Abstract
The many diverse terms used to describe the wide spectrum of changes seen in proliferative verrucous leukoplakia (PVL) have resulted in disparate clinical management. The objective of this study was to produce an expert consensus guideline for standardized assessment and reporting by pathologists diagnosing PVL related lesions. 299 biopsies from 84 PVL patients from six institutions were selected from patients who had multifocal oral leukoplakic lesions identified over several years (a minimum follow-up period of 36 months). The lesions demonstrated the spectrum of histologic features described in PVL, and in some cases, patients developed oral cavity squamous cell carcinoma (SCC). An expert working group of oral and maxillofacial and head and neck pathologists reviewed microscopic features in a rigorous fashion, in combination with review of clinical photographs when available. The working group then selected 43 single slide biopsy cases for whole slide digital imaging (WSI) review by members of the consensus conference. The digital images were then reviewed in two surveys separated by a washout period of at least 90 days. Five non-PVL histologic mimics were included as controls. Cases were re-evaluated during a consensus conference with 19 members reporting on the cases. The best inter-observer diagnostic agreement relative to PVL lesions were classified as “corrugated ortho(para)hyperkeratotic lesion, not reactive” and “SCC” (chi-square p = 0.015). There was less than moderate agreement (kappa < 0.60) for lesions in the “Bulky hyperkeratotic epithelial proliferation, not reactive” category. There was ≥ moderate agreement (> 0.41 kappa) for 35 of 48 cases. This expert consensus guideline has been developed with support and endorsement from the leadership of the American Academy of Oral and Maxillofacial Pathology and the North American Society of Head and Neck Pathologists to recommend the use of standardized histopathologic criteria and descriptive terminology to indicate three categories of lesions within PVL: (1) “corrugated ortho(para)hyperkeratotic lesion, not reactive;” (2) “bulky hyperkeratotic epithelial proliferation, not reactive;” and (3) “suspicious for,” or “squamous cell carcinoma.” Classification of PVL lesions based on a combination of clinical findings and these histologic descriptive categories is encouraged in order to standardize reporting, aid in future research and potentially guide clinical management.
Keywords: Proliferative verrucous leukoplakia, Classification, Pathology criteria, Consensus, Standardized criteria
Introduction
Proliferative verrucous leukoplakia (PVL) is a spectrum disorder of the oral mucosa that shows characteristic, focal when early, adherent multifocal and multicentric white, usually heterogeneous-appearing and often verruciform proliferations. The lesions often involve the gingiva adjacent and sometimes circumferential to the teeth and the mucosa in other intraoral locations [1]. The lesions tend to pursue a relentless clinical course with high rates (about 50%) of recrudescence and progression to squamous cell carcinoma (SCC) [2–4]. Older aged female patients are most frequently affected, generally demonstrating disease development over many years, with active and quiescent phases. Any individual clinical course is variable: most PVL lesions are slowly progressive and persistent before they demonstrate sudden rapid growth, while in a previously uninvolved site, a mass may present de novo as carcinoma. These persistent, multifocal lesions are resistant to interventions, suggesting a field cancerization phenomenon [5–7]. Given the diversity of histologic features seen within the spectrum of PVL, it has been difficult to determine uniform and reproducible histologic criteria that can be applied by both oral pathologists who may be knowledgeable clinically about the disorder, and practicing general pathologists who may not be familiar with the clinical presentation and course of this unusual disease [8–10]. While it is imperative to have good clinical descriptions and, ideally, intraoral photographs for documentation, reliable and reproducible histologic features can still be identified to support the clinical-pathological correlation required for a diagnosis of PVL. A great many diverse histomorphologic descriptive terms have been applied (including verruciform/verrucous/papillary hyperkeratosis, verruciform epithelial hyperkeratosis, verrucous epithelial proliferation/hyperplasia, papillary keratosis, atypical verrucoid proliferation, and atypical verrucous hyperplasia), such that the significance of the terminology is diluted or lost, impeding consistent diagnostic terminology by pathologists, and posing management challenges for clinicians [8]. This expert consensus guideline has been developed by members of this consensus group with support and endorsement from the leadership of the American Academy of Oral and Maxillofacial Pathology (AAOMP) and the North American Society of Head and Neck Pathologists (NASHNP) in an effort to provide uniform microscopic criteria and reporting terminology that can be applied in daily clinical practice. The intent is to guide future studies, increase accuracy of diagnosis by standardized terminology, and aid in developing better treatment options that match the lesions in each diagnostic category.
Materials and Methods
Working Group
Approval was obtained from the University of Florida Institutional Review Board (IRB).
Each representative from the working group was approved for participation within the IRB. Both board-certified oral and maxillofacial pathologists and board-certified pathologists with expertise in head and neck pathology agreed to participate, based partly on participation in the inter-observer variability study [8]. Members represented academic medical centers (SGF, IB, MNI, DMC, MWL, SBW, NV), an oral pathology private practice (SM), and an integrated managed care consortium covering 12 geographically separate medical centers that provided routine clinical cases (LDRT). The first author of the inter-observer variability study as preamble to this expert consensus guideline was also part of the working group (JDU).
Study Cohorts
Each member of the working group selected PVL patients for possible inclusion in the study based on established PVL clinicopathologic criteria [1–4]. Patients had to have the following: (1) multifocal lesions which demonstrated clinical progression or alterations over time with multicentric recurrence; (2) multiple biopsies obtained from various different sites over time showing the spectrum of histologic features known to be seen in PVL; (3) a minimum of 36 months of clinical follow-up; and (4) documentation of the development of at least one oral SCC during the period of observation (unless the patient was lost to follow-up or died of unrelated causes before carcinoma developed). Cases submitted included: (1) 63 separate biopsies from 23 patients from University of Florida (SGF, IB, MNI, DMC); (2) 55 separate biopsies from 21 patients from Southern California Permanente Medical Group (LDRT); (3) 64 separate biopsies from 20 patients from Atlanta Oral Pathology (SM); (4) 86 separate biopsies from 9 patients from University of Chicago (MWL); (5) 20 separate biopsies from 9 patients from Brigham and Women’s Hospital (SBW); and (6) 11 biopsies from 2 patients from the University of Texas School of Dentistry at Houston (NV).
All anonymized and coded hematoxylin and eosin-stained glass slides were digitized into whole slide images (WSI) using the Aperio AT2 platform (Leica Biosystems, San Diego, CA) at 20x magnification to ensure uniform, consistent, and standardized materials for review. There was no potential for discrepant diagnoses based on different or deeper levels, as could be created by serial slides sectioning; no slide breakage; no differences in staining; identical materials for review independent of time (i.e., all reviews could be done simultaneously if multiple users were logged in at the same time). The WSI were placed on a secure, authentication required server accessible to the group. All cases were reviewed using either Aperio eSlide Manager or Aperio ImageScope web-browser-based software to assess the validity of inclusion, histologic quality of the material, scanning technical specifications, fragmented or small biopsies. As digital pathology is validated and approved for primary diagnosis and all pathologists participating in the project are experienced digital pathology users, the fact that glass slides were not reviewed was considered of no practical significance. With significant histologic overlap among the 299 biopsies, the highest technical quality material was reviewed by members of the working group utilizing a modified Delphi technique. The Delphi method tries to arrive at a group opinion or decision by surveying a panel of experts with several rounds of questionnaires or surveys, from which the responses are aggregated and shared with the group by a facilitator (LDRT). While the technique is supposed to maintain anonymity, given the small pool from which to draw, this component was excluded. This process was formally finalized during an in-person conference held 21 September 2019 in Orlando, Florida. White boards were used to document histologic features already published in the literature on the diagnosis of PVL, with each member of the working group discussing how these findings were weighted, applied, or otherwise used to reach a pathologic diagnosis. Eighty cases were settled upon for potential inclusion based on including 5 pathologic distractors, an approximately equal number of cases within each of the 3 categories, recognizing the potential for interpretation differences, and trying to include a proportionately weighted case number from each member’s institution in the final survey material.
Workgroup Histologic Categories
Four categories were created for histologic lesions of PVL, recognizing they might not represent an arc of development relative to any one individual lesion’s progression, and no such continuum should be implied. It is well to recognize that there is an arbitrary nature to creating categories out of a histologic spectrum of lesions. The agreed upon categories included:
“Corrugated ortho(para)hyperkeratotic lesion, not reactive;”
“Bulky hyperkeratotic epithelial proliferation, not reactive;”
“Squamous cell carcinoma;”
“Does not fit any above category.”
These categories (see Table 1) are illustrated in the following figures, recognizing variation in each individual biopsy within a category as well as between categories.
