Abstract
Herein, we consider venous immunothrombotic mechanisms in SARS-CoV-2 infection and anti-SARS-CoV-2 DNA vaccination. Primary SARS-CoV-2 infection with systemic viral RNA release (RNAaemia) contributes to innate immune coagulation cascade activation, with both pulmonary and systemic immunothrombosis - including venous territory strokes. However, anti-SARS-CoV-2 adenoviral-vectored-DNA vaccines -initially shown for the ChAdOx1 vaccine-may rarely exhibit autoimmunity with autoantibodies to Platelet Factor-4 (PF4) that is termed Vaccine-Induced Thrombotic Thrombocytopenia (VITT), an entity pathophysiologically similar to Heparin-Induced Thrombocytopenia (HIT). The PF4 autoantigen is a polyanion molecule capable of independent interactions with negatively charged bacterial cellular wall, heparin and DNA molecules, thus linking intravascular innate immunity to both bacterial cell walls and pathogen-derived DNA. Crucially, negatively charged extracellular DNA is a powerful adjuvant that can break tolerance to positively charged nuclear histone proteins in many experimental autoimmunity settings, including SLE and scleroderma. Analogous to DNA-histone interactons, positively charged PF4-DNA complexes stimulate strong interferon responses via Toll-Like Receptor (TLR) 9 engagement. A chain of events following intramuscular adenoviral-vectored-DNA vaccine inoculation including microvascular damage; microbleeding and platelet activation with PF4 release, adenovirus cargo dispersement with DNA-PF4 engagement may rarely break immune tolerance, leading to rare PF4-directed autoimmunity. The VITT cavernous sinus cerebral and intestinal venous territory immunothrombosis proclivity may pertain to venous drainage of shared microbiotal-rich areas of the nose and in intestines that initiates local endovascular venous immunity by PF4/microbiotal engagement with PF4 autoantibody driven immunothrombosis reminiscent of HIT. According to the proposed model, any adenovirus-vectored-DNA vaccine could drive autoimmune VITT in susceptible individuals and alternative mechanism based on molecular mimicry, vaccine protein contaminants, adenovirus vector proteins, EDTA buffers or immunity against the viral spike protein are secondary factors. Hence, electrochemical DNA-PF4 interactions and PF4-heparin interactions, but at different locations, represent the common denominator in HIT and VITT related autoimmune-mediated thrombosis.
Keywords: COVID-19 pneumonia related thrombosis, Vaccine induced thrombotic thrombocytopenia (VITT), Heparin induced thrombocytopenia (HIT) DNA-PF4 interactions. VITT model
1. Introduction
The global vaccination programme against SARS-CoV-2 has been hindered by the rare -and initially inexplicable-emergence of vaccine-associated thrombosis, especially venous territory strokes or other venous obstructions, including portal vein thrombosis that has been termed Vaccine-Induced Thrombotic Thrombocytopenia (VITT) [[1], [2], [3]]. These infrequent thrombotic side effects are reminiscent of natural SARS-CoV-2 infection, itself associated with lung and systemic immunothrombosis manifesting as: chest pain, pulmonary embolism, pulmonary infarction, systemic thrombosis, including Deep Venous Thrombosis (DVT), strokes, intestinal, cardiac and renal ischaemia affecting both arterial and venous territories [4,5]. However, natural SARS-CoV-2 infection is mediated by a single stranded RNA virus, while the vaccine-associated immunothrombosis is linked to DNA adenovirus-vectored vaccines [2].
A deeper biological understanding of this emergent phenomenon has far-reaching implications, since the current situation is linked to both societal and pharmaceutical sector concerns and uncertainty, and even the adoption of outright governmental bans [6]. A model to understand the mechanisms of natural SARS-CoV-2 infection and DNA spike protein vaccines associated immunothrombosis is vital and this is especially the case because of the reported interactions between the spike protein and the vascular system. Herein, we briefly explain the difference between natural SARS-CoV-2 infection-related immunothrombosis and the immunothrombotic mechanisms following DNA vaccination that share strong similarities with the autoimmune condition known as Heparin-Induced Thrombocytopenia (HIT) [[7], [8], [9], [10]].
1.1. Spike protein-ACE2 interactions: not guilty in vaccine-associated immunothrombosis?
An obvious area of overlap between natural SARS-CoV-2 infection and the available vaccines is spike protein expression [11]. In natural viral infection, the SARS-CoV-2 spike protein facilitates host cell access via the Angiotensin-Converting Enzyme 2 (ACE2) receptor [12] and all of the available vaccines, whether DNA- or RNA-based, result in spike protein expression towards the elicitation of protective immunity [13]. The ACE2 receptor is a key component of the Renin-Angiotensin System (RAS) [14] and also impacts on platelet function with both SARS-CoV-2 virus particles or spike-protein-mediated platelet dysregulation as one theoretically common denominator for vascular pathology between native infection and vaccines [15]. Furthermore, a strong rationale for SARS-CoV-2 spike-protein-mediated downregulation of endothelial ACE2 receptor expression that predisposes to vasospasm and immunothrombosis has been put forward [16]. SARS-CoV-2 spike-protein-mediated ACE2 downregulation could theoretically predispose to endotheliopathy and cardiovascular pathology, though not specifically to thrombosis, in experimental settings [17,18]. However, the literature on ACE2 as a driver of putative platelet immunothrombotic mechanisms is contradictory in relationship to disparate reports of platelet ACE2 expression [15,19]. The available clinical data on the two spike-protein-targeting SARS-CoV-2 RNA vaccines has not been linked to a thrombotic immunopathology, but it must is acknowledged that systemic ACE2 protein expression with all vaccines is likely negligible. Non thrombotic, rare autoimmune sequelae have been reported following predominant RNA SARS-CoV-2 vaccination [20].
