Abstract
SUMMARY: Kaposiform hemangioendothelioma is a rare vascular tumor and locally aggressive endothelial-derived spindle cell neoplasm, which occurs almost exclusively in infants and adolescents. Radiologically, hemangioendothelioma, including Kaposiform hemangioendothelioma, is seen as a highly vascularized well-enhancing tumor, but no characteristic findings differentiate Kaposiform hemangioendothelioma from other soft-tissue tumors, particularly when the tumor is too small to have any locally aggressive features or identifiable large vessels. We present a case of Kaposiform hemangioendothelioma in the internal auditory canal that had no differential features on initial MR images and rapidly grew into a huge mass in a few months.
Kaposiform hemangioendothelioma is a rare vascular tumor found predominantly in infancy and early childhood.1 It is often associated with Kasabach-Merritt syndrome, but not always.2 Concerning the histopathologic classification and biologic behavior of hemangioendothelioma, Kaposiform, retiform, and composite types of hemangioendothelioma are known to be intermediate malignant tumors, and epithelioid hemangioendothelioma, to be a highly malignant tumor.3 Kaposiform hemangioendothelioma is mostly located in the retroperitoneum and skin, but it can occur occasionally in the head and neck regions, mediastinum, and deeper soft tissues of trunk and extremities, whereas other hemangioendotheliomas mostly involve the distal extremities or skin.3 To our knowledge, there has been no report of Kaposiform hemangioendothelioma appearing within the cranial vault or in the skull base. We present clinical and radiologic findings of a rapidly growing Kaposiform hemangioendothelioma in the internal auditory canal.
Case Report
A 6-month-old male infant presented with facial asymmetry associated with left facial nerve palsy. The baby had been born to healthy parents at 40 weeks of gestation by normal delivery. He had no intrauterine disease or perinatal problem. He was vaccinated as scheduled, did not undergo any surgery, and was not admitted for other diseases. On neurologic examination, facial asymmetry involving the unilateral forehead and cheek was noted, particularly when he was smiling. Facial nerve palsy of the peripheral type was suspected. Findings of laboratory studies for blood cell count and coagulation were not remarkable. Cranial imaging was performed to reveal any lesion causative of the facial nerve palsy.
Temporal bone CT showed a slight enlargement of the left internal auditory canal, but there was no bone erosion or destruction. On MR images, a small strong enhancing nodule was seen in the left internal auditory canal (Fig 1). Radiologic diagnosis for the nodule was facial or acoustic nerve schwannoma or hemangioma. However, this patient had no stigmata of neurofibromatosis that might be related to the schwannoma on physical, familial, or imaging basis. The patient was too young to receive any intervention for diagnostic or therapeutic purposes. Therefore, only a follow-up MR imaging was planned. It was performed after 6 months and unexpectedly showed a huge bone-destructing tumor at the original site, which compressed the brain stem and left temporal lobe without parenchymal signal-intensity changes but did not cause neurologic symptoms related to the compression. Multifocal hemorrhages were present within the tumor, and it was strongly enhancing with prominent intratumoral vessels (Fig 2). Clinically, left facial palsy still existed and progressive hearing loss had occurred. Findings of neurologic examination, otherwise, were unremarkable. A malignant peripheral nerve sheath tumor or malignant vascular tumor, including aggressive hemangioendothelioma or angiosarcoma, was considered at this time. To reveal the histopathologic diagnosis of the mass, an incisional biopsy was performed, resulting in the diagnosis of Kaposiform hemangioendothelioma.
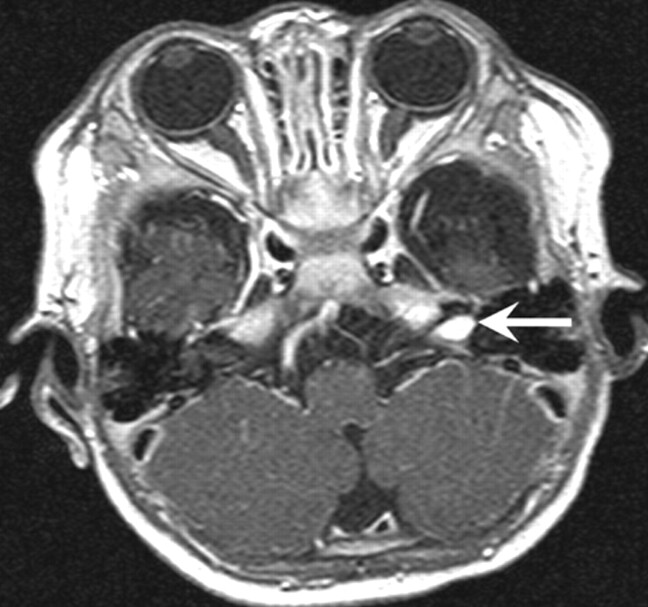
Fig 1.
