Abstract
The current WHO histopathologic criteria for oral epithelial dysplasia (ED) are based on architectural and cytologic alterations, and do not address other histopathologic features of ED. Here we propose new diagnostic criteria including architectural, organizational, and cytologic features for oral ED. Cases of unifocal leukoplakia (UL) and proliferative leukoplakia (PL) with clinical photographs and follow-up information were identified. Only cases that showed minimal cytologic atypia or mild ED were used to demonstrate critical architectural changes as defined in this study. Eight biopsies from eight UL patients and 34 biopsies from four PL patients were included. The biopsies showed (a) corrugated, verrucous or papillary architecture, (b) hyperkeratosis with epithelial atrophy, (c) bulky squamous epithelial proliferation, and (d) demarcated hyperkeratosis and “skip” segments. The architectural alterations defined here are as important as the currently used criteria for the diagnosis of ED. Clinicopathologic correlation when diagnosing oral ED is also of the utmost importance in accurate diagnosis.
Keywords: Oral epithelial dysplasia, Malignant transformation, Architectural alteration, Leukoplakia, Proliferative verrucous leukoplakia
Introduction
Oral leukoplakia is a precancerous condition [1]. It was defined in 2005 as “a white plaque of questionable risk having excluded (other) known diseases or disorders that carry no increased risk for cancer,” and this definition still stands today [1, 2]. As such, a true leukoplakia is a clinical term only after having ruled out other specific diagnoses. Histopathologically, leukoplakia exhibits hyperkeratosis or parakeratosis, epithelial atrophy or hyperplasia, epithelial dysplasia (ED), carcinoma-in-situ or invasive squamous cell carcinoma (SCC) [2, 3]. Leukoplakia progresses to malignancy in 0.1–36.4% of cases and the time to malignant transformation varies depending on the study, the severity of ED, and the length of follow-up [4–8]. Leukoplakias that exhibited ED at the time of biopsy showed malignant transformation in 6.6–36.4% of the cases, while lesions without ED at the time of biopsy showed malignant transformation rate of 0.1–14.0% [9–13].
Histopathologic signs of ED are currently divided into architectural and cytologic features [2]. Leions are divided into low, moderate, and severe ED depending on whether < 1/3, > 1/3 but < 2/3, or > 2/3 of the epithelium (but not full thickness) is affected by dysplastic cells, respectively (Table 1) [14]. In keeping with the assessment of ED at other sites, a binary system of low- and high-grade ED has been proposed [15]. However, other aspects of architectural changes, such as corrugated, verrucous or papillary morphology, are not part of the current criteria for diagnosing and grading ED [2, 14]. Verrucous hyperplasia (clinically verrucous leukoplakia) is characterized by verrucous or papillary epithelial hyperplasia with an exophytic growth pattern where cytologic features of dysplasia are variable and may be minimal to absent [14, 16, 17]. Malignant transformation occurs in up to 10% of cases in verrucous hyperplasia [18]. However, some of such verrucous hyperplasia called “mass-type,” likely already represents verrucous carcinoma or papillary SCC [18]. In addition, proliferative verrucous leukoplakia, a form of proliferative leukoplakia (PL, a more accurate term since many but not all lesions are verrucous) is an uncommon form of oral leukoplakia that often shows verrucous hyperplasia with minimal to no ED in biopsies performed in the early stage of the disease [19–21]. PL is characterized by the multifocal geographic expansion of white plaques, sometimes verrucous, and development of SCC in 70–100% of cases with long-term follow-up [20–23]. Most patients undergo multiple biopsies over years and decades. These show hyperkeratosis and often verrucous hyperplasia or epithelial atrophy without evidence of ED in the beginning, and subsequently varying degrees of ED and finally invasive SCC [20, 23–25].
Table 1.
Histopathologic features of oral epithelial dysplasia
| Proposed criteria | WHO criteria | |
|---|---|---|
| Architectural features |
Corrugated/verrucous/papillary morphology Hyperkeratosis and epithelial atrophy Bulky squamous proliferation, exophytic/endophytic growth Skip segments and demarcated hyperkeratosis Drop-shaped rete ridges |
Irregular epithelial stratification Loss of polarity of basal cells Drop-shaped rete ridges Increased number of mitotic figures Abnormally superficial mitotic figures Premature keratinization of single cells Keratin pearls within rete ridges Loss of epithelial cell cohesion |
| Organizational features |
Loss of upward maturation in the epithelium Dyscohesion Premature keratinization/dyskeratosis Keratin pearls within rete ridges Suprabasal mitotic figures |
|
| Cytologic features |
Cellular/nuclear pleomorphism Basal cell hyperplasia Increased nuclear:cytoplasmic ratio Atypical mitotic figures Enlarged and multiple nucleoli Hyperchromasia and coarse chromatin Dyskeratosis and/or glassy cytoplasm |
Abnormal variation in nuclear size Abnormal variation in nuclear shape Abnormal variation in cell size Abnormal variation in cell shape Increased nuclear:cytoplasmic ratio Atypical mitotic figures Increased number and size of nucleoli Hyperchromasia |
This histopathologic progression of PL is particularly useful in understanding oral ED because of the high rate of malignant transformation despite early lesions showing no microscopic evidence of dysplasia. Such hyperkeratotic lesions without obvious ED have been referred to as keratosis of uncertain significance to emphasize that these lesions may look innocuous histopathologically, but when evaluated in the context of the clinical presentation, raise suspicions for early ED [3]. Furthermore, verrucous carcinoma which is characterized by an endophytic squamous epithelial proliferation with a blunt and pushing pattern of invasion on a broad front rather than the conventional invasion pattern of single cells or tumor islands, exhibits minimal-to-mild cytologic atypia and the diagnosis is rendered primarily on the bulky verruciform or papillary morphology and its endophytic growth pattern [14, 17, 26–29]. Verrucous hyperplasia illustrates the significance of architectural changes in determining the fate of lesions.
The objective of this study is to demonstrate architectural alterations of oral ED, defined here as gross morphologic changes noted on low microscopic magnification with respect to four criteria illustrated through a series of cases of unifocal leukoplakia (UL) and PL (defined here as multifocal non-contiguous leukoplakias).
Materials and Methods
Cases were selected from the patient archives of the Division of Oral Medicine and Dentistry and Department of Pathology at the Brigham and Women’s Hospital (BWH), Boston, MA, and StrataDx Inc., Lexington, MA. This study was approved by the Institutional Review Board of BWH. We included only cases of UL and PL with clinical photographs and follow-up information. The current features described as architectural by WHO are given the term organizational to reflect how keratinocytes relate to each other and to where they normally reside within the spinous layer [14]. Cytologic features mostly remain unchanged and are features that are best seen at high magnification and always seen on exfoliative cytology (Table 1).
Only cases that showed minimal cytologic atypia or mild ED with the following architectural alterations were included in the study.
Corrugated, verrucous or papillary architecture.
Hyperkeratosis and/or parakeratosis with epithelial atrophy and minimal/no interface inflammation, bearing in mind that different intra-oral sites have different baseline thickness of the epithelium. For example, epithelial atrophy for the buccal mucosa may be the normal thickness of epithelium for the ventral tongue, floor of mouth, and soft palate.