1.2. Viral RNA innate immune-driven immunothrombosis in severe COVID-19 pneumonia
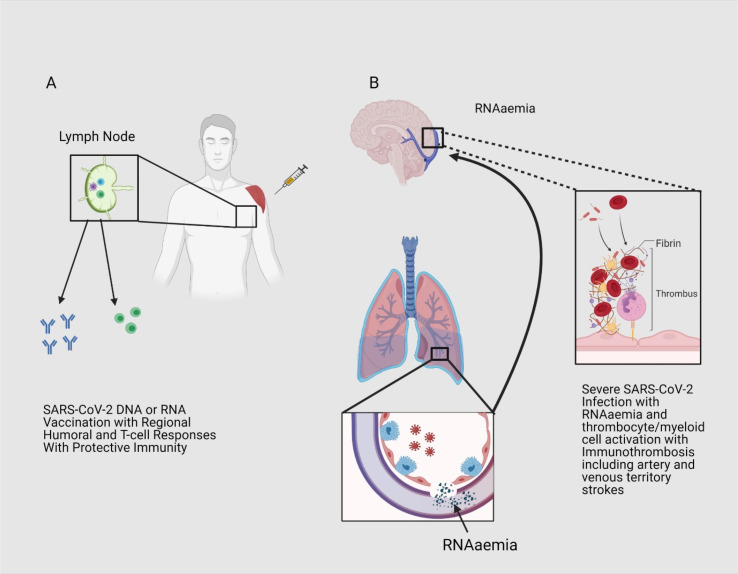
Diffuse pulmonary capillary, arteriolar and venular thrombosis is very typical of severe SARS-CoV-2 pneumonia [21,22]. We previously dubbed the pattern of SARS-CoV-2-associated lung immunothrombosis as Pulmonary Intravascular Coagulopathy (PIC) and deliberately chose this acronym to differentiate this pathology from Disseminated Intravascular Coagulation (DIC), the latter of which leads to severe platelet consumption [23,24]. It is increasingly appreciated that direct endothelial SARS-CoV-2 infection is not necessary for the PIC pathology [25,26], which points towards innate immunity mechanisms underlying the prothrombotic state [[27], [28], [29], [30]]. A contemporary model for severe COVID-19 pneumonia has proposed: i) that natural SARS-CoV-2 infection in close juxtaposition to the circulation leads to early immunothrombosis aimed at containment of thrombogenic SARS-CoV-2 RNA; but ii) that alveolar-vascular barrier disruption in severe COVID-19 pneumonia may instead lead to circulation of viral debris, including viral RNA that is termed “RNAaemia” [31]. Indeed in many studies on COVID-19 pneumonia, circulating SARS-CoV-2 viral RNA is often undetectable, which points towards the efficacy of this RNA-related immunothrombosis in constraining SARS-CoV-2 to the lung parenchyma in less severe COVID-19 pneumonia [32]. Failure of this mechanism, in severe COVID-19 pneumonia, may contribute to multi-organ ischaemia -that may mimic vasculitis-due to the immunothrombosis driven by viral RNA that has escaped the lungs and which can readily access the systemic venous circulation (Fig. 1 ) [24]. The Central Nervous System (CNS) thrombosis in severe COVID-19 is predominantly arterial, but RNA molecules may directly cross the capillary networks and then trigger venous territory thrombosis, an occurrence that is contributed to by other factors linked to hypercoagulability in severe COVID-19 pneumonia (Fig. 1).
Fig. 1.
Immunothrombosis in natural SARS-CoV-2 infection and vaccine prevention.
A) RNA and DNA SARS-CoV-2 vaccines are not associated with viral replication and systemic RNAaemia or pulmonary vascular territory immunothrombosis as a small nucleic acid inoculums are confined to the muscle and are therefore not linked to innate immune mediated thrombosis. B) Natural SARS-CoV-2 infection is associated with extensive pulmonary capillary, pulmonary arteriolar and pulmonary venular territory immunothrombosis in severe COVID-19. Viral RNA is a potent activation of the coagulation cascade and likely contributes to the immunothrombosis phenotype including arterial and venous territory strokes. Additionally, severe COVID-19 pneumonia appears to be associated with alveolar-capillary barrier breakdown with access of SARS-CoV-2 RNA or RNAaemia which can trigger an innate immune driven venous thrombosis in multiple organs including the brain. So RNAaemia and hypercoagulability from innate immune cell activation within the lung and other factors in severe COVID-19 pneumonia may predispose to venous territory strokes. Although HIT may also exhibit arterial and venous strokes it has a distinct autoimmune component.
Experimentally, it is well established that intravascular RNA can activate the coagulation cascade by providing a cofactor template for the factors XII/XI-induced contact activation with extensive RNA-dependent intravascular immunothrombosis [33]. Additionally, immune cells and platelets cross-talk following platelet RNA virus engagement and activation within the lung could contribute to systemic hypercoagulability [34] (Fig. 1). Critically ill COVID-19 cases with thrombocytopenia, some of whom had associated thrombosis, exhibited systemic platelet activation, but lacked of Platelet Factor 4 (PF4)- autoantibodies, a finding that was attributed to FcRγII-immune-complex-mediated platelet activation [35], so being distinct from HIT or VITT.
