Abstract
SUMMARY: Three patients with spontaneous dural carotid-cavernous fistulas were treated by using a combination of detachable coils and Onyx liquid embolic agent. Cavernous sinus was accessed via the superior ophthalmic vein or inferior petrous sinus approach. In all cases, a complete angiographic closure of the fistulas was achieved with full recovery from neuro-ophthalmologic symptoms. This report suggests that the controlled and excellent penetration of Onyx is superb for blocking the intricate communication of dural carotid-cavernous fistulas.
Ethylene-vinyl alcohol copolymer (EVOH) (Onyx, Micro Therapeutics, Irvine, Calif), is a nonadhesive liquid embolic agent that was evaluated at UCLA Medical Center between January 1998 and May 1999. Experimental histopathologic research in swine rete mirabile had already been performed between 1997 and 1998.1,2 The FDA approved the intravascular use of Onyx for embolization of intracranial arteriovenous malformations (AVMs) in July 2005. This article details the use of Onyx intravasculary, in combination with detachable coils, in 3 cases of spontaneous cavernous dural arteriovenous fistulas.
Case Reports and Description of Technique
Case 1
A 67-year-old woman, with well-controlled diabetes mellitus and hypertension, developed slowly progressing left eye injection, swelling, and blurry vision during a 3-week period. On the preprocedure physical examination, proptosis and significant conjunctival chemosis in the left eye were observed. The visual acuity was OS 20/200 and OD 20/70. Pupils were normal. Intraocular pressures were 8 mm Hg OD and 18 mm Hg OS. Left sixth and a partial third cranial nerve palsies were also identified. An MR image of the orbit disclosed an enlarged left superior ophthalmic vein (SOV). Right common carotid artery (CCA) injection showed an abnormal early venous drainage into the cavernous sinus. The main fistula site was located in posterior cavernous segment fed by dural branches of meningohypophyseal trunk. The left SOV was opacified in retrograde fashion through the coronary sinus. Early venous drainage was also seen in the posterior compartment of the cavernous sinus (left more than the right), extending into the inferior petrosal sinuses (IPS) and followed by cerebellar cortical veins (Fig 1A, -B). Through a femoral venous access, a 6F Envoy angled guiding catheter (Cordis, Miami Lakes, Fla) was positioned in the left internal jugular vein, at the orifice of the left IPS. Under road-mapping, an Echelon 14 microcatheter (Micro Therapeutics) and FasDasher 14 microguidewire (Boston Scientific Target, Fremont, Calif) were positioned in the left SOV through the left IPS. A total of 14 coils, using a combination of GDCs (Boston Scientific Target), Matrix II coils (Boston Scientific, Fremont, Calif) and HydroCoils (MicroVention, Aliso Viejo, Calif), were deployed into the proximal left SOV and the anterior aspect of the cavernous sinus (Fig 1C). However, multiple residual fistulas were identified on the control angiogram after coil deployment. The tip of the microcatheter was then placed among the deployed coils. Eight percent EVOH (Onyx 34) was prepared on a Vortex mixer (Scientific Industries, Bohemia, NY) for 20 minutes. The microcatheter was flushed with normal saline, followed by filling of the catheter dead space with dimethyl-sufloxide (DMSO). Onyx was slowly injected into the microcatheter dead space for 90 seconds and then embolization was started. The Onyx 34 was initially injected into the coil mesh and midsegment of the SOV (Fig 1D). The Onyx penetrated into the anterior compartment followed by posterior compartment of the cavernous sinus on the left side. Finally, the Onyx penetrated into the coronary sinus and entire dural fistula site (Fig 1E, -F). When we observed the reflux, we held the injection 30 seconds to 2 minutes to solidify the Onyx polymerization; the injection was then restarted (the reflux-hold-reinjection technique). A total volume of 2.5 mL was delivered for 46 minutes. Postprocedural neurologic examination showed marked improvement in visual acuity and ocular pressure. A partial left fourth cranial nerve palsy remained.