Bulky squamous epithelial proliferation with an exophytic and/or endophytic growth pattern (the former often associated with corrugated/verrucous/papillary architecture). Downward epithelial proliferation for at least three times the normal thickness of the epithelium was considered bulky endophytic proliferation. Spongiosis and leukocyte exocytosis should be minimal.
Demarcated hyperkeratosis and “skip” segments where the hyperkeratosis was sharply demarcated and there was multifocal hyperkeratosis with intervening non-keratinized or normally keratinized epithelium.
These features were correlated with clinical findings and follow-up information was available on cases of PL where progression was defined as development of invasive SCC.
Results
Eight biopsies from eight patients with UL (Figs. 1, 2, 3, 4, 5, 6, 7, 8) and 34 biopsies from four patients with PL (Figs. 9, 10, 11, 12) were included in the current study. Demographic and follow-up information of the cases is provided in Tables 2 and 3. In the UL group, four cases were non-homogenous leukoplakia (verrucous and speckled) and four were homogenous leukoplakia (fissured and non-fissured).
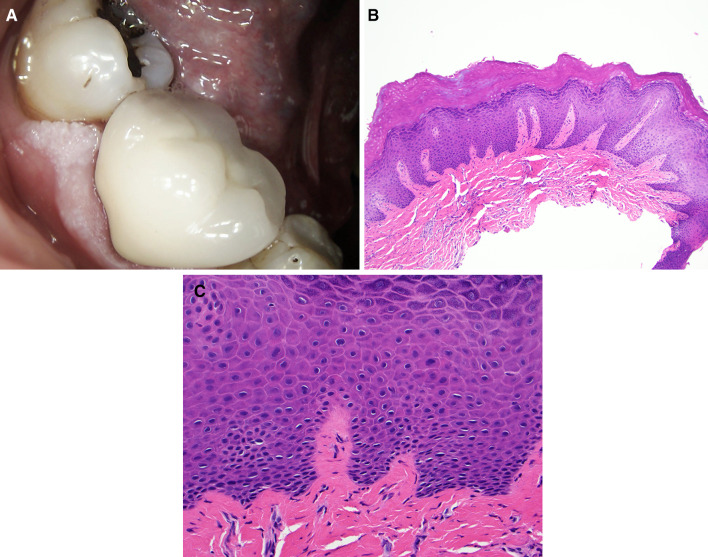
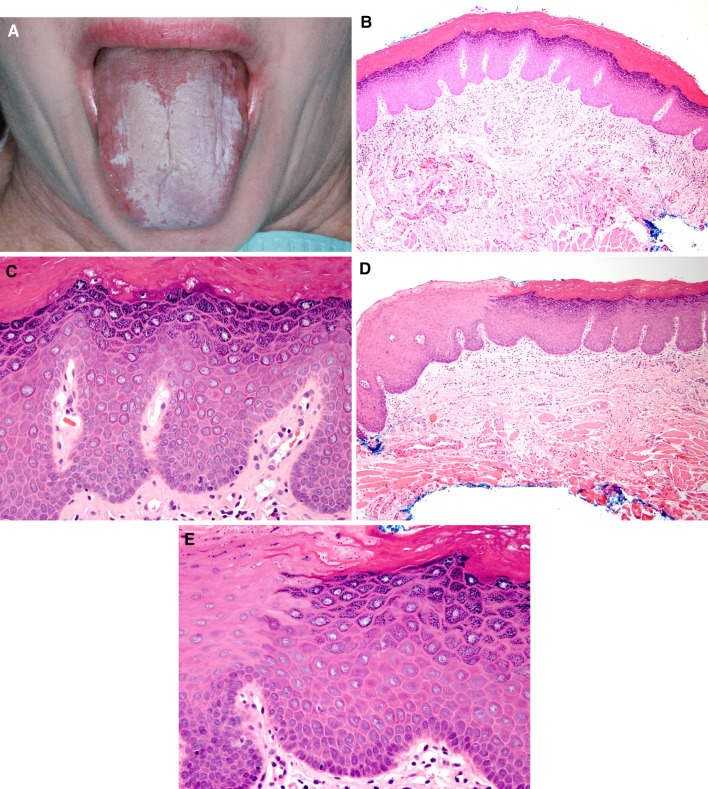
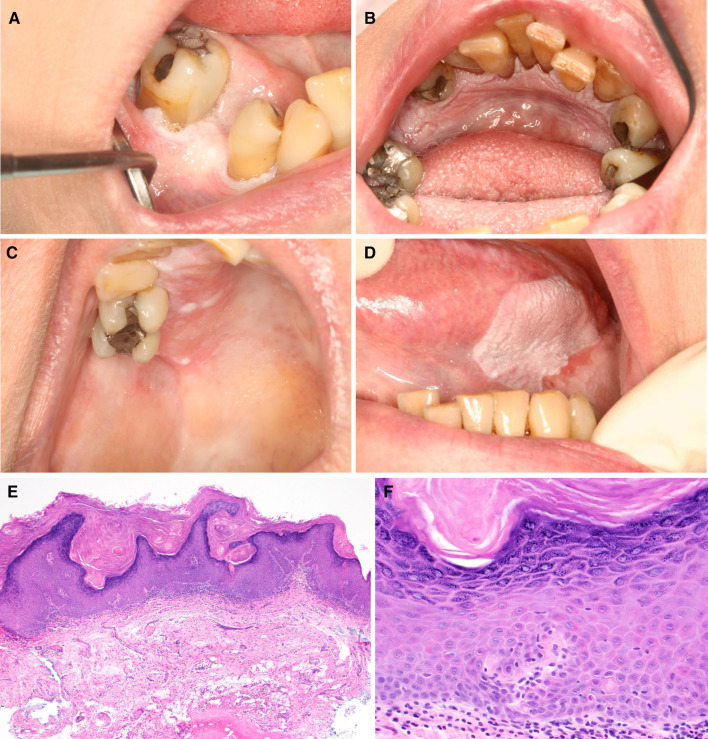
Fig. 1.
Case 1 a Unifocal non-homogenous leukoplakia on the mandibular gingiva exhibiting corrugated surface. b Corrugated hyperkeratosis, hypergranulosis and epithelial hyperplasia (H&E, original magnification ×40). c No ED present (H&E, original magnification ×400)
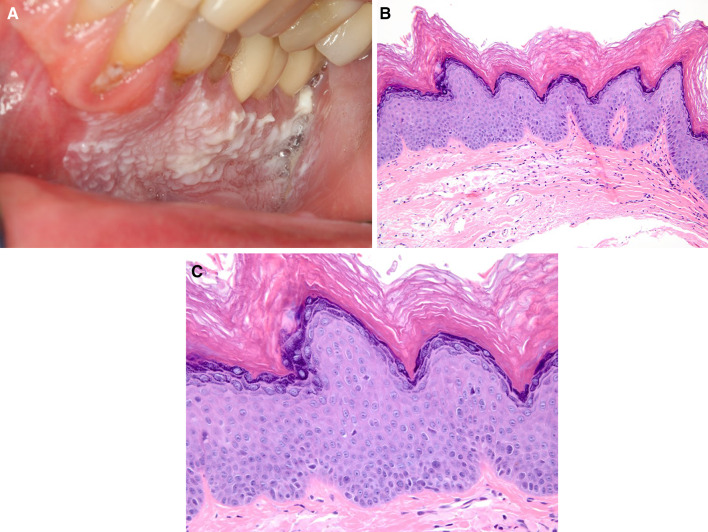
Fig. 2.
