Abstract
Background
Margin convergence has been shown to restore muscle tension in a cadaveric model of a rotator cuff tear. However, the clinical utility of this technique remains uncertain for patients with pseudoparalysis caused by an irreparable rotator cuff tear.
Questions/purposes
(1) For patients with massive irreparable rotator cuff tears, in what proportion of patients does margin convergence reverse pseudoparalysis? (2) In patients with massive irreparable rotator cuff tears, does margin convergence improve American Shoulder and Elbow Surgeons (ASES) scores? (3) What is the survivorship free from MRI evidence of retear after margin convergence?
Methods
Between 2000 and 2015, we treated 203 patients for pseudoparalysis with a rotator cuff tear. Pseudoparalysis was defined as active elevation less than 90° with no stiffness, which a physical therapist evaluated in the sitting position using a goniometer after subacromial injection of 10 cc lidocaine to eliminate pain. Of those, we considered patients who underwent at least 3 weeks of unsuccessful nonoperative treatment in our hospital as potentially eligible. Twenty-one percent (43 of 203) who either improved or were lost to follow-up within 3 weeks of nonoperative treatment were excluded. A further 12% (25 of 203) were excluded because of cervical palsy, axillary nerve palsy after dislocation or subluxation, and development of severe shoulder stiffness (passive shoulder elevation < 90°). Repair was the first-line treatment, but if tears were considered irreparable with the torn tendon unable to reach the original footprint after mobilizing the cuff during surgery, margin convergence was used. When margin convergence failed, the procedure was converted to hemiarthroplasty using a small humeral head to help complete the repair. Therefore, 21% (42 of 203) of patients treated with regular repair (18% [36 of 203]) or hemiarthroplasty (3% [6 of 203]) were excluded. That left 93 patients eligible for consideration. Of those, 13 patients were lost before the minimum study follow-up of 2 years or had incomplete datasets, and 86% (80 of 93) were analyzed (49 men and 31 women; mean age 68 ± 9 years; mean follow-up 26 ± 4 months). Seventy-six percent (61 of 80) were not evaluated in the last 5 years. We considered reversal of pseudoparalysis as our primary study outcome of interest; we defined this as greater than 90° active forward elevation; physical therapists in care measured this in the sitting position by using goniometers. Clinical outcomes were evaluated based on the ASES score from chart review, active ROM in the shoulder measured by the physical therapists, and the 8-month Kaplan-Meier survivorship free from MRI evidence of retear graded by the first author.
Results
Pseudoparalysis was reversed in 93% (74 of 80) patients, and improvement in ASES scores was observed at the final follow-up (preoperative 22 ± 10 to postoperative 62 ± 21, mean difference 40 [95% CI 35 to 45]; p < 0.01). The 8-month Kaplan-Meier survivorship free from MRI evidence of retear after surgery was 72% (95% CI 63% to 81%). There were no differences in clinical scores between patients with and without retears (intact ASES 64 ± 24, re-tear ASES 59 ± 10, mean difference 6 [95% CI -5 to 16]; p = 0.27).
Conclusion
Margin convergence can be a good option for treating patients with pseudoparalysis and irreparable rotator cuff tears despite the relatively high retear rates. The proportion of pseudoparalysis reversal was lower in patients with three-tendon involvement. Further studies will be needed to define the appropriate procedure in this group.
Level of Evidence
Level IV, therapeutic study.
Introduction
Rotator cuff tears may prevent some patients from elevating the arm to 90°, a phenomenon referred to as pseudoparalysis [10, 23, 24]. Surgery for patients with pseudoparalysis is generally satisfactory as long as the torn tendons can be completely repaired [6, 8]; however, pseudoparalysis associated with an irreparable massive tear is a challenging situation. Apart from reverse shoulder arthroplasty, many authors have reported surgical options, including partial repair, subacromial balloon, muscle transfer, patch augmentation, or superior capsule reconstruction [2, 16, 18, 21, 23]. All of these procedures have their own disadvantages, and which repair is the best option remains controversial. Margin convergence is a well-known technique to treat irreparable massive rotator cuff tears [5, 15], and its efficacy in restoring muscle tension for force transmission has been proven in a cadaveric model [11].