Vaccines against SARS-CoV-2 –whether DNA or RNA based - overall prevent the severe pneumonia that is associated with local and remote immunothrombotic complications, including strokes (Fig. 1). SARS-CoV-2 RNA or adenovirus-vectored DNA spike protein vaccines-are either not linked or are weakly linked to immunothrombosis, since RNA/DNA is present only to a limited degree in the muscle tissue - hence insufficient to drive the aforementioned immunothrombosis mechanisms (Fig. 1). The systemic access of RNA in severe COVID-19 pneumonia provides an explanation for arterial and venous territory strokes and intestinal venous territory infarction in that setting [36,37]. Arterial and venous strokes are also a feature of HIT where a fundamentally different autoimmune pathology exists to severe COVID-19 related immunothrombosis. As further set out, electrochemical interactions between heparin or DNA -both of which are negatively charged- and the positively charged PF4 autoantigen that is shared between HIT and VITT [38] can be used to construct a VITT model linked to the DNA content of adenovirus vectors.
1.3. Autoimmunity towards PF4 related to DNA in adenovirus-vectored vaccines
It must be emphasised that the DNA-vectored vaccines virtually eliminate the development of PIC pathology -so the aforementioned RNA/innate immune-mediated thrombosis in natural SARS-CoV-2 infection with systemic immune activation with pervasive hypercoagulability mechanisms is blocked, thus preventing immunothrombosis, with a great reduction in SARS-CoV-2-related mortality [39]. However, the rare emergent DNA-vaccine-associated immunothrombosis - dubbed VITT-has a radically different immunopathology to PIC and may have an incidence between 1 in 100,000 to one in a million, although further epidemiological data is needed [40].
The emergent VITT phenotype shares many clinical, laboratory and immunological features with HIT, the latter of which is well reviewed elsewhere [10]. These features include thrombocytopenia, unusual strokes (including venous strokes) and the presence of anti-PF4 autoantibodies [41]. It is well established that HIT is an autoimmune disease that nearly always develops following heparin therapy, though VITT cases have not been generally exposed to heparin. Another common feature of both HIT and VITT is the temporal emergence of PF4-associated immunothrombosis after 5 days of heparin therapy [7] or ChAdOx1 vaccination [2,42]. The quick onset of this autoimmune phenomenon is thought to be linked to prior PF4 sensitization in HIT and the kinetics of VITT in relationship to thrombosis suggest similar autoantibody pre-sensitization [8,38,43].
PF4 is a heparin-binding protein and is the target of autoimmunity in HIT, with the electrochemical interplay between negatively charged heparin and positively charged PF4 being crucial to this interaction [41,44]. Native heparin is well known for its immunomodulatory properties in vivo [45], but large heparin-PF4 complexes, analogous to PF4-bacterial complexes, render PF4 immunogenic through potential conformational changes in the molecule [8]. Outside its chemokine and heparin engagement role, megakaryocyte- and platelet-derived PF4 also binds directly to polyanionic lipids on both gram positive and gram negative bacterial cellular walls, so representing an important component of intravascular anti-bacterial innate immune responses [46,47]. Experimental bacterial polymicrobial sepsis has been associated with the elicitation of anti-PF4 autoantibodies towards the augmentation of phagocytosis in vivo, with such PF4 autoantibodies reported in normal humans and in subjects with COVID-19 pneumonia [46,48], although there is no functional evidence for HIT or VITT in severe COVID-19.
Another key aspect of PF4 autoantibodies in HIT is their T-cell independent nature and short half-life, with these belonging to the “natural autoantibody” class that plays important homeostatic roles including phagocytosis [49]. The cellular source for these short-term PF4 autoantibodies in HIT is thought to be innate immune B cells, including marginal zone B-cells that are abundant in the spleen – an organ that is filter for microbes which access the systemic circulation [50]. In HIT, the engagement of PF4 by PF4 autoantibodies on heparin-decorated endothelial cells ultimately serves to engage and activate platelet FcRγII receptors, with platelet alpha granule degranulation followed by further PF4 release and progressive immunothrombosis [51] - including autoantibody-PF4 immune complex activation of myeloid cells [52,53]. Following heparin therapy for thromboembolic disease, heparin sequestration and further PF4 entrapment may cause clot extension and new thromboembolism [54]. It has been deduced that PF4-polyanionic molecular interactions and PF4 autoantibodies may be a common feature of naturally-occurring immune responses that is recapitulated with pharmacological application of heparin [46].
1.4. DNA as an adjuvant for PF4 in VITT and how this overlaps with HIT immunothrombosis
Like heparin, double stranded DNA is negatively charged and forms DNA-PF4 complexes, with this adjuvanticity likely contributing to autoantibody development and ultimately thrombosis in VITT. Indeed, PF4 organizes polyanionic DNA into liquid crystalline immune complexes that amplified Toll-Like Receptor (TLR) 9- plasmacytoid dendritic cell interferon (IFN)-α production [55]. The ability of DNA to act as an adjuvant is well known in immunology and may underscore the pervasive autoimmunity against nucleoproteins bound to DNA in SLE in human and experimental autoimmunity [[56], [57], [58]]. Nevertheless, the first 15 years of experimental research with DNA vaccines failed to demonstrate Anti-Nuclear Autoantibody (ANA) positivity or autoimmune disease [59], with this rare complication being unmasked by mass vaccination programmes. Of note, the recognition of PF4-directed autoimmunity in VITT led to a search for the same autoantibody in severe COVID-19 pneumonia, where multiple autoantibodies -including anti-IFN and anti-endothelial cells autoantibodies-have been described [[60], [61], [62], [63]]. Recently, autoantibodies directed against PF4 have been found in about 8% of COVID-19 cases but were of low magnitude compared to VITT and were not linked to immunothrombotic phenotypes [48], so are likely part of the known role of PF4-Anti-PF4 autoantibodies in natural immunity.