Case 2 a Unifocal non-homogenous leukoplakia on the mandibular gingiva exhibiting corrugated surface. b Atypical verrucous hyperkeratosis and epithelial atrophy (H&E, original magnification ×100). c Minimal cytologic atypia present (H&E, original magnification ×400)
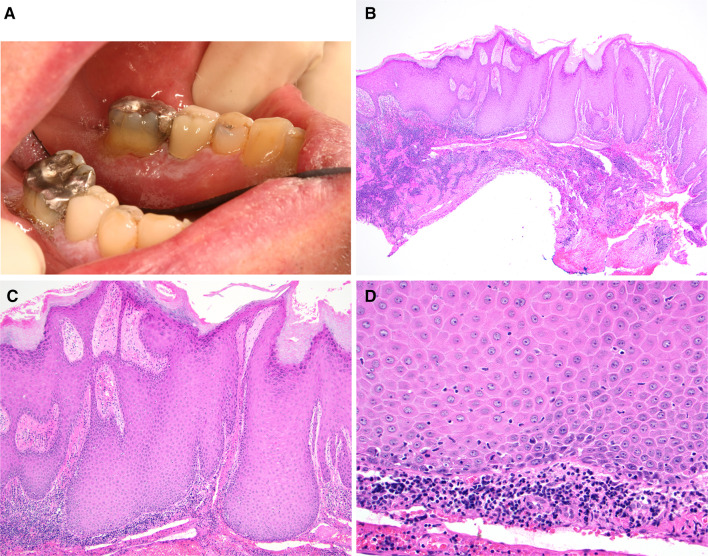
Fig. 3.
Case 3 a Unifocal non-homogenous leukoplakia on the mandibular gingiva with a focally corrugated surface. b There is bulky, verrucous proliferation slightly exo- and endo-phytic forming bulbous rete ridges (H&E, original magnification ×40). c Bulbous rete ridges (H&E, original magnification ×200). d Minimal cytologic atypia and minimal chronic inflammatory infiltrate present (H&E, original magnification ×400)
Fig. 4.
Case 4 a Unifocal homogenous leukoplakia on the hard palatal mucosa. b Hyperkeratosis with hypergranulosis and epithelial atrophy (H&E, original magnification ×40). c No ED present (H&E, original magnification ×400). d Focal surface corrugation is identified (H&E, original magnification ×400)
Fig. 5.
Case 5 a Unifocal fissured homogenous leukoplakia on the dorsal tongue. b Demarcated and corrugated hyperkeratosis with hypergranulosis, and epithelial atrophy (loss of papillae) (H&E, original magnification ×100). c Minimal cytologic atypia present (H&E, original magnification ×400). d Demarcated hyperkeratosis is noted (H&E, original magnification ×100). e Minimal ED with mild chronic inflammation present (H&E, original magnification ×400)
Fig. 6.
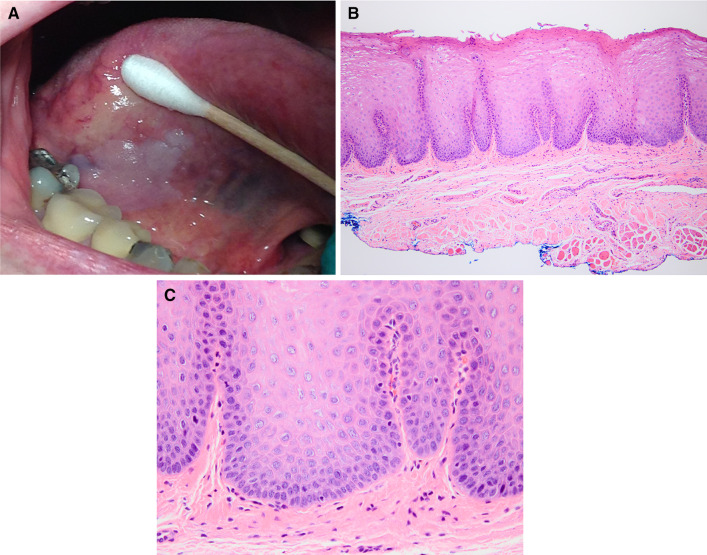
Case 6 a Unifocal homogenous leukoplakia on the ventral tongue. b There is bulky squamous epithelial proliferation (H&E, original magnification ×100). c Minimal ED present (H&E, original magnification ×400)
Fig. 7.
Case 7 a Unifocal homogenous leukoplakia on the left ventral tongue. b There is bulky, exophytic squamous epithelial proliferation (H&E, original magnification ×100). c No ED present (H&E, original magnification ×400)
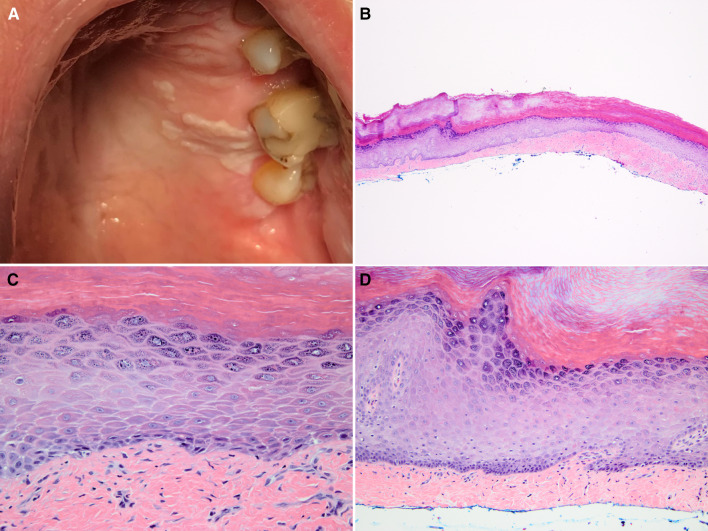
Fig. 8.
