Abstract
BACKGROUND AND PURPOSE: Accurate detection and classification of purely intracortical lesions in multiple sclerosis (MS) are important in understanding their role in disease progression and impact on the clinical manifestations of the disease. However, detection of these lesions with conventional MR imaging remains a challenge. Although double inversion recovery (DIR) has been shown to improve the sensitivity of the detection of cortical lesions, this sequence has low signal-to-noise ratio (SNR), poor delineation of lesion borders, and is prone to image artifacts. We demonstrate that intracortical lesions can be identified and classified with greater confidence by the combination of DIR with phase-sensitive inversion recovery (PSIR) images.
MATERIALS AND METHODS: A total of 16 subjects with MS were included in this study. DIR, PSIR, and fluid-attenuated inversion recovery (FLAIR) images were acquired and inspected by 3 experts, with identification of lesions by consensus. PSIR and DIR images were jointly used to classify lesions as purely intracortical, mixed gray-white matter, and juxtacortical. The difference in the number of lesions detected in each category was compared between combined PSIR and DIR and conventional FLAIR.
RESULTS: PSIR consistently allowed a clearer classification and delineation of lesions. Combined PSIR and DIR images showed a 337% improvement in the total number of lesions detected compared with FLAIR alone. Detection of intracortical lesions was improved by 417% compared with FLAIR. Detection of mixed gray-white matter and juxtacortical lesions was improved by 396% and 130%, respectively, compared with FLAIR.
CONCLUSION: Reliable detection and classification of intracortical lesions in MS are greatly improved by combined use of PSIR and DIR.
Our understanding of the archetypical white matter (WM) demyelinating lesions in multiple sclerosis (MS) has greatly improved since the introduction of MR imaging. Despite certain limitations, MR imaging is widely used to monitor disease activity in clinical trials and has become a key element of clinical diagnosis. Gray matter lesions, though acknowledged as part of the disease, are not detected routinely on conventional MR imaging. This is partly because of poor contrast between cortical lesions and the surrounding gray matter. This shortcoming limits attempts to correlate their presence with disabling clinical manifestations of MS, such as cognitive impairment, seizures, affective disorders, and speed of information processing. These difficulties also hinder understanding the impact of cortical pathologic changes on clinical progression of the disease.
Although pathologic studies dating back to 1916 identified cortical involvement in MS,1 the nature, pathogenesis, prevalence, distribution, and clinical significance of cortical lesions remain poorly understood. Two classic studies observed that some patients have a plethora of cortical lesions, whereas others have none or very few.2,3 More recently, the application of sensitive immunohistochemical techniques that identify myelin basic protein (MBP) have been used to confirm a high prevalence of purely intracortical lesions, which account for most of the total cortical demyelination. These studies also suggest that the cortical involvement may be diffuse or highly localized.4 Other studies show that intracortical lesions exhibit relatively minimal inflammatory reaction.5–7 These studies imply differences in the pathophysiologic processes of gray and white matter lesions that need to be clarified to gain a better understanding of this disease.
Many attempts have been made to increase the MR imaging conspicuity of cortical lesions. There is evidence that fluid-attenuated inversion recovery (FLAIR) sequence improves detection of lesions within the cortex, and that enhancement with gadolinium may accentuate their visibility.7–9 Unfortunately, these sequences do not clearly differentiate between purely intracortical and mixed gray-white matter lesions. In a recent study,10 even when high-resolution MR imaging of postmortem specimens were examined, considerably fewer cortical lesions were identified than when the tissues were examined histologically.
MR spectroscopy has provided some information regarding abnormalities in metabolite concentrations in normal-appearing gray matter (NAGM),11–13 which can be seen even in early relapsing-remitting MS (RRMS).14 However, there is some controversy on the findings of metabolite abnormalities in cortical gray matter by MR spectroscopy.15 Some data support the use of magnetization transfer ratio (MTR) and diffusion tensor imaging (DTI) to show damage in NAGM. Unfortunately, although information obtained from these techniques can show diffuse abnormalities in white and gray matter, it cannot provide details on isolated changes in cortical gray matter.16–18
In 1998, fast double inversion recovery imaging (DIR) was introduced and applied to MS.19 This technique simultaneously suppresses white matter and CSF signals, thus significantly increasing lesion conspicuity in both gray and white matter compared with FLAIR or T2-weighted spin-echo (SE).19 In a recent study, Geurts et al20 performed 3D DIR on 10 patients with RRMS that demonstrated a gain of 538% and 152% in the detection of intracortical lesions compared with T2-weighted SE and FLAIR, respectively. They concluded that DIR images enabled visualization of intracortical lesions and better definition of the mixed gray-white matter lesions. Despite these advantages, this sequence is prone to image artifacts such as flow, which may affect the visualization of subtle intracortical lesions. In addition, DIR sequences have poor delineation of lesion borders and intrinsically suffer from low signal-to-noise ratio (SNR), which further obscures details of small structures.