1.5. A different path to PF4-related immunothrombosis in VITT
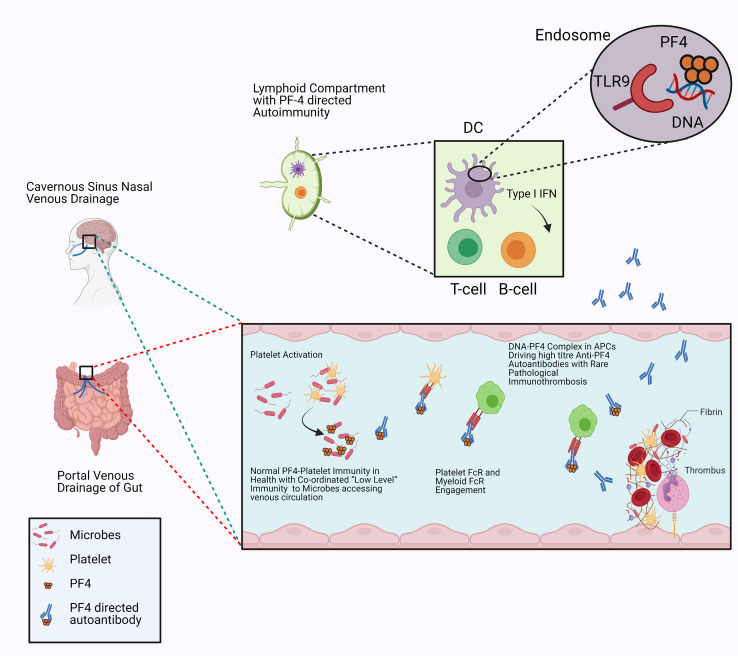
Based on the electrochemical role of PF-4 and heparin in HIT, we propose a model where negatively charged DNA that is known to interact with positively charged nuclear histone proteins likewise interacts with PF4 leading to viral nucleic acid/PF4 complex internalisation by Antigen-Presenting Cells (APCs) at the site of injection in the muscle. So HIT is intravascular linked to prior thrombosis but VITT is extravascular related to failed tissue tolerance mechanisms (Fig. 2 ). The local tissue microtrauma, alongside local microbleeding and immune cell activity, will bring adenoviral DNA in contact with PF4, followed by uptake by APCs and then memory B cell engagement in the regional lymph-nodes, with substantially increased PF4 autoantibody production (Fig. 2). However, VITT is much rarer than HIT and sometimes the venous thrombosis takes two weeks to occur, a time that raises the possibility of primary T-cell dependent immune response - since presensitising anti-PF4 antibodies have not been shown in VITT [64,65]. Unlike HIT, where vascular injury due to clot is already established and is commonly linked to autoimmune immunothrombosis, PF4 autoantibody in VITT has no vascular pre-formed “tissue specific” clot nidus, so this may explain why immunothrombosis is much less common. .
Fig. 2.
Vascular and immune topography of VITT
The VITT associated thrombosis is predominantly venous and involves the gastrointestinal portal circulation and the cavernous cerebral venous sinus circulation. Both of these venous territories share the common feature of draining the nasal sinus and intestines, thus allowing access of microbiotal, viral products and potentially toxins to the endothelial networks of lining vessels. Microbe platelet interactons with platelet factor-4 (PF4) coating and PF4/PF4 “natural” autoantibody cross-talk with platelets and myeloid cells maintains immunity and homeostasis restoration. The presence on high titre autoantibodies against PF4 in these tissue specific sites of susceptibility may lead to an exaggerated immune response including platelet and neutrophil activation, increased platelet consumption and thrombosis. Sequestration of PF4 in the presence of anti-PF4 autoantibodies triggers extensive FcRγII mediated platelet activation with further PF4 release and further platelet and immune cell chemotaxis thus initiating systemic thrombosis and platelet consumption which is based on the model of PF4 immune activation in HIT. The interaction between highly negatively charged heparin molecules on endothelial surfaces and the highly positively charged PF4 in the clot environment could further increase immunothrombosis.
According to this model, any DNA-vectored vaccine may lead to the same type of autoimmunity in susceptible individuals, which for many autoimmune diseases is the younger female population. If so, the size of the DNA payload and engagement of PF4 at sites of microvascular injury could be the key determinants. It is also possible that the mechanism of extravascular tissue injury could be associated with T-cell dependent and persistent autoantibody responses, unlike the short-lived PF4 autoantibody responses in HIT.
1.6. Other considerations
If this is a pervasive physiochemical consequence of DNA/PF4 interaction at sites of vaccine injection, then all adenovirus-based DNA delivery strategies might be expected to exhibit the same rare autoimmune VITT pathology in a wide array of settings. It must be pointed out that a role for adenoviral proteins has been suggested as a potential factor in VITT [66]. Furthermore, native adenovirus respiratory tract infection may be associated with thrombocytopenia -in turn linked to viral engagement of platelets via the Coxsackie A virus Receptor (CAR) [67,68]- although this appears to be completely distinct from the autoimmunity seen in HIT and VITT. Moreover, intravenous adenovirus gene therapy strategies have been associated with severe immunothrombosis, but case numbers were small and possibly related to the procoagulant properties of adenovirus/platelet interplay [69].
