Abstract
Background
Few studies have examined whether orthopaedic surgery, including hand surgery, is associated with patients’ financial health. We sought to understand the level of financial burden and worry for patients undergoing two common hand procedures—carpal tunnel release and open reduction and internal fixation for a distal radius fracture—as well as to determine factors associated with a higher financial burden and worry.
Questions/purposes
In patients undergoing operative treatment for isolated carpal tunnel syndrome with carpal tunnel release or open reduction and internal fixation for a distal radius fracture, we used validated financial burden and worry questionnaires to ask: (1) What percentage of patients report some level of financial burden, and what is the median financial burden composite score? (2) What percentage of patients report some level of financial worry, and what percentage of patients report a high level of financial worry? (3) When accounting for other assessed factors, what patient- and condition-related factors are associated with financial burden? (4) When accounting for other assessed factors, what patient- and condition-related factors are associated with high financial worry?
Methods
In this cross-sectional survey study, a hand and upper extremity database at a single tertiary academic medical center was reviewed for patients 18 years or older undergoing operative treatment in our hand and upper extremity division for an isolated distal radius fracture between October 2017 and October 2019. We then selected all patients undergoing carpal tunnel release during the first half of that time period (given the frequency of carpal tunnel syndrome, a 1-year period was sufficient to ensure comparable patient groups). A total of 645 patients were identified (carpal tunnel release: 60% [384 of 645 patients]; open reduction and internal fixation for a distal radius fracture: 40% [261 of 645 patients). Of the patients who underwent carpal tunnel release, 6% (24 of 384) were excluded because of associated injuries. Of the patients undergoing open reduction and internal fixation for a distal radius fracture, 4% (10 of 261) were excluded because of associated injuries. All remaining 611 patients were approached. Thirty-six percent (223 of 611; carpal tunnel release: 36% [128 of 360]; open reduction and internal fixation: 38% [95 of 251]) of patients ultimately completed two validated financial health surveys: the financial burden composite and financial worry questionnaires. Descriptive statistics were calculated to report the percentage of patients who had some level of financial burden and worry. Further, the median financial burden composite score was determined. The percentage of patients who reported a high level of financial worry was calculated. A forward stepwise regression model approach was used; thus, variables with p values < 0.10 in bivariate analysis were included in the final regression analyses to determine which patient- and condition-related factors were associated with financial burden or high financial worry, accounting for all other measured variables.
Results
The median financial burden composite score was 0 (range 0 [lowest possible financial burden] to 6 [highest possible financial burden]), and 13% of patients (30 of 223) reported a high level of financial worry. After controlling for potentially confounding variables like age, insurance type, and self-reported race, the number of dependents (regression coefficient 0.15 [95% CI 0.008 to 0.29]; p = 0.04) was associated with higher levels of financial burden, while retired employment status (regression coefficient -1.24 [95% CI -1.88 to -0.60]; p < 0.001) was associated with lower levels of financial burden. In addition, the number of dependents (odds ratio 1.77 [95% CI 1.21 to 2.61]; p = 0.004) and unable to work or disabled employment status (OR 3.76 [95% CI 1.25 to 11.28]; p = 0.02) were associated with increased odds of high financial worry.
Conclusion
A notable number of patients undergoing operative hand care for two common conditions reported some degree of financial burden and worry. Patients at higher risk of financial burden and/or worry may benefit from increased resources during their hand care journey, including social work consultation and financial counselors. This is especially true given the association between number of dependents and work status on financial burden and high financial worry. However, future research is needed to determine the return on investment of this resource utilization on patient clinical outcomes, overall quality of life, and well-being.
Level of Evidence
Level III, therapeutic study.