Some of the limitations of DIR can be overcome with a T1-weighted inversion recovery sequence and a phase-sensitive reconstruction algorithm.21 Whereas traditional magnitude reconstruction discards the sign of the magnetization, the phase-sensitive reconstruction algorithm preserves that information, effectively doubling the dynamic range.21 The phase-sensitive inversion recovery (PSIR) sequence has been shown to provide superior gray-white matter contrast.21 This technique has been widely used in the detection of myocardial infarction22 and imaging of pulmonary blood flow23 but is just now being applied to MS.21
In this study, we demonstrate that interpretation with combined PSIR and DIR images improves confidence in the detection and classification of intracortical lesions by allowing clearer delineation of lesion and tissue boundaries.
Materials and Methods
Subjects
Subjects were drawn from a population of patients with MS diagnosed by McDonald criteria,24 undergoing routine imaging at our MR imaging research center. The cohort included 4 men and 12 women. There was 1 patient with primary- progressive MS (PPMS), 3 with secondary-progressive MS (SPMS), and 12 with relapsing-remitting MS (RRMS). Their median age was 47 years (range, 24–68 years), median Expanded Disability Status Scale (EDSS) at time of scanning was 2.0 (range, 0–6.5), and median duration of disease from the onset of symptoms was 11 years (range, 1.2–45 years). The Institutional Review Board approved this study, and we obtained informed consent from all subjects before imaging. Demographic data on the patients is summarized in Table 1.
Table 1:
Demographics of patients in the study
| Age/Sex | Disease Type | Disease Duration (years) | EDSS Score |
|---|---|---|---|
| 44/M | RR | 6 | 2 |
| 50/M | SP | 10 | 3 |
| 59/F | RR | 11 | 2 |
| 50/F | RR | 1.5 | 0 |
| 55/F | RR | 26 | 2 |
| 53/F | RR | 12 | 3 |
| 49/F | RR | 25 | 5 |
| 25/F | RR | 5 | 1 |
| 64/F | SP | 29 | 6.5 |
| 62/F | SP | 45 | 6.5 |
| 24/F | RR | 5 | 3 |
| 27/F | RR | 1.5 | 0 |
| 48/F | RR | 22 | 1 |
| 35/F | RR | 1.2 | 2 |
| 68/M | PP | 24 | 4 |
| 39/F | RR | 11 | 2 |
Note:—RR indicates relapsing-remitting; SP, secondary-progressive; PP, primary-progressive; EDSS, Expanded Disability Status Scale.
Acquisition of Images
Patients were scanned from September 2004 to January 2006. All studies were performed on a 3T Intera system (Philips Medical Systems, Best, the Netherlands) with a Quasar gradient system and a standard sensitivity encoding-compatible head coil. PSIR and DIR images were obtained during every session for each subject as part of our routine MS protocol, which also included conventional dual-echo fast spin-echo (FSE) and FLAIR. We acquired all images using a 256 × 256 matrix over a 24-cm FOV, with full-brain coverage of 44 axial sections of 3-mm thickness. Relevant sequence parameters are listed in Table 2.