Molecular mimicry between spike protein and PF4 epitopes is predicated to be theoretically possible, but antibody cross reactivity has not been demonstrated, so such a mechanisms is unlikely to be linked to thrombosis [48]. Furthermore, vaccine contents -including protein contaminants-may have little impact on this model, but the number of spike protein DNA copies could be relevant, as could charged agents including EDTA that could impact on PF4-DNA interactions. That VITT is not seen with SARS-CoV-2 RNA vaccines, where needle microinjury with release of self RNA occurs, argues for a key role for viral DNA in VITT. Self DNA, that is typically released by NETotic (Neutrophil Extracellular Traps) neutrophils at sites of potential injury is quickly citrullinated, leading to electric charge rebalancing by eliminating physiochemical DNA-cationic protein interactions [70]. This is likely to also account for the lower magnitude of anti-PF4 autoantibody generation in severe COVID-19, where immunothrombosis with NETosis is common but a VITT or HIT immunopathology has not been shown [35].
1.7. Why the unusual venous territory immunothrombosis in VITT?
Why is PF4 autoimmunity restricted to discrete venous drainage basins rather than being generalised, as the putative disease-associated autoantibody has access to the entire luminal endothelial surface? We conceptualise this in terms of the immunological disease continuum of inflammation against self, whereby many autoimmune conditions have important site-specific factors that underline disease topography and localisation [71]. Of note, the splanchnic and cavernous sinus venous drainage territories share the commonality of draining the gut and respiratory barrier tissues, themselves interplaying strongly with viruses/microbiota and guarding against access of potential toxins and adjuvants to the circulation (Fig. 2).
Accordingly, endothelial activation -or microdamage-at these sites facilitate local innate immune activation towards endothelial barrier homeostasis and repair (Fig. 2). Entering this stage from the gut or nasal tissue drainage territory are microbes, where coating by PF4 and anti-PF4 may contribute to normal immunity and antigen clearance. The presence of high titre anti-PF4 autoantibodies in these environments -that is secondary to PF4-DNA complexes activating B cell response-triggers an immunopathology similar to that seen in HIT, but of course the intrinsic vascular damage -unlike the usual DVTs in HIT-is minimal or of low magnitude. In HIT, a role for site-specific factors in venous thrombosis is also well established given that this typically occurs at sites of pre-existent deep venous thrombosis or venous cannulation, with extension due to the local endothelial-heparin-PF4 interaction in normal physiology that becomes dysregulated in the presence of autoantibodies [10].
1.8. Implications of model for SARS-CoV-2 DNA vaccines
It has been proposed that the shedding of spike protein by Ad26.COV2·S (adenovirus-vectored) may be relevant for understanding immunothrombosis, while the ChAdOx1 vaccine does not shed spike protein [48]. According to our model that links electrochemical similarities between DNA and heparin -with both involved in PF4 engagement-then the central tenet predisposing to immunothrombosis is the inherent ability of PF4 to act as a DNA sensor. If this model is correct, then the size of the DNA payload of adenovirus-vectored vaccines, rather that the actual coded protein or viral structural elements, could be key to understanding this hitherto enigmatic and rare autoimmune response. Moreover, high titre anti-PF4 autoantibodies have been reported in younger -usually females-subjects [48], supporting the autoimmunity theory for this rare VITT complication, whereas the RNA-related thrombosis in natural severe COVID-19 affects older subjects and more often males (Table 1 ).
Table 1.
Comparison of COVID-19 immunothrombosis with HIT and VITT.
| COVID-19 Pneumonia | HIT | VITT | |
|---|---|---|---|
| Thrombosis Mechanism | RNAaemia Embolism from pulmonary vein territory? |
Platelet Degranulation at sites of thrombosis linked to vessel wall thrombosis or injury | Platelet degranulation at venous territory which drain microbial basins triggered by PF4 microbial interactions |
| Age | Older- Male | Younger Female | |
| PF4 Autoantibodies | 8% Reported low level and may not directly activate platelets Platelet activation by other immune complexes |
High titre | Very common high titre |
| Anion scaffold for PF4 | None | Heparin (acting in the vasculature and in marginal zone B cells in spleen) | Double stranded DNA (acting in lymph nodes leading to breakage of tolerance) |
| Location of Thrombosis | Arterial Predominant Venous reported |
Venous and arterial | Venous |
| Other Autoantibodies | Multiple but pathogenic role debatable | No | No |
| Initiating Event | Multiple mechanisms including RNA activation of coagulation | -Vascular wall insult with heparin PF4 interaction | 1) Endovascular PF4 binding of microbes 2) Extravascular DNA-PF4 interaction at sites of “needle stick injury” |
| Adjuvant | RNA | Heparin-PF4 large complexes | Viral DNA-PF4 complexes No evidence self DNA-PF4 complexes? |
| Primary Vascular Territory | Intravascular Lung Primary Secondary Systemic thrombosis –arterial and venous |
Intravascular at sites of clot –typically DVT but also arterial | Cavernous sinsus or portal venous thrombosis Would not occur with inhaled DNA vaccines? |
2. Conclusions
The venous thrombosis/venous territory haemorrhage in severe COVID-19 may be linked to the thrombotic effects of circulatory viral RNA and a myriad of systemic immune-activation-related hypercoagulability factors, including platelet and immune cell activation [72,73]. An interesting question that arises is related to the rarity of venous thrombosis in severe SARS-CoV-2 infection and VITT following vaccination. First, venous thrombosis including DVT have been reported to be very common in severe SARS-CoV-2 infection and the relative paucity of cerebral venous thrombosis with stroke likely links to the established principles of venous stasis and sluggish flow in the lower limbs for DVT. For VITT, the extreme rarity likely pertains to well-established mechanisms of immunological tolerance to self proteins, with tolerance being comparatively difficult to break. Other factors include the small size of DNA inoculums in relevant vaccines with inadequate DNA-PF4 co-engagement to break tolerance [74]. The chances of RNA or DNA –at the magnitudes currently delivered by vaccine inoculums-accessing the systemic circulation in amounts sufficient to trigger similar immunopathology appear negligible. RNA vaccines use several pattern recognition receptors -including TLR7-whereas the DNA vaccines almost exclusively use TLR9, linked to humoral and cellular immunity development against spike protein [75]. We propose that viral DNA-PF4 interplay may be a component of antiviral innate immunity, akin to this concept for bacterial intravascular innate immunity [46]. Adenovirus injection and microbleeding may bring viral DNA and PF4 together in the extracellular space, followed by APCs uptake and –rarely- leading to autoimmune disease, especially in younger subjects. Whether the subtle differences in DNA load in different SARS-CoV-2 vector vaccines or other factors may influence this rare emergent autoimmunity awaits delineation. This model has implications for the future of all injectable DNA based vaccines.
