Abstract
SUMMARY: Solitary fibrous tumors are rare spindle cell neoplasms that typically occur in the thorax but have been described in various locations within the abdomen and head and neck region. The most common extrapleural site is the oral cavity, but these tumors have been also described in the orbit, nasopharynx, paranasal sinuses, salivary glands, and larynx.1–3 We describe a case of a solitary fibrous tumor of the buccal space successfully treated with percutaneous CT-guided cryoablation.
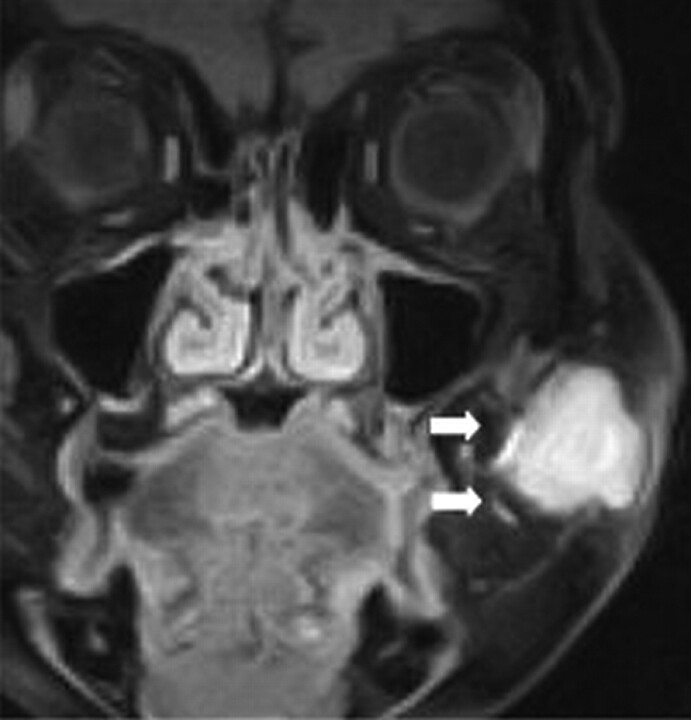
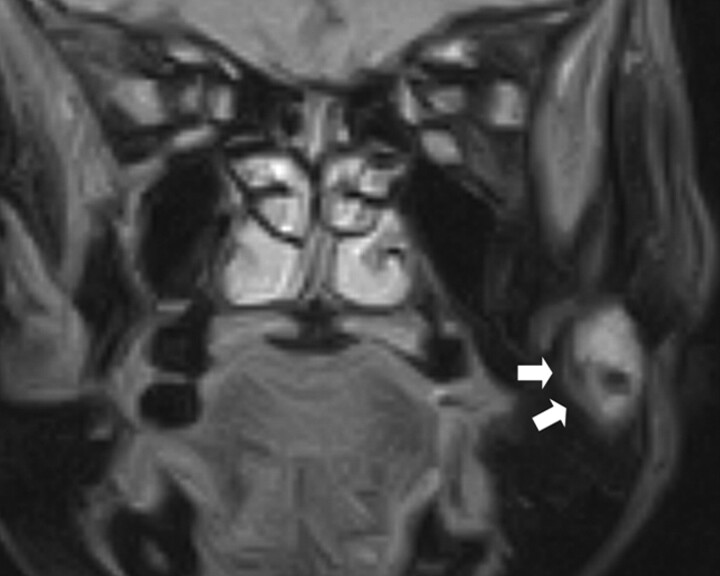
A 64-year-old woman was referred to our tumor ablation service with a complaint of progressive left facial swelling. The patient is from Puerto Rico and underwent an excisional biopsy of a left buccal space mass via a transoral approach approximately 1 year before presentation. A solid, encapsulated soft-tissue tumor was found intraoperatively. There was disruption of the capsule during removal, preventing complete excision. Pathology demonstrated a World Health Organization low-grade solitary fibrous tumor (SFT) of the buccal space with 2–3 mitotic cells per 10 high-power fields, which was CD34+ on immunohistochemical staining. Physical examination at current presentation revealed a firm, mobile, and nontender mass in the left malar soft tissues resulting in facial asymmetry. There was no numbness or facial paralysis. The overlying skin appeared normal. Oropharyngeal examination revealed no evidence of ulceration. Facial CT scan showed an enhancing mass within the left buccal space, which appeared isoattenuated to muscle. There was no calcification or necrosis, nor was there bony destruction of the mandible or maxilla. MR imaging at 0.3T revealed a well-circumscribed solid mass measuring 2.6 × 3.2 × 1.7 cm that was separate from the masseter muscle and that displaced the parotid duct and facial vein medially. The mass was isointense compared with muscle on T1-weighted precontrast images and was heterogeneous in appearance on T2-weighted sequences, containing areas of hyperintensity and hypointensity. There was homogeneous strong enhancement, most consistent with a presumed residual or recurrent SFT (Fig 1). The patient declined surgical reexcision because of the risk of facial nerve injury and for cosmetic reasons and, therefore, elected to have this lesion treated with percutaneous thermal ablation.