Table 1.
Major histologic categories of proliferative verrucous leukoplakia
| Corrugated ortho(para)hyperkeratotic lesion, not reactive | Bulky hyperkeratotic epithelial proliferation, not reactive | Suspicious for, or Squamous cell carcinoma |
|---|---|---|
|
Disproportionate orthokeratosis: Orthokeratosis > 1/2 of epithelial thickness adjacent Troughs and crests of keratosis and/or epithelium: i.e., corrugation Wave-like undulation commonly seen in sentinel lesions Prominent crests or spikes in clinically worrisome lesions (formerly “Christmas tree keratosis”) Minor subgroup in this category shows flat, dense, markedly thickened orthokeratin with atrophic underlying spinous layer (“proliferative leukoplakia”) Usually prominent granular layer Skip segments of ortho- and parahyperkeratosis Absent to scant acute surface inflammation Loss of rete pegs and/or atrophic epithelium for site Sharp demarcation/abrupt transitions Architectural distortion greater than cytologic atypia |
Amplified bulkiness of the epithelial proliferation that accounts for the lesion’s thickness rather than keratosis (usually orthokeratosis) Bulbous rete pegs that sometimes coalesce to appear confluent, with architectural abnormalities overshadowing cytologic findings Separation artifact between epithelium and stroma Lichenoid inflammation at advancing epithelial front sometimes present Consider risky sites in order: gingiva > soft palate > floor of mouth > buccal > tongue |
Voluminous squamous epithelial proliferation with acanthotic endophytic-appearing columns with complex folding and invaginations: More than 3–4 times adjacent uninvolved epithelial thickness Thick, clubby, bulbous, blunt, downwardly-directed rete peg projections: May or may not extend below level of adjacent epithelium, often lacking classical invasion or extension below adjacent epithelium Basement membrane often intact Intraepithelial microabscesses, sometimes with keratin pearls Increased intraepithelial eosinophils Muscle abutment/displacement Parakeratotic crypting Occasional church-spire hyperkeratosis in some Focal dysplasia may be present, but usually limited |
| Helpful criteria | ||
|
Biopsy non-inflamed mucosa with adequate stromal interface to allow interpretation Clinical findings include: well demarcated leuko- or erythroplakia; “ring around the collar” appearance (marginal and attached gingiva specifically); frequent association with fissuring Limited to absent dysplasia in majority of cases Shredded, shaggy keratosis with bacteria may complicate a PVL lesion secondary to trauma Limited fungal colonization in early lesions; often more prominent in carcinomas, but should not preclude interpretation of the underlying disorder Unpredictable progression | ||
Corrugated Ortho(para)hyperkeratotic Lesion, Not Reactive
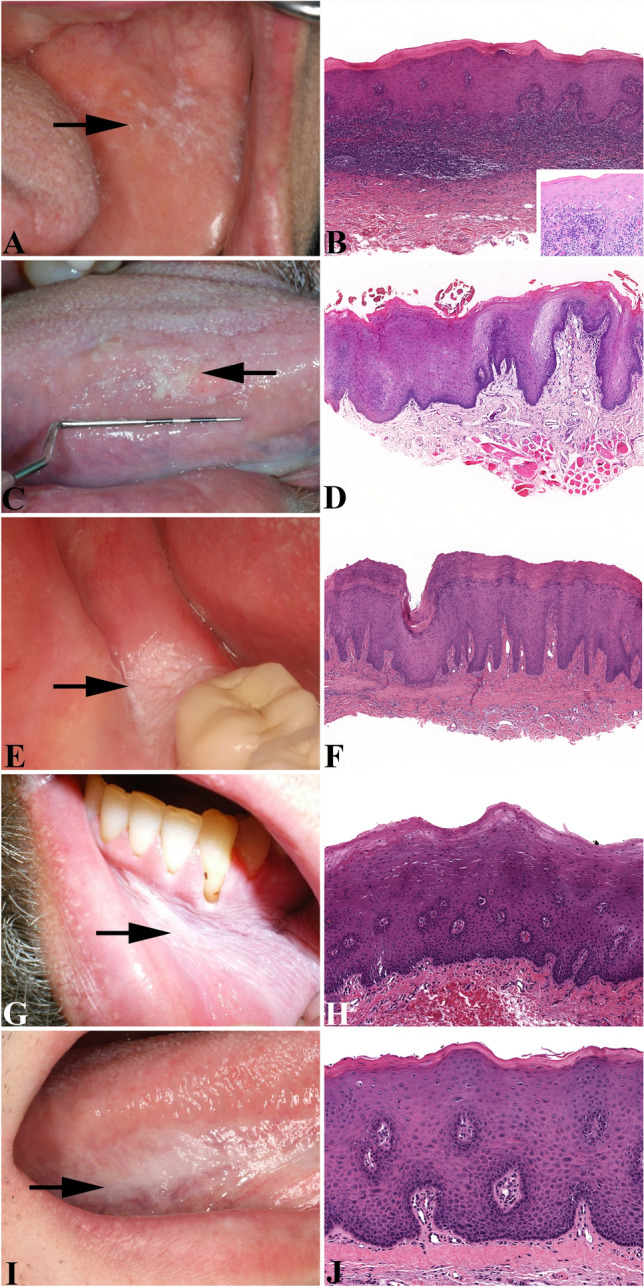
Figure 1 includes illustrations of the clinical (Fig. 1a) and histologic features seen in the corrugated ortho(para) hyperkeratotic lesion, not reactive category (Fig. 1b-e). Corrugation is seen in either the keratotic surface or the epithelial compartment, or both. There is wave-like undulation to the epithelium or to the keratosis and some areas exhibit a ‘basket-weave’ pattern (Fig. 1b). More prominent crests may be seen in some lesions (formerly the term “Christmas tree keratosis” or chevrons was applied to this pattern). Alternatively, some lesions demonstrate a flat, dense, markedly thickened layer of orthokeratin and an atrophic underlying spinous cell layer (conceptually proliferative leukoplakia rather than proliferative verrucous leukoplakia). This category demonstrates disproportionate orthokeratosis, which in many cases exceeds one half of the epithelial thickness over which it is identified (Fig. 1c). Hyperparakeratosis may also be seen, but hyperorthokeratosis is usually dominant. Shredded, shaggy keratosis with bacterial colonies may sometimes be seen in these lesions secondary to trauma. Abrupt transitions from the adjacent contiguous epithelium are usually evident (Fig. 1d), resulting in a sharp demarcation from the unaffected epithelial tissue (described here as a histologic feature, it is often also a clinical finding; Fig. 1a). Other transitions may be present as “skip” segments (i.e., normal/abnormal/normal/abnormal), specifically in relation to mounds of ortho/parahyperkeratosis (Fig. 1e). A prominent granular cell layer often stands out below the orthokeratosis. There is usually a loss of rete pegs as compared to what would normally be seen in the affected anatomic site (Fig. 1d). Epithelial atrophy relative to the specific site, may or may not be evident, recognizing that in each intraoral anatomic subsite there is a characteristic normal epithelial thickness and relationship to the underlying stroma. In some cases, a prominent band-like inflammatory infiltrate is present at the interface which can cause confusion with a lichenoid mucositis. Secondary fungal infection/colonization is quite uncommon in this type of proliferation.
Fig. 1.