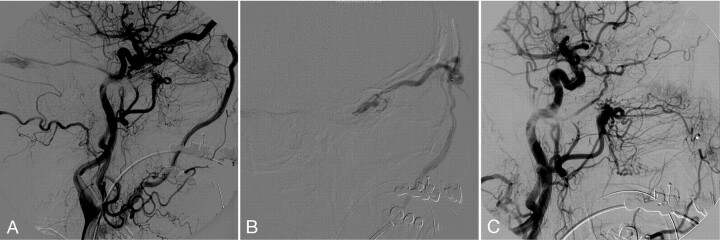
Fig. 1.
A, Pre-embolization right CCA. Frontal projection arterial phase shows the dural CCF with early venous drainage into the left cavernous sinus followed by the left IPS.
B, Lateral projection of right CCA injection late capillary phase shows retrograde filling of abnormally dilated left SOV.
C, Unsubtracted lateral projection image demonstrates transjugular-IPS venous access to the left SOV and deployed coils in the left SOV.
D, Lateral view of the right CCA injection shows the repositioned microcatheter to the anterior compartment of the cavernous sinus and partial embolization with Onyx.
E and F, Postembolization CCA angiogram. Frontal projection (E) and lateral projection (F) demonstrate complete obliteration of the fistula. Deployed coils in the left SOV and Onyx cast in the left cavernous and coronary sinuses block the fistula. There is no residual fistula.
Case 2
A 70-year-old woman developed progressively worsening headaches and left eye swelling during a 2-month interval. The patient also heard a whooshing noise in the head that became progressively louder. Although the patient denied double vision or any changes in her visual acuity, her left eye became progressively swollen. Physical examination showed significant proptosis and conjunctive chemosis on the left eye. The visual acuity was 20/40 bilaterally. Visual fields and extraocular movements were intact. No bruit was audible over the globe or temple.
CT angiography revealed enlargement of the left SOV. A carotid-cavernous fistula (CCF) was suspected on the basis of clinical and neuroimaging findings. A left common carotid angiogram revealed a dural CCF fed by meningohypophyseal trunk, accessory middle meningeal artery, and artery of foramen rotundum. There was high-flow venous drainage into the cavernous sinus, as well as a dilated left SOV and superior petrosal sinus (SPS) (Fig 2A). The ipsilateral IPS appeared to be occluded. We first attempted a transarterial approach through the abnormally dilated accessory middle meningeal artery. The small diameter of fistula prevented us from passing the microcatheter system. Therefore, a treatment decision was made to approach the fistula from the left SOV via the left facial vein. After obtaining venous access from the left common femoral vein, an 80-cm 6F Shuttle Select vascular sheath (Cook, Bloomington, Ind) was advanced into superior vena cava. A 6F angled Envoy guiding catheter was positioned in the left internal jugular vein. The ostium of the left facial vein was delineated and selected with the tip of the guiding catheter.
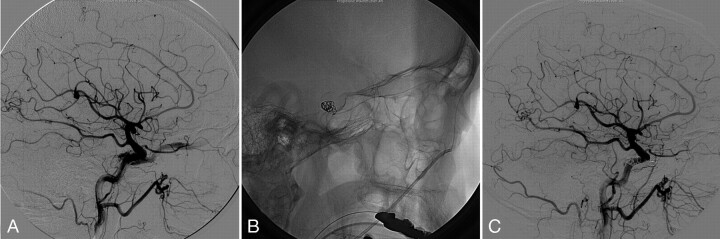
Fig. 2.
A, Left CCA angiogram lateral projection shows dural CCF fed by meningohypophyseal artery, accessory middle meningeal artery, and artery of foramen rotundum. The venous drainages are abnormally dilated left SOV and superior petrosal sinus. The IPS appeared occluded.
B, Superselective venogram of the left SOV lateral view demonstrates multiple catheter support system with a 6F angled Envoy guiding catheter in the proximal left facial vein, a 4F Tracker 38 catheter in the left angular vein, and an Echelon 10 microcatheter.
C, Postembolization with coils and Onyx angiogram of the left CCA shows complete occlusion of the fistula with no residual filling.