Fig 1.
Coronal T1-weighted MR image after intravenous gadolinium-DTPA shows a homogeneously enhancing mass in the left buccal space (arrows).
Written, informed consent was obtained from the patient before the start of the procedure. Coagulation parameters were normal. Percutaneous cryoablation was performed in the supine position via a left transmalar approach with local anesthesia and moderate sedation using intravenous midazolam hydrochloride and fentanyl. CT fluoroscopy was used for imaging guidance. Cryoablation was performed with an argon-based cryoablation system (Endocare, Mountain View, Calif) with 1.7-mm–diameter percutaneous applicators. The applicators have a 3-cm active tip and create a freeze zone of approximately 3 cm (length) by 2 cm (width). Two cryoapplicators were placed simultaneously into the mass in a parallel fashion with the tips approximately 1 cm apart (Fig 2A). Temperatures were measured during the procedure with an attached thermocouple (range, −94°C to −136°C) at the tip. Active thawing of the freeze zone was achieved using helium. The patient underwent 2 consecutive 10-minute freeze-thaw cycles. Interval unenhanced CT evaluation showed a small crescent of soft tissue not optimally treated with the freeze zone. The cryoapplicators were then repositioned into this superolateral aspect of the mass, and 2 additional 8-minute freeze-thaw cycles were performed. The freeze zone measured 3.3 × 4.5 × 3.0 cm on immediate posttreatment CT imaging and encompassed the mass along with a peripheral 5-mm margin around the mass (Fig 2B). The patient was observed for a 2-hour period after the procedure and was discharged home in stable condition.
Fig 2.
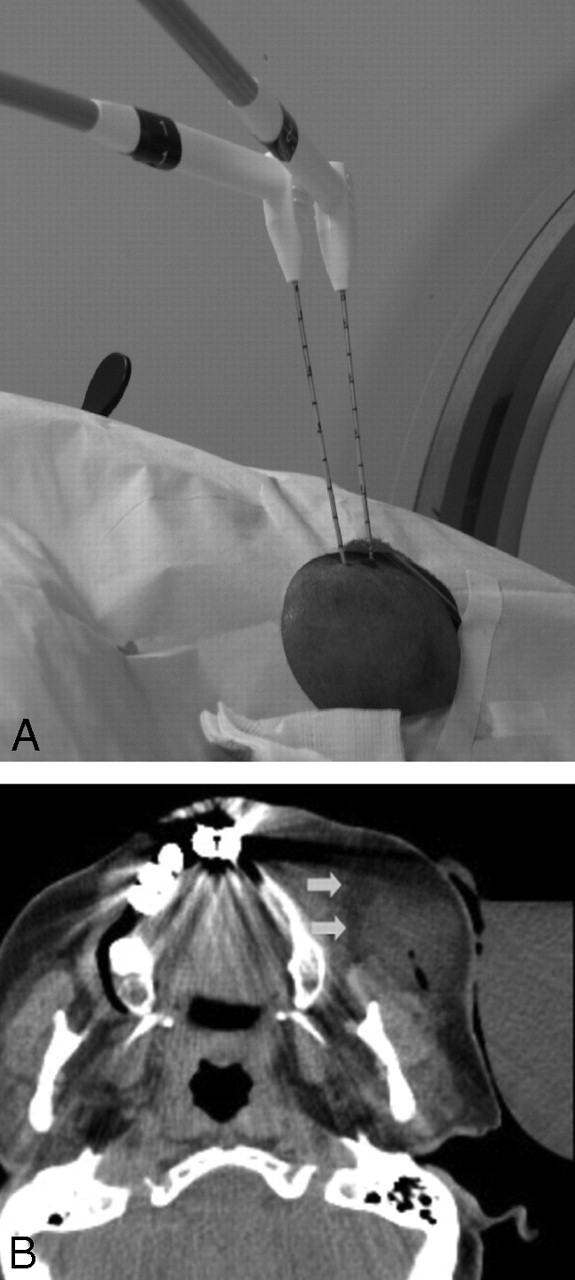
A, Procedural photograph during the CT-guided cryoablation showing 2 cryoapplicators positioned within the left cheek mass. B, Axial CT image after the last freeze shows the extent of the ice ball (arrows) beyond the medial margin of the mass. Note central needle tract from cryoapplicator.
At 2-day follow-up visit, there was some swelling of the malar soft tissues. A small eschar was noted on the skin surface along with sloughing of the buccal mucosal surface related to thermal injury. However, this completely resolved at 6-month follow-up. The patient experienced no residual pain, and there was no evidence of sensory or motor nerve deficit or duct injury. Routine follow-up MR imaging at 6 months revealed an organized fluid collection within the buccal soft tissues measuring approximately 2 cm compatible with posttreatment changes, with only a small area of peripheral enhancement. A sonography-guided fine needle aspiration was performed