Abstract
BACKGROUND AND PURPOSE: A dacryocystocele forms when tears accumulate within the lacrimal sac as a result of an obstruction more distally in the lacrimal drainage apparatus, which may occur as a complication of sinonasal surgery. The purpose of this study was to define the imaging characteristics of a postoperative dacryocystocele occurring after surgery for sinonasal cancer and to review the anatomy of the nasolacrimal drainage apparatus.
MATERIALS AND METHODS: We reviewed the clinical records and imaging findings of 8 patients who underwent surgery for sinonasal cancer and were diagnosed with a postoperative dacryocystocele between August 2001 and November 2005. The imaging studies performed at the time of diagnosis of dacryocystocele were CT in 6 patients and MR imaging in 2 patients.
RESULTS: On both CT and MR imaging, dacryocystoceles had a characteristic appearance of a fluid collection with thin rim enhancement along the course of the affected nasolacrimal duct, with no adjacent solid components. In none of the patients was the dacryocystocele confused with a recurrent tumor.
CONCLUSION: Dacryocystocele after surgery for sinonasal cancer has a characteristic appearance on CT and MR imaging. Familiarity with this complication of sinonasal surgery and its appearance on imaging will enable radiologists to avoid misinterpreting dacryocystocele as a recurrent tumor or another process.
A dacryocystocele forms when tears accumulate within the lacrimal sac as a result of an obstruction more distal within the lacrimal drainage apparatus. The causes of dacryocystocele include congenital deformities, trauma, primary and recurrent tumors affecting the nasolacrimal duct, idiopathic blockage of the nasolacrimal duct, and iatrogenic causes, including treatment of head and neck cancer in the sinonasal region.1,2 For the radiologist interpreting head and neck imaging studies in patients previously treated for cancer, it is imperative to avoid mistaking a dacryocystocele for a recurrent tumor to ensure that the patient receives the correct treatment, including a dacryocystorhinostomy (DCR). The purpose of this study was to define the imaging characteristics of postoperative dacryocystocele occurring after surgery for sinonasal cancer and to provide a better understanding of the anatomy of the nasolacrimal drainage apparatus.
Materials and Methods
The Institutional Review Board approved this study and waived the requirement for informed consent. We reviewed the clinical data and imaging studies of 8 patients who underwent surgery for sinonasal cancer and were diagnosed with postoperative dacryocystocele between August 2001 and November 2005.
Initial imaging was performed after resection of the sinonasal tumor. CT scanning was performed on GE scanners (LightSpeed; GE Healthcare, Milwaukee, Wis) after intravenous administration of contrast. The following parameters were used for the studies: section thickness, 1.25 to 5 mm; FOV, 180 to 250; 120 to 140 kVp; 180 to 220 mA. MR examinations were performed with a 1.5T unit (GE Healthcare). Pregadolinium T1-weighted (TR, 400–600; TE, 9–13) images and T2-weighted (TR, 3470–5800; TE, 90–100) images as well as gadolinium-enhanced (0.1 mmol/kg) T1-weighted images were reviewed.
Results
Eight patients (4 men and 4 women) with an age range of 32 to 93 years (mean, 61.4 years) had undergone at least a partial maxillectomy, and 4 patients had also undergone an ethmoidectomy. Two patients had squamous cell carcinoma; 1 patient each had sinonasal undifferentiated carcinoma, adenoid cystic carcinoma, osteosarcoma, chondrosarcoma, melanoma, and inverted papilloma. The interval between tumor resection and radiologic diagnosis of dacryocystocele ranged from 1 month to 57 months (median, 3 months).
Three of the 8 patients had undergone radiation therapy that ended 11.5 months to 25 years (median, 54 months) before the radiologic diagnosis of dacryocystocele and had also undergone chemotherapy that ended 1 to 10.5 months (median, 4.5 months) before the radiologic diagnosis of dacryocystocele. One patient had started chemotherapy 3.5 months before the radiologic diagnosis of dacryocystocele and was still receiving chemotherapy at the time of diagnosis.
Seven of the 8 patients were symptomatic at the time of diagnosis: 3 presented with dacryocystitis (infection of the lacrimal sac), 2 with epiphora (excessive tearing), 1 with both dacryocystitis and epiphora, and 1 with frontal headaches. One patient was asymptomatic and had the dacryocystocele detected on routine postsurgical follow-up imaging. The 4 patients with clinical symptoms of dacryocystitis did not have appreciable findings on imaging. All 8 patients had a dacryocystocele on the same side as the primary sinonasal tumor and surgery.