To obtain further support for the subsequent microcatheterization, a 4F Tracker 38 catheter (Boston Scientific) was advanced into the left facial vein followed by angular vein. A microcatheter system with Echelon 10 (Micro Therapeutics) and FasDasher 14 was navigated into the left SOV from the left angular vein (Fig 2B). First, coil embolization was performed to reduce the venous flow into the SOV before using liquid embolic material. Two GDC 10 soft 3 mm × 8 cm coils were deployed at the proximal aspect of SOV. Having obtained successful flow reduction within the SOV, the decision was made to perform Onyx embolization in the proximal segment of the SOV. Onyx and the microcatheter were prepared in the same way as described in case 1. Onyx 34 was slowly injected into the proximal segment of SOV and fistula site with the reflux-hold-reinjection technique under real-time road-mapping. A total of 0.7 mL of Onyx 34 was injected for 26 minutes. The Onyx cast well penetrated into the fistulas of SPS, and external carotid artery (ECA) from the anterior compartment of the cavernous sinus. The postembolization angiogram confirmed complete occlusion of the fistula (Fig 2C). A significant clinical improvement was obtained with resolution of pulsating tinnitus and eye symptoms.
Case 3
A 64-year-old right-handed woman had acute onset of double vision associated with mild-to-moderate retro-orbital pain. The symptoms progressed with right eye bulging, and redness. The patent denied recent history of head trauma. On examination, there was significant proptosis and chemosis on the right eye, and vertical and lateral movement of the right eye were limited. No bruit was audible. MR imaging and an MRA of the brain disclosed a prominent right SOV, consistent with dural CCF. A cerebral angiogram confirmed the right dural CCF with feeders from meningohypophyseal trunk, leading to early venous drainage into the left SOV (Fig 3A). The IPS and SPS appeared to be occluded secondary to thrombosis. There was no evidence of cortical venous reflux. No contribution of ECA was appreciated. Initial attempts to catheterize the fistula via the transfemoral venous approach through the IPS were unsuccessful. A different approach was subsequently selected to access the facial vein via the external jugular vein. The external jugular vein was selected with the tip of the 6F Envoy angled guiding catheter, then a 5F nontaper angled Glidecath XP (Terumo, Tokyo, Japan) was positioned in the facial vein. A Prowler 14 microcatheter (Cordis) and a FasDasher 14 microguidewire were successfully advanced into the cavernous sinus/SOV junction region. The cavernous dural fistula was occluded with 6 Trufill Orbits coils (Cordis; Fig 3B) followed by slow injection of Onyx 34. The postembolization angiogram showed complete occlusion of the fistula. The microcatheter was then withdrawn from the reflux Onyx cast (Fig 3C). However, a small piece of Onyx cast was fractured and dislodged in the distal segment of left SVO. A thin adhered Onyx crust was seen over the tip of the microcatheter. There was, however, no angiographic or clinical complication identified. Eye symptoms, including pain and chemosis, were resolved within 24 hours after the procedure.
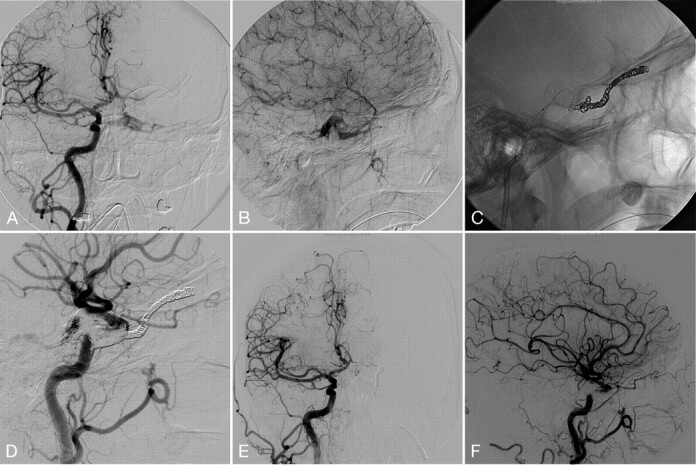
Fig. 3.