Table 2:
Acquisition parameters for MR imaging sequences in the MS protocol
| Sequence | Plane | TR (ms) | TE (ms) | TI (ms) | Image Matrix | FOV (mm) | Section (mm) | Scan Time (min) |
|---|---|---|---|---|---|---|---|---|
| PSIR | Axial | 4300 | 13 | 400 | 256 × 256 | 240 | 3 | 4.0 |
| DIR | Axial | 15,000 | 25 | 3400/325 | 512 × 512 | 240 | 3 | 6.5 |
| Dual-FSE | Axial | 6800 | 10/90 | – | 256 × 256 | 240 | 3 | 6.0 |
| FLAIR | Axial | 10,000 | 80 | 2600 | 256 × 256 | 240 | 3 | 3.0 |
Note:—MS indicates multiple sclerosis; PSIR, phase-sensitive inversion recovery; DIR, double inversion recovery; FSE, fast spin-echo; FLAIR, fluid-attenuated inversion recovery; FOV, field of view.
Considerable care was taken to optimize the DIR sequence. We initially acquired data with 1.5-mm section thickness to reduce partial volume averaging effects. However, the increased noise outweighed any advantages in small lesion conspicuity (as noted above, DIR sequences are SNR limited to begin with). Therefore, we settled for 3-mm section thicknesses as optimal and matched to the other sequences in the protocol. In addition, flow artifacts from vessels in the skull displayed hyperintense regions, which resulted in false-positive detection of lesions, even on healthy subjects. These artifacts persisted to some extent even with flow compensation. The phase-encode (PE) direction was originally set to the patients’ L/R axis, so the artifacts manifested largely within the skull. To address this issue, we swapped the PE direction to the patients’ A/P axis, which redistributed most of these artifacts outside the skull.
Interpretation of Images
Images were reviewed by a team of investigators that included 1 medical physicist with extensive experience in MR imaging, and 2 neurologists with clinical and imaging experience in MS. Identification of the cortical lesions was by consensus, and consisted of 2 phases for each individual lesion: detection and classification. The criterion for detection was visibility on both DIR and PSIR images, viewed side by side. Lesions were first visually detected on the DIR image on the basis of a signal hyperintensity on the cortical ribbon. Then the lesion was visually correlated with a corresponding hypointensity on the PSIR image at the same section location. Once it was agreed that the lesion in question was real, we proceeded to the classification phase. The FLAIR images were also inspected for comparative purposes. Using a conservative approach, we categorized the lesions as either 1) purely intracortical, 2) mixed gray-white matter, or 3) juxtacortical. We classified the lesions as purely intracortical if no there was no obvious evidence of white matter involvement. The border of the lesion was clearly confined to within the cortical ribbon, with no disruption of the contiguous gray-white matter boundary. Intracortical lesions with questionable white matter involvement from poor definition of lesion borders were classified as mixed. Lesions were considered to be mixed if the lesion volume was roughly 75% intracortical, with clear evidence of extension into the white matter. However, it should be emphasized that most of the lesion volume remained within the cortical ribbon. Finally, lesions were classified as juxtacortical if the volume was approximately 75% subcortical, with clear evidence of extension into the cortical gray matter. Purely subcortical lesions with no gray matter involvement were not the focus of this study.
Statistical Analysis
We used the Wilcoxon matched-pairs signed-rank test to compare the number of lesions of each type detected by using either of the 2 methods (combined PSIR and DIR vs FLAIR). The analysis was implemented in SAS version 9.1 (SAS, Cary, NC) and a SYSTAT 11 statistics package (SYSTAT Software, Richmond, Calif). We calculated the correlation between the number of (purely) intracortical lesions and duration of disease or EDSS with the Spearman correlation coefficient. All statistical analyses had a two-tailed alpha level of less than 0.05 as defining significance.