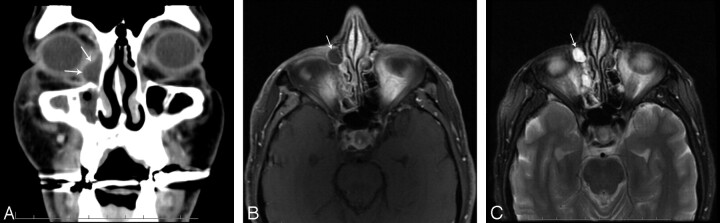
The imaging studies performed at the time of diagnosis of dacryocystocele were CT in 6 patients and MR imaging in 2 patients. In all 8 patients, the dacryocystocele had a characteristic appearance on both CT and MR imaging (Fig 1) of a cystic, fluid-filled structure with no adjacent solid components, within the anteromedial aspect of the orbit, in the lacrimal sac, measuring between 8 and 14 mm (mean, 10 mm).
Fig 1.
A 52-year-old man, status post right maxillectomy for resection of soft palate adenoid cystic carcinoma with a right dacryocystocele. A, Coronal CT. Cystic, fluid-filled structure within the anteromedial aspect of the right orbit, adjacent to the nasolacrimal duct (arrows). B, Axial T1 postgadolinium. Thin peripheral enhancement around the dacryocystocele (arrow). C, Axial T2. Appearance of a dacryocystocele as a cystic, fluid-filled structure within the anteromedial aspect of the right orbit (arrow).
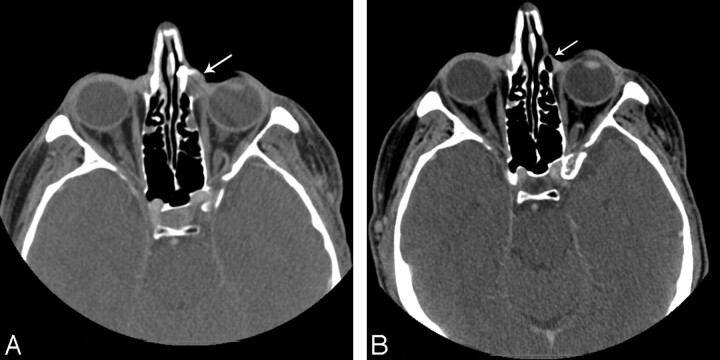
Four of the 8 patients underwent a DCR with placement of a silicone tube. Three of these patients had follow-up with CT or MR imaging between 14 and 56 months (mean, 37 months) after this treatment and had no evidence of recurrent dacryocystocele (Fig 2). The fourth patient underwent DCR with silicone tube placement shortly before this report and had not yet had follow-up imaging at the time of this writing. One of the patients treated with DCR did have a recurrent sinonasal chondrosarcoma, unrelated to the dacryocystocele, on follow-up imaging, and this chondrosarcoma was treated with surgical resection.
Fig 2.
A 52-year-old man, status post left maxillectomy and ethmoidectomy for resection of a radiation-induced osteosarcoma of the maxilla, before and after surgery. A, Axial CT. Dacryocystocele in the left medial canthal region (arrow). B, Axial CT. Resolution of the dacryocystocele (arrow) after dacryocystorhinostomy and placement of a silicone tube.
In 1 patient, the dacryocystocele resolved with conservative management as confirmed by CT 5 months after diagnosis. In another patient, conservative management resulted in a decrease in the size of the dacryocystocele from 11 × 8 mm at diagnosis to 10 × 6 mm on follow-up CT 20 months after diagnosis. That patient had no clinical symptoms of epiphora or dacryocystitis at the time of this report. Another patient was undergoing chemotherapy and radiation therapy for treatment of the sinonasal tumor at the time of this report and was scheduled to have the dacryocystocele reassessed on completion of that treatment. The final patient died of the sinonasal cancer.
Discussion
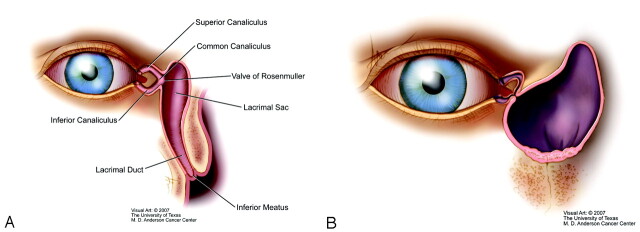
The lacrimal drainage apparatus (Fig 3A) begins in the medial aspect of the orbit with 2 orifices known as the superior and inferior puncta. These orifices drain into 2 canaliculi, superior and inferior, which then form a common canaliculus. The valve of Rosenmuller, which lies at the junction of the common canaliculus and the lacrimal sac, prevents the reflux of tears back into the canaliculus. The lacrimal sac is located within the inferomedial wall of the orbit known as the lacrimal sac fossa. The lacrimal sac is oval and measures 12 to 15 mm. The nasolacrimal duct is a membranous canal extending inferiorly for about 18 mm from the nasolacrimal sac to the inferior meatus of the nasal cavity.