The concept of margin convergence could be an option for patients with pseudoparalysis caused by irreparable rotator cuff tears because it is not a technically demanding approach. As muscle degeneration is associated with irreversible retraction, we must examine whether the procedure can restore force to reverse pseudoparalysis in patients with irreparable tears. The clinical functional scores after this surgery should be examined in comparison with those of other alternatives. A high possibility of retear is expected in the tendon, which is likely to be poor quality. The retear risk in patients with chronic cuff tears and pseudoparalysis must be examined to better understand this phenomenon.
Therefore, we asked: (1) For patients with massive irreparable rotator cuff tears, in what proportion of patients does margin convergence reverse pseudoparalysis? (2) In patients with massive irreparable rotator cuff tears, does margin convergence improve functional scores? (3) What is the survivorship free from MRI evidence of retear after margin convergence?
Methods
Although the study included patients treated before it was approved by the board, each patient provided written informed consent before their surgery to be included in any treatment study.
Between 2000 and 2015, we treated 203 patients for pseudoparalysis with rotator cuff tear. Pseudoparalysis was defined as active elevation less than 90° with no stiffness, which a physical therapist evaluated in the sitting position using a goniometer after subacromial injection of 10 cc lidocaine to eliminate pain. Of those, we considered patients who had at least 3 weeks of unsuccessful nonoperative treatment in our hospital as eligible for margin convergence surgery. Twenty-one percent (43 of 203) of patients who either improved or were lost to follow-up within 3 weeks of nonoperative treatment were excluded. A further 12% (25 of 203) were excluded because of cervical palsy, axillary nerve palsy after dislocation or subluxation, and development of severe shoulder stiffness (passive shoulder elevation < 90°). Repair was the first-line treatment, but if tears were considered irreparable with the torn tendon unable to reach the original footprint after mobilizing the cuff during surgery, margin convergence was used. When margin convergence was unsuccessful, the procedure was converted to hemiarthroplasty using a small humeral head to help complete the repair. Therefore, 21% (42 of 203) of patients treated with regular repair (18% [36 of 203]) or hemiarthroplasty (3% [6 of 203]) were excluded, leaving 93 patients eligible for consideration. Of that, 13 patients were lost before the minimum study follow-up of 2 years or had incomplete datasets, and 86% (80 of 93) were analyzed (Fig. 1). Seventy-six percent (61 of 80) were not evaluated in the last 5 years.
Fig. 1.
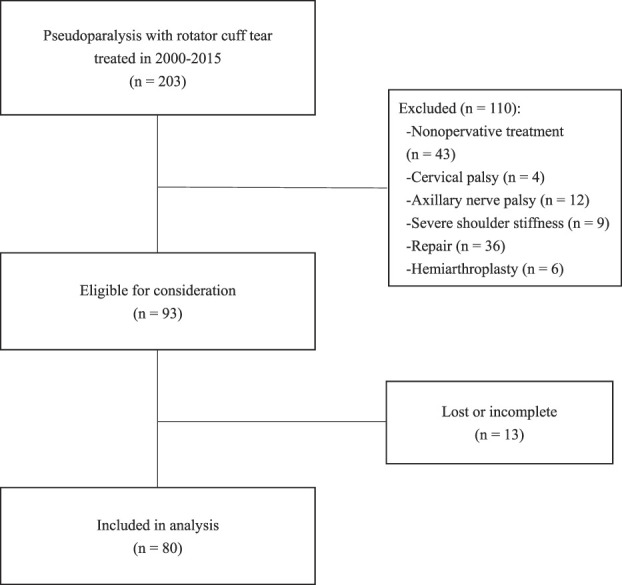
Flowchart of included and excluded patients.
Clinical Assessment
We obtained American Shoulder and Elbow Surgeons (ASES) scores and Japanese Orthopaedic Association (JOA) scores preoperatively and at the most recent follow-up. Shoulder elevation and external rotation were assessed under both active and passive conditions with the patient in the sitting position. These assessments were performed by senior physical therapists in care (none were authors) using large goniometers preoperatively and at the most recent follow-up.
Plain radiographs were evaluated preoperatively to determine the osteoarthritis stage based on the Hamada classification system [12]. In this system, Grade 1 is associated with minimal radiographic changes and Grade 2 is associated with narrowing of the subacromial space to less than 6 mm. Patients with Grade 3 osteoarthritis exhibit erosion and acetabulization of the acromion due to superior migration of the humeral head. Grade 4 and Grade 5 osteoarthritis are associated with glenohumeral arthritis and humeral head osteonecrosis, respectively. Acromiohumeral distance was measured on plain radiographs both preoperatively and at the final follow-up.