Initial MR image in a 6-month-old male infant. Gadolinium-enhanced T1-weighted axial image shows a small homogenous enhancing nodule in the left internal auditory canal (arrow).
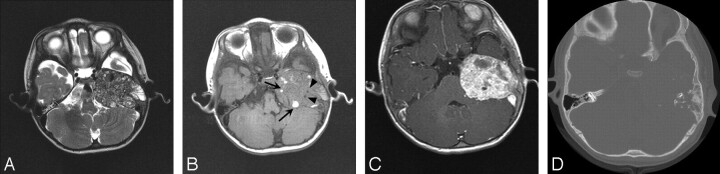
Fig 2.
Follow-up MR images obtained 6 months after initial presentation.
A, Axial T2-weighted image shows a large heterogeneous expansile mass at the temporal bone.
B, Axial T1-weighted image shows intratumoral multifocal hemorrhages (arrows) and vascular flow voids that are related to hypervascularity (arrowheads).
C, Gadolinium-enhanced T1-weighted axial image shows a strongly enhancing tumor, destruction of the petrous bone, and compression of the brain stem and medial temporal lobe.
D, Temporal bone CT reveals a large soft-tissue mass with severe bone destruction in left petrous bone.
Decompressive surgical resection was planned to prevent the tumor from causing neurologic deficits associated with the rapid growth and parenchymal compression. Immediately before surgery, preoperative embolization was performed to reduce hypervascularity. Polyvinyl alcohol (PVA) particles were administered through multiple external carotid artery branches to the tumor; this procedure resulted in near-total devascularization on postembolization angiography (Fig 3). Surgical excision was very difficult because of profound bleeding despite the preoperative embolization. Therefore, only a partial removal was undertaken, and the histopathologic specimen showed irregular lobules or sheets of poorly formed small vascular channels infiltrating and entrapping normal tissue (Fig 4). A vascular origin of these cells was confirmed by their positive test for CD34, a specific endothelial marker. The final diagnosis was also Kaposiform hemangioendothelioma, and the patient was discharged on continuing oral prednisolone and interferon.
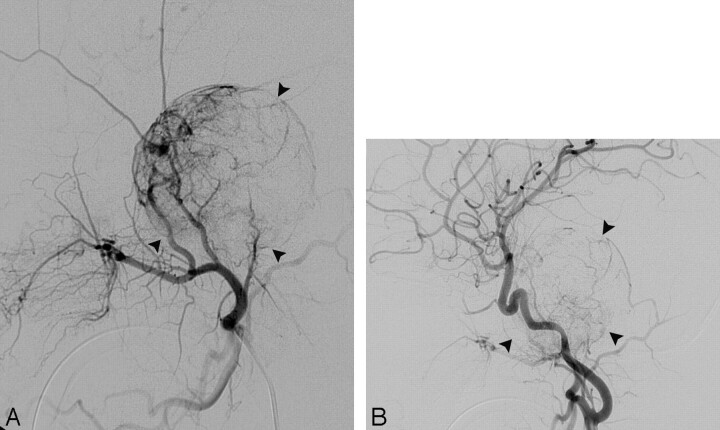
Fig 3.
Lateral projection of pre-embolization external carotid angiogram (A) reveals a hypervascular tumor (arrowheads) occupying the temporomastoid region, and postembolization common carotid angiogram (B) shows near-total devascularization of the tumor (arrowheads). PVA particles were used to occlude the intratumoral vessels.