A, Right CCA injection lateral projection demonstrates dural CCF, with feeders from meningohypophyseal trunk with early venous drainage into the right SOV. The IPS is not visualized. No contribution of ECA was appreciated.
B, Transexternal jugular-facial venous access is seen on the lateral projection with a 5F Glidecath XP in the right facial vein and a Prowler 14 microcatheter in the cavernous sinus/SOV junction, and deployed coils.
C, Postprocedure right CCA angiogram lateral projection shows complete occlusion of the fistula with deployed coil mass and Onyx cast. A small piece of dislodged Onyx cast is also shown in the distal segment of right SOV.
Discussion
These 3 patients presented with typical symptoms of spontaneous dural CCF including progressing chemosis, proptosis, and painful ophthalmoparesis with diplopia, secondary glaucoma, and visual acuity impairment. Patient 2 also complained of pulsating tinnitus. Cerebral angiograms confirmed the diagnosis and revealed anatomic characteristics of dural fistulas and venous drainages.
Case 1 showed a typical transvenous IPS approach to the diseased cavernous sinus. In cases 2 and 3, the IPSs were angiographically occult and our attempts to reach fistula sites via the internal jugular vein–IPS failed. In general, the success rate of catheterization of IPS in cases with no visualization of IPS on angiogram is reportedly 30%–50%.3-6 Once the IPS is thrombosed, the transvenous access may be carried out via the SPS, facial vein, angular vein, pterygoid sinus, and SOV. Direct access to the SOV by surgical exposure3,7,8 or sonography-guided direct puncture of facial vein9 has been reported as a therapeutic alternative to enter the diseased cavernous sinus.10 We were able to reach the fistula site through the facial venous approach. We employed triple and quadruple axial catheter systems in case 3 and case 2, respectively, to reach the fistula sites. These systems provide increased stability and catheter support for an easier navigation of the microcatheter through peripheral serpiginous veins. Once the cavernous sinus is catheterized, the transvenous embolization has a high occlusion rate and low technical and clinical morbidities.3,5,11
All 3 patients were treated with a combination of Onyx liquid embolic agent and coil embolization. The deployment of detachable coils before the Onyx injection slowed the fistula flow and provided secured anchoring to the Onyx cast.
Onyx is a nonadhesive embolic agent, which is supplied in ready-to-use vials with mixture of EVOH, DMSO, and tantalum. Currently 6% (Onyx 18) are 8% (Onyx 34) EVOH concentration (dissolved in DMSO) are available (FDA-approved) in the United States for presurgical cerebral AVM embolization. Onyx is mechanically occlusive but nonadherent to the vessel wall. Its nonadhesive property eliminates the risk of gluing of the microcatheter to the vessels and allows a slow single injection of embolic agent with concomitant check angiograms. In case 1, we carefully repositioned the microcatheter into the proximal anterior compartment of the cavernous sinus, and additional Onyx injection was performed through the same catheter. Penetration and reflux of Onyx was monitored under real-time roadmap technique. When a proximal catheter reflux was seen, the injection was discontinued for 30 seconds and then resumed with a new roadmap (reflux-hold-reinjection technique). A complete CCF occlusion was achieved in all cases.
The catheter repositioning during embolization and the reflux-hold-reinjection technique cannot be performed in embolization with n-butyl cyanoacrylate (n-BCA). Prolonged injections are not possible and may cause risks of gluing the catheter because of the adhesive nature of n-BCA. The physical properties of Onyx are excellent to fill myriad fine fistulous communications observed in dural arteriovenous fistulas. The use of Onyx in treatment of a case with CCF has been reported by Arat et al in Turkey, where Onyx has been approved for clinical use since 1999.12
All our cases were cured in a single session of endovascular treatment with Onyx and coil embolization regimen. Pertinent literature shows that approximately one third of patients required multiple treatment sessions for optimal results.5 The deployed coil mesh furnishes slow yet secure and further penetration of the liquid embolic agent at the fistula sites. Animal study using a rete swine AVM model showed no histologic evidence of recanalization after 6 months of Onyx embolization.1 None of our patients had recurrent symptoms during 2-month follow-up.