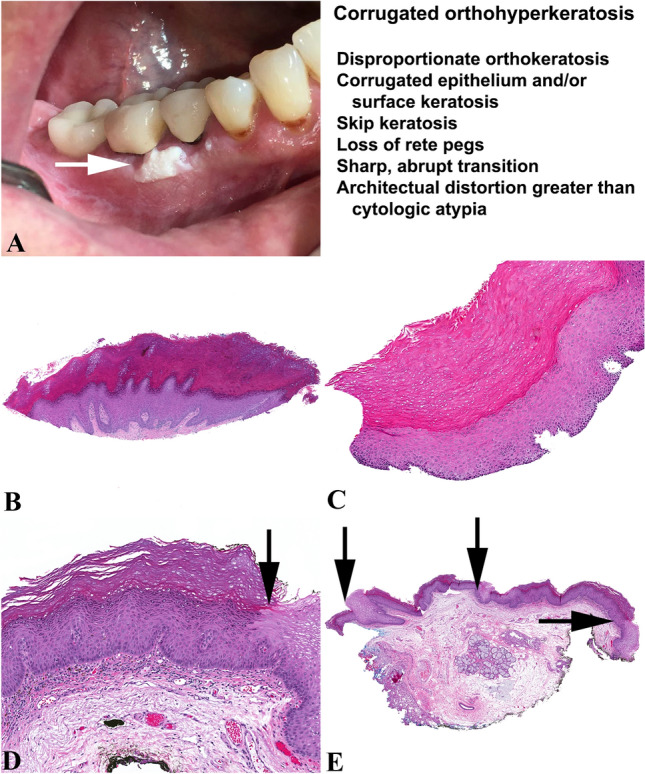
Corrugated ortho(para)hyperkeratosis, not reactive. a A clinical photograph of a gingival verruciform leukoplakia (white arrow), adjacent to teeth. b Marked orthohyperkeratosis and epithelial corrugation, with the thickness of the hyperkeratosis > 1/2 of the total biopsy thickness. c Marked orthohyperkeratosis, about twice the thickness of the epithelium below. d Corrugated keratosis and corrugated (undulating) epithelium, showing an abrupt (black arrow) transition to the adjacent epithelium showing limited epithelial dysplasia. e Abrupt, sharp transitions and skip zones of orthokeratosis (black arrows) are a common finding
Bulky Hyperkeratotic Epithelial Proliferation, Not Reactive
Figure 2 includes illustrations of the clinical (Fig. 2a) and histologic features of the bulky hyperkeratotic epithelial proliferation, not reactive category (Fig. 2b–e). This lesional category, roughly intermediate between corrugated orthohyperkeratosis and SCC, poses the greatest challenge for reaching consensus and reproducibility. In this category, the composite epithelial features are clearly amplified with either or both exophytic and endophytic proliferations (Fig. 2b and e), but are not sufficient for rendering a definitive diagnosis of carcinoma. There is a bulkiness to the epithelial proliferation: in essence, the epithelial compartment, rather than the surface hyperkeratosis, accounts for the lesion’s thickness (Fig. 2c and e). Keratosis overall is not as pronounced and orthokeratosis is not prominent in this category (Fig. 2c). The epithelium shows bulbous rete pegs that sometimes coalesce to appear confluent, and artifactual separations may be noted between the epithelium and superficial lamina propria (Fig. 2c and e). An inflammatory infiltrate is often seen at the advancing epithelial front, but without destruction of the epithelial-stromal interface (Fig. 2c and e). The degree of cytologic atypia may be modest, yet architectural disorder is readily identified and it is the architectural abnormalities that overshadow the cytologic findings. The specific sites of greatest concern include the gingiva, especially when there is a thickened “ring around the collar” effect clinically (1), followed by the palate, floor of mouth, buccal mucosa, and tongue.
Fig. 2.
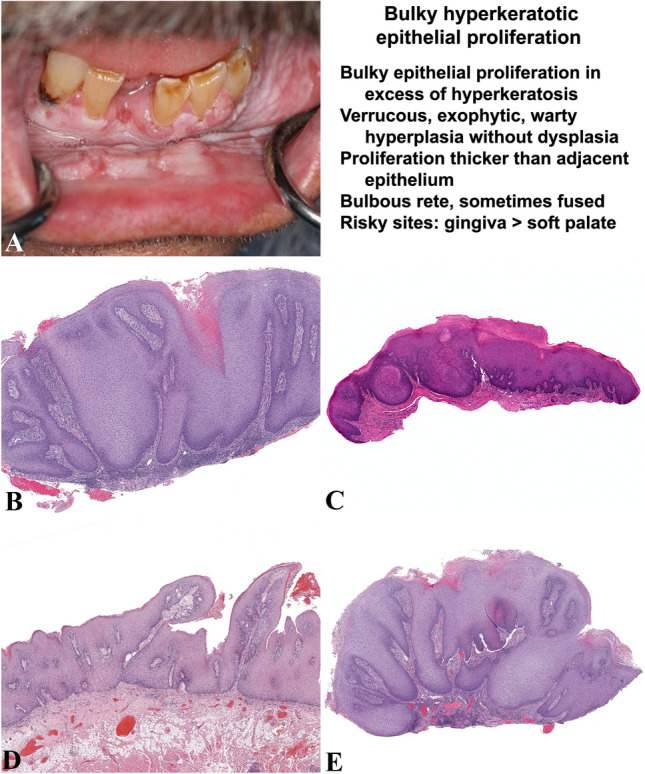
Bulky hyperkeratotic epithelial proliferation, not reactive. a Diffuse and bulky, heterogeneous white plaque affecting the mandibular anterior segment (attached gingiva, alveolar mucosa, lower labial vestibular, and labial mucosa), contiguous with the posterior buccal vestibule and buccal mucosa. Note the dry, fissured appearance of the lower left buccal vestibular mucosa. b Low power view of a mucosal wedge showing the bulky, endophytic proliferative epithelial pattern of cytologically bland cells with broad, blunted, downwardly directed rete pegs that markedly increase the top-to-bottom width of the epithelium. The rete pegs appear to merge toward one another as they attain a uniform depth. The epithelial surface is slightly undulating with a surface crypt filled with parakeratin. c The epithelium is bulky and thickened with easily identified hyperkeratosis plus expanded, blunt rete pegs. d Low power view of undulating surface epithelial proliferation with exophytic foci covered by parakeratin. The rete pegs are uniform in depth, blunt, and broad. e As a biopsy sample, the tangential sectioning artifacts affect interpretation of the endo-exophytic bulky epithelial proliferation showing an undulating surface. The rete pegs are elongated and rounded at their tips, and together they reach a uniform depth. However, comparison to the adjacent epithelium cannot be achieved and so carcinoma cannot be diagnosed
Suspicious for Squamous Cell Carcinoma or Squamous Cell Carcinoma
Figure 3 includes illustrations of the clinical (Fig. 3a) and histologic features of the suspicious for SCC or unequivocal SCC category (Fig. 3b-e). This category includes verrucous SCC (VSCC), SCC with papillary architecture (i.e., not classic HPV-associated papillary SCC), and in addition, a unique lesion of PVL also characterized by cumbrous-appearing epithelium, described frequently as having a “stuck-on” appearance, without conventional invasive growth (Fig. 3b), although pressure erosion of bone may be seen (not seen is single discontinuous cell or tumor islands definitively invading into connective tissue or bone). Aside from VSCC and SCC with papillary architecture, there are additional epithelial proliferations that impart the impression of a barnacle stuck-on a surface, but these proliferations lack exophytic verruciform or “church-spire” type keratosis (later introduced herein as “barnaculate carcinoma”). In these lesions, the epithelium shows a significantly voluminous proliferation with acanthotic, endophytic-appearing columns that exhibit complex folding and invaginations (Fig. 3c) to a much greater degree than seen in the bulky hyperkeratotic epithelial proliferation category. Quantitation cannot be provided as specimen variation precludes such an attempt, but the generalized thickness is often more than 3–4 times the thickness of the adjacent uninvolved epithelium (Fig. 3b and c), which can be used as a guide when present. There are bulbous, blunt, downwardly-directed rete peg projections that may or may not extend below the level of the adjacent epithelium (Fig. 3d). Importantly, in cases clinically consistent with PVL and similar to what is seen in verrucous carcinoma, bulky exophytic (and often endophytic) epithelial masses that project outward into the lumen of the oral cavity may lack definitive histopathological evidence of “invasion,” yet qualify for inclusion as carcinoma. The basement membrane in some instances may be intact, similar to VSCC. In other cases, there is blurring of the epithelial-stromal interface whereby the epithelium appears to trickle into the markedly inflamed connective tissue, but still lacks the definitive histopathological evidence of “invasion” that is seen in conventional SCC. Intraepithelial microabscesses intimately associated with keratin pearls are histologic indicators of a carcinoma diagnosis (Fig. 3e). Additionally, both intraepithelial and stromal infiltration by eosinophils may be seen in these particular carcinomas.
Fig. 3.