Acknowledgements
D.M, G.D.M. and C.B. are supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (LBRC). The views expressed are those of the authors and not necessarily those of the (UK) National Health Service (NHS), the NIHR, or the (UK) Department of Health.
References
- 1.Cines D.B., Bussel J.B. SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. N. Engl. J. Med. 2021 doi: 10.1056/NEJMe2106315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schultz N.H., et al. Thrombosis and thrombocytopenia after ChAdOx1 nCoV-19 vaccination. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2104882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehta P.R., et al. Cerebral venous sinus thrombosis and thrombocytopenia after COVID-19 vaccination - a report of two UK cases. Brain Behav. Immun. 2021 doi: 10.1016/j.bbi.2021.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGonagle D., et al. COVID-19 vasculitis and novel vasculitis mimics. Lanc Rheumatol. 2021;3(3):e224–e233. doi: 10.1016/S2665-9913(20)30420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Harrison S.R., et al. Chest pain mimicking pulmonary embolism may be a common presentation of COVID-19 in ambulant patients without other typical features of infection. J. Intern. Med. 2021 doi: 10.1111/joim.13267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chadwick L. Finland suspends AstraZeneca vaccine despite European regulator saying it is safe and effective. 2021. https://www.euronews.com/2021/03/18/norway-sweden-denmark-wait-before-restarting-astrazeneca-vaccinations [cited 2021 28-Apr-2021]; Available from:
- 7.Arepally G., Cines D.B. Heparin-induced thrombocytopenia and thrombosis. Clin. Rev. Allergy Immunol. 1998;16(3):237–247. doi: 10.1007/BF02737634. [DOI] [PubMed] [Google Scholar]
- 8.Greinacher A. Heparin-induced thrombocytopenia. N. Engl. J. Med. 2015;373(19):1883–1884. doi: 10.1056/NEJMc1510993. [DOI] [PubMed] [Google Scholar]
- 9.Ahmed I., Majeed A., Powell R. Heparin induced thrombocytopenia: diagnosis and management update. Postgrad. Med. 2007;83(983):575–582. doi: 10.1136/pgmj.2007.059188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arepally G.M., Cines D.B. Pathogenesis of heparin-induced thrombocytopenia. Transl. Res. 2020;225:131–140. doi: 10.1016/j.trsl.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rawat K., Kumari P., Saha L. COVID-19 vaccine: a recent update in pipeline vaccines, their design and development strategies. Eur. J. Pharmacol. 2021;892:173751. doi: 10.1016/j.ejphar.2020.173751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jeyanathan M., et al. Immunological considerations for COVID-19 vaccine strategies. Nat. Rev. Immunol. 2020;20(10):615–632. doi: 10.1038/s41577-020-00434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Parker E.P.K., Shrotri M., Kampmann B. Keeping track of the SARS-CoV-2 vaccine pipeline. Nat. Rev. Immunol. 2020;20(11):650. doi: 10.1038/s41577-020-00455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuba K., Imai Y., Penninger J.M. Angiotensin-converting enzyme 2 in lung diseases. Curr. Opin. Pharmacol. 2006;6(3):271–276. doi: 10.1016/j.coph.2006.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang S., et al. SARS-CoV-2 binds platelet ACE2 to enhance thrombosis in COVID-19. J. Hematol. Oncol. 2020;13(1):120. doi: 10.1186/s13045-020-00954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verdecchia P., et al. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhong J., et al. Angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation. 2010;122(7):717–728. doi: 10.1161/CIRCULATIONAHA.110.955369. 18 pp. following 728. [DOI] [PubMed] [Google Scholar]
- 18.Magro C.M., et al. Severe COVID-19: a multifaceted viral vasculopathy syndrome. Ann. Diagn. Pathol. 2021;50:151645. doi: 10.1016/j.anndiagpath.2020.151645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Manne B.K., et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020;136(11):1317–1329. doi: 10.1182/blood.2020007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watad A., et al. Immune-mediated disease flares or new-onset disease in 27 subjects following mRNA/DNA SARS-CoV-2 vaccination. Vaccines. 2021;9(5) doi: 10.3390/vaccines9050435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fox S.E., et al. Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lanc Respir Med. 2020;8(7):681–686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McGonagle D., et al. Increased cardiovascular mortality in African Americans with COVID-19. Lanc Respir Med. 2020;8(7):649–651. doi: 10.1016/S2213-2600(20)30244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGonagle D., et al. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun. Rev. 2020;19(6):102537. doi: 10.1016/j.autrev.2020.102537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGonagle D., et al. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lanc Rheumatol. 2020;2(7):e437–e445. doi: 10.1016/S2665-9913(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stahl K., et al. Absence of SARS-CoV-2 RNA in COVID-19-associated intestinal endothelialitis. Intensive Care Med. 2021;47(3):359–360. doi: 10.1007/s00134-020-06326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahmetaj-Shala B., et al. Resistance of endothelial cells to SARS-CoV-2 infection <em>in vitro</em>. bioRxiv. 2020 doi: 10.1101/2020.11.08.372581. 2020.11.08.372581. [DOI] [Google Scholar]