Case 8 a Unifocal non-homogenous leukoplakia on the right ventral tongue. b Demarcated hyperkeratosis with “skip” segments (H&E, original magnification ×100). c Mild ED and a mild chronic inflammatory infiltrate is identified (H&E, original magnification ×400)
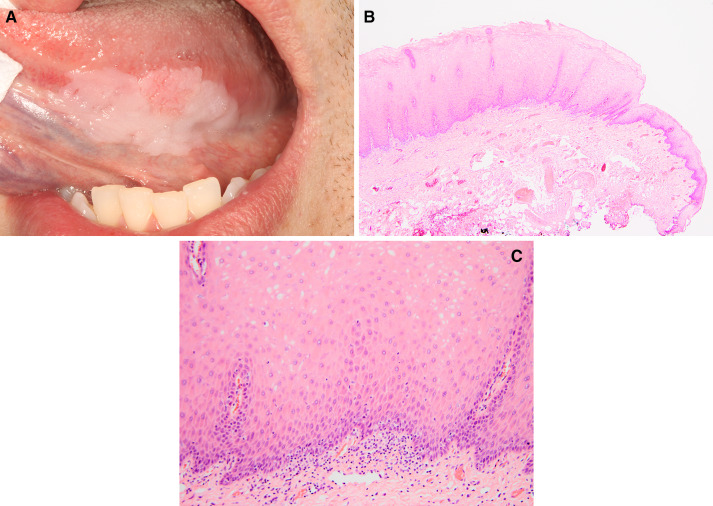
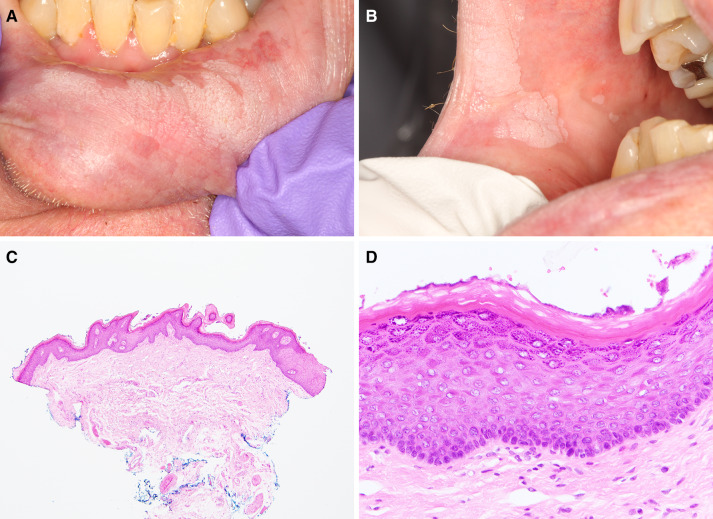
Fig. 9.
Case 9 Proliferative leukoplakia on a, b the mandibular gingiva, c the hard-palatal mucosa, and d the latero-ventral tongue. e Biopsy of tongue lesion exhibits atypical verrucous hyperplasia (H&E, original magnification ×40). f Minimal cytologic atypia and minimal inflammatory infiltrate present (H&E, original magnification × 400)
Fig. 10.
Case 10 Proliferative leukoplakia on a the lower lip mucosa and b the buccal mucosa. c There is atypical verrucous hyperkeratosis and epithelial atrophy (H&E, original magnification ×40). d ED is not identified (H&E, original magnification ×400)
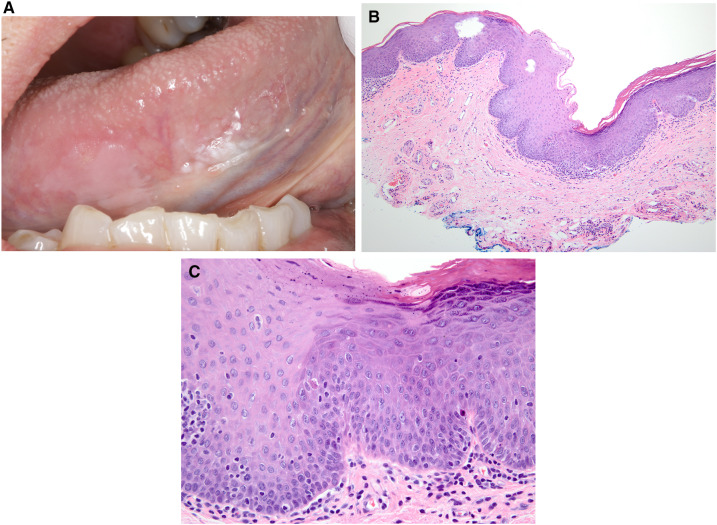
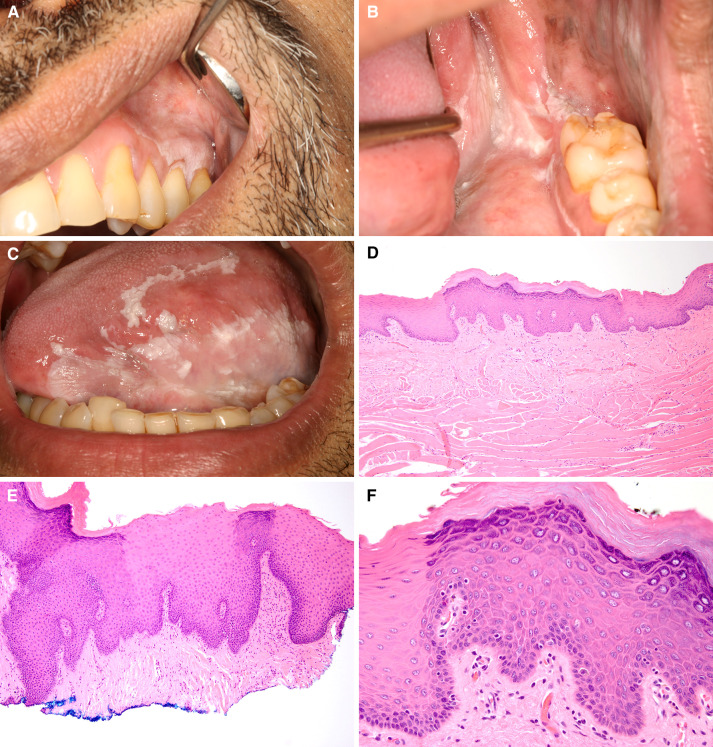
Fig. 11.
Case 11 Proliferative leukoplakia on a the gingiva, b retromolar trigone extending to the anterior tonsillar pillar, and c the latero-ventral and dorsal tongue. d Biopsy from the tongue exhibits demarcated hyperkeratosis (H&E, original magnification ×100). e A later biopsy from the tongue exhibits demarcated corrugated hyperkeratosis and acanthosis with skip segments (H&E, original magnification ×100). f Mild ED is focally present (H&E, original magnification ×400)
Fig. 12.
Case 12 a Proliferative leukoplakia on the buccal mucosa extending to the commissure area with a second lesion further posteriorly. b There is bulky squamous epithelial proliferation (H&E, original magnification ×20). c No ED present (H&E, original magnification ×400)
Table 2.
Clinical information of the cases
| Age | Gender | Number of lesions (homogenous or non-homogenous) | Lesions’ location | |
|---|---|---|---|---|
| Unifocal leukoplakia (UL) | 74 | M | 1 | G |
| 56 | M | 1 | G | |
| 75 | M | 1 | G | |
| 70 | M | 1 | HP | |
| 58 | F | 1 | DT | |
| 73 | F | 1 | VT | |
| 78 | M | 1 | VT | |
| 60 | M | 1 | VT | |
| Proliferative leukoplakia (PL) | 55 | F | 6 (4,2) | G, VT, LT, HP, BM and LM |
| 53 | M | 6 (4,2) | G, VT, FOM, SP, HP and BM | |
| 36 | M | 9 (8,1) | DT, BM and LM | |
| 88 | F | 3 (0,3) | G, TP and BM |
G gingiva, DT dorsal tongue, LT lateral border of tongue, VT ventral tongue, FOM floor of mouth, TP tonsillar pillar, BM buccal mucosa, LM labial mucosa, SP soft palate, HP hard palatal mucosa
Table 3.