to evaluate for recurrence. Cytology revealed necrotic cells without evidence of tumor. Follow-up MR imaging at 14 months showed near-complete collapse of the treatment cavity with minimal posterior residual peripheral enhancement (Fig 3). The patient's facial swelling had resolved, and her external appearance returned to normal. Despite the low-grade pathology of the tumor, continued imaging surveillance will be performed, given the recurrent nature of the original neoplasm.
Fig 3.
Fourteen-month follow-up coronal T1-weighted MR image after intravenous gadolinium-diethylene-triaminepentaacetic acid shows a small area of residual enhancement (arrows) along with central hypointensity representing coagulative necrosis.
Discussion
SFTs are spindle cell tumors that are typically associated with serosal surfaces, especially the pleura, but have been found to arise in various extrapleural locations, most notably the oral cavity. They typically present as a slow-growing, painless mass. SFTs of the thorax usually have a favorable prognosis. However, they have been reported to be malignant in 13%–23% of cases.2,3 Factors associated with malignancy include high cellularity, more than 4 mitoses per 10 high-power fields, pleomorphism, hemorrhage, and necrosis.3 Extrapleural SFTs, however, are almost always benign and are cured with simple surgical excision. In this patient, who developed a recurrence despite low-grade pathology and who refused surgery, percutaneous thermal ablation was proposed as a treatment alternative.
Additional diagnostic considerations for a mass involving the buccal space include tumors of minor salivary gland origin, such as pleomorphic adenoma, adenoid cystic carcinoma, or mucoepidermoid carcinoma, along with hemangioma, lymphoma, squamous cell carcinoma, lipoma, soft tissue sarcoma, abscess, lymph node, and nerve sheath tumor. However, because other buccal space masses can present in the same fashion, and because the imaging appearance of many of these processes is nonspecific, the diagnosis is based on the microscopic appearance and characteristic immunohistochemical staining. CD34, a transmembrane glycoprotein, has been found to be a highly sensitive marker for SFTs. Radiographically, they are characteristically isoattenuated to muscle on noncontrast CT and isointense to muscle and brain on noncontrast T1- and T2-weighted MR imaging. They typically enhance avidly in a homogeneous fashion after contrast administration. Some variability in MR imaging characteristics has been described, however, with T2 heterogeneity being the most commonly described alternative imaging appearance,4–6 as was seen in our case subject.
