Abstract
SUMMARY: We present a case of traumatic pseudoaneurysm of the middle meningeal artery (demonstrated on CT angiogram) associated with epidural hematoma that spontaneously resolved without treatment. Follow-up CT angiogram and conventional angiogram done 2 weeks later demonstrated complete resolution of the pseudoaneurysm. The literature suggests that these lesions require urgent treatment because they have a high mortality rate. We highlight the lack of proper data regarding the natural history of this disease and therefore lack of treatment guidelines.
Traumatic pseudoaneurysms of the middle meningeal artery (MMA) are rare occurrences that are usually associated with an underlying skull fracture.1 Although they are rare, they have a high mortality rate (20%) and hence need to be recognized early.1 They typically present as acute or delayed epidural hematomas but can be associated with subdural, subarachnoid, or even intracerebral bleeds.1,2 Treatment options are usually surgical closure of the hole in the vessel wall or endovascular occlusion.1,3,4
Case Report
A 25-year-old man presented to the emergency department of our hospital with history of head injury during a snowmobile crash. The Glasgow Coma Scale score was 15/15, and there were no focal localizing neurologic signs on clinical examination. Plain CT scans of the head and cervical spine were performed that revealed a left temporal bone fracture with underlying epidural hematoma, right frontal bone fracture with underlying subdural hematoma, and comminuted fracture of the left lateral mass of C2 vertebra. CT angiography (CTA) of the neck and intracranial vessels was performed because of concern about possible vertebral artery injury from the C2 fracture. The CTA demonstrated no vertebral artery injury but showed a pseudoaneurysm arising from the left MMA adjacent to the left temporal epidural hematoma (Fig 1A, -B). This MMA pseudoaneurysm was presumed to be related to the temporal bone fracture and was probably the cause of the epidural hematoma.
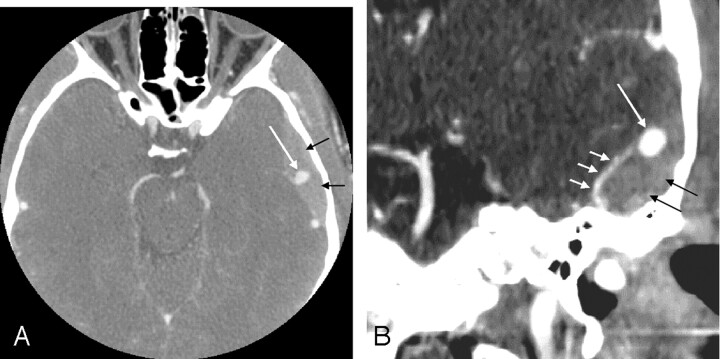
Fig 1.
CT angiogram of the brain in axial plane (A) with coronal maximum intensity projection (MIP) reconstructions (B), done at the initial time of presentation, reveals a pseudoaneurysm (long white arrow) arising from the left middle meningeal artery (MMA) (short white arrows). Left temporal epidural hematoma is also visualized (black arrows).
The patient was managed conservatively and remained clinically stable. After 2 weeks, CTA of the brain was repeated to re-evaluate the pseudoaneurysm and determine the further course of action. The CTA showed complete resolution of the pseudoaneurysm and decrease in size of the epidural hematoma (Fig 2A, -B). For confirmation of this finding, a conventional digital subtraction angiogram was performed via a right transfemoral approach, and the left external carotid artery and the left MMA were selectively catheterized. Selective injections of the left external carotid artery and the left MMA showed normal filling of the MMA and its branches with no filling of the pseudoaneurysm (Fig 3). The rest of the cerebral angiogram was also unremarkable. The patient was discharged from the hospital with no neurologic deficits. A 3-month follow-up CTA showed no recurrence of the pseudoaneurysm.
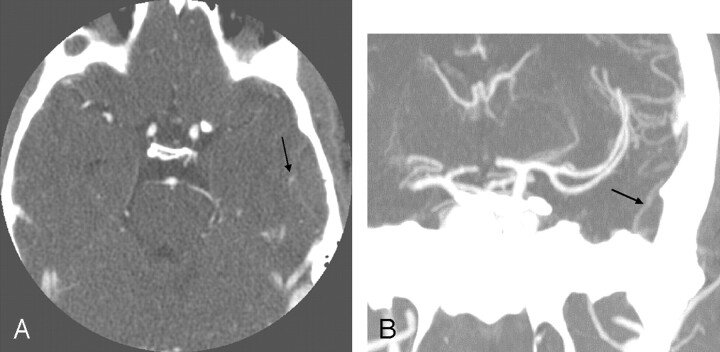
Fig 2.