Follow-up information of the PL cases
| Follow up (years) | Clinical outcome | |
|---|---|---|
| Case 9 | 11 | 3 SCCs, DoD |
| Case 10 | 8 | No disease progressiona |
| Case 11 | 14 | 3 SCCs, alive with disease undergoing palliative immunotherapy |
| Case 12 | 5 | 1 SCC, DoD |
SCC squamous cell carcinoma, DoD dead of disease
aLast follow-up 2.5 years ago
Corrugated, Verrucous or Papillary Architecture
In the UL group, Cases 1–3 exhibited a corrugated/verrucous/papillary configuration with minimal ED which corresponded to clinical lesions of verrucous leukoplakias while Case 4 exhibited focal corrugations and was clinically a homogenous leukoplakia (Figs. 1a–c, 2a–c, 3a–d, 4a–d). In the PL group, Cases 9 and 10 exhibited papillomatosis and corrugated architecture (Figs. 9a–f, 10a–d). In the PL group, 23/34 (67.6%) of lesions showed a corrugated/verrucous/papillary configuration.
Hyperkeratosis with Epithelial Atrophy and Minimal/No Interfacial Inflammation
In the UL group, Cases 2, 4, and 5 presented with hyperkeratosis, epithelial atrophy, and mild chronic inflammation, without significant ED (Figs. 2a–c, 4a–c, 5a–c). Clinically, Case 2 was a verrucous leukoplakia, Case 4 was a non-fissured homogenous leukoplakia, and Case 5 was a fissured mostly homogenous leukoplakia. In the PL group, there were 15/34 (44.1%) specimens with hyperkeratosis, epithelial atrophy, and mild chronic inflammation; 12 of those were hyperkeratotic, and three were parakeratotic (Fig. 10a–d).
Bulky Squamous Epithelial Proliferation
In the UL group, Cases 3, 6, and 7 showed a bulky endophytic growth pattern with minimal ED (Figs. 3a–d, 6a–c, 7a–c). Case 3 was clinically a verrucous leukoplakia and Cases 6 and 7 were homogenous leukoplakias. In the PL group, 9/34 (26.5%) of specimens showed a bulky squamous proliferation (Fig. 12a–c) and 7/34 (20.6%) of specimens showed an exophytic growth pattern. Some specimens had both endophytic and exophytic components.
Demarcated Hyperkeratosis and “Skip” Segments
In the UL group, all the cases clinically showed a sharp demarcation (partially in some cases) of the hyperkeratotic area from the normal mucosa. Histopathologically, there is demarcated hyperkeratosis in Case 5 (Fig. 5d, e) and “skip” segments in Case 8 (Fig. 8a–c). In the PL group, lesions were at least partially demarcated in all cases, and 6/34 (17.6%) lesions exhibited skip segments or sharp demarcation (Figs. 10c, 11a–f).
Discussion
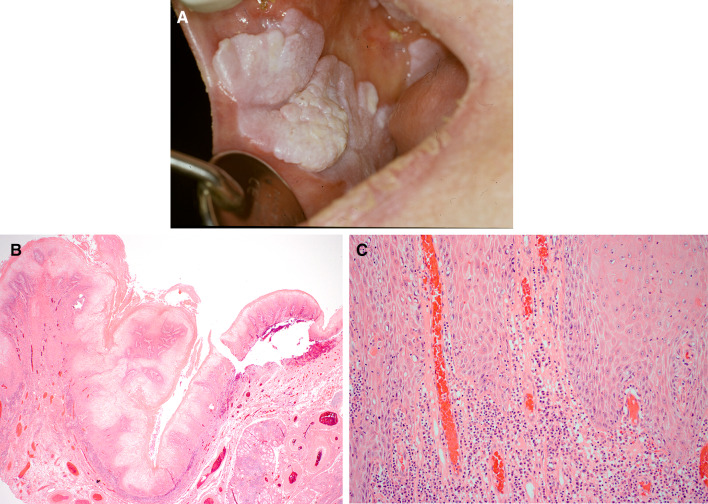
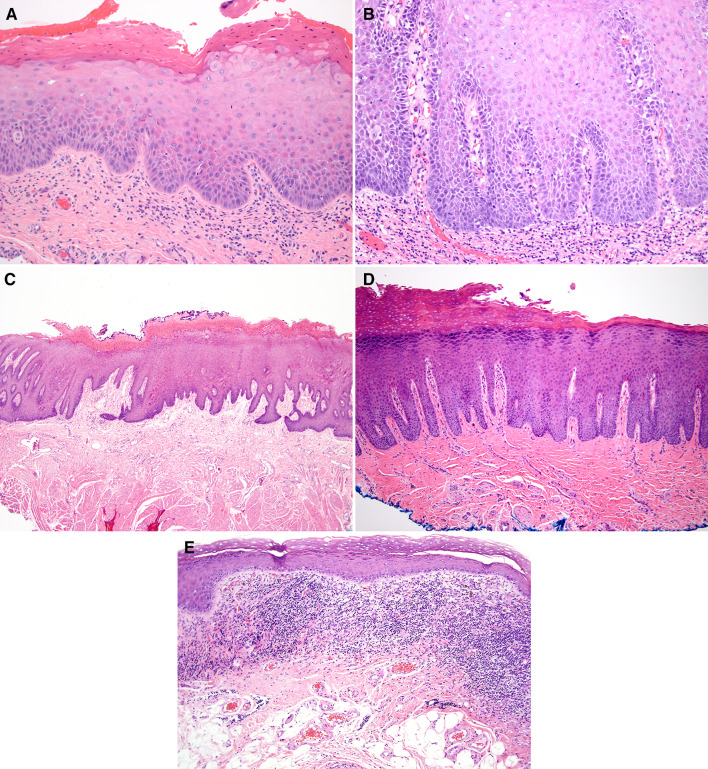
The diagnosis of mild ED has always been challenging with large inter-examiner variability [30–33]. Unlike mild ED, moderate and severe ED usually demonstrate higher inter-examiner agreement (Fig. 13a, b). Trauma, candidiasis, and inflammation may cause reactive epithelial atypia that shares many features with ED. As such, no single feature is diagnostic for ED but rather a constellation of features, correlated with the degree of inflammation and the clinical appearance of the lesion [34]. The importance of clinical correlation cannot be overstated, and this is particularly well-illustrated in the condition of PL. The recognition of this entity in 1985 was a result of realizing that the innocuous histopathology did not correlate with the clinical appearance of large, often multifocal lesions that progressed over years and decades from hyperkeratosis with epithelial atrophy, to dysplasia or/and invasive SCC in 70–100% of cases [19, 25, 35, 36]. Support for this finding can be found in previous studies that showed lesions greater than 200 mm2 correlated with poorer prognosis even if there was no ED on biopsy [37]. In this regard, the histopathologic features of early stage of PL inform the features of very early ED. PL and UL share similar histopathologic features, whether architectural, organizational, or cytologic [34].