Results
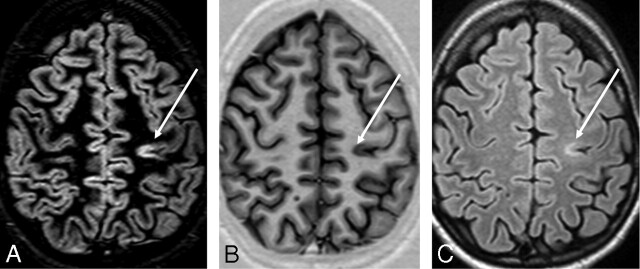
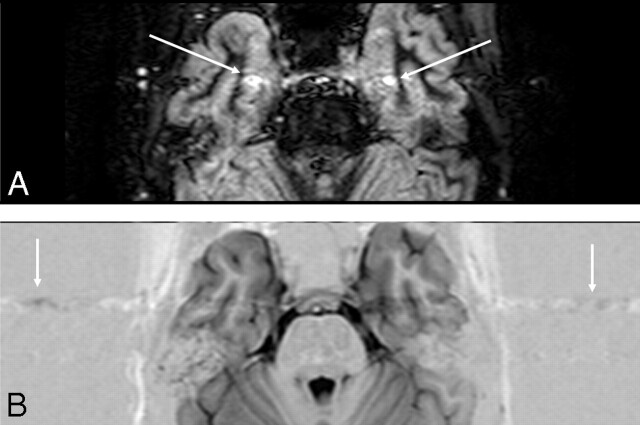
Cortical lesions were consistently hyperintense on the DIR images, but the cortical gray-white matter junction was not well defined enough to distinguish between the purely intracortical lesions and those extending into the subcortical WM (Fig 1). The lesions were hypointense on PSIR, with the clear contrast between the lesions and surrounding gray matter providing a distinct delineation of shape, size, and boundary (Fig 1). Most importantly, the superior delineation of the gray-white matter border on PSIR allowed a more confident classification of lesions into purely intracortical, mixed, or juxtacortical (Fig 2).
Fig 1.
DIR (A), PSIR (B), and FLAIR (C) images from a single patient with MS at the same section location. An intracortical lesion is evident in the left parietal area. Also note the excellent overall delineation of the gray-white matter border on PSIR.
Fig 2.
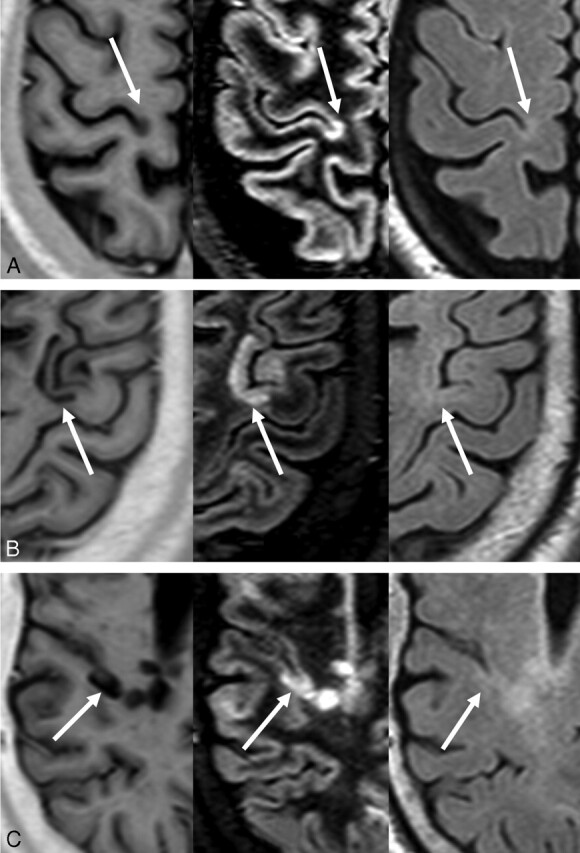
Examples of cortical lesions on PSIR (left), DIR (center), and FLAIR (right). Lesions shown are (A) purely intracortical, (B) mixed, and (C) juxtacortical.
The mean number of intracortical, mixed gray-white, and juxtacortical lesions detected by combined use of PSIR and DIR (PSIR+DIR) versus FLAIR are summarized in Table 3. PSIR and DIR showed a 337% improvement in the total number of lesions detected compared with FLAIR alone. The number of intracortical lesions detected was improved by 417% compared with FLAIR. Detection of mixed gray-white matter and juxtacortical lesions improved by 396% and 130%, respectively, compared with detection on FLAIR.
Table 3:
Mean number of lesions detected by technique
| Type of Lesion | PSIR+DIR | FLAIR | % Improvement | P Value |
|---|---|---|---|---|
| Intracortical | 7.8 ± 9.4 | 1.4 ± 1.8 | 439 | .0002 |
| Mixed | 9 ± 11 | 1.8 ± 2.4 | 414 | <.0001 |
| Juxtacortical | 2.5 ± 2.4 | 1.1 ± 1.5 | 117 | .0078 |
| Overall | 19.2 ± 21.1 | 4.3 ± 4.3 | 345 | <.0001 |
Note:—PSIR indicates phase-sensitive inversion recovery; DIR, double inversion recovery; FLAIR, fluid-attenuated inversion recovery.
