Abstract
Recently, India is at risk due to the exponential rising of COVID-19 infection, which generated a second wave. This infection rise may affect the vaccination program in India, and it can also affect vaccine production. In this manuscript, we have discussed the psychosocial and political factors that have driven the current wave of India. We have also tried to depict the psychosocial and political obstacles that are impairing the vaccination program.
Keywords: India, Second wave, COVID-19 vaccination program, Psychosocial obstacles for vaccination, Political obstacles for vaccination
1. Introduction
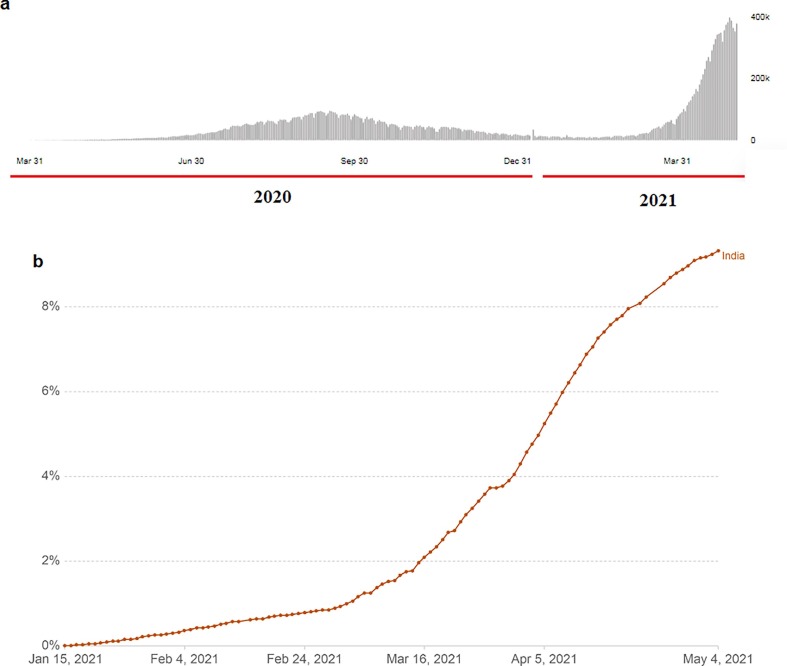
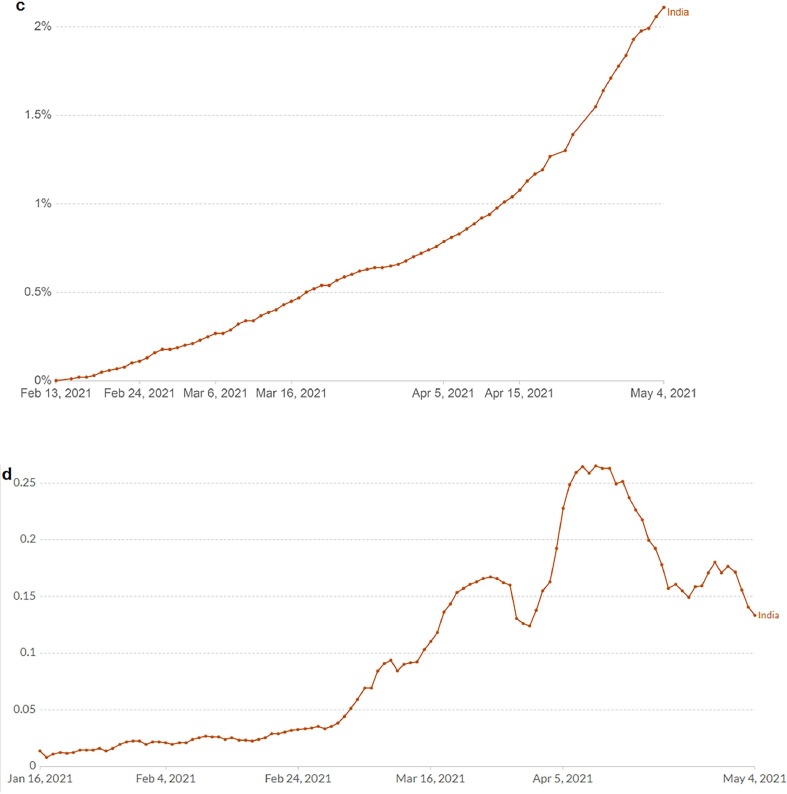
India is currently passing through a critical phase of the second wave of COVID-19. It ranks second globally in total infections (21,077,410; 3 Jan 2020–6 May 2021; Fig. 1 a) and fourth in total mortality (230,168; WHO, 2021). In major hospitals across the country, about 90% of patients are admitted for COVID-19 related complications. Thus, the ICU-ventilators are fully occupied, leading to an acute shortage of medical oxygen in major hospitals (Mallapatyy, 2021). The cremation sites are also being overflooded with bodies. In Maharashtra and Uttar Pradesh states, the situation has become serious. A Lancet editorial has recently criticized the government for not controlling the pandemic in time (Lancet, 2021).