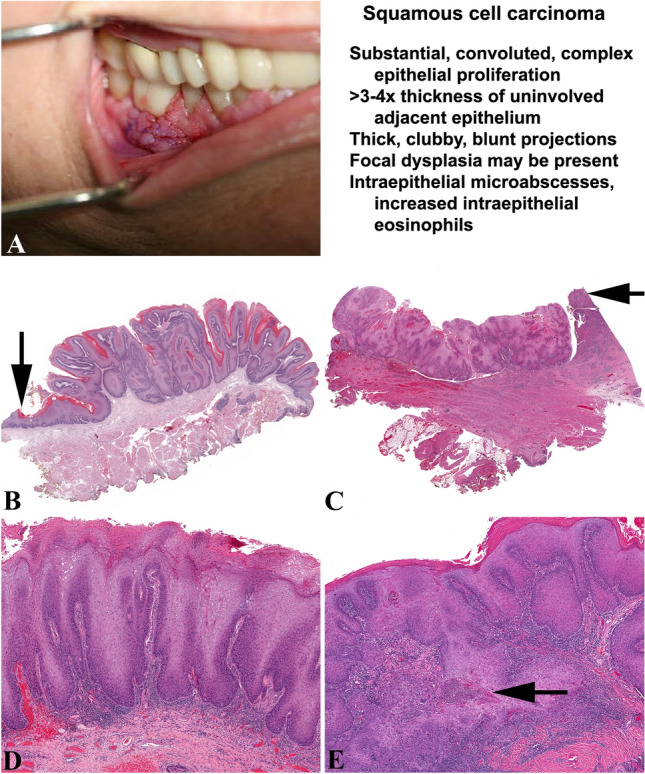
Squamous cell carcinoma. a A clinical photograph of a gingival mass enveloping several teeth, with a pebbly configuration. b A substantial, convoluted and complex epithelial proliferation much thicker than the uninvolved adjacent epithelium (black arrow), but lacking an invasive pattern below the level of the epithelium. c Broad, pushing border of infiltration displacing muscle and extending below the adjacent epithelium (black arrow). There are thick, clubby projections with a complex architecture. d The rete pegs are notably thickened and elongated; there is surface hyperkeratosis with a verrucous pattern. The rete pegs are 5x the thickness of the adjacent epithelium, but there is absence of cytologic atypia. e Conventional SCC showing broad islands and nests of destructive infiltration into the stroma. There are microabscesses present within the deep portions of the epithelium (black arrow)
In traditional VSCC, parakeratotic crypting, para- and orthohyperkeratosis, and church-spire hyperkeratosis are seen; occasionally, masticatory friction may blunt or eradicate the “church-spire” appearance in some tumors. Mild cellular atypia is observed in the basal-most epithelial strata rather than the suprabasal compartment of the epithelium. In the reviewed cases, PVL-associated carcinomas did not show cytologic pleomorphism as a prominent feature, whereas the topographic architectural characteristics of PVL-associated carcinomas comprise the more impressive features. In short, the PVL carcinomas are bulkier, lack both marked pleomorphism and increased mitoses, and are less likely to demonstrate individual cell invasion into the underlying stroma as compared to conventional oral SCCs that do not arise in PVL. Again, the exact degree of cytologic atypia cannot be reliably quantified as many findings contribute to the interpretation. However, if there are easily identified areas of pleomorphism, the lesion is more likely a conventional SCC than the verrucous, papillary, and barnaculate-types seen most often in PVL-patients.
Given the very high risk of developing carcinoma balanced against the potential for radical overtreatment, a diagnosis of “bulky exo- and endophytic squamous proliferation, suspicious for SCC” category is a useful designation for cases that fail to fully satisfy definitive histologic criteria for carcinoma or exhibit sampling artifacts, tangential sectioning artifacts, or where the stromal interface is artifactually absent.
Survey Construction
Two surveys were constructed to evaluate criteria that may be used in establishing diagnoses. Both surveys were responded to by 19 members of the group (SGF and JDU constructed the surveys with case selection, randomization, and technical considerations and thus did not submit responses). The first survey contained 50 cases, 5 of which represented non-PVL diagnoses, sent for evaluation without any clinical data (i.e., patient age, sex, anatomic site, biopsy location, clinical appearance of the lesion, and clinical photographs were not included). WSI were reviewed at the pace of the reviewer without any time constraints. A separately submitted survey form using Qualtrics survey tool was completed anonymously by the reviewer for two respective, independent completion periods: Survey 1: December 2019-February 2020; Survey 2: April-June 2020. Due to submission requirement deficiencies, two cases were removed from Survey 2. Additionally, Survey 2 included clinical data, along with clinical photographs from 27 cases.
Statistical Analysis
Inter-observer variability between pathologists relative to histologic diagnoses was evaluated by inter-rater agreement analysis using The R Project for Statistical Computing Version 4.0.2. Agreement or kappa (κ) score is commonly used to evaluate reliability of paired agreements against pure chance agreement [range 0 (random agreement) to 1 (perfect agreement) [11]; see Table 2]. Using IBM Statistical Product and Service Solutions (SPSS) version 25, paired t-test was used to compare mean agreement scores for cases between Survey 1 and 2 with normally distributed data, considering p < 0.05 at 95% confidence intervals as statistically significant; and Chi-square was used to compare differences between categorical groups.
Table 2.
Interrater agreements for surveys 1 and 2
| Inter-rater agreement | κ value | Survey 1 cases | Survey 2 cases |
|---|---|---|---|
| No agreement | < 0 | None | None |
| Slight agreement | 0.00–0.20 | None | None |
| Fair agreement | 0.21–0.40 | n = 13/48 (27%) | n = 13/48 (27%) |
| Moderate agreement | 0.41–0.60 | n = 23/48 (48%) | n = 19/48 (40%) |
| Substantial agreement | 0.61–0.80 | n = 11/48 (23%) | n = 15/48 (31%) |
| Almost perfect agreement | 0.81–1.00 | n = 1/48 (2%) | n = 1/48 (2%) |
Survey Results
Survey 1 had 100% responses from 19 reviewers, while Survey 2 had complete responses from 17 reviewers; due to technical reasons, several cases were incomplete for the remaining 2 reviewers’ evaluations. Inter-rater agreement analysis (a method of kappa testing) was performed for each case (Table 2), using standard interpretation agreements.
In general, substantial or moderate agreement was achieved for the corrugated ortho(para)hyperkeratotic lesion, not reactive category and the suspicious for SCC and SCC category, respectively, with a Chi-square of p = 0.015, while there was moderate or lesser agreement for the bulky hyperkeratotic epithelial proliferation category (kappa 0.2–0.6). Further, using a paired t-test to compare the means of kappa agreement from Survey 1 and 2, there was a mean kappa score of 0.505 for Survey 1 compared to 0.520 for Survey 2, yielding a p = 0.370 (95% confidence interval), resulting in no statistically significant difference in survey interpretation when the clinical photos and/or site of the sample were included. There were 27 cases with photographs in Survey 2. Chi-square measuring category of change (increase, decrease, or no change) between Survey 1 and 2 on comparing cases with photographs and those with no photographs was p = 0.120, showing a lack of statistical significance. The cases that yielded the highest kappa statistic of substantial to almost perfect agreement in at least one of the surveys were 11 cases from the corrugated ortho(para)hyperkeratotic lesion, not reactive category and 7 cases from the suspicious for carcinoma and carcinoma category, while only one case from the bulky hyperkeratotic epithelial proliferation category showed similar agreement.
Anatomic Subsite Designations
All members of the working group agreed that having a record of the affected oral cavity site(s) was critical, especially recognizing that in each intraoral anatomic subsite there is a characteristic normal epithelial thickness and relationship to the underlying stroma (Fig. 4). Table 3 documents the oral subsites that must be indicated on surgical pathology requisition forms and/or included in clinical history information, in order for multicentric (i.e., multiple lesions affecting contiguous or adjacent sites) and multifocal lesions (i.e., multiple topographically separate and distinct sites) to be adequately documented. Any case with bilateral involvement was considered multifocal disease. The working group also noted an increased risk of malignancy based on certain subsites within the affected oral cavity.
Fig. 4.
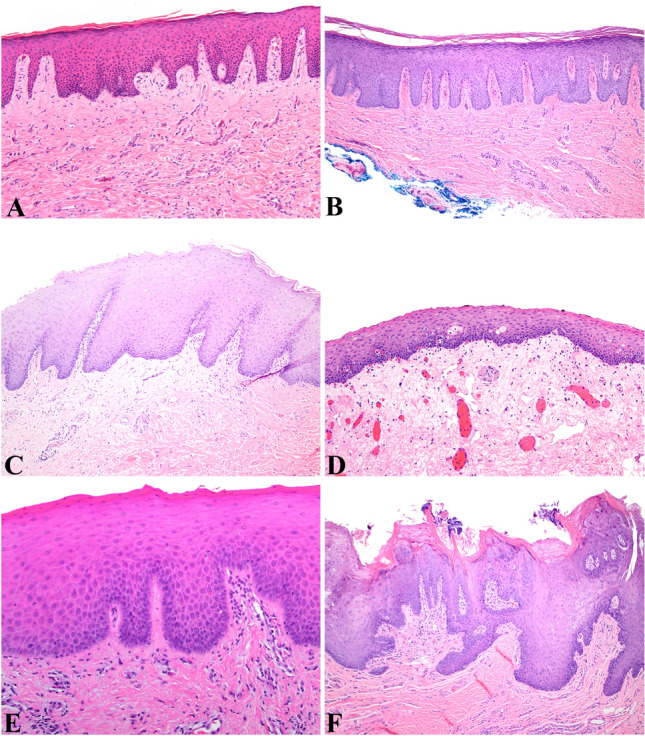
Normal histology by oral cavity subsite. a Gingiva: Stratified highly keratinized squamous epithelium with well-formed rete pegs that extensively interdigitate with the lamina propria to increase the surface area for epithelial attachment to the connective tissue. b Palate: Stratified keratinized squamous epithelium with elongate rete pegs that are composed of 4–8 cells wide that also allow for connective tissue attachment (fixed epithelium). c Buccal mucosa: A relatively thick stratified squamous non-keratinized epithelium lines the buccal mucosa and lips, with relatively broad rete (free epithelium). d Floor of mouth: A relatively thin non-keratinizing squamous epithelium without well-formed rete. e Tongue: Lateral tongue with a keratinized stratified squamous epithelium. f Dorsal Tongue: a complex epithelium containing papillae (filiform) with narrow bases and a well keratinizing surface
Table 3.
