Abstract
SUMMARY: Four patients underwent angioplasty and stenting of medically refractory symptomatic intracranial atherosclerosis with the new Wingspan stent system. In all 4 patients, CT angiography (CTA) showed an abnormality within the stented segment that was suggestive of nonocclusive in-stent thrombus. However, subsequent conventional angiography findings were typical for in-stent restenosis. The CTA imaging features of in-stent restenosis are important to recognize, and the misinterpretation of in-stent restenosis as in-stent thrombus may result in inappropriate management.
Intracranial atherosclerosis accounts for up to 10% of the 700,000 new strokes that occur in the United States each year.1 Medical therapy has a poor prognosis, and endovascular therapy of this disease has previously been limited due to device technology.2–4 Recently, the Gateway balloon and Wingspan stent (Boston Scientific, Natick, Mass) have been released for treatment of medically refractory significant intracranial stenosis.5 Little is known about the noninvasive imaging appearance of this device in follow-up after treatment.
CT angiography (CTA) appears promising as a noninvasive tool for evaluating the status of intracranial stents, but limited literature on this topic exists.6 Extensive case series are beginning to appear in the coronary literature.7, 8 We report the CTA appearance of in-stent restenosis in 4 patients who underwent Wingspan placement.
Materials and Methods
All studies were reviewed under an institutional review board–approved protocol. CT studies were performed on either a 16- or 64-section GE LightSpeed CT scanner (GE Healthcare, Waukesha, Wis). Postprocessing was performed on an Advantage Windows Workstation using CT perfusion software version 3.0 (GE Healthcare).
CTA data were acquired with a helical acquisition by using a 0.5-second rotation speed and a collimation of 2.5 mm with 50% overlap. The data were prospectively reconstructed to 1.25 collimation with a 0.625 interval. For technique, we used a kilovolt of 120 and automilliampere, setting the highest automilliampere value at 440 mA by using 12 as a noise factor (220 mAs). A pitch of 1.35 and a table speed of 13.75 allow tracking the contrast bolus in the arterial phase. CTA was performed with a 100-mL bolus of 370-mg/dL nonionic contrast media at an injection rate of 3 mL/s, followed by a 50-mL saline flush. The timing bolus requires an additional 20 mL of contrast. Axial, sagittal, and coronal overlapping thick-slab 2D maximum-intensity-projection reformations were made by using 10-mm sections with a 2.5-mm overlap. Additional magnified curved multiplanar reformations (MPRs) were performed focusing on the stented vessel segment, using a 0.625-mm slab thickness.
Sample Case
A 38-year-old woman with a history of diabetes, hypertension, and hypercholesterolemia presented with recurrent paresthesias, refractory to medical management. Angioplasty of a middle cerebral artery (MCA) stenosis was not durable; symptomatic restenosis occurred within weeks. She was then referred to our institution for intracranial stent placement. CTA showed a critical stenosis of the right M1 segment of the MCA, which was verified with digital subtraction angiography (DSA) (Fig 1A). She was continued on clopidogrel and aspirin and underwent angioplasty and stent placement (3 × 9 mm Gateway balloon and a 3.5 × 15 mm Wingspan stent) with good results (Fig 1B). CTA follow-up at 1 month showed the stented segment to be widely patent (Fig 1C). Three-month follow-up CTA performed because of recurrent symptoms showed a filling defect within the stent (Fig 1D). Curved thin-section MPRs focusing on the stented segment revealed the filling defect along the caudal aspect of the stent with contrast seen circumferentially around the filling defect, suggestive of a thrombus (Fig 1E).
Fig 1.
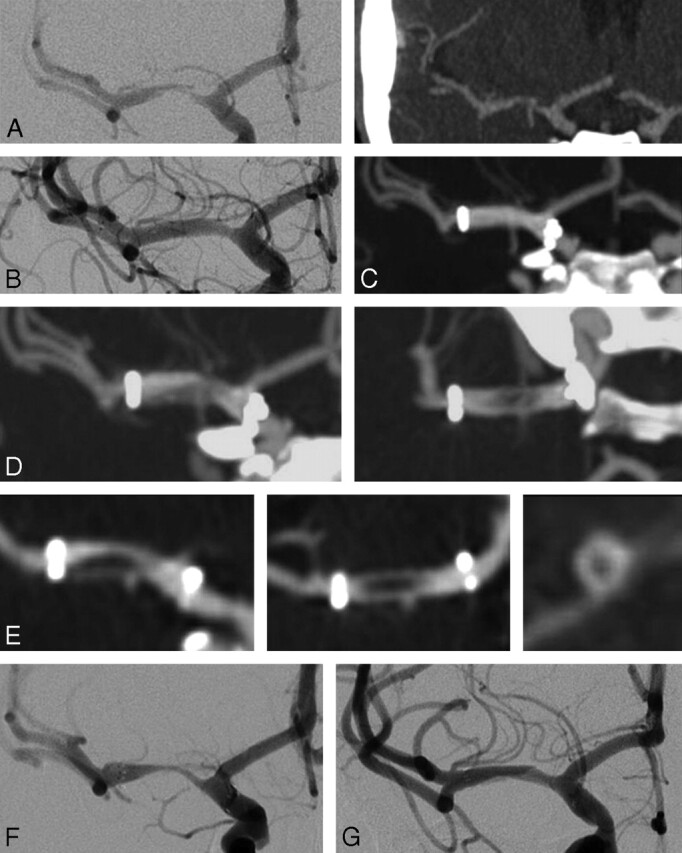
A–G, A 38-year-old woman with right MCA stenosis refractory to medical therapy and prior angioplasty. Serial imaging details restenosis and eventual angioplasty.
