Abstract
Multiple conditions such as drug rash, thromboembolism, sepsis, and heart failure can mimic differentiation syndrome; therefore, maintaining a high index of suspicion is important, as the prognosis is usually good if adequately treated.
Keywords: Differentiation syndrome, enasidenib, Sweet syndrome
Multiple conditions such as drug rash, thromboembolism, sepsis, and heart failure can mimic differentiation syndrome; therefore, maintaining a high index of suspicion is important, as the prognosis is usually good if adequately treated.
1. INTRODUCTION
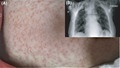
A 65‐year‐old woman was admitted to the hospital for the treatment of acute myeloid leukemia and was administered enasidenib and standard leukemia therapy. One week later, she developed a fever (102 F) and a generalized skin rash (Figure 1A); otherwise, her physical examination was normal.
FIGURE 1.

A, showing generalized papulovesicular skin rash on the anterior abdominal wall. B, showing chest X‐ray with evidence of bilateral diffuse interstitial lung infiltrates, no cardiomegaly
First, we considered that this rash could be secondary to infection, as she was neutropenic [absolute neutrophilic count (ANC)=0]. Therefore, she was administered cefepime and vancomycin. However, the next day, her rash worsened; she also complained of shortness of breath, and a chest X‐ray showed diffuse pulmonary infiltrates (Figure 1B). The ANC rapidly rose to 5, and the overall clinical picture became more suggestive of differentiation syndrome with Sweet syndrome.
She was administered dexamethasone and all symptoms improved. Importantly, a skin biopsy showed prominent edema in the superficial dermis with dense neutrophilic infiltration in the upper/mid‐dermis and endothelial swelling without evidence of vasculitis, consistent with Sweet syndrome.
Differentiation syndrome occurs in 20% of patients receiving isocitrate dehydrogenase inhibitors 1 and is sometimes associated with Sweet syndrome. The presentation can mimic drug rash, thromboembolism, infection, or heart failure, and the potential misdiagnosis may lead to death. Altogether, this clinical image highlights the need to maintain a high index of suspicion in the context of differential diagnosis, as the prognosis of Sweet syndrome with differentiation syndrome, if adequately treated, is usually good. 1 , 2
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
The author had been solely responsible for data collection and presentation.
ETHICAL APPROVAL
The patient gave us informed consent to publish the case, including publication of the images.
ACKNOWLEDGMENTS
Published with written consent of the patient.
Amr M. Enasidenib‐induced Sweet syndrome with differentiation syndrome. Clin Case Rep. 2021;9:e04099. 10.1002/ccr3.4099
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in Jama oncology and NEJM at https://doi.org/10.1001/jamaoncol.2017.4695 and https://doi.org/10.1056/NEJMoa1716984, respectively. Ref. [1, 2].
REFERENCES
- 1. Fathi AT, DiNardo CD, Kline I, et al. Differentiation syndrome associated with enasidenib, a selective inhibitor of mutant isocitrate dehydrogenase 2: analysis of a phase 1/2 study. JAMA Oncol. 2018;4(8):1106‐1110. 10.1001/jamaoncol.2017.4695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DiNardo CD, Stein EM, de Botton S, et al. Durable remissions with ivosidenib in IDH1‐mutated relapsed or refractory AML. N Engl J Med. 2018;378(25):2386‐2398. 10.1056/NEJMoa1716984 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available in Jama oncology and NEJM at https://doi.org/10.1001/jamaoncol.2017.4695 and https://doi.org/10.1056/NEJMoa1716984, respectively. Ref. [1, 2].