Oral subsites (clarifying contiguous and multifocal or multicentric involvement)
| Oral anatomic subsite | Site focality |
|---|---|
| Alveolar or gingiva (gum) mucosa upper jaw | Right, left, midline |
| Alveolar or gingiva (gum) mucosa lower jaw | Right, left, midline |
| Vestibule of mouth: maxillary | Right, left, midline |
| Vestibule of mouth: mandibular | Right, left, midline |
| Buccal/cheek mucosa | Right, left |
| Dorsum of the tongue | Right, left, midline |
| Border/lateral tongue | Right, left |
| Ventral tongue surface | Right, left, midline |
| Floor of the mouth | Right, left, midline |
| Hard palate | Right, left, midline |
| Soft palate | Right, left, midline |
| Upper lip mucosa, including vermilion border | Right, left, midline |
| Lower lip mucosa, including vermilion border | Right, left, midline |
Virtual Consensus Conference
An all-day virtual consensus conference was held 26 July, 2020 via the Zoom cloud platform for video conferencing, including audio and content sharing, with chat operated through a paid commercial account using both desktop and mobile devices, with the session cloud recorded for permanent access. Further, Poll Everywhere virtual polls were used to live-poll members of the conference in real time, with results shared instantly upon concluding the poll as it related to diagnosis of virtual cases being screen shared at the time. Virtual slides of the cases were reviewed by screen sharing, using the Leica Systems Aperio ImageScope Version 12.4.3.7009. Each member of the consensus conference (22 participants) was responsible for discussing at least one case, specifically highlighting their unique approach to case diagnosis, criteria used to inform their opinion, assessment of clinical and histologic features, and given the time equal to others to suggest approaches and criteria to consider in diagnosis. The following discussion paragraphs summarize the lively exchanges which ultimately led to categorization of lesions into three related, sometimes overlapping groups. These categories take a biologic continuum and arbitrarily try to provide distinct boundaries, recognizing that mother nature will still confound these attempts in daily practice, but accepting that initial parameters are likely to require further refinement over time and with more data.
Discussion
Background
Proliferative verrucous leukoplakia (PVL) is recognized first and foremost as a clinical-pathological phenomenon. It is characterized by the progressive, contiguous spread and multifocality of oral mucosal surface changes that are keratotic and often become increasingly textured, heterogeneous, and in some cases, nodular and possibly indurated over time. Although “verrucous” is the descriptive term included in the disease designation, not all PVL lesions exhibit a verrucous clinical appearance. As such, the term “proliferative leukoplakia” has been suggested as a better, all-encompassing term (including by authors of this manuscript)[12]. However, the histologic features and taxonomy are already fraught with inconsistencies, so that it is probably best to leave the name debate out of this presentation. Of great significance, PVL lesions have a recognized propensity for development of SCC [3, 4] in about 50% of patients. Moreover, given the characteristic multifocality of PVL, carcinomas can arise in multiple, noncontiguous oral mucosal sites. Additionally, unlike a majority of non-PVL associated SCCs, which demonstrate a predilection for the classic “oral cancer-prone sites” (lateral/ventral tongue, floor of mouth, soft palate), the carcinomas that arise in PVL show preference for other locations, most significantly the gingiva, alveolar mucosa, buccal mucosa, palate, and dorsal tongue, with contiguous extension to or from adjacent oral mucosa. Single, contiguously affected oral mucosal areas, often demonstrate the “life of the lesion,” as it progresses from a hyperkeratotic plaque to a frankly malignant mass.
Prior studies have revealed considerable inter-observer variation among pathologists in histopathologic diagnostic interpretation of oral lesions [13–22], with a notable paucity of literature concerning inter-observer variability in diagnosis of PVL specifically [8]. The various evolutionary stages within the condition’s clinical-pathological spectrum render a definitive diagnosis of PVL based strictly on histopathologic findings challenging. Aside from the historical lack of specific histopathologic diagnostic criteria for PVL, the broad diversity in histomorphologic terminology used to describe microscopic findings is subject to remarkably different interpretations, so that establishing a PVL diagnosis can be quite confounding. Clinical interpretation of terms like “verrucous hyperplasia,” “atypical verrucous lesion,” and “atypical epithelial lesion” can be perplexing, resulting in significant diagnostic and management impediments [23, 24]. Clearly, it is imperative to consider both the clinical presentation and history in concert with the histopathology of representative specimens in order to establish a PVL diagnosis. Importantly, when feasible, it is always best to avoid obtaining a biopsy in foci where there are ulcerations and obviously inflamed mucosal sites, focusing on non-inflamed mucosa and junctions with normal-appearing mucosa as the best sites for diagnostic material. The PVL consensus group asked the following questions:
What are the important differential diagnostic considerations of PVL?
Are there consistent histopathological features that correlate with the range of clinical manifestations of PVL lesions? If so, what are they and can they be systematically categorized?
Is there a reproducible or predictable clinical-pathological continuum that characterizes the development of PVL lesions?
Can an individual PVL lesion’s histopathological findings reliably predict progression to carcinoma?
Differential Diagnosis
Clinically, at initial presentation, corrugated ortho(para)hyperkeratotic lesions, not reactive and bulky hyperkeratotic epithelial proliferation, not reactive may not be easily clinically distinguished from benign reactive lesions, oral lichen planus, traumatic/frictional keratosis, alveolar ridge (hyper)keratosis, tobacco pouch keratosis, or unifocal leukoplakia. It is often, usually after several biopsies over months to years, that lesions develop multifocality or diffuse spread, finally allowing for PVL to be recognized. In fact, the diagnosis of PVL has been defined by some to require multiple non-contiguous white lesions or one lesion over 4 cm in size, which shows progression over time [12]. Although the clinical appearance of sentinel PVL lesions can vary from smooth to fissured/verruciform (dry river bed appearance) or verrucous lesions, and may also encompass erythematous or ulcerated lesions, several clinical features have been recognized as potentially worrisome [12].
Not all white mucosal plaques with hyperkeratosis are PVL. There are several other clinical-pathological entities to be considered in the differential diagnosis. Some non-PVL white, adherent plaques may also be distributed multifocally. The specific entities most appropriate for inclusion in the differential diagnosis of PVL are the following (Fig. 5).
Fig. 5.
