Abstract
BACKGROUND AND PURPOSE: An increase in the common carotid artery intima-media thickness (CCA-IMT) is generally considered an early marker of atherosclerosis. This cross-sectional study assessed the CCA-IMT and plaque score as vascular risk factors in patients with ischemic stroke and type 2 diabetes.
MATERIALS AND METHODS: Brain MR imaging and carotid ultrasonography were performed in 133 subjects with type 2 diabetes. IMT was measured at both CCAs. Differences in the variables between case and control subjects were compared statistically. To determine the independent factors related to CCA-IMT and plaque score, we performed stepwise multiple regression analysis.
RESULTS: Sex, current smoking habit, history of hypertension, and high-density lipoprotein (HDL) levels differed significantly between the case and control groups. CCA-IMT and plaque score in patients with diabetes and acute ischemic stroke were significantly greater than in patients with diabetes who were stroke-free. The crude odds ratios suggested that CCA-IMT and plaque score are risk factors of acute ischemic stroke in patients with type 2 diabetes. However, when we adjusted for cerebrovascular risk factors, CCA-IMT and plaque score did not remain significantly associated with acute ischemic stroke.
CONCLUSION: Increased CCA-IMT and plaque score are associated with acute ischemic stroke in patients with type 2 diabetes. The higher CCA-IMT and plaque score found in ischemic stroke in patients with type 2 diabetes seem to be induced by cerebrovascular risk factors. Therefore, to prevent ischemic stroke in patients with type 2 diabetes, strict control of hyperglycemia, hypertension, smoking, and low HDL, together with monitoring of CCA-IMT and carotid plaque, may be important.
B-mode sonography is a noninvasive method for examining the walls of peripheral arteries and provides a measure of intima-media thickness (IMT) and the presence of stenosis and plaques. The IMT corresponds to the intima-media complex, which comprises endothelial cells, connective tissue, and smooth muscle and is the site of lipid deposition in plaque formation. The IMT of the carotid artery is an established sonographic marker for early atherosclerosis, and thickening of the intima-media complex reflects generalized atherosclerosis.1–6
Several studies have shown an association between increased carotid IMT and myocardial infarction or stroke in elderly and middle-aged subjects.1,7–9 Increased common carotid artery (CCA)-IMT has been reported under various conditions, including hypertension, dyslipidemia, obesity, diabetes, smoking, and cardiovascular disease, including ischemic stroke. In patients with type 2 diabetes, aging, hypertension, duration of diabetes, hyperglycemia, dyslipidemia, and smoking have been identified as significant risk factors for stroke.4,10
Several studies have shown that diabetes mellitus is one of the main risk factors for cerebrovascular disease. Therefore, identifying patients with diabetes with a high risk of developing a cerebral infarction is of great clinical importance.4,11–14 Carotid plaques are frequently found in patients who have suffered a stroke.15 Few studies have specifically investigated the relationship between ischemic stroke and CCA-IMT and carotid plaques in type 2 diabetes. Therefore, we examined the relationship between IMT and plaque score and the development of cerebral infarction in patients with type 2 diabetes. In addition, we investigated the relationship between various risk factors and IMT and plaque score in these subjects.
Subjects and Methods
The cases of acute first-time ischemic stroke in patients with type 2 diabetes who visited our neurology ward were collected between January 2004 and December 2005. A stroke was defined as rapidly developing signs of focal or global disturbance of cerebral function lasting more than 24 hours with no apparent cause other than vascular. Acute ischemic stroke was confirmed based on clinical presentation, diffusion-weighted MR imaging, and apparent diffusion coefficient maps. Patients with isolated transient ischemic attack, stroke as a result of apparent cardioembolic origin, or a history of previous stroke were excluded. Cerebral infarction was categorized into lacunar infarction, cortical infarction (including territorial and borderzone infarctions), and large subcortical infarction.
Control subjects with type 2 diabetes were recruited from patients with symptoms such as headache, migraine, and dizziness during the same period. In total, 133 subjects with type 2 diabetes, including 44 case subjects and 89 control subjects, underwent both brain MR imaging and carotid ultrasonography. At the time of enrollment, laboratory data, blood pressure, and anthropometric measurements were collected for each patient.