The possible limitation of Onyx is that a limited number of DMSO-compatible delivery systems are available for clinical use.1,2 DMSO may dissolve polymers used in the structure or coating of many of the available microcatheters. Angiotoxicity with angionecrosis or vasospasm has also been considered as a possible adverse effect of DMSO. The slow injection of DMSO to disperse in the bloodstream is a safe method to avoid possible angiotoxicity, and the slow injection of the Onyx is the main success factor to obtain further penetration without reflux.
In conclusion, we presented 3 patients with dural CCF successfully treated with combined embolization with Onyx and detachable coils. Nonadhesive liquid embolic agent properties provide excellent penetration in spontaneous, complex, and fine dural CCFs. Slow and controlled endovascular delivery of Onyx with appropriate devices are key to avoid iatrogenia and improve anatomic and clinical outcomes.
References
- 1.Murayama Y, Vinuela F, Ulhoa A, et al. Nonadhesive liquid embolic agent for cerebral arteriovenous malformations: preliminary histopathological studies in swine rete mirabile. Neurosurgery 1998;43:1164–75 [DOI] [PubMed] [Google Scholar]
- 2.Jahan R, Murayama Y, Gobin YP, et al. Embolization of arteriovenous malformations with onyx: clinicopathological experience in 23 patients. Neurosurgery 2001;48:984–95; discussion 995–87 [DOI] [PubMed] [Google Scholar]
- 3.Quinones D, Duckwiler G, Gobin PY, et al. Embolization of dural cavernous fistulas via superior ophthalmic vein approach. AJNR Am J Neuroradiol 1997;18:921–28 [PMC free article] [PubMed] [Google Scholar]
- 4.Klisch J, Huppertz HJ, Spetzger U, et al. Transvenous treatment of carotid cavernous and dural arteriovenous fistulae: results for 31 patients and review of the literature. Neurosurgery 2003;53:836–56; discussion 856–37 [DOI] [PubMed] [Google Scholar]
- 5.Halbach VV, Higashida RT, Hieshima GB, et al. Transvenous embolization of dural fistulas involving the cavernous sinus. AJNR Am J Neuroradiol 1989;10:377–83 [PMC free article] [PubMed] [Google Scholar]
- 6.Vinuela F, Fox AJ, Debrun GM, et al. Spontaneous carotid-cavernous fistulas: clinical, radiological, and therapeutic considerations. Experience with 20 cases. J Neurosurg 1984;60:976–84 [DOI] [PubMed] [Google Scholar]
- 7.Berlis A, Klisch J, Spetzger U, et al. Carotid cavernous fistula: embolization via a bilateral superior ophthalmic vein approach. AJNR Am J Neuroradiol 2002;23:1736–38 [PMC free article] [PubMed] [Google Scholar]
- 8.Goldberg RA, Goldey SH, Duckwiler G, et al. Management of cavernous sinus-dural fistulas: indications and techniques for primary embolization via the superior ophthalmic vein. Arch Ophthalmol 1996;114:707–14 [DOI] [PubMed] [Google Scholar]
- 9.Berkmen T, Troffkin NA, Wakhloo AK. Transvenous sonographically guided percutaneous access for treatment of an indirect carotid cavernous fistula. AJNR Am J Neuroradiol 2003;24:1548–51 [PMC free article] [PubMed] [Google Scholar]
- 10.Meyers PM, Halbach VV, Dowd CF, et al. Dural carotid cavernous fistula: definitive endovascular management and long-term follow-up. Am J Ophthalmol 2002;134:85–92 [DOI] [PubMed] [Google Scholar]
- 11.Arteriovenous fistulae of the CNS. AJNR Am J Neuroradiol 2001;22:S22–25 [PMC free article] [PubMed] [Google Scholar]
- 12.Arat A, Cekirge S, Saatci I, et al. Transvenous injection of onyx for casting of the cavernous sinus for the treatment of a carotid-cavernous fistula. Neuroradiology 2004;46:1012–15 [DOI] [PubMed] [Google Scholar]