Because of the potential risk of distal emboli associated with an attempt at repeat angioplasty, the patient's medication was changed to warfarin (Coumadin) and aspirin, and the patient was followed for an additional 4 months. CTA again showed an irregular nonocclusive filling defect within the stent. DSA demonstrated a significant smooth tapering in-stent restenosis (Fig 1F). Balloon angioplasty (3 × 9 mm Gateway balloon) resulted in resolution of the restenosis and symptoms (Fig 1G).
Other Cases
Three other patients with restenosis following successful angioplasty and stent placement with the Wingspan system (2 MCAs and 1 supraclinoid internal carotid artery) showed similar findings with irregular nonocclusive filling defects seen on CTA within the Wingspan stent; DSA in all of these patients confirmed the restenosis but showed no evidence of intraluminal thrombus.
Discussion
There is meager literature describing the CTA appearance of in-stent restenosis associated with the Wingspan stent. In our early experience with this device, we have encountered 4 patients who, at the time of follow-up with CTA, were found to have an intraluminal filling defect suggestive of thrombus. However, on further DSA evaluation, these filling defects were found to represent in-stent restenosis.
The ability of CTA to image the lumen within cerebrovascular stents is primarily limited by CT-related artifacts.6 Blooming effects result in stent struts that appear thicker and are exaggerated by any adjacent vascular calcification.9 The stent composition and design can also play a role in the blooming effect and overall degree of artifact.10 The Wingspan stent is composed of nitinol and has an open cell design, thin struts, and a relatively low metal surface area coverage, which results in less beam hardening and scatter artifacts compared with conventional coronary stents (Fig 2A, B). Optimal intraluminal contrast enhancement is also important for reducing intrastent artifact and accurately imaging the intrastent lumen. A final limitation of CTA lies with partial volume averaging due to the small size of the cerebral vessels. All CTA scans use 0.625-mm isotropic voxels with additional thin-section curved MPRs from either a 16- or 64-section CT scanner to minimize volume-averaging effects.
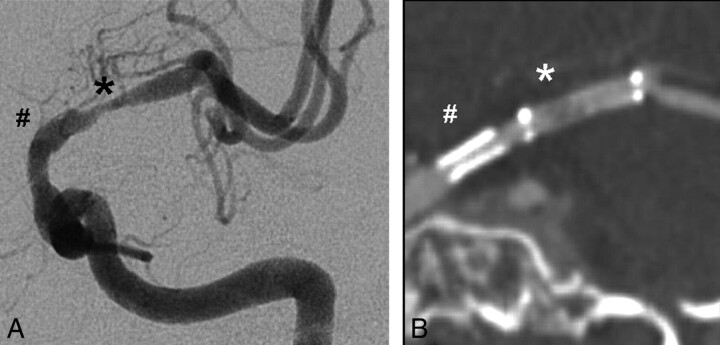
Fig 2.
MCA in-stent restenosis with correlative CTA (A) and DSA (B). This patient previously required a coronary stent (number sign) for critical supraclinoid stenosis proximal to the Wingspan stent (asterisk) in the adjacent MCA. Note the extensive blooming effect related to the coronary stent in comparison with the adjacent Wingspan stent.
Because CTA is increasingly used as a technique for evaluation and follow-up of patients who have undergone intracranial stent placement, it is important that the possibility of false-positive studies indicating intraluminal thrombus be appreciated. Because of the management implications when a finding suggestive of an intraluminal thrombus is seen on a CTA in these patients, confirmation with DSA should be strongly considered. Further studies are required to determine both the cause and the frequency of this CTA finding.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics: 2005 Update. Dallas: American Heart Association;2005
- 2.SSYLVIA Study Investigators. Stenting of symptomatic atherosclerotic lesions in the vertebral or intracranial arteries (SSYLVIA): study results. Stroke 2004;35:1388–92 [DOI] [PubMed] [Google Scholar]
- 3.Kessler IM, Mounayer C, Piotin M, et al. The use of balloon-expandable stents in the management of intracranial arterial diseases: a 5-year single-center experience. AJNR Am J Neuroradiol 2005;26:2342–48 [PMC free article] [PubMed] [Google Scholar]
- 4.Wojak JC, Dunlap DC, Hargrave KR, et al. Intracranial angioplasty and stenting: long-term results from a single center. AJNR Am J Neuroradiol 2006;27:1882–92 [PMC free article] [PubMed] [Google Scholar]
- 5.Henkes H, Miloslavski E, Lowens S, et al. Treatment of intracranial atherosclerotic stenoses with balloon dilatation and self-expanding stent deployment (WingSpan). Neuroradiology 2005;47:222–28. Epub 2005 Mar 15 [DOI] [PubMed] [Google Scholar]
- 6.Trossbach M, Hartmann M, Braun C, et al. Small vessel stents for intracranial angioplasty: in vitro evaluation of in-stent stenoses using CT angiography. Neuroradiology 2004;46:459–63 [DOI] [PubMed] [Google Scholar]
- 7.Roguin A, Resar JR. CT angiography is here: are we expected to see a change of angiography referral pattern? Int J Cardiovasc Intervent 2005;7:152–54 [DOI] [PubMed] [Google Scholar]
- 8.Pugliese F, Cademartiri F, van Mieghem C, et al. Multidetector CT for visualization of coronary stents. Radiographics 2006;26:887–904 [DOI] [PubMed] [Google Scholar]
- 9.Nieman K, Cademartiri F, Raaijmakers R, et al. Noninvasive angiographic evaluation of coronary stents with multi-slice spiral computed tomography. Herz 2003;28:136–42 [DOI] [PubMed] [Google Scholar]
- 10.Maintz D, Juergens KU, Wichter T, et al. Imaging of coronary artery stents using multislice computed tomography: in vitro evaluation. Eur Radiol 2003;13:830–35 [DOI] [PubMed] [Google Scholar]