Clinical and histologic mimics of PVL. a Clinical photo of delicate buccal lace-like striations (black arrow) in a case of lichen planus. b A dense, band-like lymphocytic infiltrate associated with vacuolar degeneration of the basal keratinocytes (inset). There is acanthosis and hyperkeratosis in this case of lichen planus. c A clinical photograph of lateral tongue keratosis with a shaggy appearance in traumatic hyperkeratosis. d Traumatic hyperkeratosis showing shaggy keratin with hyperkeratosis and thickened squamous epithelium. e A clinical photograph of retromolar pad white plaque clinically consistent with benign alveolar ridge keratosis (BARK). f This example of BARK shows moderate hyperkeratosis with a prominent granular layer and elongated, tapered rete pegs, focally coalescing at the base with scant inflammation. g A clinical photograph of fissured, gray-white leukoplakia along the sulcus in tobacco pouch keratosis. h There is epithelial thickening with thin hyperkeratosis, but neither significant atypia nor significant hyperkeratosis is seen in this example of tobacco pouch keratosis. i A clinical photograph of lateral tongue leukoplakia. j The histology shows focal hyperkeratosis with a thickened epithelium showing at least low grade dysplasia, with architectural as well as cellular atypia
Lichen Planus
Differentiation of corrugated orthohyperkeratotic lesions from oral lichen planus and associated conditions is often doubly problematic, as lichenoid type lesions may mimic PVL both clinically and histologically [25]. Classic oral lichen planus (OLP), the sine qua non of oral lichenoid lesions, is a chronic, self-limited, immune-mediated mucocutaneous disorder that mostly affects middle aged or older adults. It presents with multifocality as classic bilateral and symmetrical white, lace-like macular reticulations on the buccal mucosa, gingiva, tongue, and other oral locations (Fig. 5a). The lesions may very rarely coalesce to form plaques, often accompanied by erythema, ulceration/erosion, or atrophy. Other lichenoid conditions may also overlap with PVL. These include oral lichenoid drug reactions, oral lichenoid lesions due to dental materials or flavoring agents, and systemic conditions with a lichenoid profile, such as graft-versus-host-disease and systemic and discoid lupus erythematosus. Demographically PVL and OLP both frequently affect similar patient populations, most particularly women in middle age or older age groups. In addition, the most frequent clinical locations affected in both conditions are the gingiva and buccal mucosa [25, 26]. OLP exhibits several clinical variants which are white in appearance: these include the reticular pattern and the papular pattern. Histologically, parakeratosis or minimal to absent orthokeratosis overlies atrophic or acanthotic epithelium. The rete pegs may be “saw-tooth” or atrophic; the basal keratinocytic layer shows vacuolar change with round, eosinophilic, degenerate keratinocytes (Civatte, colloid, hyaline, or cytoid bodies) within the epithelium. Characteristically, there is an interface mucositis with basement membrane obfuscation and blurring due to a tight band-like, predominantly T-cell, lymphocytic infiltrate at the stromal-epithelial junction, intimately intermingled with the basal cells and superficial lamina propria (Fig. 5b). There may be frank ulceration and subepithelial separation or clefting in some cases. Epithelial dysplasia is absent, although in some cases, due to intense inflammatory influence, reactive atypia can be seen [25, 26].
Traumatic Hyperkeratosis (Frictional Hyperkeratosis, Benign Reactive Epithelial Hyperplasia)
Traumatic hyperkeratosis results most often from chronic biting (cheek: Morsicatio buccarum and tongue: morsicatio linguarum) and toothbrushing or other sources of abrasion such as orthodontic appliances, dentures, or parafunctional habits. Depending on the source of frictional irritation, it is possible for more than one oral site to be affected. Many lesions arise along the occlusal plane of the dentition on the buccal mucosa and lateral tongue. Patients may not be fully aware of the extent of their habit. Clinically, the mucosal surface may appear irregular, shaggy, macerated, rough, shredded, and thickened (Fig. 5c), with or without erythema or ulceration. Histologically, there is acanthosis, and hyperparakeratosis showing normal maturation and cytology, edema within keratinocytes, and plasma pooling typical of reactive lesions. Shaggy or frayed keratin often with bacterial surface colonies may be noted (Fig. 5d). There may or may not be an inflammatory infiltrate [24, 27–30].
Linea alba is a very specific and commonly encountered presentation of benign, reactive hyperkeratosis that appears on one or both buccal mucosae as a uniform, adherent horizontal white line along the occlusal plane. It is entirely attributable to friction from the repetitive interdigitation of the teeth in the course of daily function and is not attributable to a parafunctional habit.
Alveolar Rdge (Hyper)keratosis
Alveolar ridge (hyper)keratosis (also known as benign alveolar ridge keratosis, or “BARK”) presents as a white plaque without erythema or ulceration on the retromolar pad (Fig. 5e) or on the crestal gingiva of an edentulous region of the alveolar ridge. BARK is analogous to lichen simplex chronicus of skin. BARK is typically confined to the crest of the alveolar ridge in edentulous areas where trauma from mastication occurs. If edentulous ridge areas are involved in a corrugated orthohyperkeratotic lesion, the changes are generally not confined exclusively to the crestal area of trauma, but usually extend to contiguous areas. BARK lesions also frequently exhibit “fading margins” clinically, lacking the abrupt demarcation of corrugated orthohyperkeratotic lesions [30]. Histologically, there is hyperorthokeratosis and hypergranulosis. The rete pegs are elongated, tapered, and may coalesce at their bases (Fig. 5f). Inflammation is insignificant and lesions typically lack plasma pooling or edema of keratinocytes [30–33].
Tobacco Pouch Keratosis
Tobacco pouch keratosis refers to the epithelial alterations attributable to habitual snuff or chewing tobacco use. Clinically, there is a soft to leathery, often fissured gray-white mucosal patch where tobacco is usually placed and held, typically on the labial or buccal and adjacent vestibular mucosae (Fig. 5g). The histological findings include acanthosis, with characteristic chevron-like ortho- or parakeratotic epithelial surface peaks (Fig. 5h). The epithelial cytology and maturation pattern are often normal. However, in some cases atypia or dysplasia is evident. Generally, there is minimal, if any, inflammation [34–36].
Epithelial Dysplasia, Not Attributable to PVL
Cytologic abnormalities, maturation disarray, and in many instances, increased surface keratinization are indicative of epithelial dysplasia, a lesion with potential for progression to carcinoma. The most common entity associated with epithelial dysplasia in the oral cavity is unifocal leukoplakia. Unifocal leukoplakia more commonly affects males, while PVL more commonly affects females. The most common locations for unifocal leukoplakia (lateral and ventral surfaces of the tongue [Figure 5i], floor of mouth, and soft palate-uvula complex) are different from the most common sites for PVL (gingiva and buccal mucosa)[12].
Histopathology reveals epithelial architectural disturbance with blunt rete pegs, increased width of the basal-most stratum, premature (i.e., individual spinous cell) keratinization (dyskeratosis), and a variable degree of nuclear enlargement, pleomorphism, and hyperchromasia (Fig. 5j). Mitoses are frequently increased and may include atypical forms [37, 38]. Frank dysplasia is more frequently found in isolated leukoplakia than in PVL [12]. The malignant transformation rate for non-PVL oral leukoplakia has been recently estimated at 9.5%, compared to the much higher rate of about 50% for PVL [39].
PVL Clinical and Histopathology Features
Two of the categories specifically include “not reactive” in the name to alert the clinician that the lesion does not represent a reaction to friction, trauma, a topical agent, infection, or a vesiculo-bullous disorder. Reactive lesions (discussed below) have a different disease arc that does not bend toward neoplasia, in contrast to what is true of PVL, where neoplastic progression is almost inevitable. Dysplasia is a well accepted term, with various grades and an often predictable arc of clinical development. Since the histologic features in PVL are usually lacking in pleomorphism/dysplasia, this term was also eschewed. It goes without saying that dysplasia can be seen in PVL-lesions, but it should be emphasized that it is uncommon. If dysplasia is present, that diagnosis would be employed instead of any of the categories outlined herein. There are two “not reactive” categories, which creates a binary system, but it must be recognized that one lesion does not necessarily develop into the other and may resolve, persist, or further develop, while the “carcinoma” category is a malignant category.
Viewed microscopically, PVL lesions exhibit a wide range of findings that correlate with clinically apparent lesional tissue volume, and thus, within some guideposts, nearly any clinical presentation is possible and described. But practically, the descriptions included herein cover the vast majority of lesions and may serve more as an overview than an exhaustive exhortation on the topic. For example, an individual white plaque-type lesion in the corrugated ortho(para)hyperkeratotic lesion, not reactive category may demonstrate ortho- or parahyperkeratosis at the surface with or without a prominent granular cell layer if orthokeratin is present; there is often an abrupt or sharp demarcation from the adjacent normal epithelium. The keratin layer may be half to the same thickness of the underlying epithelial compartment in some cases. It may be corrugated with troughs and crests, or flat and dense, although the latter is not as common. Similarly, the underlying viable epithelium is corrugated and can vary in width considerably, from atrophic to acanthotic for that particular oral location. Fungal colonization, while possible, tends to be unlikely in this phase of the disease. Additionally, there may be “skip” segments where a normal surface keratinization for that anatomic location alternates with an abnormal quantity and/or quality of surface keratinization. Or, the epithelial maturation and cytology can vary such that some lesions may exhibit both a normal maturation pattern and normal cytology, while in other lesions cytologic atypia may be evident, alternating abruptly with foci of cytologic normality. If there is both architectural disturbance plus cytologic atypia of varying degree, the composite maturation disarray would indicate epithelial dysplasia. Among the working group there was controversy with regard to recognizing and grading of epithelial dysplasia. As this topic clearly warrants another consensus conference, suffice it to say that in general, PVL-associated lesions may have some atypical cytologic features evident, but the architectural disarray is the overwhelmingly preponderant abnormality.