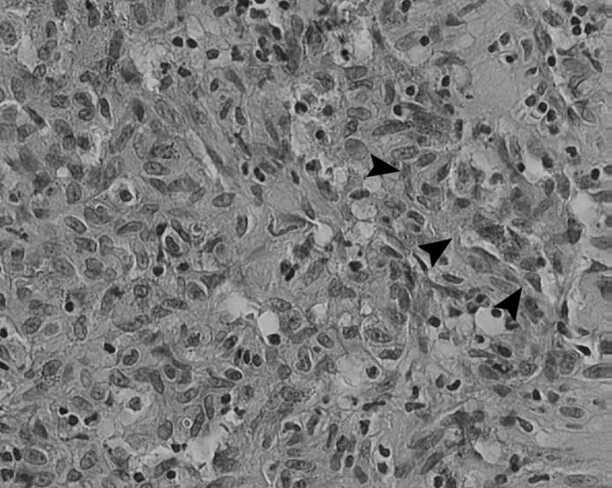
Fig 4.
Photomicrograph of histopathologic specimen shows fascicles of spindle cells (arrowheads) admixed with small vascular channels, which is characteristic of kaposiform hemangioendothelioma (hematoxylin-eosin, original magnification ×200).
Discussion
Zukerberg et al4 introduced the term “Kaposiform hemangioendothelioma” in 1993 as a distinctive lesion in childhood. In contrast to the fact that most vascular tumors occurring in childhood, including juvenile hemangioma, cavernous hemangioma, and angiomatosis, are benign, Kaposiform hemangioendothelioma shows aggressive behavior and no tendency to regress spontaneously. It is characterized by a locally aggressive growth without distant metastasis and, for this reason, has been classified as an intermediate malignancy.4
It typically occurs in infancy and the first decade of life, but adult cases are increasingly recognized.3 The peritoneum or retroperitoneum is known to be a predominant location, and other sites such as the upper and lower extremities, chest wall, face, ear, and temporal bone could be also involved.2 However, intracranial or cranial nerve origin of Kaposiform hemangioendothelioma is extremely rare, and to our knowledge, our case is the first report of Kaposiform hemangioendothelioma involving the internal auditory canal in the English literature.
Kaposiform hemangioendothelioma is often associated with Kasabach-Merritt phenomenon, a condition characterized by profound thrombocytopenia, life-threatening hemorrhage, and lymphangiomatosis.2 A previous report of Kaposiform hemangioendothelioma involving the right ear and mastoid bone showed the association of the case with Kasabach-Merritt phenomenon.1 However, biologic behavior and associated coagulopathy are greatly influenced by the site and extent of disease.4 Furthermore, Lyons et al2 reported that 44% of cases with Kaposiform hemangioendothelioma did not show Kasabach-Merritt phenomenon, as in our case.
Histologically, Kaposiform hemangioendothelioma consists of irregular, infiltrating nodules of compressed vessels, which modulate between areas resembling capillary hemangioma and Kaposi sarcoma.2 Kaposiform hemangioendothelioma is differentiated from Kaposi sarcoma and capillary hemangioma, in that there is a lack of periodic-acid-Schiff–positive globules and well-formed spindle cell fascicles, respectively.1
In general, a large Kaposiform hemangioendothelioma complicated by Kasabach-Merritt syndrome does not respond well to therapy, particularly when it occurs in intraabdominal sites.3 The treatment of choice for Kaposiform hemangioendothelioma has been complete surgical excision, occasionally combined with radiation.5, 6 Medical treatment by using interferon, prednisolone, or vincristine may also be applied with some effectiveness.1, 2, 7, 8
Our case was confusing in the initial diagnosis because it occurred in infancy and was seen as only a small enhancing nodule in the internal auditory canal, without characteristic features. A malignant peripheral nerve sheath tumor or malignant vascular tumor could not be suggested until follow-up imaging. The rapid growth and bone destruction led us to consider a malignant tumor. Among the tumors arising from the internal auditory canal, acoustic and facial nerve schwannomas are the most common but are extremely rare in children unless related to neurofibromatosis. Meningioma was also unlikely because the tumor was confined to the internal auditory canal in the initial images and occurred in infancy.9 Vascular lesions such as hemangioma should be included in the differential diagnosis, although it is rare in the internal auditory canal.10 Finally, metastatic tumors in the internal auditory canal from breast cancer, nasopharyngeal cancer, and colon cancer have been reported in adult cases, and they appear only as well-enhancing masses.11
Radiologically, hemangioendothelioma in the head and neck regions has been reported to have an aggressive destructive tendency, particularly at the temporomastoid region.1, 6 Ibarra et al5 described hemangioendothelioma as a large well-defined expansile osteolytic lesion involving the temporal bone with hemorrhagic foci on CT and MR images. Kaposiform hemangioendothelioma may contain flow voids of vascular structures indicating a hypervascular tumor.5 Panow et al12 reported Kaposiform hemangioendothelioma in the mandible, showing infiltrative mass formation on MR imaging and spiculating features on CT. Doppler sonography of hemangioendothelioma shows an ill-defined heterogeneous lesion with intratumoral high vascularity (2–5 vessels/cm2) and high systolic Doppler shift.13 Despite these reported imaging findings, Kaposiform hemangioendothelioma appearance may be variable, particularly in relation to the tumor size; a small Kaposiform hemangioendothelioma in its early stage might be shown as a nonspecific benign-looking tumor.