Fig. 13.
a Moderate ED characterized by drop-shaped rete ridges, cells with increased nuclear:cytoplasmic ratio and dyskeratosis involving approximately half the thickness of the epithelium (H&E, original magnification ×200). b Severe ED characterized by bulbous rete ridges, dyscohesion, cells with increased nuclear:cytoplasmic ratio, dyskeratosis and slight nuclear pleomorphism and hyperchromasia involving greater than 2/3 the thickness of the epithelium (H&E, original magnification ×200). c Chronic bite/factitial keratosis (morsicatio mucosae oris) with parakeratosis and acanthosis (H&E, original magnification ×100). d Benign alveolar ridge keratosis with hyperkeratosis, wedge-shaped hypergranulosis and acanthosis (H&E, original magnification ×100). e Lichen planus exhibiting hyperkeratosis, epithelial atrophy, and interface inflammation (H&E, original magnification ×100)
We believe that the assessment of oral ED should be based on three categories of findings, namely architectural (readily seen at low power), organizational (readily seen at intermediate to high power) and cytologic which are the conventional features best identified on high power microscopy and on exfoliative cytology (Table 1) [2, 31, 32, 34]. The architectural features described by Kujan et al. [15] and in the WHO classification [14] fall primarily into the category of organizational changes within the epithelium as described here. Organizational features show how keratinocytes have lost their normal relationship to each other (e.g. dyscohesion), and to their abnormal position within the epithelium such as location of basal cells and mitoses beyond the usual 1–2 layers of the basal and parabasal cells. We suggest that the term “architectural features” as defined in this study be used for features that are clearly discernible with low power microscopy and refer to gross microscopic morphology. These include the well-recognized corrugated/verrucous/papillary architecture, hyperkeratosis with epithelial atrophy, bulky and usually endophytic squamous proliferation, sharply demarcated keratinization and “skip” segments, as well as bulbous and drop-shaped rete ridges, this last feature being already well-established. These architectural features are seen in both PL and UL lesions, often with ED and as such, should be considered worrisome even in the absence of cytologic dysplasia in the leukoplakic lesions.
Corrugated/verrucous/papillary architecture was noted in 67.6% of biopsies of PL, and this often occurred without, or with minimal evidence of cytologic dysplasia. Historically, non-homogenous leukoplakias with a verrucous/nodular appearance progress to SCC in 33 per 1000 cases every year with an overall transformation rate 50–60% [14, 38, 39]. This architecture is a common predictor of malignant transformation especially to verrucous carcinoma and must be included in any system for grading ED [14, 17, 40].
In the original and seminal article on PL by Hansen, many PL cases showed hyperkeratosis with epithelial atrophy [25]. In our PL cohort, 15/34 cases (44.1%) showed hyperkeratosis and epithelial atrophy. Most classifications focus on epithelial hyperplasia as precursors to ED [41, 42]. However, such hyperplasia or acanthosis is seen frequently in response to local irritation and injury (e.g., morsicatio mucosae oris and benign alveolar ridge keratosis) (Fig. 13c, d) [43–45]. It would be highly unusual to see epithelial atrophy in reaction to local irritation. In addition, the clinical appearance of a demarcated plaque also speaks against local injury and suggests clonal proliferation. Lichen planus may show hyperkeratosis and epithelial atrophy or erosion but these findings are always associated with degeneration of the basal cells, colloid bodies and a lymphohistiocytic infiltrate at the interface, as well as other reactive changes within the epithelium due to inflammation (Fig. 13e). Furthermore, hyperkeratotic lesions with epithelial atrophy and a lymphocytic band at the interface in the clinical setting of a demarcated plaque should be viewed with caution because such a “lichenoid” pattern has been noted in 29% of ED [46]. It is likely that such infiltrates represent a lymphocytic host response to ED or tumor-promoting inflammation, a hallmark of cancer as noted by Hanahan and Weinberg [47]. Such lymphocytes, well recognized in invasive carcinoma, are the basis for the immunotherapy in head and neck cancer [48].
Studies have shown that “hyperkeratosis without dysplasia” may progress to dysplasia and carcinoma from 0.1 to 14.0% of cases [9–13]. It is unclear whether such reports relied exclusively on the use of cytologic criteria, resulting in an under-diagnosis of dysplasia. A recent study showed that such lesions harbored the same mutations as lesions with moderate and severe ED used as controls [49]. As such, we suggest that the term “hyperkeratosis, not reactive” should be applied in the absence of ED and where the histopathologic features are unlikely to be a result of inflammation rather than “hyperkeratosis, no dysplasia” which may lead to patients being discharged from follow-up.
On the other hand, bulky squamous epithelial proliferation that expands the epithelial thickness at least three-fold is concerning for developing ED. In this series, this feature was noted in 16/34 (47.1%) of PL cases. These often exhibit an endophytic growth pattern and the term “atypical endophytic squamous proliferation” is often used. Bulky squamous proliferation borders on neoplasia in many cases, and verrucous carcinoma is a prime example of such a pattern of squamous proliferation and yet, is still a carcinoma with a “blunt” pattern of invasion [50]. Corresponding to the at least partially demarcated clinical lesions of both UL and PL, biopsies taken from the margin of such lesions will show demarcated hyperkeratosis, and “skip” segments in 20.6% of PL cases.
These architectural features may occur alone or in combination; for example, it is common to see verrucous/papillary hyperplasia exhibiting bulky endophytic growth pattern, and hyperkeratosis with atrophy exhibiting “skip” segments. We have consolidated some of the WHO criteria here. Irregular epithelial stratification and loss of polarity of basal cells is recognizable at medium power and is characterized by loss of upward maturation, an organizational criterion. The four cytologic criteria of variation of nuclear and cell shape and size are consolidated into a single feature of pleomorphism for simplicity. The presence of atypical mitotic figures is more appropriately categorized as a cytologic feature while the location of normal-appearing mitotic figures beyond the basal and parabasal cells is an organizational feature of ED (Table 1).
Currently, the WHO grades oral ED into mild, moderate and severe depending on the thickness of epithelium [31], while grading of “squamous intra-epithelial neoplasia (SIN)” for laryngeal lesions designates lesions as SIN I (low grade) and SIN II (high grade) in increasing order of severity of dysplasia [51]. A binary system of grading oral ED into “high risk” and “low risk” has been proposed as is used for other mucosal sites and we believe that architectural features of ED as defined here must be included in any grading system for accuracy [15]. Larger scale studies with long term follow up information are needed to fully investigate the correlation between the architectural alterations, clinical outcome, and importantly, the molecular signature of oral ED. Finally, it cannot be overstated that clinical information is of the utmost importance in arriving at an accurate diagnosis namely size, multifocality and the appearance of lesions.