Introduction
Musculoskeletal conditions are the most common self-reported medical concerns among adults in the United States, with one of every two people reporting such a health issue [20]. Further, surgical care is expensive, and follow-up costs can be financially burdensome [17]. The unsustainable level of healthcare spending [3] and its associated costs have a number of negative impacts, one of which is the daily effect on patients. Across the United States, nearly half (45%) of the American public share concerns that a major health event could lead to personal bankruptcy [6]. Much of this concern is borne out in a recent National Health Interview Survey from the United States National Center for Health Statistics, which found that 1 in 5 patients were in families struggling to pay medical bills [5]. Therefore, given how common and expensive orthopaedic surgery is at large, it is reasonable to suspect that financial burden and worry would be a problem in this patient population.
To our knowledge, there are limited data examining whether orthopaedic surgery–related financial burden and worry occurs. One study examined patients with a wide range of traumatic musculoskeletal injuries and demonstrated high rates of financial worry and distress [2]. However, it remains unclear whether these findings are generalizable to all orthopaedic patient subgroups, including patients undergoing common hand procedures for traumatic or atraumatic conditions. Further, examining risk factors associated with financial burden and high financial worry in patients undergoing common hand procedures—such as carpal tunnel release or open reduction and internal fixation for a distal radius fracture—would possibly allow for more actionable steps to be taken to support such patients.
We therefore asked: (1) What percentage of patients report some level of financial burden, and what is the median financial burden composite score? (2) What percentage of patients report some level of financial worry, and what percentage of patients report a high level of financial worry? (3) When accounting for other assessed factors, what patient- and condition-related factors are associated with perceived financial burden? (4) When accounting for other assessed factors, what patient- and condition-related factors are associated with high financial worry?
Patients and Methods
Study Setting
We reviewed the hand and upper extremity database at one tertiary academic medical center to identify all patients 18 years or older undergoing operative treatment in our hand and upper extremity division for an isolated distal radius fracture between October 2017 and October 2019. We then selected all patients undergoing carpal tunnel release during the first half of that period (given the frequency of carpal tunnel syndrome, a 1-year period was sufficient to ensure comparable patient groups). All patients undergoing other or additional operative management for hand and wrist conditions were excluded.
Patients
A total of 645 patients were identified. Sixty percent of the patients (384 of 645) underwent carpal tunnel release for carpal tunnel syndrome, while 40% (261 of 645) underwent open reduction and internal fixation for a distal radius fracture. Based on a record review, 24 patients in the carpal tunnel release group and 10 patients in the open reduction and internal fixation for distal radius fracture groups were excluded because of associated injuries. A final sample of 611 possible patients (360 patients in the carpal tunnel release group; 251 patients in the open reduction and internal fixation for distal radius fracture group) formed the basis for this study.
All 611 eligible patients were contacted by mail to participate in the study and were subsequently approached by telephone to complete a set of two surveys. None of the researchers had been involved in the clinical care of any of the patients. When examining patient subgroups, there was no difference in the percentage of carpal tunnel release patients (36% [128 of 360]) and open reduction and internal fixation for distal radius fracture patients (38% [95 of 251]) who consented and completed both study surveys (p = 0.56). Overall, this led to the inclusion of 36% (223 of 611) of all patients who were contacted for the study.
Patients were contacted at a mean of 1.1 ± 0.5 years after their surgical intervention (Table 1). The mean age of our patient sample was 60 ± 15 years, and 74% (165 of 223) of the patients were women.
Table 1.
