Abstract
BACKGROUND AND PURPOSE: Management of acute symptomatic internal carotid artery (ICA) occlusion remains controversial. We evaluated outcome predictors of a good recovery in patients with acute symptomatic ICA occlusion.
MATERIALS AND METHODS: We retrospectively evaluated 33 consecutive patients (men/women, 23/10; mean age, 66 years) with: 1) acute symptomatic ICA occlusion within 6 hours of symptom onset or with mismatch of symptoms and an early infarct area, 2) National Institutes of Health Stroke Scale (NIHSS) score of 6 or more, and 3) attempted endovascular revascularization of the occluded ICA. Various single and multiple variable analyses were conducted to assess the association of 14 predictors with short-term (1-month NIHSS) and long-term (1-year modified Rankin Scale [mRS]) outcomes.
RESULTS: Successful recanalization (at or more than grade 2 distal residual occlusion) was obtained in 14 (42%) of 33 and good recovery (mRS ≤2) after 1 year in 11 (33%) of 33. Distal residual occlusion (DRO; P = .005), initial NIHSS score (P = .023), and postprocedural thrombolysis in cerebral infarction (P = .027), retrograde ICA filling (P = .036), and ophthalmic collaterals (P = .046) were significant predictors of short-term outcome. DRO (P = .018) and initial NIHSS (P = .033) were significant predictors of long-term outcome on univariable analysis. DRO was the only significant predictor for short-term (P = .026) and long-term outcome (P = .033) on multivariable logistic regression.
CONCLUSIONS: Active revascularization of acute symptomatic ICA occlusion resulted in good recovery in one third of patients after 1 year. DRO is an independent predictor of a favorable clinical outcome.
Compared with studies regarding the effect of middle cerebral artery (MCA) occlusion,1 there have only been a few studies regarding the efficacy of revascularization in patients with symptomatic acute internal carotid artery (ICA) occlusion.2–5 Acute ICA occlusions are more resistant than MCA occlusions to administration of intravenous tissue plasminogen activator (tPA).6–8
ICA occlusion of intravenous thrombolysis trials in patients with acute stroke have been based on the CT exclusion of hemorrhage9 and on CT parenchymal evaluation10,11 but have not pursued the exact cause or the level of occlusion. Optimal management of an ICA occlusion with a concomitant MCA occlusion has not been clearly established, though MCA occlusion can only be a target of revascularization.12–15
The prognosis for patients with acute progressive stroke caused by carotid occlusion is known to be poor, with only 2%–12% good recovery.16 In addition, the management of patients with acute symptomatic carotid artery occlusion remains controversial, though the angiographic finding of ICA occlusion reveals a spectrum of ICA occlusions, as well as a tandem lesion in the intracranial artery in addition to the level (below or above the ophthalmic artery) and type (atherosclerotic or embolic) of lesion.2,17 We evaluated outcome of the acute symptomatic ICA occlusion and estimated how the clinical outcome differs according to the 14 prognostic factors associated with the clinical outcomes.
Materials and Methods
From the acute stroke management data base of 87 patients in our department from January 2001 to December 2003, 33 consecutive patients (male/female, 23/10; mean age, 66 years) who experienced the following: 1) acute symptomatic ICA occlusion within 6 hours of symptom onset or with mismatch of symptoms and early infarct area, 2) initial National Institutes of Health Stroke Scale (NIHSS) ≥6, and 3) attempted intraarterial revascularization, were enrolled in this study. Our Institutional Review Board approved this retrospective study. Written informed consent was obtained from each patient's family.
Analysis of Angiogram
Occlusion sites showing the flow arrest were located above the ophthalmic artery (n = 7), in the cavernous segment below the ophthalmic artery (n = 13), and in the cervical segment (n = 13; Fig 1). Collateral filling of the intradural (antegrade filling) or cavernous (retrograde filling) segment of the ICA through the ophthalmic artery was considered to have collaterals via the ophthalmic artery (Fig 2). The filling of the ophthalmic artery was helpful in defining the extent of the ICA occlusion and for estimating the lumen size and clot burden of the ICA. An ophthalmic artery collateral was observed in 13 patients (39%). Antegrade filling of the intradural ICA occurred with (n = 11) or without (n = 2) retrograde ICA filling. Retrograde filling of the ICA through the ophthalmic artery collateral down to the occlusion site of the ICA on the delayed phase of the angiogram was complete in 4 patients and incomplete in 7. We included the ophthalmic artery collateral and retrograde filling of the ICA as separate variables.