The traditional risk factors for cerebrovascular disease in both case and control subjects—age, sex, body mass index, history of hypertension, history of smoking, low-density and high-density lipoprotein (HDL) cholesterol levels, triglyceride levels, hemoglobin (Hb) A1c levels, and ischemic heart disease—were also evaluated. The survey on smoking was based on the participants' recall. Smoking was defined as having at least 1 cigarette daily, as well as having smoked in the past. Nonsmoking was defined as self-reported lifetime abstinence.
Brain MR Imaging
All subjects underwent brain MR imaging. Patients with acute ischemic stroke underwent brain MR imaging within 2 days from the onset of symptoms. The median time between brain infarction and CCA-IMT evaluation was 8.1 days (range, 1–78 days) for case subjects and 7.5 days between brain MR imaging and CCA-IMT evaluation (range, 0–80 days) for control subjects. Diffusion-weighted, T1- and T2-weighted, and fluid-attenuated inversion recovery (FLAIR) images were obtained with a 1.5T Gyroscan Intera system (Philips, Bothell, Wash).
Carotid Ultrasonography
We confined IMT measurements to the CCA because of the relatively common occurrence of plaques at the origin of the internal carotid artery (ICA). All case and control subjects underwent ultrasonography of both carotid arteries. CCA-IMT and plaque score were evaluated using high-resolution sonography equipped with a linear transducer at 7.5 MHz in B mode (HDI 5000 SonoCT; Philips), and one neuroradiologist examined the results.
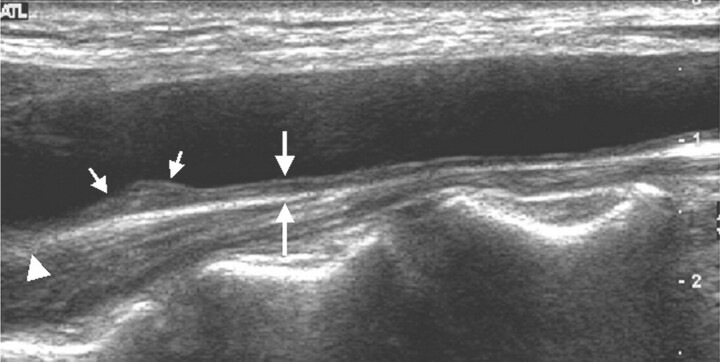
We assessed the presence of plaques in the CCA, bifurcation, and ICA, and defined plaques as focal widening of the vessel wall of more than 50% relative to adjacent segments, with protrusion into the lumen, composed of calcified or noncalcified components. Protrusion was visually determined. The total plaque score reflected the total number of sites with plaques and ranged from 0 to 6 (each of the CCAs, bifurcations, and ICAs, bilaterally). To access CCA-IMT, we focused on far-wall IMT, because far-wall measurements are considered more valid than near-wall measurements. IMT of the far wall was defined as the distance between the leading edge of the lumen-intima interface and the leading edge of the media-adventitia interface (Fig 1).
Fig 1.
Longitudinal scan of carotid ultrasonogram. Measurement of CCA-IMT (large arrows) at the far wall of the common carotid artery is shown. The carotid plaque (small arrows) in the distal common carotid artery is seen. The arrowhead represents carotid bifurcation.
Far-wall IMT of both CCAs was measured at 3 sites (thickest point, and at sites 1 cm upstream and downstream, free from plaque) using Digimatic calipers (Mitutoyo, Kawasaki, Japan) on the longitudinal views. The maximum and mean IMT of the carotid arteries were assessed. The mean CCA-IMT was defined as the mean IMT of the right and left CCAs, calculated from 3 measurements on each side. The maximum CCA-IMT (max CCA-IMT) was defined as the average of the thickest wall of the right and left CCAs. If there was uniform intimal thickening in the CCA, we measured intimal thickness every 1 cm from the bifurcation to the end of the CCA. Then, we made 3 measurements: at the thickest point and 1 cm upstream and downstream.