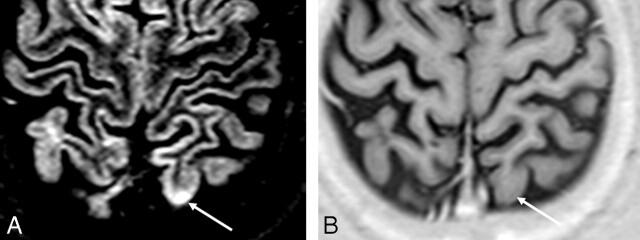
Relatively small differences were observed in the number of lesions detected on PSIR and DIR images. A total of 15 small, hyperintense areas suspicious for lesions on DIR were not seen on PSIR. Of these, 10 were judged to be the result of flow-related artifacts (Fig 3), and the rest were thought to be related to radiofrequency inhomogeneity (Fig 4). Only 2 questionable lesions were seen on PSIR and not on DIR.
Fig 3.
Example of flow artifact. On the DIR image (A), apparent cortical lesions (arrows) are visible. However, on the PSIR image (B), there are no corresponding hypointense signals. On PSIR, a flow artifact is seen more clearly (arrows), which is the likely source of the false-positive.
Fig 4.
Example of RF inhomogeneity artifact. On the DIR image (A), an apparent cortical lesion is visible (white arrow). On the PSIR image (B), there is again no corresponding hypointensity. On DIR, the signal intensity is 38% higher for the apparent lesion than the contralateral area, compared with 14% for PSIR. The relative insensitivity of PSIR to the RF artifact allows rejection of the lesion on DIR as a false-positive.
The P values for the number of lesions detected on each type of sequence are also listed in Table 3. No significant correlations were observed between duration of disease or EDSS and the number of purely intracortical lesions.
Discussion
The main purpose of this study was to evaluate if a combination of DIR and PSIR improved detection and classification of cortical lesions in MS compared with DIR alone. Accurate identification and classification of these lesions are important to understand the potential influence of cortical involvement in cognitive impairment and their impact on other aspects of clinical disability.
A secondary aim was to quantitatively assess the advantages, if any, of the combined use of DIR with PSIR over FLAIR. It is important to reemphasize that we did not include lesions that were visible on either DIR or PSIR alone; every lesion identified was clearly visible on both sequences. The combination of DIR and PSIR allowed us to confirm the presence of lesions, reject artifacts, and improve our ability to categorize the lesions. The use of DIR alone would likely result in slightly more lesions detected, but our observations suggest that such an increase would likely be from false-positive results from artifacts.
Our current knowledge about the in vivo behavior of lesions restricted to the cerebral cortex is limited. Newer techniques such as MTR and DTI have been able to show diffuse microscopic damage in gray and white matter,16–18 but they do not provide localization of lesions within the gray matter. DIR alone is highly sensitive to lesion foci within the cortex20 but is inherently SNR limited and does not depict lesion boundaries with enough accuracy to reliably distinguish purely intracortical lesions from those with intrusion into subcortical white matter. Accurate classification of purely intracortical lesions is the first step toward insight into mechanisms underlying their formation. Histopathologic studies have shown minimal inflammatory reaction and a predominance of subpial lesions in both MS5,25,26 and the marmoset experimental autoimmune encephalo myelitis (EAE) model,27 implying that these mechanisms may differ from lesions in white matter.
The DIR sequence used in the present study was a 2D acquisition, unlike the 3D technique described previously by Geurts et al.20 The traditional advantages of 3D methods compared with 2D are thin sections for reduced partial volume averaging and improved spatial resolution. However, section-interleaved acquisitions in 2D, as implemented in the current studies, can substantially reduce the “dead time” in a TR period, enabling additional signal intensity averaging to make up the SNR deficit. Our sequence used a total of 4 signal intensity averages, which, along with the higher field strength and considerably shorter TE, makes our 2D approach competitive with the 3D sequence described previously. With respect to image resolution, the voxel size of 2.7 mm3 in our 2D implementation compares favorably with the 2.8 mm3 voxels of the 3D method used by Geurts et al.20 Our findings relative to FLAIR suggest that the DIR method itself, regardless of its specific implementation, is the key to increased detection of lesions.
