To the Editor: Prisons and jails are high-risk settings for Covid-19, with case and mortality rates far exceeding those in the general community.1 More incarcerated people have died from Covid-19 in U.S. correctional facilities in the past year than died by capital punishment in the past 70 years.2 Some states, including California, have prioritized incarcerated people for vaccination.
The California Department of Corrections and Rehabilitation (CDCR) provided anonymized data at the person-day level for all California prison residents from December 22, 2020, when the CDCR vaccination program began, through March 4, 2021. The data, which are described in the Supplementary Appendix (available with the full text of this letter at NEJM.org) and elsewhere,3 included variables that indicated which residents were offered doses of the BNT162b2 (Pfizer–BioNTech) or mRNA-1273 (Moderna) vaccine and which residents accepted. Our goal was to calculate the percentage of residents who accepted at least one dose among the residents who were offered doses and to use multivariable logistic regression analysis to estimate the probability of the acceptance of at least one dose according to the residents’ race or ethnic group, age group, medical vulnerability, and history of Covid-19. We also analyzed acceptance among residents who were reoffered vaccination after they had initially declined.
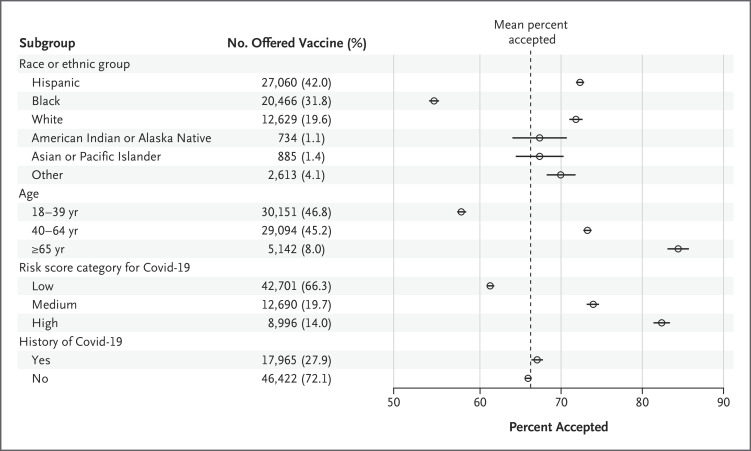
Two thirds of the 97,779 incarcerated residents were offered vaccines; among those offered a vaccine, 66.5% (42,952 of 64,633) accepted at least one dose. The results of adjusted analyses of the data for residents who were offered vaccination indicated that acceptance was highest among Hispanic residents (72.6%; 99.6% confidence interval [CI], 72.1 to 73.1) and White residents (72.1%; 99.6% CI, 71.3 to 72.9), slightly lower among American Indian or Alaska Native residents (67.7%; 99.6% CI, 64.4 to 71.0) and Asian or Pacific Islander residents (67.7%; 99.6% CI, 64.8 to 70.6), and substantially lower among Black residents (54.9%; 99.6% CI, 54.3 to 55.5) (Figure 1). Younger and healthier residents were less likely to accept vaccines than older and medically vulnerable residents. The percentages of residents who accepted did not differ appreciably according to residents’ history of Covid-19. Among the residents who had initially declined and were subsequently reoffered vaccination, 45.9% (901 of 1962) accepted at least one dose.
Figure 1. Percentage of Residents Offered Covid-19 Vaccination Who Accepted at Least One Dose.
Shown are the predicted margins estimated from the results of multivariable logistic-regression analyses of the sample of 64,387 incarcerated residents who were offered at least one dose of the BNT162b2 or mRNA-1273 vaccine, with adjustments for room type (defined according to the number of residents housed in a room), participation in penal labor, security level, and prison. Details of the model specification and a complete set of results are provided in Table S3 in the Supplementary Appendix. All the categories of race or ethnic group other than Hispanic indicate non-Hispanic residents. The California Department of Corrections and Rehabilitation (CDCR) developed a risk score to grade residents’ likelihood of severe Covid-19–related disease. The risk score sums weighted values for 17 items identified in the scientific literature as risk factors for severe outcomes after SARS-CoV-2 infection (Table S1). We categorized scores into low risk (score of 0 or 1), medium risk (2 or 3), and high risk (≥4). Residents were considered to have had a history of Covid-19 if they had had a positive test result while in CDCR custody, before the date of the first offer of a vaccine.
Most of the residents who were offered vaccines in the first 10 weeks of this program accepted, and the percentages of older and more medically vulnerable residents who accepted are similar to those reported in long-term care facilities.4 However, acceptance was markedly lower among residents at low risk for severe illness from Covid-19 and among non-Hispanic minorities, especially Black residents. Fewer than half of young, Black residents accepted at least one dose (Fig. S2), a finding that may reflect mistrust in correctional authorities and clinicians or a lack of access to reliable information on vaccine safety and efficacy.5 However, an encouraging finding was that a substantial proportion of residents who had initially declined a first dose later accepted a reoffer — an important indication that hesitancy is not necessarily fixed.
Even when Covid-19 vaccines become widely available in correctional institutions, achievement and maintenance of sufficient population-level immunity to avoid large outbreaks will be challenging. High and equitable vaccination uptake is crucial; attaining it may depend on successful efforts to build trust and vaccine confidence and on regular reoffers to those who decline initially.
Supplementary Appendix
Disclosure Forms
This letter was published on May 12, 2021, at NEJM.org.
Footnotes
Supported in part by the Covid-19 Emergency Response Fund at Stanford, established with a gift from the Horowitz Family Foundation; a grant (R37-DA15612), awarded to Dr. Salomon, from the National Institute on Drug Abuse; a grant (NU38OT000297-02), awarded to Dr. Salomon, from the Centers for Disease Control and Prevention though the Council of State and Territorial Epidemiologists; a grant (DGE-1656518), awarded to Ms. Chin, from the National Science Foundation Graduate Research Fellowship Program; and a grant (OR2020-69521), awarded to Dr. Alarid-Escudero, from Open Society Foundations.
Disclosure forms provided by the authors are available at NEJM.org.
References
- 1.Hawks L, Woolhandler S, McCormick D. COVID-19 in prisons and jails in the United States. JAMA Intern Med 2020;180:1041-1042. [DOI] [PubMed] [Google Scholar]
- 2.Snell TL. Capital punishment, 2018 — statistical tables. Washington, DC: Department of Justice, Bureau of Justice Statistics, September 2020. (https://www.bjs.gov/content/pub/pdf/cp18st.pdf). [Google Scholar]
- 3.Chin ET, Ryckman T, Prince L, et al. Covid-19 in the California state prison system: an observational study of decarceration, ongoing risks, and risk factors. March 8, 2021. (https://www.medrxiv.org/content/10.1101/2021.03.04.21252942v1). preprint. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gharpure R, Patel A, Link-Gelles R. First-dose COVID-19 vaccination coverage among skilled nursing facility residents and staff. JAMA 2021;325:1670-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Momplaisir F, Haynes N, Nkwihoreze H, Nelson M, Werner RM, Jemmott J. Understanding drivers of COVID-19 vaccine hesitancy among Blacks. Clin Infect Dis 2021. February 9 (Epub ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.