MRIs were performed using an open-type scanner (APERTO Eterna, Hitachi, Tokyo, Japan) before surgery and 6 ± 2 months after surgery. Fatty degeneration of the supraspinatus was evaluated on preoperative images using the grading system described by Goutallier et al. [9]. This system classifies fatty degeneration into the following five stages: Stage 0, completely normal muscle without any fatty streaks; Stage 1, muscle with some fatty streaks; Stage 2, increased fatty infiltration but still more muscle than fat; Stage 3, equal parts fat and muscle; and Stage 4, more fat than muscle. To evaluate repair integrity, each repaired rotator cuff was classified into one of five types in accordance with the system described by Sugaya et al. [22]: Type I, sufficient thickness with homogeneous low intensity (Fig. 2A); Type II, sufficient thickness with partial high intensity; Type III, insufficient thickness without discontinuity; Type IV, minor discontinuity in more than one slice; and Type V, major discontinuity (Fig. 2B). Type IV and Type V were regarded as retears. Tendon involvement was assessed on each operative recording.
Fig. 2.
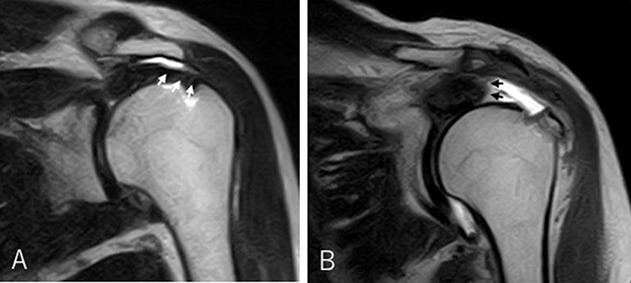
A-B (A) The tendon (white arrows) shows sufficient thickness with homogeneous low intensity (Type I Sugaya grade of retear), indicating that it is intact. (B) The tendon (black arrows) shows a discontinuity to the bone (Type V Sugaya grade of retear), indicating a retear.
All of the scoring systems of plain radiographs and MRIs (Hamada, including acromiohumeral distance, Goutallier stage, and Sugaya grade of retear) were evaluated by the first author (HI) before knowing their clinical results.
The mean time to follow-up was 26 ± 4 months. There were 49 men and 31 women, and the mean age was 68 ± 9 at the time of surgery (Table 1).
Table 1.
Patient demographics
| Pseudoparalysis | Number (n = 80) |
| Age in years, mean ±SD | 68 ± 9 |
| Gender, % (n) | |
| Men | 61 (49) |
| Women | 39 (31) |
| Mean symptom duration in weeks | 6 ± 14 |
| Torn tendons, % (n) | |
| SSP + ISP | 51 (41) |
| SSP + SC | 3 (2) |
| SSP + ISP + SC/TM | 46 (37) |
| Torn LHB tendon, % (n) | 19 (15) |
| Hamada grade, % (n) | |
| 1 | 13 (10) |
| 2 | 55 (44) |
| 3 | 26 (21) |
| 4a | 0 ( 0) |
| 4b | 6 ( 5) |
| 5 | 0 (0) |
| Goutallier stage, % (n) | |
| 0/1 | 0 ( 0) |
| 2 | 51 (41) |
| 3 | 35 (28) |
| 4 | 14 (11) |
SC = subscapularis; SSP = supraspinatus; ISP = infraspinatus; TM = teres minor; LHB = long head of the biceps brachii.
Surgical Procedure and Postoperative Management
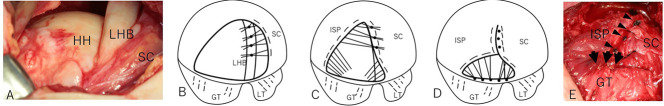
A mini-open approach that split the anterior deltoid was used with the patient in the beach chair position under general anesthesia. Adhesions around the rotator cuff and capsular contractures were thoroughly released from both the bursal and articular sides. Repair was the first-line treatment, but the margin convergence technique was used when the free tendon edge was unable to reach the original footprint after mobilizing the cuff tendon (Fig. 3A). If the long head of the biceps brachii (LHB) tendon was intact, the anterior side of the cuff was attached to it without tenotomy at its distal side (Fig. 3B). Side-to-side repair of the anterior and posterior rotator cuff was performed from the proximal site of the tear, and the free margin of the cuff converged toward the footprint (Fig. 3C). Pulling the humeral head downward may simplify side-to-side repair because the distance between the anterior and posterior tendons is relatively short, but when this side-to-side repair is impossible, we converted to hemiarthroplasty using a small humeral head to help complete the repair. Lastly, the lateral free edge was transosseously attached to the greater tuberosity (Fig. 3D), and coverage of the humeral head was completed (Fig. 3E).