Percutaneous cryoablative techniques have been described for the treatment of primary neoplastic and metastatic disease in various organ systems, most notably the liver and prostate. Recent literature has also shown benefit in palliating painful bony and extra-abdominal soft-tissue metastases using percutaneous image-guided cryoablation.7,8 Benefits of this minimally invasive treatment option include the absence of a surgical scar, reduced recovery time, and the ability to visualize the treated tumor both during and immediately after the procedure to determine treatment success. Probe diameters have also decreased in recent years, further making use of this technique to other sites of disease safer and easier with less postprocedural bleeding. Cryoablation offers a few specific advantages over heat-based therapies. These include less procedural pain due to the anesthetic effect of freezing; direct visualization of the ice ball with CT, MR imaging, or ultrasound so that the treatment margins can be monitored in real time, with less disruption of underlying supportive tissue making it safer for lesions next to skin, nerve, and hollow viscera; and the ability to treat lesions with multiple applicators so that large and irregularly shaped masses can be ablated at one sitting.
Within the head and neck region, thermal ablative techniques using radiofrequency energy have been described to treat adenoid cystic carcinoma and recurrent thyroid carcinoma.9,10 However, to our knowledge, this is the first reported use of percutaneous cryoablation to treat a mass in this region. Further investigation of the possible benefits of cryoablation over excision for benign masses would be beneficial.
References
- 1.Goodlad JR, Fletcher CD. Solitary fibrous tumor arising at unusual sites: analysis of a series. Histopathology 1991;19:512–22 [DOI] [PubMed] [Google Scholar]
- 2.Hanau CA, Miettinen M. Solitary fibrous tumor: histological and immunohistochemical spectrum of benign and malignant variants presenting at different sites. Hum Pathol 1995;26:440–49 [DOI] [PubMed] [Google Scholar]
- 3.England DM, Hochholzer L, McCarthy MJ. Localized benign and malignant fibrous tumors of the pleura: a clinicopathologic review of 223 cases. Am J Surg Pathol 1989;13:640–58 [DOI] [PubMed] [Google Scholar]
- 4.Ganly I, Patel SG, Stambuk HE, et al. Solitary fibrous tumors of the buccal space. Arch Otolaryngol Head Neck Surg 2006;132:517–25 [DOI] [PubMed] [Google Scholar]
- 5.Shin JH, Sung IY, Suh JH, et al. Solitary fibrous tumor in the buccal space: MR findings with pathologic correlation. AJNR Am J Neuroradiol 2001;22:1890–92 [PMC free article] [PubMed] [Google Scholar]
- 6.Dunfee BL, Sakai O, Spiegel JH, et al. Solitary fibrous tumor of the buccal space. AJNR Am J Neuroradiol 2005;26:2114–16 [PMC free article] [PubMed] [Google Scholar]
- 7.Callstrom MR, Atwell TD, Charboneau JW, et al. Painful metastases involving bone: percutaneous image-guided cryoablation–prospective trial interim analysis. Radiology 2006;241:572–80 [DOI] [PubMed] [Google Scholar]
- 8.Beland MD, Dupuy DE, Mayo-Smith WW. Percutaneous cryoablation of symptomatic extraabdominal metastatic disease: preliminary results. AJR Am J Roentgenol 2005;184:926–30 [DOI] [PubMed] [Google Scholar]
- 9.Monchik JM, Donatini G, Iannuccilli J, et al. Radiofrequency ablation and percutaneous ethanol injection treatment for recurrent local and distant well-differentiated thyroid carcinoma. Ann Surg 2006;244:296–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bui Q, Dupuy DE. Percutaneous CT-guided radiofrequency ablation of an adenoid cystic carcinoma of the head and neck. AJR Am J Roentgenol 2002;179:1333–35 [DOI] [PubMed] [Google Scholar]