- 27.Biswas I., Khan G.A. Coagulation disorders in COVID-19: role of toll-like receptors. J. Inflamm. Res. 2020;13:823–828. doi: 10.2147/JIR.S271768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avila J., et al. Thrombotic complications of COVID-19. Am. J. Emerg. Med. 2021;39:213–218. doi: 10.1016/j.ajem.2020.09.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singh B., Kaur P., Maroules M. Splanchnic vein thrombosis in COVID-19: a review of literature. Dig. Liver Dis. 2020;52(12):1407–1409. doi: 10.1016/j.dld.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vinayagam S., Sattu K. SARS-CoV-2 and coagulation disorders in different organs. Life Sci. 2020;260:118431. doi: 10.1016/j.lfs.2020.118431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McGonagle D., Bridgewood C., Meaney J.F.M., et al. A tri-compartmental model of lung oxygenation disruption in severe COVID-19 explains pulmonary and systemic pathology. Lanc Respirat Med. 2021 doi: 10.1016/S2213-2600(21)00213-7. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fajnzylber J., et al. SARS-CoV-2 viral load is associated with increased disease severity and mortality. Nat. Commun. 2020;11(1):5493. doi: 10.1038/s41467-020-19057-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kannemeier C., et al. Extracellular RNA constitutes a natural procoagulant cofactor in blood coagulation. Proc. Natl. Acad. Sci. U. S. A. 2007;104(15):6388–6393. doi: 10.1073/pnas.0608647104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Koupenova M., et al. The role of platelets in mediating a response to human influenza infection. Nat. Commun. 2019;10(1):1780. doi: 10.1038/s41467-019-09607-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nazy I., et al. Platelet-activating immune complexes identified in critically ill COVID-19 patients suspected of heparin-induced thrombocytopenia. J. Thromb. Haemostasis. 2021;19(5):1342–1347. doi: 10.1111/jth.15283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh B., et al. COVID-19 and bleeding at unusual locations: report of four cases. Hematol Transfus Cell Ther. 2021 doi: 10.1016/j.htct.2021.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ram-Mohan N., et al. SARS-CoV-2 RNAemia predicts clinical deterioration and extrapulmonary complications from COVID-19. Clin. Infect. Dis. 2021 doi: 10.1093/cid/ciab394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Prechel M.M., Walenga J.M. Emphasis on the role of PF4 in the incidence, pathophysiology and treatment of heparin induced thrombocytopenia. Thromb. J. 2013;11(1):7. doi: 10.1186/1477-9560-11-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dagan N., et al. BNT162b2 mRNA covid-19 vaccine in a nationwide mass vaccination setting. N. Engl. J. Med. 2021;384(15):1412–1423. doi: 10.1056/NEJMoa2101765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mahase E. Covid-19: unusual blood clots are "very rare side effect" of Janssen vaccine, says EMA. BMJ. 2021;373:n1046. doi: 10.1136/bmj.n1046. [DOI] [PubMed] [Google Scholar]
- 41.Cines D.B., et al. Antigen and substrate withdrawal in the management of autoimmune thrombotic disorders. Blood. 2012;120(20):4134–4142. doi: 10.1182/blood-2012-06-389445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Greinacher A., et al. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N. Engl. J. Med. 2021 doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cines D.B., et al. Heparin-associated thrombocytopenia. N. Engl. J. Med. 1980;303(14):788–795. doi: 10.1056/NEJM198010023031404. [DOI] [PubMed] [Google Scholar]
- 44.Rauova L., et al. Role of platelet surface PF4 antigenic complexes in heparin-induced thrombocytopenia pathogenesis: diagnostic and therapeutic implications. Blood. 2006;107(6):2346–2353. doi: 10.1182/blood-2005-08-3122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tang Y., et al. Heparin prevents caspase-11-dependent septic lethality independent of anticoagulant properties. Immunity. 2021;54(3):454–467 e6. doi: 10.1016/j.immuni.2021.01.007. [DOI] [PubMed] [Google Scholar]
- 46.Krauel K., et al. Platelet factor 4 binds to bacteria, [corrected] inducing antibodies cross-reacting with the major antigen in heparin-induced thrombocytopenia. Blood. 2011;117(4):1370–1378. doi: 10.1182/blood-2010-08-301424. [DOI] [PubMed] [Google Scholar]
- 47.Krauel K., et al. Platelet factor 4 binding to lipid A of Gram-negative bacteria exposes PF4/heparin-like epitopes. Blood. 2012;120(16):3345–3352. doi: 10.1182/blood-2012-06-434985. [DOI] [PubMed] [Google Scholar]
- 48.Greinacher A., et al. Towards understanding ChAdOx1 nCov-19 vaccine-induced immune thrombotic thrombocytopenia (VITT) Res. Sq. 2021 doi: 10.21203/rs.3.rs-440461/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Elkon K., Casali P. Nature and functions of autoantibodies. Nat. Clin. Pract. Rheumatol. 2008;4(9):491–498. doi: 10.1038/ncprheum0895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Staibano P., et al. The unique immunological features of heparin-induced thrombocytopenia. Br. J. Haematol. 2017;177(2):198–207. doi: 10.1111/bjh.14603. [DOI] [PubMed] [Google Scholar]