Patient characteristics (n = 223)
| Characteristic | Number |
| Surgical intervention | |
| Carpal tunnel release | 57 (128) |
| Open reduction and internal fixation for a distal radius fracture | 43 (95) |
| Survey follow-up time in years | 1.1 ± 0.5 |
| Age in years | 60 ± 15 |
| Gender, women | 74 (165) |
| Insurance type | |
| Private | 55 (123) |
| Medicare | 34 (76) |
| Medicaid | 3 (6) |
| Other | 8 (18) |
| Racea | |
| White | 68 (151) |
| Black | 9 (19) |
| Other or unknown | 24 (53) |
| Ethnicitya (n = 214) | |
| Non-Hispanic | 81 (174) |
| Hispanic | 19 (40) |
| Marital status | |
| Married | 58 (129) |
| Single | 26 (59) |
| Other | 16 (35) |
| Number of dependents | 0.54 ± 0.94 |
| Education level (n = 218) | |
| Some high school | 6 (13) |
| Completed high school | 26 (56) |
| Postsecondary education | 68 (149) |
| Employment status (n = 221) | |
| Full-time | 44 (97) |
| Part-time | 9 (20) |
| Unemployed | 6 (13) |
| Retired | 29 (64) |
| Unable to work or disabled | 12 (27) |
| Hand dominance (n = 219) | |
| Right | 88 (193) |
| Left | 12 (26) |
| Hand injured (n = 220) | |
| Right | 47 (104) |
| Left | 35 (77) |
| Both | 18 (39) |
| Prior loan? | |
| Yes | 16 (35) |
Results are presented as % (n) or mean ± SD.
Patient self-report.
Surveys
The surveys included two validated measures of personal financial hardship that have been used in studies on orthopaedic surgery [2, 16, 21] (see Appendix 1; Supplemental Digital Content 1, http://links.lww.com/CORR/A487). The financial burden composite score, a six-item survey scored from 0 to 6, with 6 representing the highest possible financial burden, was administered first. The second questionnaire was the dichotomized worry scale survey, where a 5-point Likert scale is transformed to a binary “high worry” or “low worry” designation. In this survey, “low worry” is indicated by a patient answering 1, 2, or 3 on the Likert scale; in contrast, “high worry” is indicated by a 4 or 5 on the Likert scale. Similar to a prior study on orthopaedic surgery [2], we recorded changes in discretionary and nondiscretionary spending.
In addition to operative treatment and questionnaire scores, the following patient- and condition-related characteristics were recorded: age (years), gender (men or women), insurance type (private, Medicare, Medicaid, or other), self-reported race (white, Black, or other), ethnicity (Hispanic or non-Hispanic), national Area Deprivation Index, marital status (married, single, or other), number of dependents, education level (some high school, completed high school, or postsecondary education), employment status (full-time, part-time, unemployed, retired, or unable to work or disabled [this includes those unable to work or disabled because of physical and/or mental health issues]), presence of prior loans (yes or no), hand dominance (right or left), and hand inured (right, left, or both).
Ethical Approval
This cross-sectional survey study was determined to be exempt by the Beth Israel Deaconess Medical Center institutional review board (CCI #2019P000900).
Statistical Analysis
We used a statistical approach that was similar to the approach used in previous studies that included these two questionnaires [2, 16, 18]. Overall descriptive statistics were calculated and reported, including the distribution of financial burden and worry. Bivariate analyses were also used to assess differences between patients who completed the two study surveys and those who did not to note any potential bias in our sample. These two patient groups were generally similar, limiting potential sampling bias (see Appendix 2; Supplemental Digital Content 2, http://links.lww.com/CORR/A488). We compared categorical variables using the chi-square or Fisher exact tests, and we compared continuous variables using t-tests or one-way ANOVA. We used Fisher exact tests when the cell being analyzed had fewer than five observations (that is, n < 5) [10].
To determine factors associated with an increased financial burden, we used a multivariable Poisson regression. To determine factors associated with high financial worry, we used a multivariable logistic regression analysis. To ensure that overfitting was minimized, we used a forward stepwise regression model approach [2]. Similar to prior studies, we included in the final regression model factors associated with the outcome of interest in the bivariate regression analysis at the p < 0.10 level [19]. The following factors were ultimately included in the financial burden composite score multivariable Poisson regression: age (years), insurance type (private, Medicare, Medicaid, or other), self-reported race (white, Black, or other), number of dependents, employment status (full-time, part-time, unemployed, retired, or unable to work or disabled), presence of prior loans (yes or no), and national Area Deprivation Index. The following factors were ultimately included in the high financial worry multivariable logistic regression: number of dependents, employment status (full-time, part-time, unemployed, retired, or unable to work or disabled), and presence of prior loans (yes or no).