Statistical Analysis
IMT values were log transformed to obtain a normal distribution. Differences in variables between case and control subjects were analyzed for statistical significance by using the t test, Wilcoxon rank-sum test, χ2 test, and Fisher exact test. Multiple logistic regression analysis was performed to calculate the odds ratio of ischemic stroke associated with increased CCA-IMT and plaque score by adjusting for available risk factors of stroke.
Results
The baseline characteristics of the study subjects are shown in Table 1. Forty-four acute ischemic stroke cases were confirmed by imaging studies. They comprised 26 lacunar infarctions, 12 cortical infarctions, including territorial and borderzone infarctions, and 6 large subcortical infarctions. Significant differences were observed between the case and control groups in sex, current smoking habit, history of hypertension, and HDL levels.
Table 1:
Clinical characteristics of case and control subjects with type 2 diabetes
| Control Subjects (89) | Case Subjects (44) | P | |
|---|---|---|---|
| Age, years | 62.2 ± 10.6 | 64.0 ± 9.3 | .33 |
| Male sex | 55.8% | 44.2% | .03 |
| Smoking (Y) | 11.1% | 34.7% | .02 |
| Hypertension (Y) | 51.2% | 70.7% | .03 |
| HDL-C (>40 mmol/L) | 62.5% | 30.9% | .001 |
| LDL-C (>130 mmol/L) | 41.6% | 27.3% | .32 |
| Triglyceride, mmol/L | 195.9 ± 46.5 | 187.5 ± 42.2 | .14 |
| BMI, kg/m2 | 25.9 ± 3.49 | 24.6 ± 2.79 | .32 |
| HbA1c > 7, % | 72.9% | 69.1% | .65 |
| IHD (Y) | 12.1% | 12.5% | 1.00 |
Note:—Y indicates yes; HDL-C, high-density lipoprotein-cholesterol; LDL-C, low-density lipoprotein-cholesterol; BMI, body mass index; Hb, hemoglobin; IHD, ischemic heart disease. Continuous data are presented as mean ± SD, noncontinuous data as percentages.
The CCA-IMT (max IMT and mean IMT) and plaque score in the case subjects were higher than in control subjects (Table 2). In addition, the crude odds ratios suggested that CCA-IMT and plaque score were risk factors for of acute ischemic stroke in patients with type 2 diabetes (Table 3). However, after adjusting for the significant variables in Table 1, the statistical significance disappeared.
Table 2:
IMT and plaque score in case and control subjects
| Control Subjects (89) | Case Subjects (44) | P | |
|---|---|---|---|
| Log mean IMT (m (sd)) | −0.186 (0.23) | −0.098 (0.22) | .04 |
| Log max IMT (m (sd)) | −0.043 (0.27) | 0.067 (0.27) | .03 |
| Plaque score | |||
| 0 | 45.5% | 21.4% | <.001 |
| 1–3 | 50.0% | 26.1% | |
| 4–6 | 4.5% | 26.1% |
Note:—IMT indicates intima-media thickness.
Table 3:
Association between CCA-IMT and plaque score and ischemic stroke on multiple logistic regression analysis
| Odds Ratio | 95% CI |
||
|---|---|---|---|
| Lower | Upper | ||
| Log (mean IMT) | |||
| Crude | 5.29 | 1.05 | 26.7 |
| Adjusted* | 1.64 | 0.14 | 19.4 |
| Log (max. IMT) | |||
| Crude | 4.58 | 1.16 | 18.1 |
| Adjusted* | 2.08 | 0.24 | 18.1 |
| Plaque score | |||
| Crude | 3.14 | 1.67 | 5.93 |
| Adjusted* | 2.14 | 0.80 | 5.73 |
Note:—CCA-IMT indicates common carotid artery intima-media thickness; CI, confidence interval.