Fig. 1.
COVID-19 infection and vaccination status in India (as on May 4, 2021) (a) COVID-19 infection cases (b) Indian population who obtained at least single dose of COVID-19 vaccine (Data source: WHO) (c) Indian population fully vaccinated against COVID-19 (Data source: Our World in Data) (d) Daily COVID-19 vaccine doses given per 100 individuals. Data have shown the rolling seven day average per 100 individuals in the total population. (Data source: Our World in Data).
2. Factors driving the second wave
2.1. Psychosocial factors
The first case, COVID-19, was reported on 27 January 2020 and the first wave took off at the end of March 2020. On 12 September, the highest first wave of infections was recorded (97,570). During the first week of February 2021, the lowest infections were noted, and at that time, mask hesitancy was common among the people.
A survey found the fact that people were aware of the significance of face masks. But, only 40% were actually wearing them. We have observed three categories of face mask usage behavior among people. First, people were casual in using the masks, and maximum belonged to this category. The second involved the half-opened face mask using behavior associated to low illiteracy on the infective nature of COVID-19. The last category of people felt discomfort in using the mask as they felt it as “suffocating” and among them, no changes in oxygen saturation level (SpO2) were noted.
Another significant factor is associated with the lack of social distancing in some cases. Due to some people's crowded style of living arrangements, it creates a challenging situation to maintain the necessary distancing to minimize the disease transmission.
2.2. Political factors
The Government was satisfied with prevention measures to control the first wave since the infection rate declined during the end of 2020. Hence, the government declared the assembly elections in the Pondicherry Union Territory and states such as West Bengal, Tamil Nadu, Kerala, and Assam during March-April 2021. Massive rallies and public gatherings have followed during the election campaigns without adhering to the COVID-19 disease prevention protocols.
At the same time, the Kumbh Mela pilgrimage was celebrated in the Ganges river at Haridwar, Uttarakhand state, where large crowds gathered. The major political and Hindu religious gatherings involving large crowds of people have contributed to the second wave (Lancet, 2021).
2.3. Biological factor
Indian scientists have recorded a double mutant B.1.617 variant from Maharashtra state, which is more infectious (Vaidyanathan, 2021). In addition, the B.1.1.7v ariant from the UK is also circulating throughout India, along with the P.1 lineage from Brazil and the B.1.351 lineage from South Africa. These new variants have also contributed to the surge of the second wave of COVID-19 infection in India.
3. Indian COVID-19 vaccines
Mass vaccinations have started in several countries worldwide. India has also begun to vaccinate its people, and it has a long history of producing vaccines (Lahariya, 2014). India currently contributes about 60% of the global vaccine manufacturing and supply, and it has the potential to deliver 3 billion doses of COVID-19 vaccines annually (Sharun and Dhama, 2021). It also makes low-cost vaccines (Chakraborty and Agoramoorthy, 2020). India's first native COVID-19 vaccine has been produced by Bharat Biotech (Covaxin). This inactivated vaccine (BBV152), formulated by the National Institute of Virology, collaborates with the Indian Council of Medical Research. Other significant COVID-19 vaccine candidates are Covishield from the Serum Institute of India, ZyCoV-D from Zydus Cadila, and Sputnik V from Dr. Reddys Lab.