For all analyses, significance was set a priori at p < 0.05. All statistical analyses were conducted using Stata/SE 14.2 for Mac (StataCorp, College Station, TX, USA).
Results
Overall Level of Financial Burden
Although 63% (141 of 223) of respondents denied having a financial burden related to surgical treatment for their condition, the remaining 37% (82 of 223) reported some level of financial burden. The median financial burden composite score was 0 (range, 0 [lowest possible financial burden] to 6 [highest possible financial burden]) (Fig. 1).
Fig. 1.
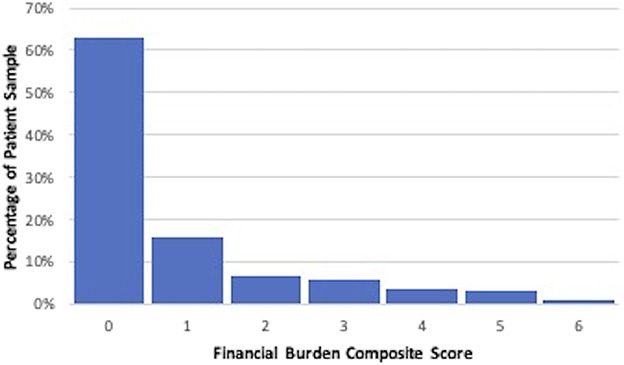
This bar graph shows the distribution of composite scores for financial burden. A score of 0 represents the lowest possible financial burden and a score of 6 represents the highest possible financial burden.
Overall Level of Financial Worry
Although 59% (131 of 223) of the respondents denied any level of financial worry associated with surgical treatment for their hand condition, the remaining 41% (92 of 223) reported some level of financial worry. When the score was dichotomized, 13% (30 of 223) of patients reported a high level of financial worry secondary to their hand surgery treatment (Fig. 2).
Fig. 2.
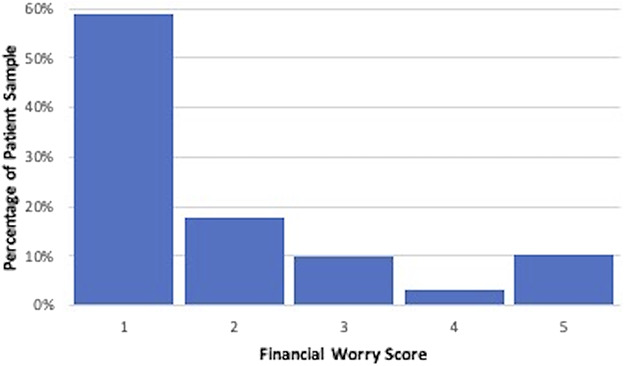
This bar graph shows the distribution of scores for financial worry. A score of 1 represents the lowest level of financial worry and a score of 5 represents the highest level of financial worry. In this figure, “low worry” is indicated by a patient answering 1, 2, or 3 on the Likert scale; in contrast, “high worry” is indicated by a 4 or 5 on the Likert scale.
Factors Associated with Financial Burden
After accounting for several key factors (age, insurance type, self-reported race, number of dependents, employment status, presence of prior loans, and national Area Deprivation Index), the number of dependents (regression coefficient 0.15 [95% CI 0.008 to 0.29]; p = 0.04) was associated with higher levels of financial burden, as measured by the financial burden composite score (Table 2). In contrast, retired employment status (regression coefficient -1.24 [95% CI -1.88 to -0.60]; p < 0.001) was associated with lower levels of financial burden, as measured by the financial burden composite score.
Table 2.
