Abstract
SUMMARY: MR imaging has found abnormalities compatible with low-grade edema in the brain of patients with cirrhosis that have been related to hepatic encephalopathy. We present 3 patients with hepatic encephalopathy who exhibit supratentorial focal or diffuse white matter lesions compatible with small-vessel brain disease. The volume and number of white matter lesions reduced with the improvement of hepatic encephalopathy, suggesting the participation of the blood-brain barrier in the pathogenesis of brain edema in hepatic encephalopathy.
MR studies of the brain have described several abnormalities in cirrhosis.1–3 These abnormalities appear to be relevant, because it has been postulated that low-grade brain edema is involved in the pathogenesis of hepatic encephalopathy (HE).4 The previous studies and recent experimental evidence5 indicate that brain edema in liver failure is mainly located in white matter. White matter lesions (WMLs) are often seen on MR images of elderly people and have been related to cognitive decline.6 WMLs are attributed to degenerative small-vessel disease and are progressive. The development of WMLs can be prevented with adequate treatment of vascular risk factors,7 but once present, they are considered irreversible areas of demyelination, gliosis, and loss of axons.8 We observed 3 patients with HE and T2 hyperintense focal WMLs who experienced an important decrease in their volume with the improvement of HE.
Cases
Case 1
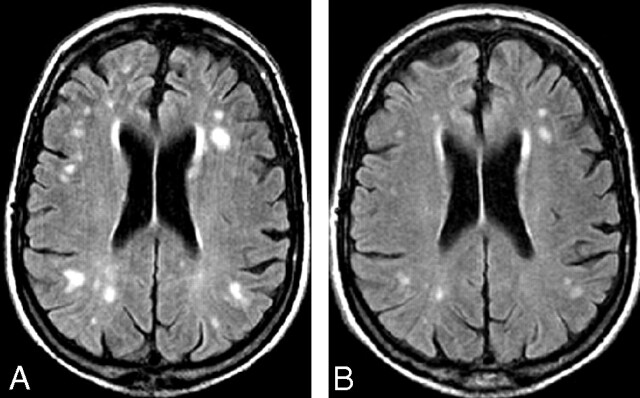
A 70-year-old male patient with hepatitis C cirrhosis and a history of myocardial infarction developed an episode of HE in 2003. After the episode of HE, he showed fluctuating manifestations of cognitive decline (apathy, inattention, and somnolence), compatible with persistent HE. In 2004, his liver function showed a Child Pugh Score of 7. At that time, the neurologic examination revealed that he was disoriented in time and showed bradykinesia. Brain MR imaging showed multifocal supratentorial WMLs (Fig 1A), and neuropsychologic assessment indicated severe impairment. The treatment of HE was optimized. Neomycin and branched chain amino acids were prescribed, and furosemide was withdrawn. Six months later, a follow-up MR imaging demonstrated a decrease in the number and size of WMLs (Fig 1B) associated with a significant improvement of the neuropsychologic function. Lesion volume from fast fluid-attenuated inversion recovery (FLAIR) images were outlined on hard copies. The lesion volumes were measured semiautomatically by a previously trained operator with the program DispImage9 (Dave Plummer, University College London Hospitals, London, UK. Available at: http://www.ucl.ac.uk/MedPhys/toast/misc/dispimg.htm) by using the hard copies as reference.
Fig 1.
A, MR image (transverse T2-weighted fast-FLAIR images, 9900 ms/110 ms/2500 ms/1 [TR/TE/inversion time/acquisitions]) obtained in patient 1 at baseline, while showing signs of overt hepatic encephalopathy. The image shows multiple focal supratentorial WMLs (total lesion volume, 7,507 mm3). B, Patient 1 after improvement of hepatic encephalopathy: MR shows a clear reduction in size and number of these focal WMLs (final lesion volume of 2,033 mm3).