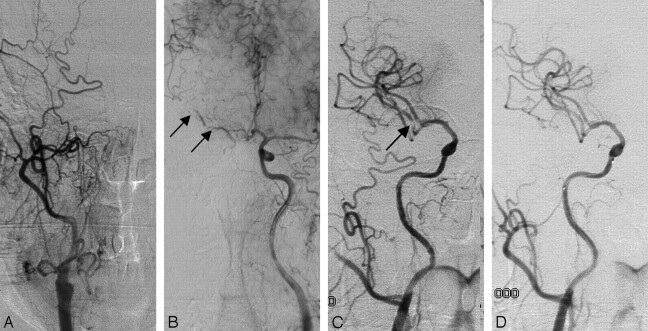
Fig 1.
A 64-year-old man with cardiac arrhythmia presented with dysarthria, facial palsy, and left-sided weakness. The patient had improvement of the NIHSS score from 14 to 2. His mRS was 1 after 1 year.
A, Anteroposterior view of the right common carotid arteriogram shows complete occlusion of the right ICA.
B, The left ICA arteriogram reveals good leptomeningeal collateral circulation through the anterior cerebral artery. Note the filling defects (arrows) in the right M1 because of intracranial emboli.
C, Reopening of the right ICA bulb with stent placement reveals a residual filling defect (arrow) in the right M2 segment.
D, Final angiogram obtained after intra-arterial administration of thrombolytic agents showed no residual emboli in the middle cerebral arterial branches.
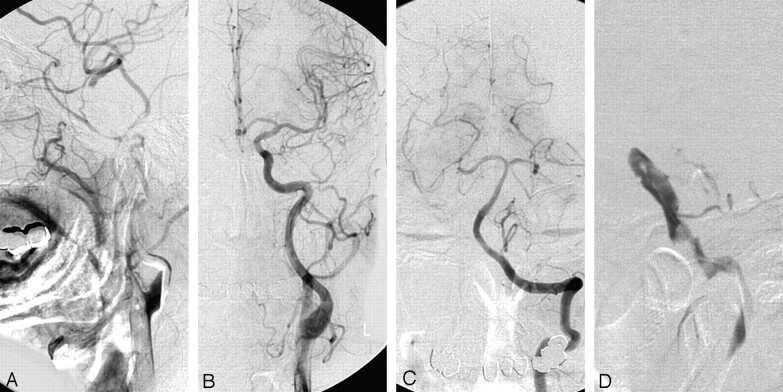
Fig 2.
A 60-year-old man presented with left-sided motor weakness. The patient had improvement of NIHSS score from 9 to 7. His mRS was 4 after 1 year.
A, The right ICA arteriogram shows complete occlusion of the right ICA. Good collateral circulation through the ophthalmic artery reveals no intracranial occlusion.
B, The left ICA arteriogram shows filling of the right anterior cerebral artery through the anterior communicating artery.
C, Vertebral angiogram shows a good leptomeningeal collateral circulation.
D, Microcatheter introduction reveals an occluded end of ICA below the level of the ophthalmic artery. The ICA occlusion could not be revascularized. There was a trigeminal artery variation.
We used the Thrombolysis in Myocardial Infarction (TIMI) and the Thrombolysis in Cerebral Infarction (TICI) grades at the site of occlusion before and after revascularization.18,19 TICI grade consists of perfusion and collateral categories. TICI perfusion categories include grade 0 (no perfusion), grade 1 (penetration with minimal perfusion), grade 2 (partial perfusion), grade 2a (only partial filling; less than two thirds of the entire vascular territory), grade 2b (complete but slow filling of all of the expected vascular territory), and grade 3 (complete filling).19
TICI collateral categories include grade 0 (no collaterals visible to the ischemic site), grade 1 (slow collaterals to the periphery of the ischemic site with persistence of some of the defect), grade 2 (rapid collaterals to the periphery of the ischemic site with persistence of some of the defect and to only a portion of the ischemic territory), grade 3 (collaterals with slow but compete angiographic blood flow of the ischemic bed by the late venous phase), and grade 4 (complete and rapid collateral blood flow to the vascular bed in the entire ischemic territory by retrograde perfusion).19
We also evaluated DRO at the distal carotid or intracranial branches beyond the occlusion level after revascularization. The DRO grade was defined on the final angiogram to simply categorize the residual occlusion level. We rated DRO as grade 0 when there was no change in the occlusion level, grade 1 when there was a distal occlusion in the ICA despite the partial opening in the occlusion site, grade 2 when there was an occlusion at the M1, and grade 3 when there was an occlusion at M2 or beyond.