Multivariable models to determine factors associated with the composite score for financial burden and high financial worry
| Characteristic | Financial burden composite score | High financial worry | ||
| Regression coefficient (95% CI) | p value | OR (95% CI) | p value | |
| Age in years | -0.009 (-0.02 to 0.004) | 0.18 | ||
| Insurance type | ||||
| Private | Ref | |||
| Medicare | 0.34 (-0.002 to 0.68) | 0.05 | ||
| Medicaid | 0.52 (-0.19 to 1.24) | 0.15 | ||
| Other | 0.42 (-0.09 to 0.94) | 0.11 | ||
| Racea | ||||
| White | Ref | |||
| Black | 0.47 (-0.05 to 0.99) | 0.08 | ||
| Other or unknown | -0.15 (-0.55 to 0.24) | 0.45 | ||
| Number of dependents | 0.15 (0.008 to 0.29) | 0.04 | 1.77 (1.21 to 2.61) | 0.004 |
| Employment status | ||||
| Full-time | Ref | Ref | ||
| Part-time | 0.04 (-0.49 to 0.57) | 0.89 | 1.24 (0.29 to 5.32) | 0.77 |
| Unemployed | 0.45 (-0.05 to 0.95) | 0.08 | 3.47 (0.84 to 14.32) | 0.09 |
| Retired | -1.24 (-1.88 to -0.60) | < 0.001 | 0.43 (0.09 to 2.12) | 0.30 |
| Unable to work or disabled | 0.22 (-0.22 to 0.65) | 0.33 | 3.76 (1.25 to 11.28) | 0.02 |
| Prior loan | 0.17 (-0.20 to 0.55) | 0.37 | 1.89 (0.69 to 5.22) | 0.22 |
| National Area Deprivation Index | 0.0006 (-0.006 to 0.008) | 0.87 | ||
Patient self-report; ; OR = odds ratio.
Factors Associated with High Financial Worry
After accounting for several critical factors (number of dependents, employment status, and presence of prior loans), the number of dependents (odds ratio 1.77 [95% CI 1.21 to 2.61]; p = 0.004) and the employment status of unable to work or disabled (OR 3.76 [95% CI 1.25 to 11.28]; p = 0.02) were associated with increased odds of high financial worry (Table 2).
Discussion
Surgical care is expensive [7], accounting for more than 50% of Medicare expenditures [8]. Among surgical subspecialties, expenditures for hand surgery have grown at one of the fastest rates [8]. Further, despite insurance coverage, many patients face out-of-pocket expenses related to their orthopaedic care [1]. Prior research in orthopaedic trauma has demonstrated that patients with a wide range of traumatic musculoskeletal injuries have high rates of financial worry and distress [2]. However, it is unclear whether such findings are generalizable to specific orthopaedic subgroups, including hand patients undergoing common hand procedures for traumatic or atraumatic conditions. Further, factors associated with financial burden and high financial worry in such hand patients, which can help guide resource allocation, are unknown. In the present study, we found a notable number of patients undergoing operative hand care for two common conditions reported some degree of financial burden and worry. For example, having more dependents (such as having two dependents compared with one dependent) was associated with higher financial burden; number of dependents and being unable to work or disabled were two factors that were each associated with greater odds of high financial worry.