Adjusted for sex, smoking habit, high-density lipoprotein, and hypertension history
Discussion
The development of sonography technology has allowed the noninvasive evaluation of atherosclerosis in the carotid arteries. The initial manifestation of carotid atherosclerosis is characterized by a subtle increase in vascular IMT, the progression of which leads to plaque formation and vascular narrowing. Reflecting systemic atherosclerosis, increased CCA-IMT is associated with a higher risk for stroke.2,16–19
In a case-control study,9 increased IMT was associated with an increased risk of stroke. In another study,7 an association between increased IMT and the risk of incident stroke was observed; the relative risk increased in a linear fashion with increasing IMT and was of the same magnitude as the relative risk for myocardial infarction. Touboul et al3 observed that an increased CCA-IMT was associated with brain infarctions, both overall and in the main subtypes, and concluded that an increased IMT may help to identify patients at high risk for brain infarction. Several studies5,20,21 have demonstrated the potential value of CCA-IMT and plaque score for assessing the risk of atherothrombotic infarction and lacunar infarction but not for other stroke subtypes, such as cardioembolic infarction, cerebral hemorrhage, and other or unclassified stroke. They demonstrated that atherosclerosis does not play an important role in cardioembolic infarction, cerebral hemorrhage, and other or unclassified stroke.
In addition, the existence of carotid artery plaques is associated with increased risk of stroke, irrespective of their location. In neurologically asymptomatic subjects, carotid plaques are likely to be both markers of generalized atherosclerosis and sources of thromboemboli.15,17,22–24 Kitamura et al16 reported that wall thickening of the CCA and the formation of uncalcified plaque in the ICA were positively associated with an increased risk of stroke in elderly Japanese men. Ebrahim et al2 showed that carotid artery plaques were more strongly associated with elevated cardiovascular risk than a diffuse increase in IMT.
Based on these findings, carotid atherosclerosis, even in the absence of advanced stenosis, appears to be associated with a risk of stroke. Therefore, we evaluated the value of CCA-IMT and plaque score for identifying patients with type 2 diabetes at high risk of cerebral infarction.
We demonstrated that increased CCA-IMT and plaque score correlated with acute ischemic stroke in patients with type 2 diabetes. Sex, history of smoking, history of hypertension, and low HDL were statistically significant in the case subjects. However, after we adjusted for these 4 factors, CCA-IMT and plaque score did not remain significantly associated with acute ischemic stroke, indicating though that CCA-IMT and plaque score are not independent cerebrovascular risk factors.
Although many studies have reported that CCA-IMT and plaque score are independent risk factors for ischemic stroke, even after adjusting for conventional risk factors,1–5,7 our results showed that CCA-IMT and plaque score were not independent factors for ischemic stroke. CCA-IMT is associated with modifiable (eg, blood pressure, blood cholesterol, smoking, diabetes, and obesity) and nonmodifiable risk factors (age, sex, genes, and currently unknown risk factors).18
An increased carotid IMT has been observed in patients with type 2 diabetes. Diabetes itself might be of crucial importance for the development of atherosclerosis because of the clustering of various interrelated metabolic disturbances, as well as hyperglycemia. The cause of atherosclerosis in type 2 diabetes could be sought in the glucose toxicity to the endothelium and glycosylation processes, as indicated by the higher levels of plasma glucose and HbA1c in patients with diabetes, as well as in the significant increase in cardiovascular risk factors. Therefore, they emphasize that hyperglycemia and clustering of conventional risk factors are related to IMT.25 Kawamori et al10 reported that aging, hypertension, dyslipidemia, duration of diabetes, and smoking habits were related to CCA-IMT. Epidemiologic studies have reported associations between a range of cerebrovascular risk factors and IMT; Temelkova-Kurktschiev et al25 also reported a trend between a greater number of risk factors, and a thicker intima-media.4
Hence, we argue that because IMT reflects exposure to cerebrovascular risk factors, IMT itself may not play a direct role in ischemic infarction and that it can be considered an intermediate factor in the causal pathway between clinical risk factors and stroke. Therefore, to prevent atherosclerosis of the carotid arteries in patients with type 2 diabetes, strict control of hypertension, hyperglycemia, smoking habits, and dyslipidemia seem to be important.