Subtype classification of large-artery atherosclerosis or cardioembolism for ischemic stroke was based on the modified Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification.20,21 Sixteen patients revealed large-artery atherosclerosis in which we were able to identify the occlusion site when the occluded vessel was opened and could differentiate whether the occlusion was due to emboli or de novo atherosclerotic plaque associated with thrombi. Seventeen other patients with high or medium risks were classified as having possible cardioembolism in which we could determine the cause of the lesion in conjunction with the angiographic finding of filling defect in the lumen. Angiographic findings suggesting dissection, such as a filling defect of the intimal flap, were not identified in our study patients.22
Patient Evaluation and Statistical Analysis
The patients’ pretherapeutic and 1-month posttherapeutic neurologic status was evaluated by neurologists by using the NIHSS. Modified Rankin Scale (mRS) was used to assess the final clinical outcome after 1 year. The effects of 14 variables (ie, age, sex, occlusion level, retrograde ICA filling, tandem intracranial occlusion, type of occlusion, TICI collaterals [rapidity and persistence of the defect at the ischemic site], ophthalmic collaterals, initial NIHSS, DRO, postprocedural TIMI at the occlusion site, postprocedural TICI, time from symptom onset to needle time, and initial infarction volume) were evaluated for both short-term outcome (NIHSS at 1 month) and long-term outcome (mRS at 1 year).
All of the variables were dichotomized before statistical analysis: age (≥65 versus <65 years); sex (male versus female); occlusion level (above ophthalmic artery versus below ophthalmic artery); retrograde ICA filling (no versus yes); tandem intracranial stenosis (yes versus no); type of occlusion (embolic versus de novo); TICI collaterals (grade 0 or 1 versus grade 2 or 3); ophthalmic collaterals (no versus yes); initial NIHSS (>12 versus ≤12); DRO (grade 0 or 1 versus grade 2 or 3); postprocedural TIMI (grade 0 or 1 versus grade 2 or 3); postprocedural TICI (grade 0 or 1 versus grade 2 or 3); time from onset to procedure (≥4 versus <4 hour); and infarction volume (≥30 mL versus <30 mL). Then, univariable logistic regression analysis was first conducted to determine the candidates for multivariable analysis. Variables of P < .10 on univariate analysis were entered into multivariable logistic regression analysis. Multivariable logistic regression models were adjusted for age and sex. A P < .05 was considered significant. Calculations were performed with SPSS for Windows (version 10.0; SPSS, Chicago, Ill).
Imaging Study and Revascularization Procedure
Image evaluation included MR diffusion-weighted imaging in 28 patients and CT in 5 patients. Time-of-flight MR angiography was obtained in 26 patients and MR perfusion-weighted imaging in 7 patients. A decision regarding revascularization was made when there was a mismatch between the diffusion-weighted MR imaging and the patient symptoms after discussion regarding each patient with a neurologist and a neuroradiologist. Precontrast CT (n = 5) and MR perfusion-weighted imaging (n = 7) were used to make this decision. tPA was intravenously infused within 3 hours of the onset of their symptoms into 4 patients in the amount of 0.6 mg/kg and in the other 4 in the amount of 0.9 mg/kg according to the level of occlusion or the time interval of the intraarterial revascularization procedure.
Revascularization included various attempts to reopen the occluded artery by intra-arterial fibrinolytic agent infusion (IAFI) only (n = 16), IAFI plus stent placement (n = 9; Fig 1) and/or intra-arterial thrombectomy, IAFI plus angioplasty (n = 3), and stent placement only (n = 2). In 3 patients, revascularization was abandoned because of the presence of tortuous vessels, absence of response to the thrombolytic agent, or a large amount of thromboemboli (Fig 2). Two patients treated by intra-arterial thrombectomy were included in a previous report.23
Digital subtraction angiography of the ipsilateral and contralateral common carotid arteries and of the vertebral artery was performed to demonstrate ICA and MCA, as well as to assess potential collateral routes. After occlusion was demonstrated, attempts were made to cross the lesion with a 0.014-inch microwire and/or a microcatheter after infusion of a fibrinolytic agent through a microcatheter just in front of the occluded end of the ICA stump. Once the occluded ICA was opened, angioplasty and/or stent placement were performed in case there was significant luminal narrowing at the site of occlusion. Angioplasty was done in 3 patients in whom the stent placement was abandoned because of the tortuousness of their vessels.
