Abstract
The etiologies of unilateral exophthalmos are multiple, rarely represented by an intra- or extra-conical vascular mass. Orbito-palpebral varixes are rare (2% of orbital masses) and represent a main cause of unilateral intermittent exophthalmos, often of an inflammatory nature.
We report a Case of right orbito-palpebral varix in a 65-year-old adult, with no particular history, evolving for 2 years. The ophthalmological examination showed a right palpebral mass, extended to the right external canthus, with palpebral collateral circulation, moderate right ptosis with exophthalmos, non-axial, non-pulsatile, without thrill, painless, without complication, without visual deficit. A vascular mass was suspected and MRI revealed a right orbito-palpebral varix with temporal extension, confirmed by ANGIO-MRI. The latter also allowed to search for a cerebral venous malformation, an encephalocele or a bone defect, associated and also to eliminate differential diagnoses (tumor, arteriovenous fistula …). Color Doppler ultrasound in the proclive position confirmed the diagnosis of orbital varices. A preventive low-dose anticoagulant treatment was started to avoid thrombosis, with therapeutic abstention in the absence of complications. A rigorous monthly follow-up in consultation is ensured.
Orbito-palpebral varices are characterized by an extensive posterior intra-orbital character, often during their evolution and imposes a strict surveillance. In Case of complication (thrombosis, hemorrhage, pain, compressive signs of the optic nerve), surgical removal or sclerosis of the varix can be envisaged with disappointing results (recurrence, hemorrhage).
Keywords: Exophthalmos, Orbit, Imaging, Varix
Highlights
-
•
Orbito-palpebral varixes are rare and represent a main cause of unilateral intermittent exophthalmos.
-
•
Imaging under appropriate conditions is essential to establish the diagnosis and eliminate differential diagnoses.
-
•
Orbito-palpebral varices are characterized by an extensive posterior intra-orbital character, often during their evolution and imposes a strict surveillance.
-
•
Surgery is mainly indicated for symptomatic patients with complications or aesthetic damage.
1. Introduction
Unilateral exophthalmos is most often due to an expansive intraorbital process, with more or less insidious development depending on the etiology. The etiologies of unilateral exophthalmos are multiple, rarely represented by an intra- or extra-conical vascular mass and representing about 10% of orbital tumors [1,2]. Orbital varixes are rare, representing 2% of orbital expansive processes and are due to proliferation and dilation of intraorbital venous elements [2,3]. They are revealed by an intermittent exophthalmos aggravated by effort or the proclive position. Imaging, in particular MRI with injected sequences or angiography but also color Doppler ultrasound, allows the diagnosis to be made. The management is variable, discussed on a Case-by-case basis, and consists of either abstention with surveillance or aggressive surgery or sclerotherapy.
In this Case, we report a case of orbito-palpebral varices of insidious evolution, with unusual extra-orbital palpebral extension. We will discuss the diagnostic difficulties and therapeutic possibilities.
2. Case presentation
Our work consists of a single Case report and has been reported in accordance with SCARE 2020 criteria [4].
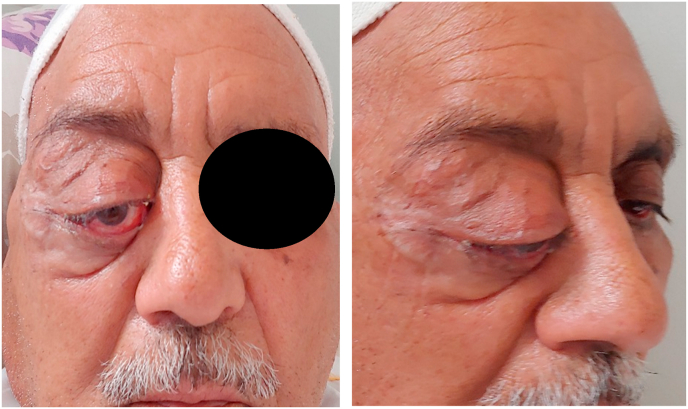
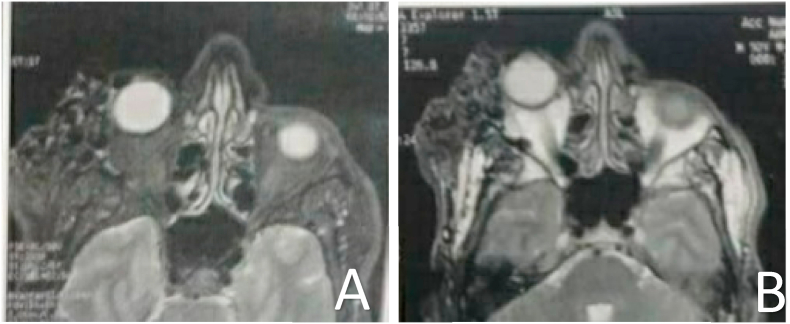
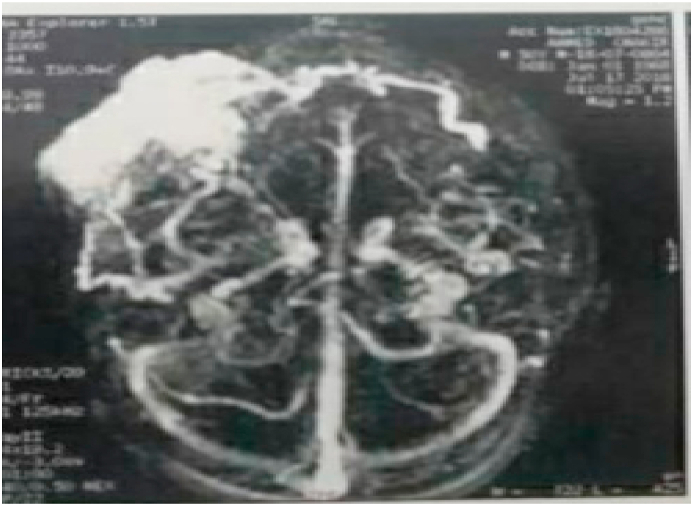
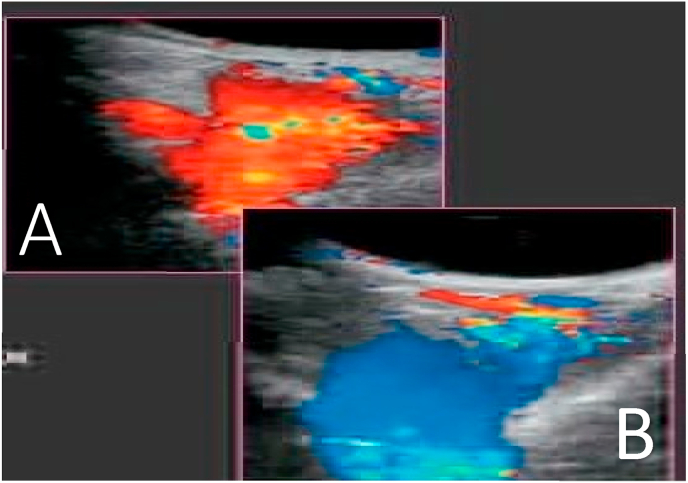