As shown in our case, a small enhancing nodule in the internal auditory canal seen on MR images, particularly in an infant, does not always mean an usual benign tumor. Therefore, a short-term follow-up imaging should be performed to determine malignant hypervascular characteristics of the tumor. The earlier diagnosis for the malignant hypervascular tumor may enable total resection with minimum intraoperative bleeding.
References
- 1.Lalaji TA, Haller JO, Burgess RJ. A case of head and neck kaposiform hemangioendothelioma simulating a malignancy on imaging. Pediatr Radiol 2001;31:876–78 [DOI] [PubMed] [Google Scholar]
- 2.Lyons LL, North PE, Mac-Moune Lai F, et al. Kaposiform hemangioendothelioma: a study of 33 cases emphasizing its pathologic, immunophenotypic, and biologic uniqueness from juvenile hemangioma. Am J Surg Pathol 2004;28:559–68 [DOI] [PubMed] [Google Scholar]
- 3.Tsang WY. Kaposiform hemangioendothelioma. In: Fletcher C, Unni K, Mertens F. Pathology and Genetics of Tumors of Soft Tissue and Bone. Lyon, France: IARC Press;2002. :163–64
- 4.Zukerberg LR, Nickoloff BJ, Weiss SW. Kaposiform hemangioendothelioma of infancy and childhood: an aggressive neoplasm associated with Kasabach-Merritt syndrome and lymphangiomatosis. Am J Surg Pathol 1993;17:321–28 [DOI] [PubMed] [Google Scholar]
- 5.Ibarra RA, Kesava P, Hallet KK, et al. Hemangioendothelioma of the temporal bone with radiologic findings resembling hemangioma. AJNR Am J Neuroradiol 2001;22:755–58 [PMC free article] [PubMed] [Google Scholar]
- 6.Hardisson D, Prim MP, De Diego JI, et al. Kaposiform hemangioendothelioma of the external auditory canal in an adult. Head Neck 2002;24:614–17 [DOI] [PubMed] [Google Scholar]
- 7.Chung MT, Chen CH, Chiu CH, et al. Successful nonoperative therapy for Kaposiform hemangioendothelioma involving the neck: report of 1 case. Otolaryngol Head Neck Surg 2003;129:605–07 [DOI] [PubMed] [Google Scholar]
- 8.Haisley-Royster C, Enjolras O, Frieden IJ, et al. Kasabach-Merritt phenomenon: a retrospective study of treatment with vincristine. J Pediatr Hematol Oncol 2002;24:459–62 [DOI] [PubMed] [Google Scholar]
- 9.Massinger C, Gawehn J, Keilmann A. Acoustic schwannoma with progressive hearing loss in children: a case report [in German]. Laryngorhinootologie 2003;82:92–96 [DOI] [PubMed] [Google Scholar]
- 10.Barrera JE, Jenkins H, Said S. Cavernous hemangioma of the internal auditory canal: a case report and review of the literature. Am J Otolaryngol 2004;25:199–203 [DOI] [PubMed] [Google Scholar]
- 11.Huang TW, Young YH. Differentiation between cerebellopontine angle tumors in cancer patients. Otol Neurotol 2002;23:975–79 [DOI] [PubMed] [Google Scholar]
- 12.Panow C, Berger C, Willi U, et al. MRI and CT of a hemangioma of the mandible in Kasabach-Merritt syndrome. Neuroradiology 2000;42:215–17 [DOI] [PubMed] [Google Scholar]
- 13.Dubois J, Garel L, David M, et al. Vascular soft-tissue tumors in infancy: distinguishing features on Doppler sonography. AJR Am J Roentgenol 2002;178:1541–45 [DOI] [PubMed] [Google Scholar]