The sentinel lesions of PVL encompass “keratosis of unknown significance” (KUS) which histologically lacks overt cytological atypia and is not reactive [30], estimated to be the initial finding in up to 50% of PVL cases [40]. Additional architectural disorder is seen as a corrugated surface pattern, herein referred to as corrugated ortho(para)hyperkeratotic lesions, not reactive. Terminology currently in use varies widely and includes verrucous hyperplasia, verrucous hyperkeratosis, or verruco-papillary hyperkeratosis. These lesions generally display an abnormal architecture without significant cytological pleomorphism or any signs of overt malignancy [24]. The diagnosis of PVL is made by clinical and pathological correlation, often requiring multiple biopsies over extended time, in part due to the unremarkable or benign appearance on initial biopsy and often slow progression towards multifocality.
The location is a significant consideration as PVL most commonly affects the gingiva and alveolar ridge, followed by buccal mucosa and less frequently, the tongue [9, 12, 41–44]. Areas within the oral cavity subject to frequent trauma include the buccal mucosa along the occlusal plane, the lower labial mucosa, and the lateral tongue. Thus, when unexplained white lesions are present on the gingiva and/or alveolar ridge, PVL must be considered. Conventional unifocal leukoplakia occurs most frequently on the tongue and floor of mouth [45], not the most common sites of PVL.
An important clinical feature of corrugated orthohyperkeratotic lesions is a sharp and abrupt demarcation from the surrounding tissues, a feature not generally observed in reactive oral lesions [12, 30, 40]. A characteristic, although not exclusive feature, is clinical fissuring or corrugation which sometimes correspond histologically to a skip pattern of keratosis [12, 40]. Gingival PVL lesions commonly exhibit a distinctive linear marginal gingival leukoplakia, with growth that follows the marginal gingiva of single or multiple teeth. With time it may progress to a circumferential lesion surrounding the tooth (“ring around the collar”), seen in early (non-malignant) lesions of PVL, but also seen in PVL-associated carcinomas [1]. One as yet unanswered question is whether all such gingival lesions, regardless of size (for example, involving only one tooth) should be considered PVL.
A key feature of the architectural abnormality in corrugated orthohyperkeratotic lesions, not reactive relates to the normal tissue keratin pattern of the oral cavity. Unlike skin, normal oral mucosa in most locations does not exhibit significant orthokeratin, and any basket-weave orthokeratin is abnormal in the oral cavity (Fig. 4). Site dependent and specific, the amount of keratin is quite varied. For example, the hard palatal mucosa is normally covered by a thin layer of orthokeratin (Fig. 4b) while the floor of mouth is not keratinized (Fig. 4d), and as such, any keratin in a floor of mouth lesion is abnormal even in the absence of cellular atypia (although it could be reactive to trauma, such as from a denture flange).
PVL lesions may show epithelial atrophy [12]. Inflammation is often minimal, normal rete peg configuration may be lost, and trauma-associated plasma pooling or edema of the keratinocytes is not seen [30].
Cytologic pleomorphism or overt dysplasia is rare in corrugated orthohyperkeratotic lesions. In a recent literature review with meta-analysis of 102 patients with PVL, 84% of early stage lesions showed no dysplasia or only mild dysplasia [41]. If high grade dysplasia or carcinoma in situ is present in a biopsy from a patient with clinical PVL, it is not classified as corrugated orthohyperkeratotic lesion, but rather conventional dysplasia.
The histologic features of OLP may be seen in corrugated orthohyperkeratotic lesions. In a study evaluating lichenoid histologic features in 70 cases of oral verrucous hyperplasia, band-like T cell lymphocytic response and basement membrane degeneration were the most commonly observed features in approximately one-third of the cases, with “saw-tooth” rete peg formation, interface stomatitis, and dyskeratotic keratinocyte formation less frequently found [46]. Direct immunofluorescence findings are nonspecific; similar results can be seen in PVL-type lesions and dysplastic lesions with a lichenoid response [47]. Most importantly, OLP diagnosis requires destruction of the basal cells, a strict absence of epithelial dysplasia (although reactive atypia may be present because of inflammation), and an absence of the verrucous epithelial architectural changes frequently seen in corrugated orthohyperkeratotic lesions [26]. The distinction between the two entities is of utmost importance, as OLP has been generally estimated to have a malignant transformation rate of less than 2%, with oral lichenoid lesions slightly higher in some studies [39, 48], while PVL may have an annual malignant transformation rate of up to 10% for patients affected, with a roughly 50% overall malignant transformation rate [12, 39, 41].
Bulky Hyperkeratotic Epithelial Proliferation and Carcinoma Categories
As a PVL lesion assumes a more textured, verruciform, or exuberant bulky, sometimes barnacle-like character clinically, histopathology reveals a corresponding increased magnitude of the squamous epithelium (i.e., a bulky hyperkeratotic epithelial proliferation), with notable architectural disturbance recognizable as elongated, broad, and blunt rete pegs, sometimes accompanied by degrees of cytologic atypia (including premature keratinization), with or without a corresponding increase in surface keratosis. Concurrent fungal colonization/infection may be seen, but the degree of epithelial proliferation is disproportionately greater than what would be expected for an infectious etiology alone. Histopathology may reveal either an exophytic or endophytic epithelial proliferation but usually both patterns coexist. Ultimately, the broadly accepted, key criterion for classifying a PVL lesion as a carcinoma is when there is evidence of epithelial invasion into the underlying stroma or markedly “pushing” encroachment on muscle or other deep submucosal structures (Fig. 3b–e). However, some PVL lesions classified within the bulky hyperkeratotic proliferation category generated considerable controversy. As such, the consensus committee struggled with the features of more advanced PVL. When verrucous carcinoma or conventional type SCC was seen, there was ready agreement in diagnosis. The difficulty was with a particular histologic variant unique in the setting of PVL that does not conform to the defined parameters of VSCC, SCC with papillary architecture, or conventional SCC; therefore, some were reluctant to render a diagnosis of carcinoma. This histologic variant was first described by Shear and Pindborg in 1980 as verrucous hyperplasia [49], occasionally with attendant cytologic and architectural atypia. Since that report, the recognition of PVL has been further defined and refined, but the pathology community still has not acknowledged this unusual histologic pattern as cancer. Distinct from verrucous SCC, there is a notable bulkiness to the epithelial proliferation with voluminous acanthotic, exophytic, and endophytic-appearing columns that exhibit complex foldings and invaginations (Fig. 6a-f). The epithelial thickness is often more than 3–4 times the thickness of the adjacent uninvolved epithelium (Figs. 3b, c, 6a, and c). There are bulbous, blunt, downwardly-directed rete peg projections that may or may not extend below the level of the adjacent unaffected epithelium (Figs. 3c and 6c). The amount of keratosis is variable and parakeratosis rather than orthokeratosis is prominent in this category; however, unlike verrucous SCC, church spire-type hyperkeratosis is generally absent. The basement membrane in some instances may be intact similar to what is characteristic of VSCC. In other cases, there is blurring of the epithelial-stromal interface, whereby the epithelium appears to trickle into the markedly inflamed connective tissue, but still lacks definitive histopathological evidence of the destructive “invasion” seen in conventional SCC. The degree of cytologic atypia may be modest, yet architectural disorder is readily identified. Intraepithelial microabscesses intimately associated with keratin pearls, is another histologic indicator that favors a carcinoma diagnosis (Fig. 6b and d). Additionally, both intraepithelial and stromal infiltration by eosinophils commonly attends these particular carcinomas.
Fig. 6.