Conclusion
Oral ED is a precursor lesion of oral SCC. Here we propose that ED be diagnosed based on not only the well-recognized organizational and cytologic criteria but also on architectural features. Eight UL and four PL cases were presented to illustrate architectural features of ED that may occur with minimal evidence of cytologic atypia/dysplasia. These include corrugated, verrucous or papillary architecture, hyperkeratosis or parakeratosis with epithelial atrophy, bulky squamous epithelial proliferation with exophytic and/or endophytic growth pattern, and sharply demarcated hyperkeratosis and/or skip lesions. These features are commonly seen in lesions of PL in early stages and precede development of other features of ED and SCC which occur in the majority of patients over time.
Funding
No funding obtained.
Compliance with Ethical Standards
Conflict of interest
No conflict of interest to disclose.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. J Oral Pathol Med. 2007;36(10):575–580. doi: 10.1111/j.1600-0714.2007.00582.x. [DOI] [PubMed] [Google Scholar]
- 2.Reibel J, Gale N, Hille J, et al. Oral potentially malignant disorders and oral epithelial dysplasia. WHO Classif Head Neck Tumours. 2017;9:112. [Google Scholar]
- 3.Woo SB, Grammer RL, Lerman MA. Keratosis of unknown significance and leukoplakia: a preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(6):713–724. doi: 10.1016/j.oooo.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 4.Napier SS, Speight PM. Natural history of potentially malignant oral lesions and conditions: an overview of the literature. J Oral Pathol Med. 2008;37(1):1–10. doi: 10.1111/j.1600-0714.2007.00579.x. [DOI] [PubMed] [Google Scholar]
- 5.Kumar A, Cascarini L, McCaul JA, et al. How should we manage oral leukoplakia? Br J Oral Maxillofacial Surg. 2013;51(5):377–383. doi: 10.1016/j.bjoms.2012.10.018. [DOI] [PubMed] [Google Scholar]
- 6.Silverman S, Jr, Gorsky M, Lozada F. Oral leukoplakia and malignant transformation. A follow-up study of 257 patients. Cancer. 1984;53(3):563–568. doi: 10.1002/1097-0142(19840201)53:3<563::aid-cncr2820530332>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 7.Arduino PG, Bagan J, El-Naggar AK, Carrozzo M. Urban legends series: oral leukoplakia. Oral Dis. 2013;19(7):642–659. doi: 10.1111/odi.12065. [DOI] [PubMed] [Google Scholar]
- 8.Liu W, Shi LJ, Wu L, et al. Oral cancer development in patients with leukoplakia–clinicopathological factors affecting outcome. PLoS ONE. 2012;7(4):e34773. doi: 10.1371/journal.pone.0034773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schepman KP, van der Meij EH, Smeele LE, van der Waal I. Malignant transformation of oral leukoplakia: a follow-up study of a hospital-based population of 166 patients with oral leukoplakia from The Netherlands. Oral Oncol. 1998;34(4):270–275. [PubMed] [Google Scholar]
- 10.Rosin MP, Cheng X, Poh C, et al. Use of allelic loss to predict malignant risk for low-grade oral epithelial dysplasia. Clin Cancer Res. 2000;6(2):357–362. [PubMed] [Google Scholar]
- 11.Brouns E, Baart J, Karagozoglu K, Aartman I, Bloemena E, van der Waal I. Malignant transformation of oral leukoplakia in a well-defined cohort of 144 patients. Oral Dis. 2014;20(3):e19–24. doi: 10.1111/odi.12095. [DOI] [PubMed] [Google Scholar]
- 12.Wang YY, Tail YH, Wang WC, et al. Malignant transformation in 5071 southern Taiwanese patients with potentially malignant oral mucosal disorders. BMC Oral Health. 2014;14:99. doi: 10.1186/1472-6831-14-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaturvedi AK, Udaltsova N, Engels EA, et al. Oral leukoplakia and risk of progression to oral cancer: a population-based cohort study. J Natl Cancer Inst. 2019. [DOI] [PMC free article] [PubMed]
- 14.Muller S. Oral epithelial dysplasia, atypical verrucous lesions and oral potentially malignant disorders: focus on histopathology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(6):591–602. doi: 10.1016/j.oooo.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 15.Kujan O, Oliver RJ, Khattab A, Roberts SA, Thakker N, Sloan P. Evaluation of a new binary system of grading oral epithelial dysplasia for prediction of malignant transformation. Oral Oncol. 2006;42(10):987–993. doi: 10.1016/j.oraloncology.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 16.van der Waal I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 2009;45(4–5):317–323. doi: 10.1016/j.oraloncology.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 17.Zhu LK, Ding YW, Liu W, Zhou YM, Shi LJ, Zhou ZT. A clinicopathological study on verrucous hyperplasia and verrucous carcinoma of the oral mucosa. J Oral Pathol Med. 2012;41(2):131–135. doi: 10.1111/j.1600-0714.2011.01078.x. [DOI] [PubMed] [Google Scholar]
- 18.Wang YP, Chen HM, Kuo RC, et al. Oral verrucous hyperplasia: histologic classification, prognosis, and clinical implications. J Oral Pathol Med. 2009;38(8):651–656. doi: 10.1111/j.1600-0714.2009.00790.x. [DOI] [PubMed] [Google Scholar]
- 19.Bagan JV, Jimenez-Soriano Y, Diaz-Fernandez JM, et al. Malignant transformation of proliferative verrucous leukoplakia to oral squamous cell carcinoma: a series of 55 cases. Oral Oncol. 2011;47(8):732–735. doi: 10.1016/j.oraloncology.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 20.Cerero-Lapiedra R, Balade-Martinez D, Moreno-Lopez LA, Esparza-Gomez G, Bagan JV. Proliferative verrucous leukoplakia: a proposal for diagnostic criteria. Med Oral Patol Oral Cir Bucal. 2010;15(6):e839–845. [PubMed] [Google Scholar]
- 21.Villa A, Menon RS, Kerr AR, et al. Proliferative leukoplakia: Proposed new clinical diagnostic criteria. Oral Dis. 2018;24(5):749–760. doi: 10.1111/odi.12830. [DOI] [PubMed] [Google Scholar]
- 22.Gillenwater AM, Vigneswaran N, Fatani H, Saintigny P, El-Naggar AK. Proliferative verrucous leukoplakia: recognition and differentiation from conventional leukoplakia and mimics. Head Neck. 2014;36(11):1662–1668. doi: 10.1002/hed.23505. [DOI] [PubMed] [Google Scholar]
- 23.Ghazali N, Bakri MM, Zain RB. Aggressive, multifocal oral verrucous leukoplakia: proliferative verrucous leukoplakia or not? J Oral Pathol Med. 2003;32(7):383–392. doi: 10.1034/j.1600-0714.2003.00180.x. [DOI] [PubMed] [Google Scholar]