Stent placement was preceded by predilation by using a 1.5–4-mm-diameter balloon according to the level of occlusion. A balloon-expandable stent was inserted for occlusion of the ICA into the cavernous segment. For the carotid bulb lesion, a self-expandable stent was deployed and inserted into the stenotic vessel from the internal carotid to the common carotid artery. Postdilation was done by using a 4–6-mm-diameter balloon. During the procedure, 3000 IU of heparin was introduced intravenously. In most patients, antiplatelet agents of 200 mg of aspirin and 300 mg of clopidogrel were introduced orally in cases of angioplasty and/or stent placement.24 A postprocedural CT scan was obtained after the procedure to visualize any evidence of hemorrhage.
Results
Analysis of outcomes was summarized in Table 1. The initial NIHSS was a median of 15 (range: 6–27). Univariate analysis showed that retrograde ICA filling (P = .036), ophthalmic collaterals (P = .046), initial NIHSS (P = .023), DRO (P = .005), and postprocedural TICI (P = .027) were significant prognostic variables (predictor) for the short-term outcome (Table 2). The time from the onset to the procedure was only marginally significant (P = .069).
Table 1:
Outcome of the 33 patients according to degree of DRO
| DRO Grade | 0 | 1 | 2 | 3 | Total |
|---|---|---|---|---|---|
| No. of patients | 13 | 6 | 4 | 10 | 33 |
| No. of recanalized ICA (rate) | 19 (58%) | 14 (42%) | 33 | ||
| Initial NIHSS, median (range) | 15 (6–22) | 17 (12–27) | 11.5 (8–18) | 10.5 (6–21) | |
| 1-month NIHSS, median (range) | 14 (2–42*) | 29 (6–42) | 7 (1–14) | 5 (2–17) | |
| No. of deaths | 3 | 3 | 0 | 0 | 6 (18%) |
| mRS >3 at 1 year (mean mRS %) | 10 (77) | 6 (100) | 2 (50) | 4 (40) | 22 (67) |
| mRS ≤2 at 1 year (mean mRS %) | 3 (23) | 0 (0) | 2 (50) | 6 (60) | 11 (33) |
Note:—DRO indicates distal residual occlusion; ICA, internal carotid artery; NIHSS, National Institutes of Health Stroke Scale; mRS, modified Rankin Scale. DRO grades are defined in the text.
NIHSS score of 42 means death.
Table 2:
Univariate association of prognostic variables at 1 month
| Variables (Based on NIHSS) | Odds Ratio (95% CI) | P |
|---|---|---|
| Age (≥ 65 vs <65) | 2.75 (0.63–11.97) | .178 |
| Sex (male vs female) | 1.38 (0.31–6.20) | .679 |
| Occlusion level (above vs below the OA) | 4.00 (0.65–24.69) | .136 |
| Retrograde ICA filling (no vs yes) | 6.50 (1.13–37.48) | .036 |
| Tandem intracranial occlusion (yes vs no) | 3.06 (0.68–13.79) | .145 |
| Type of occlusion (embolic vs de novo) | 1.88 (0.47–7.53) | .375 |
| TICI collaterals (grade 0, 1 vs grade 2, 3) | 0.69 (0.16–2.87) | .606 |
| Ophthalmic collaterals (no vs yes) | 5.00 (1.04–24.03) | .046 |
| Initial NIHSS score (>12 vs ≤ 12) | 6.29 (1.29–30.54) | .023 |
| Distal residual occlusion (grade 0, 1 vs grade 2, 3) | 13.00 (2.19–77.27) | .005 |
| Postprocedural TIMI (grade 0, 1 vs grade 2, 3) | 3.00 (0.72–12.46) | .131 |
| Postprocedural TICI (grade 0, 1 vs grade 2, 3) | 5.50 (1.22–24.81) | .027 |
| Time from onset to procedure (≥ 4 vs <4 h) | 0.24 (0.05–1.12) | .069 |
| Infarction volume (≥ 30 mL vs <30 mL) | 2.36 (0.58–9.58) | .231 |
Note:—NIHSS indicates National Institutes of Health Stroke Scale; CI, confidence interval; OA, ophthalmic artery; ICA, internal carotid artery; TICI, Thrombolysis in Cerebral Infarction; TIMI, Thrombolysis in Myocardial Infarction.
