed August 16, 2020.
- 10.Vindrola-Padros C, Vindrola-Padros B. Quick and dirty? A systematic review of the use of rapid ethnographies in healthcare organisation and delivery. BMJ Qual Saf. 2018;27:321–330. [DOI] [PubMed] [Google Scholar]
- 11.Forrest CB, Chesley FD, Jr, Tregear ML, et al. Development of the learning health system researcher core competencies. Health Serv Res. 2018;53:2615–2632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkins D, Kilbourne AM, Shulkin D. Moving from discovery to system-wide change: the role of research in a learning health care system: experience from three decades of health systems research in the Veterans Health Administration. Annu Rev Public Health. 2017;38:467–487. [DOI] [PubMed] [Google Scholar]
- 13.Kilbourne AM, Elwy AR, Sales AE, et al. Accelerating research impact in a learning health care system: VA’s Quality Enhancement Research Initiative in the Choice Act Era. Med Care. 2017;55(suppl 7 suppl 1):S4–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Veterans’ Access to Care through Choice, Accountability, and Transparency Act of 2014, H.R. 3230, 113th Cong. 2014. Available at: https://www.congress.gov/bill/113th-congress/house-bill/3230. Accessed August 16, 2020.
- 15.Gellad WF. The Veterans Choice Act and dual health system use. J Gen Intern Med. 2016;31:153–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones AL, Fine MJ, Stone RA, et al. Veteran satisfaction with early experiences of health care through the Veterans Choice Program: a concurrent mixed methods study. J Gen Intern Med. 2019;34:1925–1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tsai J, Yakovchenko V, Jones N, et al. “Where’s My Choice?” An examination of Veteran and provider experiences with hepatitis C treatment through the Veteran Affairs Choice Program. Med Care. 2017;55(suppl 7 suppl 1):S13–S19. [DOI] [PubMed] [Google Scholar]
- 18.Stroupe KT, Martinez R, Hogan TP, et al. Experiences with the Veterans’ Choice Program. J Gen Intern Med. 2019;34:2141–2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nevedal AL, Wagner TH, Ellerbe LS, et al. A qualitative study of primary care providers’ experiences with the Veterans Choice Program. J Gen Intern Med. 2019;34:598–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zuchowski JL, Chrystal JG, Hamilton AB, et al. Coordinating care across health care systems for veterans with gynecologic malignancies: a qualitative analysis. Med Care. 2017;55(suppl 7 suppl 1):S53–S60. [DOI] [PubMed] [Google Scholar]
- 21.US Department of Veterans Affairs. VA MISSION Act; 2019. Available at: https://missionact.va.gov/. Accessed November 13, 2019. [DOI] [PubMed]
- 22.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Darkins A, Ryan P, Kobb R, et al. Care Coordination/Home Telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed J E Health. 2008;14:1118–1126. [DOI] [PubMed] [Google Scholar]
- 24.US Department of Veterans Affairs. VA Telehealth; 2020. Available at: https://telehealth.va.gov/. Accessed August 25, 2020.
- 25.Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qual Health Res. 2002;12:855–866. [DOI] [PubMed] [Google Scholar]
- 28.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26:1753–1760. [DOI] [PubMed] [Google Scholar]
- 29.Hamilton AB, Finley EP. Reprint of: Qualitative methods in implementation research: an introduction. Psychiatry Res. 2020;283:112629. [DOI] [PubMed] [Google Scholar]
- 30.Finley EP, Huynh AK, Farmer MM, et al. Periodic reflections: a method of guided discussions for documenting implementation phenomena. BMC Med Res Methodol. 2018;18:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guerrero EG, Hahn EE, Khachikian T, et al. Interdisciplinary dissemination and implementation research to advance translational science: challenges and opportunities. J Clin Transl Sci. 2017;1:67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hamilton AB, Brunner J, Cain C, et al. Engaging multilevel stakeholders in an implementation trial of evidence-based quality improvement in VA women’s health primary care. Transl Behav Med. 2017;7:478–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davis K, Minckas N, Bond V, et al. Beyond interviews and focus groups: a framework for integrating innovative qualitative methods into randomised controlled trials of complex public health interventions. Trials. 2019;20:329–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