Fig. 3.
A-E (A) An irreparable tear involving the supraspinatus and infraspinatus. Both tendons had retracted to the glenoid edge and cannot be seen in this figure. The subscapularis remained attached to the lesser tuberosity but appeared to displace anteroinferiorly. The long head of the biceps brachii was intact, running along the superior part of the humeral head. (B) The subscapularis is anchored to the long head of the biceps brachii. (C) The infraspinatus is sutured to the subscapularis augmented by the long head in a side-to-side manner from the proximal site of the tear. (D) The free lateral edge of the cuff is attached to the facet of the great tuberosity. (E) The humeral head was covered completely with the side-to-side stiches (arrow heads) and transosseous sutures (black arrows); HH = humeral head; LHB = long head of the biceps brachii; SC = subscapularis; GT = greater tuberosity; LT = lesser tuberosity; ISP = infraspinatus.
Postoperatively, the shoulder was kept in an abduction brace for 4 to 6 weeks. Each patient was supervised by a physical therapist. Patients began pendulum exercises and assisted ROM exercises within several days after surgery. Active exercises were started at 6 weeks. Strenuous intrinsic or extrinsic muscle training was initiated at 3 months, and all occupational or sports activities were permitted at 6 months.
Primary and Secondary Study Endpoints
We considered reversal of pseudoparalysis as our primary study outcome of interest; we defined this as greater than 90° active forward elevation, which physical therapists measured in the sitting position by using goniometers.
Our secondary endpoints of interest were improvement in ASES and survivorship free from MRI evidence of retear. Pre- and postoperative ASES scores at final follow-up were obtained from chart review, and the first author (HI) graded retears on MRI at approximately 6 months after surgery.
Ethical Approval
The study protocol was approved by the institutional review board of our hospital (No. J188).
Statistical Analysis
Data are presented as the mean ± SD. We compared findings between the retear and intact groups using unpaired t-tests and between the preoperative and postoperative settings using paired t-tests. Survivorship free from MRI evidence of retear was estimated using Kaplan-Meier analysis because 13 patients were lost prior to the minimum study follow-up or had incomplete datasets, and MRI was not always taken at the same period after surgery. The level of statistical significance was set to p < 0.05.
Results
Reversal of Pseudoparalysis
Postoperatively, pseudoparalysis was reversed in 93% (74 of 80) of patients. Three tendons (the supraspinatus, the infraspinatus, and the subscapularis or the supraspinatus, the infraspinatus, and the teres minor) were affected in all six patients with residual pseudoparalysis, all of whom also exhibited severe fatty degeneration (Stage 3 or 4) (Table 2). In total, the study included 46% (37 of 80) of patients with three affected tendons and 49% (39 of 80) of patients with severe fatty degeneration (35% [28 of 80] of patients had Stage 3 and 14% [11 of 80] of patients had Stage 4). Pseudoparalysis was reversed in 84% (31 of 37) of patients with three-tendon involvement and in 85% (33 of 39) of patients with severe fatty degeneration.
Table 2.
Patients with residual pseudoparalysis
| Patient | Age/gender | Torn tendons | LHB | Hamada grade | Goutallier stage |
| 1 | 76/woman | SC + SSP + ISP | + | 4b | 4 |
| 2 | 78/woman | SC + SSP + ISP | + | 3 | 3 |
| 3 | 71/man | SC + SSP + ISP | + | 2 | 4 |
| 4 | 79/woman | SSP + ISP + TM | - | 2 | 3 |
| 5 | 71/woman | SC + SSP + ISP | - | 4b | 4 |
| 6 | 76/man | SC + SSP + ISP | - | 2 | 4 |
SC = subscapularis; SSP = supraspinatus; ISP = infraspinatus; TM = teres minor; LHB = long head of the biceps brachii.