The primary limitation of this study was the relatively small number of subjects. An increased cohort size would have permitted prospective studies to explore possible correlations among cortical lesion load, cognitive impairment, EDSS, and duration of disease. Another limitation was that the section thickness of 3 mm used in our acquisitions likely resulted in partial-volume (PV) averaging across the cortical ribbon. This PV effect may either mask the presence of small cortical lesions or lead to a false classification of a given lesion as purely intracortical when, in fact, the lesion may have a subcortical extension. The PV effect is a concern for almost all imaging studies of cortical lesions in the literature and can only be ameliorated by high-resolution imaging methods.
Conclusions
Combined use of DIR and PSIR allows more reliable detection of cortical lesions in MS than DIR alone. The addition of PSIR also provides better delineation of lesion boundaries, which results in a more confident classification of lesions as purely intracortical, mixed, or juxtacortical. Accurate detection and classification of intracortical lesions are the first steps toward insight into their behavior in vivo, influence on progression of disease, and correlation with clinical manifestations of MS.
Acknowledgments
The authors thank Vipulkumar Patel for his expertise in acquiring the images and optimizing the acquisition protocol, and the University of Texas MR imaging-AC team for its assistance in image processing.
Footnotes
Portions of this work previously presented as a poster at: 22nd Congress of the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), September 29, 2006; Madrid, Spain.
This study was supported in part by the National Institutes of Health/National Institute of Biomedical Imaging and Bioengineering, grant R01 EB002095-05 (PAN).
References
- 1.Dawson JW. The histology of disseminated sclerosis. Trans Roy Soc Edinb 1916;50:517–740 [Google Scholar]
- 2.Brownell B, Hughes JT. The distribution of plaques in the cerebrum in multiple sclerosis. J Neurol Neurosurg Psychiatry 1962;25:315–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lumsden CE. The neuropathology of multiple sclerosis. In: Vinken PJ, Bruyn GW, eds. Handbook of Clinical Neurology. Vol. 9. Amsterdam: Elsevier Science Publishers;1970. :217–309
- 4.Bo L, Vedeler CA, Nyland HI, et al. Subpial demyelination in the cerebral cortex of multiple sclerosis patients. J Neuropathol Exp Neurol 2003;62:723–32 [DOI] [PubMed] [Google Scholar]
- 5.Brink BP, Veerhuis R, Breij EC, et al. The pathology of multiple sclerosis is location-dependent: no significant complement activation is detected in purely cortical lesions. J Neuropathol Exp Neurol 2005;64:147–55 [DOI] [PubMed] [Google Scholar]
- 6.Peterson JW, Bö L, Mörk S, et al. Transected neurites, apoptotic neurons, and reduced inflammation in cortical multiple sclerosis lesions. Ann Neurol 2001;50:389–400 [DOI] [PubMed] [Google Scholar]
- 7.Kidd D, Barkhof F, McConnell R, et al. Cortical lesions in multiple sclerosis. Brain 1999;122:17–26 [DOI] [PubMed] [Google Scholar]
- 8.Bakshi R, Ariyaratana S, Benedict RH, et al. Fluid-attenuated inversion recovery magnetic resonance imaging detects cortical and juxtacortical multiple sclerosis lesions. Arch Neurol 2001;58:742–48 [DOI] [PubMed] [Google Scholar]
- 9.Lazeron RH, Langdon DW, Filippi M, et al. Neuropsychological impairment in multiple sclerosis patients: the role of (juxta)cortical lesion on FLAIR. Mult Scler 2000;6:280–85 [DOI] [PubMed] [Google Scholar]
- 10.Geurts JJ, Bo L, Pouwels PJ, et al. Cortical lesions in multiple sclerosis: combined postmortem MR imaging and histopathology. AJNR Am J Neuroradiol 2005;26:572–77 [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma R, Narayana PA, Wolinsky JS. Grey matter abnormalities in multiple sclerosis: proton magnetic resonance spectroscopic imaging. Mult Scler 2001;7:221–26 [DOI] [PubMed] [Google Scholar]