Fig 3.
A, Anatomy of the nasolacrimal drainage apparatus. Note the position of the nasolacrimal duct. B, Illustration of a dacryocystocele with cystic dilation of the lacrimal sac.
The cause of a dacryocystocele in patients with sinonasal cancer may result from the tumor itself 3 or may be related to ablative surgery,3,4 radiation therapy,5 or various chemotherapeutic drugs with canalicular stenosis as a known side effect such as docetaxel or 5-flourouracil.6–8 All of these treatments are known to cause damage to the lacrimal drainage apparatus with resultant blockage of the nasolacrimal duct and, in some instances, dilation of the lacrimal sac and thus formation of a dacryocystocele (Fig 3B).
Patients with dacryocystocele may present clinically with a pink or blue mass in the medial canthal region. Obstruction of the nasolacrimal duct may lead to epiphora. Secondary infection of a dilated lacrimal sac may lead to dacryocystitis and mucopurulent discharge and/or periorbital or facial cellulitis.1 Unless there are imaging findings such as preseptal soft tissue swelling1,9 or adjacent bone destruction, the diagnosis of dacryocystitis is generally made on a clinical basis. In our series, 4 patients had clinical symptoms of dacryocystitis that could not be appreciated with imaging.
Our findings regarding the CT appearance of postoperative dacryocystocele after resection of a sinonasal malignant tumor are similar to those reported in case reports of infants with congenital dacryocystoceles. For example, Meyer et al10 stated that the CT criteria for dacryocystocele in infants include the following triad: cystic medial canthal mass, dilation of the nasolacrimal sac, and a submucosal nasal cavity mass. Rand et al11 reported that the CT findings in 4 infants with congenital dacryocystoceles were cystic dilation of the lacrimal sac and a thin-walled cystic mass with slight rim enhancement. Glatt et al3 described a technique known as computed tomographic dacryocystography in which contrast medium is placed into the canaliculi and fills the dacryocystocele. This technique may aid in excluding recurrent tumor and provide guidance to the surgeon in operative planning.
The findings on MR imaging in our study were similar to those reported in several case reports of prenatal and childhood dacryocystoceles. Bianchini et al12 described the appearance of a prenatal dacryocystocele on MR imaging without contrast enhancement as a T2 homogenous, hyperintense cystic mass within the medial canthal region. Farrer et al13 reported that a congenital dacryocystocele in a 3-year-old child appeared on MR imaging as a 1.0-cm mass with low signal intensity on T1-weighted images and T2 signal hyperintensity. The mass was centered in the region of the medial canthus and extended inferiorly into the nasal cavity, elevating the inferior turbinate.
The most worrisome alternative diagnosis that would need to be considered in the differential diagnosis of dacryocystocele in patients previously treated for head and neck cancer is recurrent sinonasal cancer or a second primary tumor in the medial canthal region. However, our study demonstrates that the characteristic imaging appearance of a dacryocystocele is quite different from that of a recurrent tumor, which should be associated with a solid enhancing mass. On imaging diagnosis of a dacryocystocele, a careful search for a recurrent tumor along the course of the lacrimal duct, down to the inferior meatus in the nasal cavity, should be performed to exclude a tumor as the cause of the dacryocystocele.
Treatment options for dacryocystocele and associated dacryocystitis, which is often recurrent and chronic, include conservative management with placement of warm compresses, massaging of the blocked lacrimal sac, and administration of systemic antibiotics.14 If conservative treatment is not successful, then a DCR may be performed. This procedure involves creating an iatrogenic bypass opening between the lacrimal sac and the middle meatus of the nasal cavity. Silicone tubes may be placed at the time of surgery to act as stents to improve the likelihood of long-term success for this operation. Diba et al15 have shown that DCR alleviates blockage of the nasolacrimal duct in most patients with head and neck tumors and is not associated with unusual complications. In patients who are not good candidates for DCR because of significant medical comorbidities, a simple incision and drainage of the infected lacrimal sac can be performed in the office, with the patient under local anesthesia. This latter procedure does not alleviate epiphora but can relieve the acute inflammatory signs and acute infection associated with the dacryocystitis, which is often associated with the finding of a dacryocystocele on imaging studies.