CT angiogram of the brain in axial plane (A) with coronal maximum intensity projection (MIP) reconstructions (B), performed 2 weeks after the acute event, shows resolution of the previously seen pseudoaneurysm arising from the middle meningeal artery (MMA) (arrow).
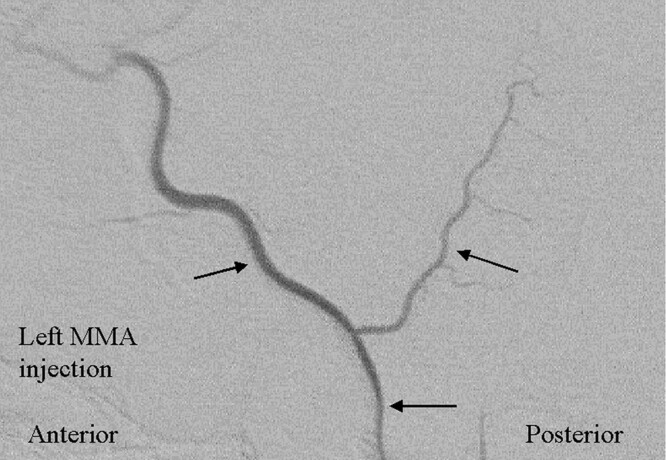
Fig 3.
Superselective left middle meningeal artery (MMA) angiogram in lateral projection shows normal filling of the MMA and its anterior and posterior divisions (arrows) with no pseudoaneurysm demonstrated.
Discussion
Aneurysms of the MMA are rare and are of 2 types: the true aneurysm and the pseudoaneurysm.1 The true aneurysm is usually seen with pathologic conditions such as Paget disease,5 hypertension,6 meningioma,7 and dural arteriovenous malformations8 and shares the same histologic characteristics with cerebral aneurysms. Pseudoaneurysms, on the other hand, are associated with a skull fracture causing a tear in the arterial wall in most cases.1 From a histologic perspective, there is only fibroconnective tissue surrounding the hole in the wall, and none of the normal arterial layers are present in the pseudoaneurysm.1
Meningeal pseudoaneurysms usually arise from the MMA or from one of its 2 branches.1 They are known to have specific angiographic characteristics, which include peripheral location, absence of neck, and filling and emptying in a delayed, slow fashion during an angiogram.9 For this reason they may be visible only in the late phase of an external carotid arteriogram.9
Meningeal pseudoaneurysms typically present with acute or delayed epidural hematoma, but they can also be associated with subdural, subarachnoid, or intracerebral bleeds.1, 2 The natural evolution of these lesions is not clear. One possible course of events includes the initial formation of a tear in the arterial wall that is not large enough to result in an epidural hematoma. There is then formation of clot that contains further leakage of blood and results in the formation of a pseudoaneurysm. This pseudoaneurysm can rupture in a delayed fashion, resulting in an intracranial hematoma and clinical deterioration. This series of events has been reported with meningeal pseudoaneurysms in which the patients typically recovered completely after the initial trauma but deteriorated clinically in a delayed fashion from secondary rupture of the pseudoaneurysm.9, 10 The initial tear in the arterial wall can also be large enough to cause an acute intracranial hematoma, and a pseudoaneurysm can result from the fresh clot walling off the tear.2, 11 This was probably the initial occurrence in our patient. Meningeal pseudoaneurysms have also been diagnosed without any associated ipsilateral intracranial hematoma in a few patients and were considered unruptured in these patients.10, 12, 13 Pseudoaneurysms of the MMA can also be associated with arteriovenous fistula, though this is rare, and both of these conditions carry a risk of delayed hemorrhage.4, 12, 14
In contrast to nontraumatic true aneurysms, which have a good prognosis, the prognosis in traumatic pseudoaneurysms has been reported to be generally poor.1 A mortality rate of 20% has been quoted in the literature, which has been partly attributed to the severity of the initial head trauma.1 These data, however, are based on a review of literature and a collection of only case reports. It is likely to be limited in its ability to comment on the natural history of disease. Based on a review of literature, the true frequency of these pseudoaneurysms is unclear; whether the simple presence of a pseudoaneurysm is an indication for intervention is also unclear. Because only a few cases of MMA pseudoaneurysms are reported in the literature and the incidence of incidental pseudoaneurysms is essentially unknown, there are no definite treatment guidelines. Some authors recommend that treatment be carried out without any delay because of the risk of secondary rupture.1, 4 Both surgical and endovascular therapies (coils, glue) have been performed successfully.1, 3, 4 In our patient, conservative management was followed for the first 2 weeks and then the pseudoaneurysm was re-evaluated; however, both the CTA and conventional angiogram revealed that the pseudoaneurysm had resolved, probably as a result of spontaneous thrombosis. Spontaneous thrombosis of MMA pseudoaneurysm is a rare event that has been reported before by Namba et al.15 Because the pseudoaneurysm had spontaneously resolved, we pursued no further aggressive management.