- 51.Warkentin T.E., et al. Sera from patients with heparin-induced thrombocytopenia generate platelet-derived microparticles with procoagulant activity: an explanation for the thrombotic complications of heparin-induced thrombocytopenia. Blood. 1994;84(11):3691–3699. [PubMed] [Google Scholar]
- 52.Joglekar M., et al. Heparin enhances uptake of platelet factor 4/heparin complexes by monocytes and macrophages. J. Thromb. Haemostasis. 2015;13(8):1416–1427. doi: 10.1111/jth.13003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rauova L., et al. Monocyte-bound PF4 in the pathogenesis of heparin-induced thrombocytopenia. Blood. 2010;116(23):5021–5031. doi: 10.1182/blood-2010-03-276964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Patriarcheas V., et al. Heparin-induced thrombocytopenia: pathophysiology, diagnosis and management. Cureus. 2020;12(3) doi: 10.7759/cureus.7385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lande R., et al. CXCL4 assembles DNA into liquid crystalline complexes to amplify TLR9-mediated interferon-alpha production in systemic sclerosis. Nat. Commun. 2019;10(1):1731. doi: 10.1038/s41467-019-09683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cooke M.S., et al. Immunogenicity of DNA damaged by reactive oxygen species--implications for anti-DNA antibodies in lupus. Free Radic. Biol. Med. 1997;22(1–2):151–159. doi: 10.1016/s0891-5849(96)00283-3. [DOI] [PubMed] [Google Scholar]
- 57.Wilson H.L., et al. Immune mechanisms and therapeutic potential of CpG oligodeoxynucleotides. Int. Rev. Immunol. 2006;25(3–4):183–213. doi: 10.1080/08830180600785868. [DOI] [PubMed] [Google Scholar]
- 58.Bode C., et al. CpG DNA as a vaccine adjuvant. Expert Rev. Vaccines. 2011;10(4):499–511. doi: 10.1586/erv.10.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kutzler M.A., Weiner D.B. DNA vaccines: ready for prime time? Nat. Rev. Genet. 2008;9(10):776–788. doi: 10.1038/nrg2432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang E.Y., et al. Diverse functional autoantibodies in patients with COVID-19. medRxiv. 2020 doi: 10.1101/2020.12.10.20247205. [DOI] [PubMed] [Google Scholar]
- 61.Zhang Y., et al. Coagulopathy and antiphospholipid antibodies in patients with covid-19. N. Engl. J. Med. 2020;382(17):e38. doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zhang Q., et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19. Science. 2020;(6515):370. doi: 10.1126/science.abd4570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhou Y., et al. Clinical and autoimmune characteristics of severe and critical cases of COVID-19. Clin Transl Sci. 2020;13(6):1077–1086. doi: 10.1111/cts.12805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Salter B.S., et al. Heparin-induced thrombocytopenia: a comprehensive clinical review. J. Am. Coll. Cardiol. 2016;67(21):2519–2532. doi: 10.1016/j.jacc.2016.02.073. [DOI] [PubMed] [Google Scholar]
- 65.Warkentin T.E., et al. Studies of the immune response in heparin-induced thrombocytopenia. Blood. 2009;113(20):4963–4969. doi: 10.1182/blood-2008-10-186064. [DOI] [PubMed] [Google Scholar]
- 66.Sadoff J., Davis K., Douoguih M. Thrombotic thrombocytopenia after Ad26.COV2.S vaccination - response from the manufacturer. N. Engl. J. Med. 2021 doi: 10.1056/NEJMc2106075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Atasheva S., Yao J., Shayakhmetov D.M. Innate immunity to adenovirus: lessons from mice. FEBS Lett. 2019;593(24):3461–3483. doi: 10.1002/1873-3468.13696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Raadsen M., et al. Thrombocytopenia in virus infections. J. Clin. Med. 2021;10(4) doi: 10.3390/jcm10040877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Othman M., et al. Adenovirus-induced thrombocytopenia: the role of von Willebrand factor and P-selectin in mediating accelerated platelet clearance. Blood. 2007;109(7):2832–2839. doi: 10.1182/blood-2006-06-032524. [DOI] [PubMed] [Google Scholar]
- 70.Jenne C.N., Kubes P. Virus-induced NETs--critical component of host defense or pathogenic mediator? PLoS Pathog. 2015;11(1) doi: 10.1371/journal.ppat.1004546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.McGonagle D., McDermott M.F. A proposed classification of the immunological diseases. PLoS Med. 2006;3(8):e297. doi: 10.1371/journal.pmed.0030297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nicolai L., et al. Immunothrombotic dysregulation in COVID-19 pneumonia is associated with respiratory failure and coagulopathy. Circulation. 2020;142(12):1176–1189. doi: 10.1161/CIRCULATIONAHA.120.048488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Skendros P., et al. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Invest. 2020;130(11):6151–6157. doi: 10.1172/JCI141374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Suh Y.J., et al. Pulmonary embolism and deep vein thrombosis in COVID-19: a systematic review and meta-analysis. Radiology. 2021;298(2):E70–E80. doi: 10.1148/radiol.2020203557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Teijaro J.R., Farber D.L. COVID-19 vaccines: modes of immune activation and future challenges. Nat. Rev. Immunol. 2021;21(4):195–197. doi: 10.1038/s41577-021-00526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]