Case 2
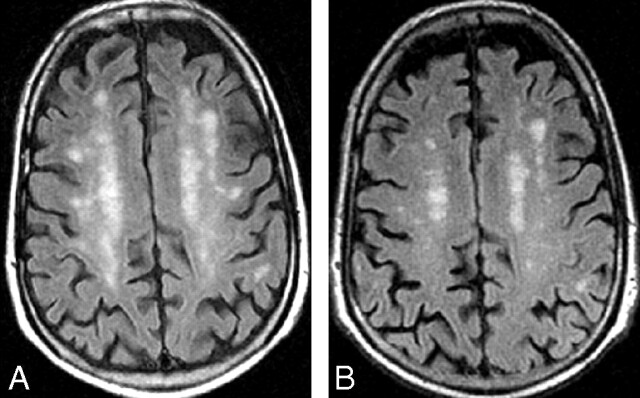
A 65-year-old male patient with alcoholic cirrhosis and a history of insulin-dependent diabetes mellitus developed an episode of HE in 2004. After the episode of HE, he experienced manifestations of persistent HE. In May 2006, his Child Pugh Score was 13. At neurologic examination, he was oriented but exhibited flapping tremor, slurred speech, and bradykinesia, and neuropsychologic assessment indicated severe impairment. Brain MR imaging showed diffuse WMLs (Fig 2A). He was receiving diuretics that were withdrawn, and neomycin and branched chain amino acids were prescribed. After 1 month, the extension of WMLs (calculated in the same way as in case 1) decreased (Fig 2B). On physical examination, he appeared more rapid on mental processing, and the family reported an obvious improvement of daily activities.
Fig 2.
A, MR image (transverse T2-weighted fast-FLAIR images, 9900 ms/110 ms/2500 ms/1 [TR/TE/inversion time/acquisitions ]) obtained in patient 1 at baseline, while showing signs of overt hepatic encephalopathy. The scan shows multiple diffuse supratentorial WMLs (total lesion volume, 25,901 mm3). B, Patient 2 after improvement of hepatic encephalopathy: MR shows a clear reduction in size and number of diffuse WMLs (final lesion volume, 16,586 mm3).
Case 3
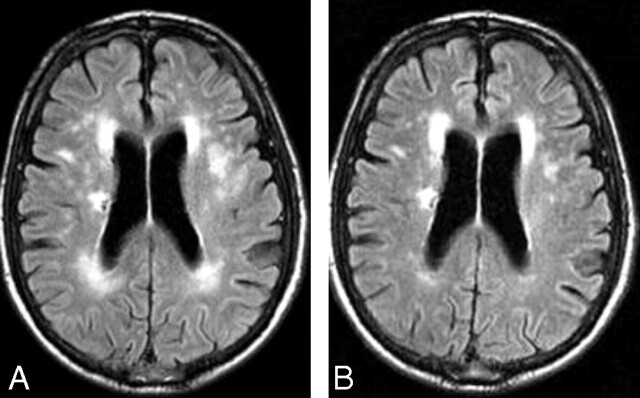
A 73-year-old male patient with hepatitis C cirrhosis was referred with a history of arterial hypertension and a lacunar infarction in 1990 that caused left hemiparesis. In 2004, when his Child Pugh Score was 10, he developed gait disturbance accompanied by bradykinesia that was attributed to vascular Parkinsonism. In 2005, he experienced 2 episodes of confusion and worsening left hemiparesis of several days’ duration that were diagnosed as episodic HE. A brain MR imaging, performed during the second episode (Fig 3A) showed, in addition to a chronic lacunar infarct within the right centrum ovale, multifocal subcortical and periventricular WML. He was discharged and received treatment with neomycin. A follow-up MR imaging was obtained 6 months later (Fig 3B), which showed a decrease in size and volume of the WML, calculated in the same way as in case 1. At that time, neurologic examination was unremarkable except for mild left hemiparesis with pyramidal signs, and the neuropsychologic assessment showed only mild impairment on attention and speed of mental processing.
Fig 3.
A, MR image (transverse T2-weighted fast-FLAIR images, 9900 ms/110 ms/2500 ms/1 [TR/TE/inversion time/acquisitions]) obtained in patient 3 at baseline, while showing signs of overt hepatic encephalopathy. MR shows multiple focal WMLs (total lesion volume, 18,601 mm3). B, Patient 3 after improvement of hepatic encephalopathy: MR shows clear reduction in size and number of focal WMLs (final lesion volume, 10,393 mm3).
Discussion
The present study shows supratentorial focal and diffuse WMLs compatible with small-vessel brain disease in 3 patients with cirrhosis and HE. These lesions, which are common in the general population, have probably been observed in patients with cirrhosis more frequently than reported.10 They are secondary to arteriolosclerosis and usually attributed to advanced age or hypertension.6 Thus, they have probably been ignored and interpreted as signs of normal involutive or chronic ischemic changes. In accordance with the interpretation of an ischemic source of their WMLs, the 3 patients of our study exhibited vascular risk factors.