For the long-term outcome, univariate analysis showed that DRO (P = .018) and the initial NIHSS (P = .033) were significant independent variables (Table 3). Retrograde ICA filling (P = .075), ophthalmic collaterals (P = .051), and postprocedural TICI (P = .057) were variables of borderline significance.
Table 3:
Univariate association of prognostic variables at 1 year
| Variables (based on mRS) | Odds Ratio (95% CI) | P |
|---|---|---|
| Age (≥65 vs <65) | 1.46 (0.34–6.35) | .615 |
| Sex (male vs female) | 1.52 (0.33–7.15) | .593 |
| Occlusion level (above vs below OA) | 3.75 (0.39–35.92) | .252 |
| Retrograde ICA filling (no vs yes) | 4.08 (0.87–19.23) | .075 |
| Tandem intracranial stenosis (yes vs no) | 3.12 (0.54–17.97) | .204 |
| Type of occlusion (embolic vs de novo) | 2.53 (0.57–11.26) | .224 |
| TICI collaterals (grade 0, 1 vs grade 2, 3) | 1.20 (0.27–5.25) | .809 |
| Ophthalmic collaterals (yes vs no) | 4.67 (1.00–21.895) | .051 |
| Initial NIHSS score (>12 vs ≤ 12) | 5.71 (1.15–28.35) | .033 |
| Distal residual occlusion (grade 0, 1 vs grade 2, 3) | 7.11 (1.40–36.12) | .018 |
| Postprocedural TIMI (grade 0, 1 vs grade 2, 3) | 2.67 (0.56–12.79) | .220 |
| Postprocedural TICI (grade 0, 1 vs grade 2, 3) | 4.67 (0.96–22.79) | .057 |
| Time from onset to procedure (≥ 4 vs <4 h) | 0.60 (0.12–2.89) | .525 |
| Infarction volume (≥ 30 mL vs <30 mL) | 2.10 (0.47–9.30) | .328 |
Note:—mRS indicates modified Rankin Scale; CI, confidence interval; OA, ophthalmic artery; ICA, internal carotid artery; NIHSS, National Institutes of Health Stroke Scale; TIMI, Thrombolysis in Myocardial Infarction; TICI, Thrombolysis in Cerebral Infarction.
Multivariate logistic regression analysis conducted with independent variables of a P < .10 and adjusted for age and sex revealed that DRO was a significant variable for both the short-term outcome (P = .026) and the long-term outcome (P = .033; Tables 4 and 5). DRO and postprocedural TICI were highly correlated with each other and were therefore entered separately into the multivariable analysis. DRO was significantly related to a better short-term outcome with an odds ratio of 48.4 (95% confidence interval: 1.60–1468.34) and was also related to a better long-term outcome with an odds ratio of 11.5 (95% confidence interval: 1.22–109.30).
Table 4:
Results of multivariable analysis for short-term (1 month) outcome
| Variables (based on NIHSS) | Odds Ratio (95% CI) | P |
|---|---|---|
| Age (≥ 65 vs <65) | 2.21 (0.21–24.38) | .517 |
| Sex (male vs female) | 2.52 (0.30–21.31) | .396 |
| Time from onset to procedure (≥ 4 vs <4 h) | 0.07 (0.00–1.79) | .108 |
| Retrograde ICA filling (no vs yes) | 0.34 (0.02–6.15) | .468 |
| Distal residual occlusion (grade 0, 1 vs grade 2, 3) | 48.45 (1.60–1468.34) | .026 |
| Initial NIHSS score (>12 vs ≤ 12) | 11.13 (0.69–179.42) | .089 |
Note:—NIHSS indicates National Institutes of Health Stroke Scale; CI, confidence interval; ICA, internal carotid artery.