Conclusion
Our report suggests that postoperative dacryocystocele in patients with sinonasal cancer has a characteristic appearance on CT and MR imaging of a cystic, fluid-filled structure with thin rim enhancement and no solid components. Our report further suggests that once the radiologist is familiar with these imaging characteristics and also has an understanding of the anatomic mechanisms that underlie formation of a dacryocystocele and the clinical scenarios that may lead to formation of a dacryocystocele in patients with head and neck cancer, it is unlikely that a dacryocystocele in such a patient would be mistaken for a recurrent tumor. Correct imaging diagnosis of a dacryocystocele will lead to the appropriate surgical or medical therapy and prevent complications such as an unnecessary biopsy or surgical resection of this benign process.
Acknowledgments
We thank Stephanie Deming for assistance in the preparation of this manuscript and David Aten for developing the illustrations of the nasolacrimal duct anatomy and dacryocystocele.
Footnotes
Previously presented at: Annual Meeting of the American Society of Neuroradiology, May 1–5, 2006; San Diego, Calif.
References
- 1.Shashy RG, Durairaj V, Holmes JM, et al. Congenital dacryocystocele associated with intranasal cysts: diagnosis and management [published erratum appears in Laryngoscope 2005;115:759]. Laryngoscope 2003;113:37–40 [DOI] [PubMed] [Google Scholar]
- 2.Bhaya M, Meehan R, Har-El G. Dacryocystocele in an adult: endoscopic management. Am J Otolaryngol 1997;18:131–34 [DOI] [PubMed] [Google Scholar]
- 3.Glatt HJ, Chan AC. Lacrimal obstruction after medial maxillectomy. Ophthalmic Surg 1991;12:757–58 [PubMed] [Google Scholar]
- 4.Osguthorpe JD, Weissman RA. ‘Medial maxillectomy’ for lateral nasal wall neoplasms. Arch Otolarygol Head Neck Surg 1991;117:751–56 [DOI] [PubMed] [Google Scholar]
- 5.Gordon KB, Char DH, Sagerman RH. Late effects of radiation of the eye and ocular adnexa. Int J Radiat Oncol Biol Phys 1995;31:1123–39 [DOI] [PubMed] [Google Scholar]
- 6.Esmaeli B, Ahmadi MA, Rivera E, et al. Docetaxel secretion in tears: association with lacrimal damage obstruction. Arch Ophthalmol 2002;120:1180–82 [PubMed] [Google Scholar]
- 7.Agarwal MR, Esmaeli B, Burnstine MA. Squamous metaplasia of the canaliculi associated with 5-fluorouracil: a clinicopathologic case report. Ophthalmology 2002;109:2359–61 [DOI] [PubMed] [Google Scholar]
- 8.Esmaeli B, Amin S, Valero V, et al. Prospective study of incidence and severity of epiphora and canalicular stenosis in patients with metastatic breast cancer receiving docetaxel. J Clin Oncol 2006;24:3619–22 [DOI] [PubMed] [Google Scholar]
- 9.Asheim J, Spickler E. CT demonstration of dacryolithiasis complicated by dacryocystitis. AJNR Am J Neuroradiol 2005;26:2640–41 [PMC free article] [PubMed] [Google Scholar]
- 10.Meyer JR, Quint DJ, Holmes JM, et al. Infected congenital mucocele of the nasolacrimal duct. AJNR Am J Neuroradiol 1993;14:1008–10 [PMC free article] [PubMed] [Google Scholar]
- 11.Rand PK, Ball WS, Kulwin DR. Congenital nasolacrimal mucoceles: CT evaluation. Radiology 1989;173:691–94 [DOI] [PubMed] [Google Scholar]
- 12.Bianchini E, Zirpoli S, Righini A, et al. Magnetic resonance imaging in prenatal diagnosis of dacryocystocele: report of 3 cases. J Comput Assist Tomogr 2004;28:422–27 [DOI] [PubMed] [Google Scholar]
- 13.Farrer RS, Mohammed TL, Hahn FJ. MRI of childhood dacryocystocele. Neuroradiology 2003;45:259–61 [DOI] [PubMed] [Google Scholar]
- 14.Schnall BM, Christian CJ. Conservative treatment of congenital dacryocele. J Pediatr Ophthalmol Strabismus 1996;33:219–22 [DOI] [PubMed] [Google Scholar]
- 15.Diba R, Saadati H, Esmaeli B. Outcomes of dacryocystorhinostomy in patients with head and neck tumors. Head Neck 2005;27:72–75 [DOI] [PubMed] [Google Scholar]