Limitations
Our study has several limitations. First, our patient sample comes from a hand clinic at a single, urban academic medical center. Thus, our findings may be most generalizable to similar clinical settings but not to more rural and/or community-based hospitals or health systems. Hand surgeons in more rural and/or community-based hospitals or health systems should seek to compare our patient sample characteristics to their patient populations to better determine whether our findings may be applicable. Second, our response proportion was 36%. Two prior studies evaluating financial burden reported response proportions of 32% and 60.1% [2, 4]; thus, our response proportion fits within this previously acceptable range. Further, there was no difference in response rates between patients undergoing a carpal tunnel release compared with an open reduction and internal fixation for a distal radius fracture. Additionally, those who did and did not respond to our survey requests were generally similar across baseline patient characteristics (see Appendix 2; Supplemental Digital Content 2, http://links.lww.com/CORR/A488). Therefore, we believe our sample represents our patient population at large. Third, our study focused on patients who underwent operative treatment of only two hand conditions (carpal tunnel syndrome and distal radius fracture). The level of financial burden and worry experienced by patients undergoing these two procedures may not represent that of all patients with hand conditions undergoing surgery. However, by including both a traumatic and atraumatic condition, we believe our findings are more generalizable overall across a greater number of hand conditions than if we just included one of them. Fourth, patients may have completed questionnaires with a bias to underreport or overreport their financial burden and worry. In addition, the consistent order of survey completion—financial burden composite score followed by the dichotomized worry scale survey—may also introduce bias in how patients report their financial distress. However, as noted in other studies, the direction of bias is unknown, and these validated surveys have been successfully used in the past [2]. Fifth, our study did not evaluate surgical outcomes, including patient-reported outcome measures. It is plausible that complications may affect our findings, as poor clinical outcomes may require additional operative or nonoperative treatment; this could lead to greater levels of financial burden and high financial worry. Although our dataset did not allow for evaluation of clinical outcomes, complication rates for carpal tunnel release and open reduction and internal fixation for distal radius fractures tend to be quite low. Nonetheless, future work can build on our findings to evaluate whether financial burden and high financial worry are associated with clinical outcomes. Lastly, our results may be impacted by recall bias because patients were contacted at a mean of about 1 year postoperatively. We feel it is crucial to evaluate the full level of financial distress once all insurance processes are finalized and the patient can reflect on her complete or near complete recovery experience instead of in the midst of ongoing clinical and/or financial challenges, as this may also bias findings. Further, because the effect of possible financial strain related to healthcare costs may persist for some time, we believe it is unlikely that those who truly had a measurable financial burden or worry early on in their postoperative recovery process did not accurately report it.
Overall Level of Financial Burden
In the present study, nearly 40% of patients reported some level of financial burden. However, the median financial burden composite score was 0 (range, 0 [lowest possible financial burden] to 6 [highest possible financial burden]), indicating that the overall financial worry among patients with upper extremity injuries was relatively low. Previous research evaluating patients with a wide range of orthopaedic traumatic injuries found relatively high levels of financial burden compared with the present study [2]. We believe the driving difference between our findings and prior results is the extent of the injury. Although a distal radius fracture can be debilitating, it may not require patients to take time off from work as frequently as patients experiencing other, more extensive traumatic injuries (such as polytraumas). This is especially true for individuals who do not have jobs requiring notable manual labor. Further, depending on a patient’s profession, carpal tunnel release may not require any time off from work. Prior research has shown that moderate-to-severe traumatic injuries are associated with patient well-being and return to work [14, 15]. Therefore, financial burden may be associated not only with certain patient characteristics before injury but also with the resulting effect on employment after treatment. Hand surgeons may benefit from considering a patient’s career preoperatively, whenever possible, and seeking assistance from support services such as social work and financial counseling throughout the care process to try to minimize financial burden for patients as much as possible.
Overall Level of Financial Worry
Although 41% of our patient sample reported some level of financial worry, only 13% of patients reported high financial worry resulting from their care. Similar to our financial burden findings, these results are lower than prior research evaluating financial worry levels in patients undergoing care for musculoskeletal trauma [2]. Again, we believe this may be most related to the severity of injury or condition and the subsequent inability to return to work that differs between a carpal tunnel release or isolated open reduction and internal fixation for a distal radius fracture compared with major musculoskeletal trauma or polytrauma. Indeed, even when comparing patients with isolated distal radius fractures to isolated calcaneus fractures, those with isolated calcaneus fractures missed more days from work [12]. Therefore, we feel it is reasonable to assume that even more complex or severe trauma, such as a femoral shaft fracture or periprosthetic fracture, would lead to even more days off from work, increasing the possibility of greater financial worry. We suspect, as we did for our financial burden findings, that the use of vital health system support services such as social work and financial counseling may benefit patients at risk for higher levels of financial worry. However, future research is warranted to determine how best to use these limited, but invaluable, services. Through additional research, it would also be of value to better understand whether the use of such resources leads to better clinical outcomes, especially in populations at risk for high financial worry.