Table 5:
Results of multivariate analysis for long-term (1 year) outcome
| Variables (based on mRS) | Odds Ratio (95% CI) | P |
|---|---|---|
| Age (≥ 65 vs <65) | 0.84 (0.09–7.46) | .874 |
| Sex (male vs female) | 4.91 (0.52–46.58) | .166 |
| Time from onset to procedure (≥ 4 vs <4 h) | 0.66 (0.08–5.20) | .693 |
| Retrograde ICA filling (no vs yes) | 0.50 (0.04–5.65) | .573 |
| Distal residual occlusion (grade 0, 1 vs grade 2, 3) | 11.54 (1.22–109.30) | .033 |
| Initial NIHSS score (>12 vs ≤ 12) | 4.85 (0.38–61.29) | .222 |
Note:—mRS indicates modified Rankin Scale; CI, confidence interval; ICA, internal carotid artery; NIHSS, National Institutes of Health Stroke Scale.
Hemorrhage was detected in 9 patients (27%) within 1 month after procedure. Two patients revealed a focal hemorrhage on the immediate postprocedural CT scan. Seven patients with delayed hemorrhage (1–8 days; median: 3 days) revealed a focal hemorrhage in 6 patients and a massive hemorrhage leading to the death in 1.
Six deaths (15%) in the 33 study patients occurred in the early time period after the procedure (1–6 days). The causes of death were related to massive infarction (n = 5) or hemorrhage (n = 1).
Discussion
Recanalization rate of the occluded ICA (DRO ≥2) in our study was 48%, which is comparable with the 46% in the Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial.25 Good outcome (an mRS score of ≤2 at 1 year) in our study was 33% compared with the 28% of patients who reached an mRS score of ≤2 at 90 days in the MERCI trial.25
Based on the evaluation of predictors of good outcome, our results indicate that better short- and long-term outcomes were related to the degree of DRO after revascularization in acute symptomatic ICA occlusion. It is noteworthy that improvement of the flow itself at the occlusion site was not directly related to a favorable patient outcome, because local improvement of flow, especially at the ICA level, was not directly related to the improvement of cerebral perfusion.15 Therefore, we also suggest that adequate distal filling of cerebral arteries is a simple and critical predictor (surrogate marker) of favorable outcome in acute symptomatic ICA occlusion.26
Retrograde ICA filling, ophthalmic collateral, initial NIHSS, and postprocedural TICI were related to better short-term outcomes on univariate analysis as shown in Table 1. Among them, initial NIHSS was the only significant variable for long-term outcome, as shown in Table 2. We believe that this result also seems to be a good supportive piece of data for the therapeutic decision-making process conducted on an emergency basis, because patients who presented with an acute progressive stroke within 6 hours of symptom onset were less likely to show early clinical improvement than patients who presented subacutely with neurologic fluctuations because of the ICA occlusion.3
Although our study is retrospective, and the patient number is limited, to the best of our knowledge, there has been no study of prognostic factor analysis as detailed and complete as our study. Further evaluation using a randomized, controlled prospective study might prove these results more accurately, though thrombolysis or mechanical revascularization is only possible in a hospital with high-quality medical equipment and an experienced stroke patient management team.3,27
Conclusions
Our study suggests that active revascularization of acute ICA occlusion appears to be feasible and effective, leading to good recovery in one third of the patients, and was associated with early neurologic improvement depending on the degree of revascularization. Therefore, active revascularization can be considered in selected patients with acute ICA occlusion and deteriorating neurologic symptoms.
Footnotes
This study was supported by a grant (2005-143) from the Asan Institute for Life Sciences, Seoul, Korea.