This is a 65-year-old man from a disadvantaged social background, known to be a type 2 diabetic for 30 years, balanced on monotherapy with self-medicated oral antidiabetic drugs. He was referred to the ophthalmologic emergency room by his diabetologist who had seen him for almost 3 years to control his diabetes. His physician referred him for management of a unilateral inflammatory exophthalmos. Questioning revealed an insidious evolution over the past 2 years of a left upper palpebral swelling extending temporally, initially intermittent with a postural character, but becoming constant and rapidly increasing in volume over the past 6 months. He reported no notion of trauma, no ocular symptomatology, and no rhinological history. The ophthalmological examination revealed a moderate right ptosis, with a significant exophthalmos, non-axial, non-pulsatile, without thrill, painless. Hypotropia with limited globe elevation is noted, without lagophthalmos. A soft, painless right palpebral mass extending to the right external canthus with palpebral collateral circulation was also observed [Fig. 1]. No perilimbic conjunctival abnormality was found, especially in the medusa head. The visual acuity of the right eye is 4/10 without correction. The ocular tone is normal, at 15 mmHg on the Goldmann tonometer. The anterior segment examination revealed a small inferior exposure keratitis, without anterior chamber reaction, a preserved photo-motor reflex (direct and consensual) with a grade 2 cortical cataract. At the fundus, the papilla was normal with a flat retina, without visualization of choroidal folds. The examination of the contralateral eye was without notable abnormality with a distance visual acuity of 5/10 without correction, and a grade 2 cortical cataract, normal fundus. The specialized examination of the rhinology, the cavum and the cranial pairs was normal. Orbital CT revealed a polylobed left palpebral and temporal formation, poorly limited, without intimate contact with the intraconical contents, without calcification within it. MRI confirmed the presence of a subcutaneous palpebral and left temporal vascular formation, measuring 73 mm in width and 31 mm in anteroposterior diameter, with multiple serpiginous structures in T1 and T2 hyposignal [Fig. 2A and B] enhanced after contrast injection, related to a vascular platoon [Fig. 3]. The MRI angiographic sequence showed drainage at the level of the facial vein, with no other involvement [Fig. 4]. The color Doppler ultrasound revealed a soft, anechoic, depressible mass with increasing volume during the Valsalva maneuver [Fig. 5]. In view of all these data, the diagnosis of orbito-palpebral varix with extra-conical development and temporal extension was made. The diagnosis and prognosis were clearly explained to the patient. Our therapeutic attitude was to institute a low-dose anticoagulant treatment of 4000 IU/day to prevent thrombosis and we opted for a conservative attitude with strict surveillance. The indication was mainly based on the fact that the lesion did not extend intra-orbitally without any notable complication, despite the aesthetic prejudice that did not bother the patient. The patient is warned of possible complications such as bleeding, pain or serious ocular complications, requiring an emergency intervention. A local ocular treatment is instituted, consisting of eyewash with saline 3 times a day, an antibiotic eye drop 4 times a day for 10 days, single-dose artificial tears and vitamin A-based ophthalmic ointment, as well as the use of Steri-Strip in the evening at bedtime. He is also followed up in a specialized orbito-palpebral consultation for his varixes every month. In addition, the patient is readmitted to his primary care physician for follow-up of his diabetes.