In conclusion, it is important to be aware of possible meningeal pseudoaneurysms in cases of head trauma, especially if the fracture crosses the expected location of the middle meningeal artery. In contradistinction to our case, the literature seems to suggest a poor natural history of disease. The literature, however, is limited to case reports, and the incidence of these lesions, including their spontaneous resolution, is unknown. It is possible that more of these lesions will be detected with increased use of noninvasive vascular imaging. More work is required to better delineate the natural history of this condition and to come up with treatment guidelines.
References
- 1.Bruneau M, Gustin T, Zekhnini K, et al. Traumatic false aneurysm of the middle meningeal artery causing an intracerebral hemorrhage: case report and literature review. Surg Neurol 2002;57:174–78 [DOI] [PubMed] [Google Scholar]
- 2.Albert FK, Oldenkott P, Sigmund E. Subarachnoid hemorrhage and intracerebral hematoma in injury of the middle meningeal artery. Zentralbl Neurochir 1989;50:153–56 [PubMed] [Google Scholar]
- 3.Okumura H, Tenjin H, Ueda S. A case of traumatic pseudoaneurysm of the middle meningeal artery treated with endovascular surgery. No Shinkei Geka 1998;26:929–33 [PubMed] [Google Scholar]
- 4.Tsutsumi M, Kazekawa K, Tanaka A, et al. Traumatic middle meningeal artery pseudoaneurysm and subsequent fistula formation with the cavernous sinus: case report. Surg Neurol 2002;58:325–28 [DOI] [PubMed] [Google Scholar]
- 5.New PF. True aneurysm of the middle meningeal artery, cranial Paget’s disease and hypertension: a triad. Clin Radiol 1967;18:154–57 [DOI] [PubMed] [Google Scholar]
- 6.Sandin III JA, Salamat MS, Baskaya M, et al. Intracerebral hemorrhage caused by the rupture of a nontraumatic middle meningeal artery aneurysm: case report and review of the literature. J Neurosurg 1999;90:951–54 [DOI] [PubMed] [Google Scholar]
- 7.O’Neill OR, Barnwell SL, Silver DJ. Middle meningeal artery aneurysm associated with meningioma: case report. Neurosurgery 1995;36:396–98 [DOI] [PubMed] [Google Scholar]
- 8.Kahara VJ. Middle meningeal artery aneurysm: case illustration. J Neurosurg 1999;91:518. [DOI] [PubMed] [Google Scholar]
- 9.Higazi I, El-Banhawy A, El-Nady F. Importance of angiography in identifying false aneurysm of the middle meningeal artery as a cause of extradural hematoma: case report. J Neurosurg 1969;30:172–76 [DOI] [PubMed] [Google Scholar]
- 10.Aoki N, Sakai T, Kaneko M. Traumatic aneurysm of the middle meningeal artery presenting as delayed onset of acute subdural hematoma. Surg Neurol 1992;37:59–62 [DOI] [PubMed] [Google Scholar]
- 11.Toro VE, Fravel JF, Weidman TA, et al. Posttraumatic pseudoaneurysm of the posterior meningeal artery associated with intraventricular hemorrhage. AJNR Am J Neuroradiol 1993;14:264–66 [PMC free article] [PubMed] [Google Scholar]
- 12.Salazar Flores J, Vaquero J, Garcia Sola R, et al. Traumatic false aneurysms of the middle meningeal artery. Neurosurgery 1986;18:200–03 [DOI] [PubMed] [Google Scholar]
- 13.Treil J, Morel C, Bonafe A, et al. Traumatic rupture of the middle meningeal artery: angiographic appearances. J Neuroradiol 1977;4:399–414 [PubMed] [Google Scholar]
- 14.Sicat LC, Brinker RA, Abad RM, et al. Traumatic pseudoaneurysm and arteriovenous fistula involving the middle meningeal artery. Surg Neurol 1975;3:97–103 [PubMed] [Google Scholar]
- 15.Namba K, Ban S, Oda Y, et al. [Case of traumatic false aneurysm of the middle meningeal artery with epidural hematoma: comparison with a case resulting in spontaneous thrombosis] [in Japanese]. Rinsho Shinkeigaku 1972;12:165–70 [PubMed] [Google Scholar]