Factors Associated with Financial Burden
We found that having more dependents is associated with greater perceived financial burden, while being retired is associated with lower perceived financial burden. The number of dependents associated with financial burden is likely because of added strain of caring for another person during the recovery period with more-limited financial resources. The fact that retired patients have less financial burden may be related to their ability to use retirement funds, if needed, to supplement insurance coverage. Additionally, this finding may further be explained as retirees have a known consistent stream of monthly income via Social Security, in addition to Medicare coverage, that is present without the need to return to work. Interestingly, we did not find an association between the insurance type and financial burden, while Bhashyam et al. [2] reported such a link. We speculate that our findings support the idea that an increased financial burden is a result of the quality of the type of insurance coverage, rather than access to that type of insurance. For example, all private health insurance plans are not the same in terms of coverage quality. This is a shared sentiment in a cardiovascular study by Khera et al. [9], which found high levels of financial burden across all types of insurance coverage. Overall, discussions with patients about their home and employment situations may be beneficial in determining which patients may need additional support postoperatively from other members of the overall care team (for example, social work). Having this knowledge about patients preoperatively may accelerate the support received postoperatively by allowing for early consult placement and general planning; however, the possible clinical benefits to this are yet to be determined and area ripe for future research.
Factors Associated with High Financial Worry
We found the number of dependents and being unable to work/having a disability were associated with increased odds of high financial worry. Similar to the above, we believe that a greater number of dependents may lead to added financial concern for patients because any savings or other funds available for necessities (such as food) may need to be stretched further. In addition, notable health disparities exist among patients with disabilities [11]. The US Surgeon General has recognized these inequities in a call to action and urges healthcare professionals to actively participate in providing care for these patients [13]. Thus, similar to our recommendation regarding our financial burden findings, our high financial worry insights may help guide resource allocation of vital support services, such as social work and financial counseling, to these vulnerable patient populations both pre- and postoperatively. The impact of these services in this setting remains unknown, but we suggest that it could improve clinical outcomes and holistic well-being by reducing stress associated with high financial worry. However, such research is needed to confirm or refute this theory.
Conclusion
Surgery for carpal tunnel syndrome or a distal radius fracture may directly, and successfully, address the underlying hand pathology causing issues for a patient; however, there are other considerations that hand surgeons should consider to a patient’s overall recovery and general well-being. In the present study, we found that a notable number of patients undergoing operative hand care for two common conditions (carpal tunnel syndrome and distal radius fracture) reported some degree of financial burden and high financial worry. This was independent of insurance type or whether the surgery was planned or unplanned. We noted that the number of dependents was associated with higher personal financial burden. Additionally, we identified patients at a particularly high risk of financial worry, including those who are disabled and those with a larger number of dependents. We believe these patients require additional discussion and screening for potential financial hardship to maximize available resources for their support. Indeed, we suggest having these patients meet with a social worker and/or financial counselor preoperatively. If possible, a detailed list of expected out-of-pocket expenses and time off from work associated with a given procedure would be of value as well. Future research is warranted to determine the best way to utilize such resources as well as their impact—positive, negative, or neutral—on clinical outcomes and patient well-being. Lastly, it will be important to verify that our findings are consistent across other orthopaedic conditions and procedures.
Supplementary Material
Footnotes
One of the authors certifies that he (DNB), or a member of his immediate family, has received or may receive payments or benefits, during the study period, in an amount of less than USD 10,000 from Horizon Therapeutics and in an amount of USD 10,000 to USD 100,000 from the Institute for Strategy and Competitiveness at Harvard Business School, outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
This study was determined to be exempt by the Beth Israel Deaconess Medical Center institutional review board (CCI #2019P000900).
References
- 1.Amanatullah DF, Murasko MJ, Chona DV, Crijns TJ, Ring D, Kamal RN. Financial distress and discussing the cost of total joint arthroplasty. J Arthroplasty. 2018;33:3394-3397. [DOI] [PubMed] [Google Scholar]
- 2.Bhashyam AR, McGovern MM, Mueller T, Heng M, Harris MB, Weaver MJ. The personal financial burden associated with musculoskeletal trauma. J Bone Joint Surg Am. 2019;101:1245-1252. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. National Health Expenditure Data. 2019. Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData. Accessed April 20, 2020.