Therapeutic interventions with blood pressure-lowering agents and lipid-lowering agents, as well as multifactorial interventions in patients with diabetes, can slow the progression of or even reduce carotid IMT. Carotid IMT has been recently recognized as a surrogate marker for evaluating therapeutic interventions in atherosclerotic disease.14,18,26
One limitation of our study is that it focused on acute stroke only and did not include diabetic subjects with chronic ischemic stroke or isolated transient ischemic attack (TIA). In future, the relationship between IMT and plaque score and ischemic stroke must be examined in all patients with diabetes, segregating them into patients with strokes (TIA, acute, and chronic) and without strokes.
Conclusion
Increased CCA-IMT and plaque score were correlated with acute ischemic stroke in patients with type 2 diabetes. However, the greater CCA-IMT and plaque score found in ischemic stroke for patients with type 2 diabetes seem to be induced by cerebrovascular risk factors prevalent in patients with diabetes, and CCA-IMT and plaque score seem to be vascular risk factors that reflect the degree of exposure to cerebrovascular risk factors. Therefore, CCA-IMT and plaque score in patients with type 2 diabetes can be considered intermediate factors in the causal pathway between cerebrovascular risk factors and ischemic stroke, not independent factors for ischemic stroke.
To prevent ischemic stroke in patients with type 2 diabetes, strict control of hyperglycemia, hypertension, smoking, and dyslipidemia, together with monitoring of CCA-IMT and carotid plaque, may be important. Large prospective studies are need to establish the link between earlier carotid atherosclerosis and the future stroke risk in patients with type 2 diabetes.
References
- 1.Cupini LM, Pasqualetti P, Diomedi M, et al. Carotid artery intima-media thickness and lacunar versus nonlacunar infarcts. Stroke 2002;33:689–94 [DOI] [PubMed] [Google Scholar]
- 2.Ebrahim S, Papacosta O, Whincup P, et al. Carotid plaque, intima media thickness, cardiovascular risk factors, and prevalent cardiovascular disease in men and women: The British Regional Heart Study. Stroke 1999;30:841–50 [DOI] [PubMed] [Google Scholar]
- 3.Touboul PJ, Elbaz A, Koller C, et al. Common carotid artery intima-media thickness and brain infarction: the Etude du Profil Genetique de l'Infarctus Cerebral (GENIC) case-control study: the GENIC Investigators. Circulation 2000;102:313–18 [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto K, Sera Y, Nakamura H, et al. Correlation between common carotid arterial wall thickness and ischemic stroke in patients with type 2 diabetes mellitus. Metabolism 2002;51:244–247 [DOI] [PubMed] [Google Scholar]
- 5.Vemmos KN, Tsivgoulis G, Spengos K, et al. Common carotid artery intima-media thickness in patients with brain infarction and intracerebral hemorrhage. Cerebrovasc Dis 2004;17:280–86 [DOI] [PubMed] [Google Scholar]
- 6.Davis PH, Dawson JD, Riley WA, et al. Carotid intima-medial thickness is related to cardiovascular risk factors measured from childhood through middle age. The Muscatine study. Circulation 2001;104:2815–19 [DOI] [PubMed] [Google Scholar]
- 7.O'Leary DH, Polak JF, Kronmal RA, et al. Carotid artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 1999;340:14–22 [DOI] [PubMed] [Google Scholar]
- 8.Hodis HN, Mack WJ, LaBree L, et al. The role of carotid arterial intima-media thickness in predicting clinical coronary events. Ann Intern Med 1998;128:262–69 [DOI] [PubMed] [Google Scholar]
- 9.Bots ML, Hoes AW, Koudstaal PJ, et al. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation 1997;96:1432–1437 [DOI] [PubMed] [Google Scholar]