Fig. 1.
Right exophthalmos with upper palpebral mass and presence of palpebral collateral venous circulation.
Fig. 2.
MRI in T1(A) and T2 (B) axial slices showing a palpebral and temporal vascular formation in hyposignal.
Fig. 3.
MRI in axial slices after injection of gadolinium in FAT-SAT, showing intense enhancement of the lesion characterizing a vascular platoon.
Fig. 4.
Angio-MRI sequence showing the drainage of the varix in the facial vein.
Fig. 5.
Color Doppler image of an orbital varix (A: filling time, B: emptying time)
2.1. Clinical discussion
The etiologies of unilateral exophthalmos are multiple, rarely represented by an intra- or extra-conical vascular mass. Vascular tumors and anomalies account for 10% of orbital tumors [1,5]. Among these tumors, hemangiomas, lymphangiomas, and orbital varixes are the most common [2,6]. Orbital varixes are rare, representing 2% of orbital expansive processes. They are congenital venous malformations, characterized by the proliferation of venous elements, associated with the major dilatation of one of the orbital veins. They are often of congenital or idiopathic origin, occurring and evolving insidiously [[1], [2], [3], [4], [5], [6]]. Orbital varixes may also occur post-traumatically. They may be associated with a hemangioma or secondary to an arteriovenous fistula [5]. Their clinical presentation is variable. It is most often an intermittent exophthalmos occurring during exertion, the proclive position or the Valsalva maneuver. This exophthalmos is non-pulsatile, positionally variable and sometimes painful [1,3,5]. It is a more or less characteristic exophthalmos often, in the absence of complications. However, when the location of the varicose vein is not exclusively intra-orbital, or when there is an extra-orbital palpebral extension, the signs can be noisy with a significant exophthalmos, constant in change of position, possibly inflammatory and a palpebral mass can be palpated. This is the Case of the patient reported here, with even visualization of a palpebral collateral circulation. Even if the clinical picture is quite evocative, imaging remains mandatory to eliminate a differential diagnosis (tumor, arteriovenous fistula, …) and to look for a cerebral venous malformation, an encephalocele or an associated bone defect (4%). This imaging includes CT and MRI which are quite complementary, but also color Doppler ultrasound, all performed in different positions. By comparing the decubitus and procubitus views, a formation that increases in volume with the Valsalva maneuver or in procubitus position, and that is strongly enhanced with the presence of suggestive calcifications: phleboliths [1,5], can be observed. MRI or CT can also detect thrombosed areas, which are inconstant but indicate the aggressive nature of the lesion. However, the ANGIO-MRI sequence is very important, in that it allows objectification of venous malformations and identification of the drainage vein. Recently, Shchurova IN et al. demonstrate in a study that CT or MRI, including scanning in the prone position, as well as minimally invasive CT- and MR-TRICKS-angiography and ophthalmological studies of the patient, determine a comprehensive approach to the diagnosis and selection of adequate treatment for orbital venous varices [7]. In our case, the angio-MRI sequence identified the facial vein as the drainage vein.
On ultrasonography, we classically observe a soft, anechoic, depressible mass, and in color Doppler mode, it is a malformation with a venous-type flow that changes position according to a filling/emptying mode.