4. Vaccination status in India
India has started a mass vaccination program. As of May 4, 2021, about 29.1 million people, or 2.1% of the total population, were fully vaccinated against COVID-19 (Fig. 1b). India has so far given 1581 million doses, and over 8% of the population has received one dose (Fig. 1c). The daily usages of the vaccine doses given per 100 people in India are not constant (Fig. 1d), and the maximum vaccine usage was recorded during mid-April 2021. Afterward, the dose administered curve started to decrease from April end to early May 2021, which indicated the acute vaccine shortage. The government has also halted the export of vaccines to reduce the scarcity of Covishield (Padma, 2021).
5. Obstacles impairing the vaccination program
5.1. Psychosocial obstacles
Three psychosocial obstacles are observed in the vaccination program. The vaccine acceptance rate in India is about 74%. The major obstacle of the COVID-19 is vaccine hesitancy linked to the efficacy of vaccines. Several health/frontline workers are infected even when they are fully vaccinated, creating public doubts about the vaccines' competence. The second obstacle involves vaccine illiteracy, especially in rural areas. The third obstacle involves the high cost of the vaccine, which is not favorable to the low-income group of people.
The vaccine is distributed through government hospitals/centers and private centers. In government centers, people are vaccinated freely by producing their identity cards. But they have to wait in queue for 10 to 12 h. People who visit private centers pay US$7 for the vaccine. In both places, minimum vaccines are only available daily, and people may return empty-handed after visiting 2–3 times, which may lead to hesitancy.
5.2. The political obstacles
The distribution policy of the COVID-19 vaccine has created a debate between the central and state governments due to the shortage of vaccine availability. Although India needs to increase the vaccine production capabilities urgently, the current status may affect vaccine production. To solve this crisis, the Government can approve other vaccines so that the globally developed vaccines can also be manufactured and distributed in India.
6. Conclusion
The COVID-19 infection cases are increasing daily due to infective double mutant variant and the people's casual behavior. Only 2.1% of the people have been vaccinated in India, which is low compared to the total population. It will be a challenging task to vaccinate everyone quickly. India must develop short and long-term strategies to vaccinate the people fast to restrain the second wave and end the pandemic.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This study was supported by Hallym University Research Fund and by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF - 2020R1C1C1008694 & NRF- 2020R1I1A3074575).
References
- Chakraborty C., Agoramoorthy G. India’s cost-effective COVID-19 vaccine development initiatives. Vaccine. 2020;38(50):7883–7884. doi: 10.1016/j.vaccine.2020.10.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahariya C. A brief history of vaccines & vaccination in India. Indian J. Med. Res. 2014;139:491. [PMC free article] [PubMed] [Google Scholar]
- Lancet The., 2021. India's COVID-19 emergency. The Lancet; 397(10286):1683. Doi: 10.1016/S0140-6736(21)01052-7. [DOI] [PMC free article] [PubMed]
- Mallapaty S. India's massive COVID surge puzzles scientists. Nature. 2021;7856:667–668. doi: 10.1038/d41586-021-01059-y. [DOI] [PubMed] [Google Scholar]
- Padma T. India’s COVID-vaccine woes—by the numbers. Nature. 2021;592(7855):500–501. doi: 10.1038/d41586-021-00996-y. [DOI] [PubMed] [Google Scholar]
- Sharun K., Dhama K. India’s role in COVID-19 vaccine diplomacy. J. Travel Med. 2021 doi: 10.1093/jtm/taab064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaidyanathan, G., 2021. Coronavirus variants are spreading in India — what scientists know so far. Nature. https://www.nature.com/articles/d41586-021-01274-7. [DOI] [PubMed]
- WHO, 2021. India Situation. WHO. https://covid19.who.int/region/searo/country/in.