- 4.Chino F, Peppercorn J, Taylor DH, Jr, et al. Self-reported financial burden and satisfaction with care among patients with cancer. Oncologist. 2014;19:414-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cohen RA, Kirzinger WK. Financial burden of medical care: a family perspective. NCHS Data Brief. 2014:1-8. [PubMed] [Google Scholar]
- 6.Ellrich M, Stevens L. Americans fear personal and national healthcare cost crisis. Available at: https://news.gallup.com/opinion/gallup/248108/americans-fear-personal-national-healthcare-cost-crisis.aspx. Accessed April 20, 2020.
- 7.Hollingsworth JM, Oerline MK, Ellimoottil C, Herrel LA, Hollenbeck BK. Effects of the Medicare Modernization Act on spending for outpatient surgery. Health Serv Res. 2018;53(suppl 1):2858-2869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaye DR, Luckenbaugh AN, Oerline M, et al. Understanding the costs associated with surgical care delivery in the Medicare population. Ann Surg. 2020;271:23-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khera R, Valero-Elizondo J, Okunrintemi V, et al. Association of put-of-pocket annual health expenditures with financial hardship in low-income adults with atherosclerotic cardiovascular disease in the United States. JAMA Cardiol. 2018;3:729-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim HY. Statistical notes for clinical researchers: chi-squared test and Fisher's exact test. Restor Dent Endod. 2017;42:152-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015;105(suppl 2):S198-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Hara NN, Isaac M, Slobogean GP, Klazinga NS. The socioeconomic impact of orthopaedic trauma: a systematic review and meta-analysis. PLoS One. 2020;15:e0227907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Office of the Surgeon General, Office on Disability. Reports of the Surgeon General. The Surgeon General's Call to Action to Improve the Health and Wellness of Persons with Disabilities. Office of the Surgeon General (US); 2005. Available at: https://www.ncbi.nlm.nih.gov/books/NBK44667/. [PubMed] [Google Scholar]
- 14.Plomb-Holmes C, Luthi F, Vuistiner P, Leger B, Hilfiker R. A return-to-work prognostic model for orthopaedic trauma patients (WORRK) updated for use at 3, 12 and 24 months. J Occup Rehabil. 2017;27:568-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rainer TH, Yeung JH, Cheung SK, et al. Assessment of quality of life and functional outcome in patients sustaining moderate and major trauma: a multicentre, prospective cohort study. Injury. 2014;45:902-909. [DOI] [PubMed] [Google Scholar]
- 16.Regenbogen SE, Veenstra CM, Hawley ST, et al. The personal financial burden of complications after colorectal cancer surgery. Cancer. 2014;120:3074-3081. [DOI] [PubMed] [Google Scholar]
- 17.Scott AR, Rush AJ, 3rd, Naik AD, Berger DH, Suliburk JW. Surgical follow-up costs disproportionately impact low-income patients. J Surg Res. 2015;199:32-38. [DOI] [PubMed] [Google Scholar]
- 18.Shankaran V, Jolly S, Blough D, Ramsey SD. Risk factors for financial hardship in patients receiving adjuvant chemotherapy for colon cancer: a population-based exploratory analysis. J Clin Oncol. 2012;30:1608-1614. [DOI] [PubMed] [Google Scholar]
- 19.Teunis T, Thornton ER, Jayakumar P, Ring D. Time seeing a hand surgeon is not associated with patient satisfaction. Clin Orthop Relat Res. 2015;473:2362-2368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Bone and Joint Initiative (USBJI). Fact Sheets. Available at: https://www.boneandjointburden.org/fact-sheets. Accessed April 21, 2020.
- 21.Veenstra CM, Regenbogen SE, Hawley ST, et al. A composite measure of personal financial burden among patients with stage III colorectal cancer. Med Care. 2014;52:957-962. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