References
- 1.Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA 1999;282:2003–11 [DOI] [PubMed] [Google Scholar]
- 2.Imai K, Mori T, Izumoto H, et al. Emergency carotid artery stent placement in patients with acute ischemic stroke. AJNR Am J Neuroradiol 2005;26:1249–58 [PMC free article] [PubMed] [Google Scholar]
- 3.Jovin TG, Gupta R, Uchino K, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke 2005;36:2426–30 [DOI] [PubMed] [Google Scholar]
- 4.Sugg RM, Malkoff MD, Noser EA, et al. Endovascular recanalization of internal carotid artery occlusion in acute ischemic stroke. AJNR Am J Neuroradiol 2005;26:2591–94 [PMC free article] [PubMed] [Google Scholar]
- 5.Fox AJ, Eliasziw M, Rothwell PM, et al. Identification, prognosis, and management of patients with carotid artery near occlusion. AJNR Am J Neuroradiol 2005;26:2086–94 [PMC free article] [PubMed] [Google Scholar]
- 6.Jansen O, von Kummer R, Forsting M, et al. Thrombolytic therapy in acute occlusion of the intracranial internal carotid artery bifurcation. AJNR Am J Neuroradiol 1995;16:1977–86 [PMC free article] [PubMed] [Google Scholar]
- 7.Linfante I, Llinas RH, Selim M, et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke 2002;33:2066–71 [DOI] [PubMed] [Google Scholar]
- 8.Mori E, Yoneda Y, Tabuchi M, et al. Intravenous recombinant tissue plasminogen activator in acute carotid artery territory stroke. Neurology 1992;42:976–82 [DOI] [PubMed] [Google Scholar]
- 9.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–87 [DOI] [PubMed] [Google Scholar]
- 10.Hacke W, Kaste M, Fieschi C, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA 1995;274:1017–25 [PubMed] [Google Scholar]
- 11.Hacke W, Kaste M, Fieschi C, et al. Randomised double-blind placebo-controlled trial of thrombolytic therapy with intravenous alteplase in acute ischaemic stroke (ECASS II). Second European-Australasian Acute Stroke Study Investigators. Lancet 1998;352:1245–51 [DOI] [PubMed] [Google Scholar]
- 12.Adams HP Jr, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke Association. Stroke 2003;34:1056–83 [DOI] [PubMed] [Google Scholar]
- 13.Adams HP Jr, Bendixen BH, Leira E, et al. Antithrombotic treatment of ischemic stroke among patients with occlusion or severe stenosis of the internal carotid artery: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 1999;53:122–25 [DOI] [PubMed] [Google Scholar]
- 14.Kole MK, Pelz DM, Lee DH, et al. Intra-arterial thrombolysis of embolic middle cerebral artery using collateral pathways. Can J Neurol Sci 2005;32:257–60 [DOI] [PubMed] [Google Scholar]
- 15.Qureshi AI. Endovascular revascularization of symptomatic acute extracranial internal carotid artery occlusion. Stroke 2005;36:2335–36 [DOI] [PubMed] [Google Scholar]
- 16.Meyer FB, Sundt TM Jr, Piepgras DG, et al. Emergency carotid endarterectomy for patients with acute carotid occlusion and profound neurological deficits. Ann Surg 1986;203:82–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ringelstein EB, Berg-Dammer E, Zeumer H. The so-called atheromatous pseudoocclusion of the internal carotid artery. A diagnostic and therapeutical challenge. Neuroradiology 1983;25:147–55 [DOI] [PubMed] [Google Scholar]
- 18.The Thrombolysis in Myocardial Infarction (TIMI) trial. Phase I findings. TIMI Study Group. N Engl J Med 1985;312:932–36 [DOI] [PubMed] [Google Scholar]
- 19.Higashida RT, Furlan AJ, Roberts H, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 2003;34:e109–37 [DOI] [PubMed] [Google Scholar]
- 20.Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993;24:35–41 [DOI] [PubMed] [Google Scholar]
- 21.Gordon DL, Bendixen BH, Adams HP Jr, et al. Interphysician agreement in the diagnosis of subtypes of acute ischemic stroke: implications for clinical trials. The TOAST Investigators. Neurology 1993;43:1021–27 [DOI] [PubMed] [Google Scholar]
- 22.Jeon SB, Suh DC, Lee DH, et al. Emergent stenting in carotid artery dissection: MRI-guided therapeutic decision-making. Cerebrovasc Dis 2005;19:347–50 [DOI] [PubMed] [Google Scholar]
- 23.Xu GF, Suh DC, Choi CG, et al. Aspiration thrombectomy of acute complete carotid bulb occlusion. J Vasc Interv Radiol 2005;16:539–42 [DOI] [PubMed] [Google Scholar]
- 24.Davies ER, Sutton D. Pseudo-occlusion of the internal carotid artery in raised intracranial pressure. Clin Radiol 1967;18:245–52 [DOI] [PubMed] [Google Scholar]
- 25.Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 2005;36:1432–38 [DOI] [PubMed] [Google Scholar]
- 26.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 2007;38:967–73 [DOI] [PubMed] [Google Scholar]
- 27.Klijn CJ, Hankey GJ. Management of acute ischaemic stroke: new guidelines from the American Stroke Association and European Stroke Initiative. Lancet Neurol 2003;2:698–701 [DOI] [PubMed] [Google Scholar]