The remarkable finding of our study is not the presence of WMLs but the observation that the volume and number of WMLs can be reduced with the improvement of HE. WMLs are considered irreversible consequences of small-vessel disease. The neuropathologic substrate of WMLs is a combination of perivascular demyelination, edema, gliosis, loss of axons, and glial cells accompanied by spongiosis. Of the different elements that constitute the neuropathologic substrate of WMLs, the one that can reverse in a short period of time is edema. The residual WML after improvement of HE probably corresponds with gliosis and other irreversible processes. MR studies in patients with minimal HE have demonstrated an increase in brain water, which may be involved in the pathogenesis of neurologic manifestations.11 The decrease of WMLs in parallel to the improvement of HE in the 3 patients of our study is in accordance with the association between brain edema and HE. Changes in the volume of edema in areas of small vessel-induced lesion support the participation of the blood-brain barrier in the pathogenesis of brain edema in liver failure.12
From a clinical perspective, the description that the volume of WMLs can decrease is important for the adequate interpretation of cognitive impairment in cirrhotic patients. This is especially important during the evaluation of candidates for liver transplantation. The presence of vascular risk factors and the finding of large WMLs may cause one to question the reversibility of the neurologic impairment after liver transplantation. According to our findings, in these patients, WMLs should be reassessed after therapy for HE to recognize to what extent the lesions can be reversible after liver transplantation.
In conclusion, we have observed a decrease in the volume and number of WMLs in relation to improvement of HE. These findings suggest that cognitive impairment in HE may be related to interstitial edema and dysfunction of cerebral microvasculature.
Footnotes
This study was supported by Instituto de Salud Carlos III (FIS PI03/0072). B.M. was the recipient of a grant FIS CM04/00044.
References
- 1.Spahr L, Butterworth RF, Fontaine S, et al. Increased blood manganese in cirrhotic patients: relationship to pallidal magnetic resonance signal hyperintensity and neurological symptoms. Hepatology 1996;24:1116–20 [DOI] [PubMed] [Google Scholar]
- 2.Rovira A, Cordoba J, Raguer N, et al. Magnetic resonance imaging measurement of brain edema in patients with liver disease: resolution after transplantation. Curr Opin Neurol 2002;15:731–37 [DOI] [PubMed] [Google Scholar]
- 3.Kale RA, Gupta RK, Saraswat VA, et al. Demonstration of interstitial cerebral edema with diffusion tensor MR imaging in type C hepatic encephalopathy. Hepatology 2006;43:698–706 [DOI] [PubMed] [Google Scholar]
- 4.Haussinger D, Kircheis G, Fischer R, et al. Hepatic encephalopathy in chronic liver disease: a clinical manifestation of astrocyte swelling and low-grade cerebral edema? J Hepatol 2000;32:1035–38 [DOI] [PubMed] [Google Scholar]
- 5.Sen S, Rose C, Ytrebo LM, et al. Effect of albumin dialysis on intracranial pressure increase in pigs with acute liver failure: a randomized study. Crit Care Med 2006;34:158–64 [DOI] [PubMed] [Google Scholar]
- 6.de Groot JC, de Leeuw FE, Oudkerk M, et al. Cerebral white matter lesions and subjective cognitive dysfunction: the Rotterdam Scan Study. Neurology 2001;56:1539–45 [DOI] [PubMed] [Google Scholar]
- 7.Dufouil C, Chalmers J, Coskun O, et al. Effects of blood pressure lowering on cerebral white matter hyperintensities in patients with stroke: the PROGRESS (Perindopril Protection Against Recurrent Stroke Study) Magnetic Resonance Imaging Substudy. Circulation 2005;112:1644–50 [DOI] [PubMed] [Google Scholar]
- 8.Pantoni L, Garcia JH. Pathogenesis of leukoaraiosis: a review. Stroke 1997;28:652–59 [DOI] [PubMed] [Google Scholar]
- 9.Plummer D. DispImage: a display and analysis tool for medical images. Rev Neuroradiol 1992;5:489–95 [Google Scholar]
- 10.Matsusue E, Kinoshita T, Ohama E, et al. Cerebral cortical and white matter lesions in chronic hepatic encephalopathy: MR-pathologic correlations. AJNR Am J Neuroradiol 2005;26:347–51 [PMC free article] [PubMed] [Google Scholar]
- 11.Cordoba J, Alonso J, Rovira A, et al. The development of low-grade cerebral edema in cirrhosis is supported by the evolution of 1H-magnetic resonance abnormalities after liver transplantation. J Hepatol 2001;35:598–604 [DOI] [PubMed] [Google Scholar]
- 12.Nguyen JH, Yamamoto S, Steers J, et al. Matrix metalloproteinase-9 contributes to brain extravasation and edema in fulminant hepatic failure mice. J Hepatol 2006;44:1105–14 [DOI] [PMC free article] [PubMed] [Google Scholar]