- 24.Gillenwater AM, Vigneswaran N, Fatani H, Saintigny P, El-Naggar AK. Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity! Adv Anat Pathol. 2013;20(6):416–423. doi: 10.1097/PAP.0b013e3182a92df1. [DOI] [PubMed] [Google Scholar]
- 25.Hansen LS, Olson JA, Silverman S., Jr Proliferative verrucous leukoplakia. A long-term study of thirty patients. Oral Surg Oral Med Oral Pathol. 1985;60(3):285–298. doi: 10.1016/0030-4220(85)90313-5. [DOI] [PubMed] [Google Scholar]
- 26.McCoy JM, Waldron CA. Verrucous carcinoma of the oral cavity. A review of forty-nine cases. Oral Surg Oral Med Oral Pathol. 1981;52(6):623–629. doi: 10.1016/0030-4220(81)90081-5. [DOI] [PubMed] [Google Scholar]
- 27.Hazarey VK, Ganvir SM, Bodhade AS. Verrucous hyperplasia: A clinico-pathological study. J Oral Maxillofacial Pathol. 2011;15(2):187–191. doi: 10.4103/0973-029X.84492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walvekar RR, Chaukar DA, Deshpande MS, et al. Verrucous carcinoma of the oral cavity: a clinical and pathological study of 101 cases. Oral Oncol. 2009;45(1):47–51. doi: 10.1016/j.oraloncology.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 29.Ishiyama A, Eversole LR, Ross DA, et al. Papillary squamous neoplasms of the head and neck. Laryngoscope. 1994;104(12):1446–1452. doi: 10.1288/00005537-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 30.Abbey LM, Kaugars GE, Gunsolley JC, et al. Intraexaminer and interexaminer reliability in the diagnosis of oral epithelial dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(2):188–191. doi: 10.1016/s1079-2104(05)80201-x. [DOI] [PubMed] [Google Scholar]
- 31.Warnakulasuriya S, Reibel J, Bouquot J, Dabelsteen E. Oral epithelial dysplasia classification systems: predictive value, utility, weaknesses and scope for improvement. J Oral Pathol Med. 2008;37(3):127–133. doi: 10.1111/j.1600-0714.2007.00584.x. [DOI] [PubMed] [Google Scholar]
- 32.Kujan O, Khattab A, Oliver RJ, Roberts SA, Thakker N, Sloan P. Why oral histopathology suffers inter-observer variability on grading oral epithelial dysplasia: an attempt to understand the sources of variation. Oral Oncol. 2007;43(3):224–231. doi: 10.1016/j.oraloncology.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 33.Upadhyaya JD, Fitzpatrick SG, Cohen DM, et al. Inter-observer variability in the diagnosis of proliferative verrucous leukoplakia: clinical implications for oral and maxillofacial surgeon understanding: a collaborative pilot study. Head Neck Pathol. 2020;14(1):156–165. doi: 10.1007/s12105-019-01035-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Woo SB. Oral epithelial dysplasia and premalignancy. Head Neck Pathol. 2019;13(3):423–439. doi: 10.1007/s12105-019-01020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pentenero M, Meleti M, Vescovi P, Gandolfo S. Oral proliferative verrucous leucoplakia: are there particular features for such an ambiguous entity? A systematic review. Br J Dermatol. 2014;170(5):1039–1047. doi: 10.1111/bjd.12853. [DOI] [PubMed] [Google Scholar]
- 36.Klanrit P, Sperandio M, Brown AL, et al. DNA ploidy in proliferative verrucous leukoplakia. Oral Oncol. 2007;43(3):310–316. doi: 10.1016/j.oraloncology.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 37.van der Waal I, Schepman KP, van der Meij EH. A modified classification and staging system for oral leukoplakia. Oral Oncol. 2000;36(3):264–266. doi: 10.1016/s1368-8375(99)00092-5. [DOI] [PubMed] [Google Scholar]
- 38.Speight PM. Update on oral epithelial dysplasia and progression to cancer. Head Neck Pathol. 2007;1(1):61–66. doi: 10.1007/s12105-007-0014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chuang SL, Wang CP, Chen MK, et al. Malignant transformation to oral cancer by subtype of oral potentially malignant disorder: a prospective cohort study of Taiwanese nationwide oral cancer screening program. Oral Oncol. 2018;87:58–63. doi: 10.1016/j.oraloncology.2018.10.021. [DOI] [PubMed] [Google Scholar]
- 40.Thomson PJ, Goodson ML, Smith DR. Profiling cancer risk in oral potentially malignant disorders—a patient cohort study. J Oral Pathol Med. 2017;46(10):888–895. doi: 10.1111/jop.12625. [DOI] [PubMed] [Google Scholar]
- 41.Gale N, Kambic V, Michaels L, et al. The Ljubljana classification: a practical strategy for the diagnosis of laryngeal precancerous lesions. Adv Anat Pathol. 2000;7(4):240–251. doi: 10.1097/00125480-200007040-00006. [DOI] [PubMed] [Google Scholar]
- 42.Gale N, Michaels L, Luzar B, et al. Current review on squamous intraepithelial lesions of the larynx. Histopathology. 2009;54(6):639–656. doi: 10.1111/j.1365-2559.2008.03111.x. [DOI] [PubMed] [Google Scholar]
- 43.Woo SB, Lin D. Morsicatio mucosae oris—a chronic oral frictional keratosis, not a leukoplakia. J Oral Maxillofac Surg. 2009;67(1):140–146. doi: 10.1016/j.joms.2008.08.040. [DOI] [PubMed] [Google Scholar]
- 44.Natarajan E, Woo SB. Benign alveolar ridge keratosis (oral lichen simplex chronicus): a distinct clinicopathologic entity. J Am Acad Dermatol. 2008;58(1):151–157. doi: 10.1016/j.jaad.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 45.Almazyad A, Li CC, Woo SB. Benign alveolar ridge keratosis: clinical and histopathologic analysis of 167 cases. Head Neck Pathol. 2020. [DOI] [PMC free article] [PubMed]
- 46.Fitzpatrick SG, Honda KS, Sattar A, Hirsch SA. Histologic lichenoid features in oral dysplasia and squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(4):511–520. doi: 10.1016/j.oooo.2013.12.413. [DOI] [PubMed] [Google Scholar]
- 47.Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 48.Hanna GJ, Lizotte P, Cavanaugh M, et al. Frameshift events predict anti-PD-1/L1 response in head and neck cancer. JCI Insight. 2018;3(4):e98811. doi: 10.1172/jci.insight.98811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Villa A, Hanna GJ, Kacew A, Frustino J, Hammerman PS, Woo SB. Oral keratosis of unknown significance shares genomic overlap with oral dysplasia. Oral Dis. 2019;25(7):1707–1714. doi: 10.1111/odi.13155. [DOI] [PubMed] [Google Scholar]
- 50.Wang D, Chen TY, Menon RS, et al. Clinical and histopathologic features of oral bluntly invasive squamous cell carcinoma. Mod Pathol. 2020;33(suppl 2):1308. [Google Scholar]
- 51.Cho KJ, Song JS. Recent changes of classification for squamous intraepithelial lesions of the head and neck. Arch Pathol Lab Med. 2018;142(7):829–832. doi: 10.5858/arpa.2017-0438-RA. [DOI] [PubMed] [Google Scholar]