Orbital varixes usually evolve towards volume increase, thrombosis and endothelial hyperplasia [1]. Therapeutic modalities are limited in the management of orbital vascular masses and much less so for orbital varixes [5]. The treatment is rather conservative and/or preventive of complications. Preventive low-dose anticoagulation can be discussed in patients without contraindications, to avoid thrombosis. In the absence of complications, careful monitoring should be preferred [1,5]. Invasive treatment consists of surgical removal in symptomatic or complicated patients. This may be due to severe exophthalmos, orbital hemorrhage, optic nerve and/or posterior segment compression, or intolerable pain [8,9].
We opted for strict surveillance in our patient with low-dose anticoagulation to prevent any thrombosis, because there were no ophthalmological complications, notably optic nerve compression or, in this Case, an orbital behavior syndrome related to this varicose vein. This is despite the aesthetic damage which does not seem to bother the patient.
Surgery has the advantage of resecting the entire varicose complex with its drainage vein. Especially in the Case of non-extension of the intra-orbital varicose vein, as in the case of our patient, who has a palpebral extension.
After surgery, recurrences are quite frequent, due to the posterior development of the varixes near the optic nerve, and the significant decrease of the volume of the lesion in decubitus and under general anesthesia. This makes complete removal difficult, and recurrences likely [1,8]. Alternatively, in Case of complications, sclerosis of the varix can be considered, with disappointing results (recurrences, hemorrhages) [9].
3. Conclusion
Orbital varixes are usually revealed by an intermittent exophthalmos, of progressive evolution but which can evolve rapidly. They are of congenital or secondary origin. Imaging under appropriate conditions is essential to establish the diagnosis and eliminate differential diagnoses. In the absence of complications, therapeutic abstention is indicated with rigorous surveillance. Surgery is mainly indicated for symptomatic patients with complications or aesthetic damage. It should be noted that the recurrence rate is not negligible.
Ethical approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
The authors declared that this study has received no financial support.
Author contribution
Issiaka Moctar: Corresponding author writing the paper, Jamaleddine Hamza: writing the paper, El Belhadji Mohamed: Correction of the paper, Iro Salissou: writing the paper, Slimani Faiçal: Correction of the paper.
Registration of research studies
Name of the registry: research registry
Unique Identifying number or registration ID: 6712.
Hyperlink to your specific registration (must be publicly accessible and will be checked).
Guarantor
ISSIAKA MOCTAR.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
Authors of this article have no conflict or competing interests. All of the authors approved the final version of the manuscript.
References
- 1.Cophignona J., d'Hermies F., Civit T. Tumeurs vasculaires de l’orbite. Neurochirurgie. 2010;56:197–212. doi: 10.1016/j.neuchi.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 2.Aydin A., Velioglu M., Ersanli D. Orbital varix presenting with enophthalmos. A Case report. J. Fr. Ophtalmol. 2010;33 doi: 10.1016/j.jfo.2010.03.012. 344.e1-5. [DOI] [PubMed] [Google Scholar]
- 3.Howells M.S., Sharma R. Orbital varices. BMJ Case Rep. 2019;12(12) doi: 10.1136/bcr-2019-232887. Dec 8, PMID: 31818898; PMCID: PMC6904158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical Case REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 5.Naggara O., Koskas P., Lafitte F., Heran F., Piekarski J.D., Meder J.F. Vascular tumours and malformation of the orbit. J. Radiol. 2006;87:17–27. doi: 10.1016/s0221-0363(06)73965-8. [DOI] [PubMed] [Google Scholar]
- 6.Athanasiov P.A., Prabhakaran V.C., Selva D. Non-traumatic enophthalmos: a review. Acta Ophtalmol. 2008;86:356–364. doi: 10.1111/j.1755-3768.2007.01152.x. [DOI] [PubMed] [Google Scholar]
- 7.Shchurova I.N., Pronin I.N., Melnikova-Pitskhelauri T.V., Serova N.K., Batalov A.I., Solozhentseva K.D. Orbital'nyi venoznyi varikoz: sovremennye metody diagnostiki i differentsial'nyi diagnoz [Orbital venous varices: modern diagnostic methods and differential diagnosis] Zh Vopr Neirokhir Im N N Burdenko. 2020;84(6):33–48. doi: 10.17116/neiro20208406133. PMID: 33306298. [DOI] [PubMed] [Google Scholar]
- 8.Guigon-Souquet B., Grubain-Netter S., Macarez R., Giordano P., Bazin S. Varice intra orbitaire non compliquée : un problème thérapeutique difficile. J. Fr. Ophtalmol. 2002;25:840–842. [PubMed] [Google Scholar]
- 9.Fanthou L., Laroche C., Baudouin P. SFP P-006 - varice orbitaire chez un adolescent : à propos d’un cas. Arch. Pediatr. 2014;21(Issue 5) [Google Scholar]