Outcomes Scores
Margin convergence improved ASES scores (preoperative 22 ± 10 to postoperative 62 ± 21, mean difference 40 [95% CI 35 to 45]; p < 0.01) (Table 3). Similarly, JOA scores improved (preoperative 47 ± 8 to postoperative 74 ± 10, mean difference 28 [95% CI 25 to 30]; p < 0.01). Active elevation also improved (preoperative 38° ± 20° to postoperative 110° ± 33°, mean difference 71° [95% CI 62° to 79°]; p < 0.01). However, there was no difference in active external rotation (preoperative 33° ± 23° to postoperative 35° ± 19°, mean difference 2° [95% CI -5° to 9°]; p = 0.54).
Table 3.
Pre- and postoperative shoulder scores and active ROM
| Shoulder scores and ROM | Preoperative | Postoperative | Mean difference (95% CI) | p value |
| ASES | 22 ± 10 | 62 ± 21 | 40 (35 to 45) | < 0.01 |
| JOA | 47 ± 8 | 74 ± 10 | 28 (25 to 30) | < 0.01 |
| Active elevation in degrees | 38 ± 20 | 110 ± 33 | 71 (62 to 79) | < 0.01 |
| Active ER in degrees | 33 ± 23 | 35 ± 19 | 2 (-5 to 9) | 0.54 |
ASES = American Shoulder and Elbow Surgeons; JOA = Japanese Orthopaedic Association; ER = external rotation.
There was no difference in acromiohumeral distance (preoperative 6.5 ± 2.8 mm to postoperative 6.7 ± 2.9 mm, mean difference 0.1 mm [95% CI -1.1 to 1.4]; p = 0.98).
Survivorship Free from Retear
The 8-month Kaplan-Meier survivorship free from MRI evidence of retear after surgery was 72% (95% CI 63% to 81%). All six patients with residual pseudoparalysis exhibited retears on postoperative MRI. Four of six patients could not gain any elevation. In these patients, follow-up radiographs revealed further superior migration of the humeral head. Pseudoparalysis was reversed in the remaining two patients until trauma occurred 6 to 12 months after the surgery, again impairing elevation. Patients with and without retears had no difference in outcome scores (intact ASES 64 ± 24, retear ASES 59 ± 10, mean difference 6 [95% CI -5 to 16]; p = 0.27).
Discussion
Pseudoparalysis associated with an irreparable tear is a challenging situation. Many authors have reported surgical options, but all of them are technically challenging, costly, or have their own disadvantages [2, 16, 18, 21, 23]. Margin convergence is an easy technique to decrease the gap size in massive rotator cuff tears with proximal side-to-side stitches [5, 15], and it could be a reasonable treatment option in this difficult-to-manage group of patients. The current study showed that margin convergence was effective in reversing pseudoparalysis with improved ASES scores in patients with pseudoparalysis and irreparable rotator cuff tears despite the relatively high retear rates.
Limitations
The present study has some limitations. First, the study included selection bias. After unsuccessful conservative treatment, we treated patients with pseudoparalysis with regular repair, margin convergence, or hemiarthroplasty with a small humeral head. The priority of the procedures was consistently in this order, but we must admit the inherent risk of surgeon bias. Second, the study included transfer bias. Fourteen percent (13 of 93) of patients were lost before 2 years of follow-up or had incomplete datasets. We confirmed from their medical records that all the lost patients had pseudoparalysis reversal after surgery, but we did not know whether their clinical courses were uneventful or not, which could change our results. In addition, most patients have not been evaluated in the last 5 years, and we cannot deny that they must have had problems that have gone unreported. Third, there was no control group for comparison. This means that we do not know whether our approach was better than available alternatives such as partial repair, subacromial balloon, muscle transfer, patch augmentation, or superior capsule reconstruction. However, margin convergence is a procedure with only the addition of several stitches to a regular repair. We thought it meaningful to show that the technique has the potential to treat patients with irreparable tears and pseudoparalysis. Lastly, assessor bias must be considered. In particular, all of the scoring systems (Hamada, including acromiohumeral distance, Goutallier, and Sugaya grading of retear) were evaluated by a single shoulder surgeon (the first author [HI]). This method of evaluation may be acceptable for the identification of full-thickness retears, which provided high interobserver reliability [14]; however, we must be careful using the data in others with less reliability [4, 20]. Although we used it to roughly identify patient characteristics in this study, our method of radiographic evaluation would be inadequate for future studies guiding treatment in special groups such as patients with residual pseudoparalysis.