- 10.Kawamori R, Yamasaki Y, Matsushima H, et al. Prevalence of carotid atherosclerosis in diabetic patients. Diabetes Care 1992;15:1290–94 [DOI] [PubMed] [Google Scholar]
- 11.Nakatou T, Nakata K, Nakamura A, et al. Carotid hemodynamic parameters as risk factors for cerebral infarction in type 2 diabetic patients. Diabet Med 2004;21:223–29 [DOI] [PubMed] [Google Scholar]
- 12.Fujishima M, Kiyohara Y, Kato I, et al. Diabetes and cardiovascular disease in a prospective population survey in Japan: the Hisayama study. Diabetes 1996;45:S14–S16 [DOI] [PubMed] [Google Scholar]
- 13.Tanizaki Y, Kiyohara Y, Kato I, et al. Incidence of risk factors for subtypes of cerebral infarction in a general population: the Hisayama study. Stroke 2000;31:2616–22 [DOI] [PubMed] [Google Scholar]
- 14.Beishuizen ED, Van de Ree MA, Jukema JW, et al. Two-year statin therapy does not alter the progression of intima-media thickness in patients with type 2 diabetes without manifest cardiovascular disease. Diabetes Care 2004;27:2887–92 [DOI] [PubMed] [Google Scholar]
- 15.Sabetai MM, Tegos TJ, Nicolaides AN, et al. Hemispheric symptoms and carotid plaque echomorphology. J Vasc Surg 2000;31:39–49 [DOI] [PubMed] [Google Scholar]
- 16.Kitamura A, Iso H, Imano H, et al. Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke 2004;35:2788–94 [DOI] [PubMed] [Google Scholar]
- 17.Nagai Y, Kitagawa K, Sakaguchi M, et al. Significance of earlier carotid atherosclerosis for stroke subtypes. Stroke 2001;32:1780–85 [DOI] [PubMed] [Google Scholar]
- 18.Touboul PJ, Labreuche J, Vicaut E, et al. GENIC Investigators. Carotid intima-media thickness, plaques, and Framingham risk score as independent determinants of stroke risk. Stroke 2005;36:1741–45 [DOI] [PubMed] [Google Scholar]
- 19.Bonithon-Kopp C, Touboul PJ, Berr C, et al. Relation of intima-media thickness to atherosclerotic plaques in carotid arteries. The Vascular Aging (EVA) Study. Arterioscler Thromb Vasc Biol 1996;16:310–16 [DOI] [PubMed] [Google Scholar]
- 20.Tsivgoulis G, Vemmos KN, Spengos K, et al. Common carotid artery intima-media thickness for the risk assessment of lacunar infarction versus intracerebral hemorrhage. J Neurol 2005;252:1093–100 [DOI] [PubMed] [Google Scholar]
- 21.Nagai Y, Kitagawa K, Yamagami H, et al. Carotid artery intima-media thickness and plaque score for the risk assessment of stroke subtypes. Ultrasound Med Biol 2002;28:1239–43 [DOI] [PubMed] [Google Scholar]
- 22.Hollander M, Bots ML, Del Sol AI, et al. Carotid plaques increase the risk of stroke and subtypes of cerebral infarction in asymptomatic elderly: the Rotterdam study. Circulation 2002;105:2872–77 [DOI] [PubMed] [Google Scholar]
- 23.Polak JF, Shemanski L, O'Leary DH, et al. Hypoechoic plaque at US of the carotid artery: an independent risk factor for incident stroke in adults aged 65 years or older. Cardiovascular Health Study [published erratum appears in Radiology 1998;209:288–89]. Radiology 1998;208:649–54 [DOI] [PubMed] [Google Scholar]
- 24.Rothwell PM. Carotid artery disease and the risk of ischaemic stroke and coronary vascular events. Cerebrovasc Dis 2000;10:21–33 [DOI] [PubMed] [Google Scholar]
- 25.Temelkova-Kurktschiev TS, Koehler C, Leonhardt W, et al. Increased intima-media thickness in newly developed type 2 diabetes. Diabetes Care 1999;22:333–38 [DOI] [PubMed] [Google Scholar]
- 26.Hedblad B, Wikstrand J, Janzon L, et al. Low-dose metoprolol CR/XL and fluvastatin slow progression of carotid intima-media thickness: Main results from the Beta-Blocker Cholesterol-Lowering Asymptomatic Plaque Study (BCAPS). Circulation 2001;103:1721–26 [DOI] [PubMed] [Google Scholar]