- 12.Kapeller P, McLean MA, Griffin CM, et al. Preliminary evidence for neuronal damage in cortical grey matter and normal appearing white matter in short duration relapsing-remitting multiple sclerosis: a quantitative MR spectroscopic imaging study. J Neurol 2001;248:131–38 [DOI] [PubMed] [Google Scholar]
- 13.Narayana PA, Wolinsky JS, Rao SB, et al. Multicentre proton magnetic resonance spectroscopy imaging of primary progressive multiple sclerosis. Mult Scler 2004;10 Suppl 1:S73–78 [DOI] [PubMed] [Google Scholar]
- 14.Chard DT, Griffin CM, McLean MA, et al. Brain metabolite changes in cortical grey and normal-appearing white matter in clinically early relapsing-remitting multiple sclerosis. Brain 2002;125:2342–52 [DOI] [PubMed] [Google Scholar]
- 15.Geurts JJ, Reuling IE, Vrenken H, et al. MR spectroscopic evidence for thalamic and hippocampal, but not cortical, damage in multiple sclerosis. Magn Reson Med 2006;55:478–83 [DOI] [PubMed] [Google Scholar]
- 16.Bozzali M, Cercignani M, Sormani MP, et al. Quantification of brain gray matter damage in different MS phenotypes by use of diffusion tensor MR imaging. AJNR Am J Neuroradiol 2002;23:985–88 [PMC free article] [PubMed] [Google Scholar]
- 17.Rovaris M, Bozzali M, Iannucci G, et al. Assessment of normal-appearing white and gray matter in patients with primary progressive multiple sclerosis: a diffusion-tensor magnetic resonance imaging study. Arch Neurol 2002;59:1406–12 [DOI] [PubMed] [Google Scholar]
- 18.Dehmeshki J, Chard DT, Leary SM, et al. The normal appearing grey matter in primary progressive multiple sclerosis: a magnetisation transfer imaging study. J Neurol 2003;250:67–74 [DOI] [PubMed] [Google Scholar]
- 19.Bedell BJ, Narayana PA. Implementation and evaluation of a new pulse sequence for rapid acquisition of double inversion recovery images for simultaneous suppression of white matter and CSF. J Magn Reson Imaging 1998;8:544–47 [DOI] [PubMed] [Google Scholar]
- 20.Geurts JJ, Pouwels PJ, Uitdehaag BM, et al. Intracortical lesions in multiple sclerosis: improved detection with 3D double inversion-recovery MR imaging. Radiology 2005;236:254–60 [DOI] [PubMed] [Google Scholar]
- 21.Hou P, Hasan KM, Sitton CW, et al. Phase-sensitive T1 inversion recovery imaging: a time-efficient interleaved technique for improved tissue contrast in neuroimaging. AJNR Am J Neuroradiol 2005;26:1432–38 [PMC free article] [PubMed] [Google Scholar]
- 22.Huber AM, Schoenberg SO, Hayes C, et al. Phase-sensitive inversion-recovery MR imaging in the detection of myocardial infarction. Radiology 2005;237:854–60 [DOI] [PubMed] [Google Scholar]
- 23.Mai VM, Chen Q, Bankier AA, et al. Imaging pulmonary blood flow and perfusion using phase-sensitive selective inversion recovery. Magn Reson Med 2000;43:793–95 [DOI] [PubMed] [Google Scholar]
- 24.McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: Guidelines from the International Panel on the Diagnosis of Multiple Sclerosis. Ann Neurol 2001;50:121–27 [DOI] [PubMed] [Google Scholar]
- 25.Kutzelnigg A, Lucchinetti CF, Stadelmann C, et al. Cortical demyelination and diffuse white matter injury in multiple sclerosis. Brain 2005;128:2705–12 [DOI] [PubMed] [Google Scholar]
- 26.Bo L, Vedeler CA, Nyland H, et al. Intracortical multiple sclerosis lesions are not associated with increased lymphocyte infiltration. Mult Scler 2003;9:323–31 [DOI] [PubMed] [Google Scholar]
- 27.Pomeroy IM, Matthews PM, Frank JA, et al. Demyelinated neocortical lesions in marmoset autoimmune encephalomyelitis mimic those in multiple sclerosis. Brain 2005;128:2713–21 [DOI] [PubMed] [Google Scholar]