Reversal of Pseudoparalysis
Margin convergence was useful in reversing pseudoparalysis in patients with massive rotator cuff tears. The success rate for pseudoparalysis reversal ranged from 76% to 90% after primary rotator cuff repair in patients with massive rotator cuff tears [8, 19]. Pseudoparalysis could be reversed after complete cuff repair, but reversal of pseudoparalysis with partial repair was reportedly not as predictable [6, 8]. Trials are also ongoing using balloon interposition arthroplasty to widen the acromial space to restore shoulder biomechanics, but the efficacy in reversing pseudoparalysis is uncertain [21]. Superior capsule reconstruction, which is a procedure using patch grafts, has recently gained popularity, and its reversal rate is 90% to 95% [7, 17]. Birmingham and Neviaser [3] achieved 100% reversal using latissimus dorsi transfer for failed rotator cuff repair, but Aoki et al. [1] reported 3 of 12 patients with postoperative elevation less than 90°, indicating that the procedure was not always effective. Despite its simple approach, margin convergence was compatible in the reversal of pseudoparalysis with technically demanding procedures that require graft harvesting or muscle advancement.
Outcomes Scores
In patients with massive rotator cuff tears, margin convergence improved functional outcome scores at 2 years. The improvement in ASES scores ranged from 43 to 47 in two studies on primary rotator cuff repair for massive tears causing pseudoparalysis [8, 19]. The improvement ranged from 37 to 56 in two studies on superior capsule reconstruction for patients with irreparable rotator cuff tears and pseudoparalysis [7, 17]. It ranged from 18 to 25 in two studies on latissimus dorsi transfer for irreparable rotator cuff repairs [3, 18]. The improvement in ASES scores in the current study was 40 points. We could not determine from improvement in ASES scores whether our procedure is superior to the other alternatives, but we may say that the procedure was a success because 96% (77 of 80) of patients had a more than 15-point improvement that was reportedly the minimal clinically important difference in shoulder surgery [13].
Survivorship Free from Retear
Although approximately one-third of patients may experience a retear, improvements in ASES scores remained the same between the groups with and without a retear at the final follow-up. The risk of retear was compatible with the study by Kim et al. [15], who reported on repair integrity after arthroscopic margin convergence in patients with massive tears. Kim’s study also showed that retears tended to be smaller than the original size despite the high retear rate. In patients who maintained arm elevation with favorable functional scores after retear, proximal side-to-side sutures might have remained intact, keeping the effect of margin convergence, although repair integrity at the insertion was affected.
Conclusion
Margin convergence can be a good option for treating patients with pseudoparalysis and irreparable rotator cuff tears despite the relatively high retear rates. The reversal rate of pseudoparalysis was lower in patients with three-tendon involvement. Further studies will be needed to define the appropriate procedure in this group.
Footnotes
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Ethical approval for this study was obtained from Institutional Review Board in Nobuhara Hospital and Institute of Biomechanics (No. J188).
References
- 1.Aoki M, Okamura K, Fukushima S, Takahashi T, Ogino T. Transfer of latissimus dorsi for irreparable rotator-cuff tears. J Bone Joint Surg Br. 1996;78:761-766. [PubMed] [Google Scholar]
- 2.Bailey JR, Kim C, Alentorn-Geli E, et al. Rotator cuff matrix augmentation and interposition: a systematic review and meta-analysis. Am J Sports Med. 2019;47:1496-1506. [DOI] [PubMed] [Google Scholar]
- 3.Birmingham PM, Neviaser RJ. Outcome of latissimus dorsi transfer as a salvage procedure for failed rotator cuff repair with loss of elevation. J Shoulder Elbow Surg. 2008;17:871-874. [DOI] [PubMed] [Google Scholar]
- 4.Brolin TJ, Updegrove GF, Horneff JG. Classifications in brief: Hamada classification of massive rotator cuff tears. Clin Orthop Relat Res. 2017;475:2819-2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burkhart SS, Athanasiou KA, Wirth MA. Margin convergence: a method of reducing strain in massive rotator cuff tears. Arthroscopy. 1996;12:335-338. [DOI] [PubMed] [Google Scholar]
- 6.Burkhart SS, Denard PJ, Adams CR, Brady PC, Hartzler RU. Arthroscopic superior capsular reconstruction for massive irreparable rotator cuff repair. Arthrosc Tech. 2016;5:e1407-e1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burkhart SS, Hartzler RU. Superior capsular reconstruction reverses profound pseudoparalysis in patients with irreparable rotator cuff tears and minimal or no glenohumeral arthritis. Arthroscopy. 2019;35:22-28. [DOI] [PubMed] [Google Scholar]
- 8.Denard PJ, Lädermann A, Brady PC, et al. Pseudoparalysis from a massive rotator cuff tear is reliably reversed with an arthroscopic rotator cuff repair in patients without preoperative glenohumeral arthritis. Am J Sports Med. 2015;43:2373-2378. [DOI] [PubMed] [Google Scholar]
- 9.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83. [PubMed] [Google Scholar]
- 10.Gschwend N, Ivosević-Radovanović D, Patte D. Rotator cuff tear-relationship between clinical and anatomopathological findings. Arch Orthop Trauma Surg. 1988;107:7-15. [DOI] [PubMed] [Google Scholar]
- 11.Halder AM, O'Driscoll SW, Heers G, et al. Biomechanical comparison of effects of supraspinatus tendon detachments, tendon defects, and muscle retractions. J Bone Joint Surg Am. 2002;84:780-785. [DOI] [PubMed] [Google Scholar]
- 12.Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Roentgenographic findings in massive rotator cuff tears. A long-term observation. Clin Orthop Relat Res. 1990;254:92-96. [PubMed] [Google Scholar]
- 13.Jones IA, Togashi R, Heckmann N, Vangsness CT, Jr. Minimal clinically important difference (MCID) for patient-reported shoulder outcomes. J Shoulder Elbow Surg. 2020;29:1484-1492. [DOI] [PubMed] [Google Scholar]
- 14.Khazzam M, Kuhn JE, Mulligan E, et al. Magnetic resonance imaging identification of rotator cuff retears after repair: interobserver and intraobserver agreement. Am J Sports Med. 2012;40:1722-1727. [DOI] [PubMed] [Google Scholar]
- 15.Kim KC, Shin HD, Cha SM, Kim JH. Repair integrity and functional outcomes for arthroscopic margin convergence of rotator cuff tears. J Bone Joint Surg Am. 2013;95:536-541. [DOI] [PubMed] [Google Scholar]
- 16.Makovicka JL, Chung AS, Patel KA, et al. Superior capsule reconstruction for irreparable rotator cuff tears: a systematic review of biomechanical and clinical outcomes by graft type. J Shoulder Elbow Surg. 2020;29:392-401. [DOI] [PubMed] [Google Scholar]
- 17.Mihata T, Lee TQ, Hasegawa A, et al. Arthroscopic superior capsule reconstruction can eliminate pseudoparalysis in patients with irreparable rotator cuff tears. Am J Sports Med. 2018;46:2707-2716. [DOI] [PubMed] [Google Scholar]
- 18.Namdari S, Voleti P, Baldwin K, Glaser D, Huffman GR. Latissimus dorsi tendon transfer for irreparable rotator cuff tears: a systematic review. J Bone Joint Surg Am. 2012;94:891-898. [DOI] [PubMed] [Google Scholar]
- 19.Oh JH, Kim SH, Shin SH, et al. Outcome of rotator cuff repair in large-to-massive tear with pseudoparalysis: a comparative study with propensity score matching. Am J Sports Med. 2011;39:1413-1420. [DOI] [PubMed] [Google Scholar]
- 20.Slabaugh MA, Friel NA, Karas V, et al. Interobserver and intraobserver reliability of the Goutallier classification using magnetic resonance imaging: proposal of a simplified classification system to increase reliability. Am J Sports Med. 2012;40:1728-1734. [DOI] [PubMed] [Google Scholar]
- 21.Stewart RK, Kaplin L, Parada SA, et al. Outcomes of subacromial balloon spacer implantation for massive and irreparable rotator cuff tears: a systematic review. Orthop J Sports Med. 2019;7:2325967119875717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953-960. [DOI] [PubMed] [Google Scholar]
- 23.Tokish JM, Alexander TC, Kissenberth MJ, Hawkins RJ. Pseudoparalysis: a systematic review of term definitions, treatment approaches, and outcomes of management techniques. J Shoulder Elbow Surg. 2017;26:e177-e187. [DOI] [PubMed] [Google Scholar]
- 24.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476-1486. [DOI] [PubMed] [Google Scholar]