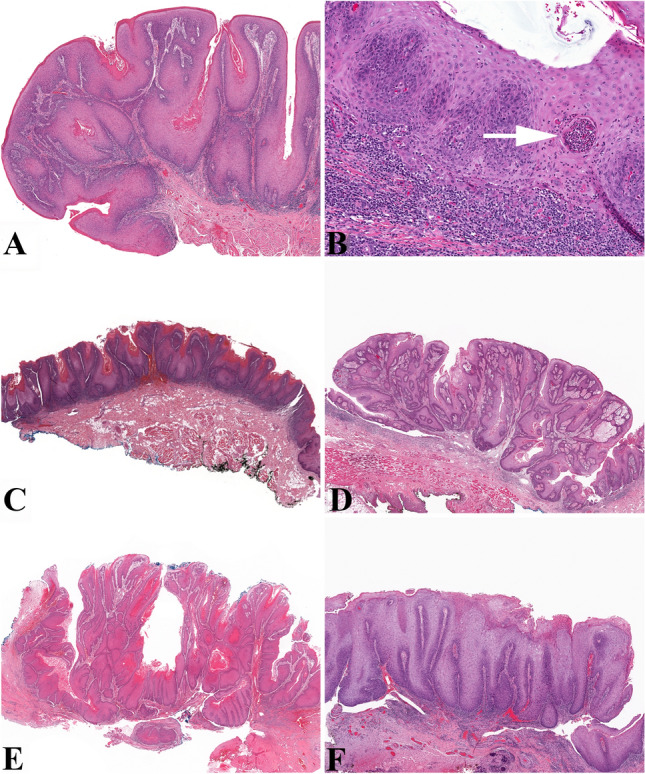
Features of barnaculate squamous cell carcinoma. a Low power shows acanthotic epithelium with both an exophytic and endophytic proliferation of complex foldings and invaginations of the epithelium. The epithelial rete pegs are bulbous, with variable keratosis extending deep into the epithelial folds. b The basement membrane is poorly demarcated. Other findings include an intraepithelial microabscess (white arrow), dyskeratosis, and inflammatory cell exocytosis. c This barnaculate carcinoma shows wide bulbous rete with associated hyperkeratosis, but is at the level of the adjacent epithelium, appearing “stuck on.” Inflammation is noted at the advancing edge. d The “stuck-on” appearance is easily identified, with a substantial endo- and exophytic appearance, but nearly all of the base of the lesion is at the same level without a significant “invasive” front. There is no church-spire keratosis, no significant keratosis, and no parakeratotic crypting. e This is an example of verrucous carcinoma, showing a predominantly exophytic growth pattern. The keratin plunges down into the epithelial crypts. This histology correlates well with the clinical presentation of a carpet-like proliferation of verrucous epithelium with fissuring. f This barnaculate carcinoma is characterized by a substantial and significant epithelial proliferation showing a nearly flat surface (rounded) with elongated and bulbous rete that all reach the same level, and does not show a significant or destructive invasion. In this case, the bulk of the proliferation is exophytic into the lumen
Just as Lauren Ackerman in 1948 described verrucous SCC as a previously unrecognized variant of SCC (Fig. 6e) [50], now, perhaps 40 years after Shear and Pindborg’s description of verrucous hyperplasia, the time has come to recognize a new variant of SCC of the oral cavity that is strongly associated with PVL. The term barnaculate carcinoma is suggested to highlight the neoplasm’s similarity to barnacles: a corpulent, bulky tumor without classical invasion or extension below the adjacent epithelium, showing numerous broad columns with surface keratin, behaving as a localized tumor mass but generally lacking significant metastatic potential. As this term is coined herein, confusion with other tumor types and names should be averted, recognizing that several different types of SCCs may be seen in the setting of PVL, but that the particular histologic features described here and ascribed to this tumor may lead to better management of the patient. Given the cases included here, none of them died of disease nor developed lymph node metastasis (mean 70 months of follow-up after carcinoma diagnosis). This is certainly preferable to giving the patient and treating clinician an indeterminate diagnosis, which is frequently the current practice. Additional research using the criteria herein provided for barnaculate carcinoma would provide further support and guidance about management.
It must be emphasized that disease progression is remarkably unpredictable. This observation generated debate as to whether the atypical epithelial findings in the bulky hyperkeratotic epithelial proliferation category reflect a stage in the lesion’s evolution to carcinoma or were actually consistent with an unequivocal carcinoma diagnosis. It seems this “intermediate” category most likely comprises two distinct subgroups of lesions: one that is primarily exophytic, with a corrugated or papillated surface and complex “papillary” lamina propria, in essence topographically barnacle-like and not obviously invasive; and another that is similar to verrucous SCC, in that it demonstrates both a verruciform, Christmas tree-keratotic surface configuration and markedly endophytic growth with blunt, downward-directed, occasionally confluent rete pegs, mild cytologic atypia, and plugged keratotic surface crypts. The latter lesion’s histomorphologic composite of atypical, “pushing” architectural pattern, and aberrant keratinization without evidence of invasion by individual nests or cells may actually represent a form of carcinoma that does not satisfy the criteria for verrucous carcinoma (spire-like hyperkeratosis, broad, bulbous, plunging rete pegs with parakeratin-filled crypts and clefts), SCC with papillary architecture, or conventional SCC, but is instead a carcinoma most likely unique to PVL. Clearly, there are unique carcinoma patterns described (such as “bluntly invasive well-differentiated SCC”), and so this subtype will represent an additional one recognized in the category.
Conclusions
In conclusion, it must be stated that no single case in this exercise was ever diagnosed uniformly in any one particular category. Thus, these criteria, while carefully considered and clarified, are recognized as being insufficient to classify all lesions unequivocally. There will continue to be differences in interpretation and diagnosis. Still, at the conclusion of the conference, cases which initially had diagnoses in all four of the respective categories during the surveys, now showed substantial to almost perfect agreement with > 80% concordance in an individual diagnostic category, whereas previously, the kappa statistic was 0.32 to 0.56. With time, familiarity with the terms and the features, and with daily application in practice, it is hoped that these terms can become better proxies for PVL lesions, and improve diagnostic accuracy of pathologists’ diagnosis, and thereby aid in standardizing patient management of a relentless clinical disease. While not the focus of this white paper which was developed to harmonize and standardize diagnostic criteria, it is hoped we have provided the structural scaffolding for further and on-going investigation into the biologic and genetic findings of this disorder to potentially guide treatment in the future. It is a glaring admission that with all of the work achieved thus far, relatively little is reported on molecular pathways and biologic factors that may be seen in PVL.
In summary:
What are the important differential diagnostic considerations of PVL? The most important lesions include oral lichen planus, traumatic hyperkeratosis, alveolar ridge hyperkeratosis, tobacco pouch keratosis, and unifocal dysplasia.
Are there consistent histopathological features that correlate with the range of clinical manifestations of PVL lesions? If so, what are they and can they be systematically categorized? Yes, there are features as detailed extensively above that should make a pathologist suspicious they are dealing with a PVL lesion, and although it is impossible in every case to distinctly separate lesions found on a continuum, these broad categories provide a good framework.
Is there a reproducible or predictable clinical-pathological continuum that characterizes the development of PVL lesions? Within certain limitations, we have shown architectural findings that often are more important than atypical cytologic features; they can begin as atrophic lesions and become bulky as they develop, and can show a pattern of invasion similar to verrucous SCC with a broad pushing but not infiltrative front.
Can an individual PVL lesion’s histopathological findings reliably predict progression to carcinoma? Although the answer is possibly yes at present, with further genetic and progression studies, we may be able to more accurately determine a risk progression model to predict behavior and thereby influence management.
Acknowledgements
Statistical analysis of inter-rater agreement was provided by Sijia Yue, MS at the University of Florida College of Public Health and Health Professions Department of Biostatistics.
Funding
No external funding was obtained for this study, with support from institutional review boards and the sponsoring societies.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this retrospective data analysis involving human participants were in accordance with the ethical standards of the institutional review board, which did not require informed consent.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lester D. R. Thompson and Sarah G. Fitzpatrick share equal authorship contribution.
References
- 1.Upadhyaya JD, Fitzpatrick SG, Islam MN, et al. Marginal linear gingival leukoplakia progressing to “ring around the collar”—an ominous sign of proliferative verrucous leukoplakia. J Periodontol. 2020 doi: 10.1002/jper.19-0621. [DOI] [PubMed] [Google Scholar]
- 2.Hansen LS, Olson JA, Silverman S. Proliferative verrucous leukoplakia. A long-term study of thirty patients. Oral Surg Oral Med Oral Pathol. 1985;60(3):285–98. doi: 10.1016/0030-4220(85)90313-5. [DOI] [PubMed] [Google Scholar]
- 3.Cabay RJ, Morton TH, Jr, Epstein JB. Proliferative verrucous leukoplakia and its progression to oral carcinoma: a review of the literature. J Oral Pathol Med. 2007;36(5):255–61. doi: 10.1111/j.1600-0714.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- 4.Silverman S, Jr, Gorsky M. Proliferative verrucous leukoplakia: a follow-up study of 54 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84(2):154–7. doi: 10.1016/s1079-2104(97)90062-7. [DOI] [PubMed] [Google Scholar]
- 5.Bagan JV, Murillo J, Poveda R, et al. Proliferative verrucous leukoplakia: unusual locations of oral squamous cell carcinomas, and field cancerization as shown by the appearance of multiple OSCCs. Oral Oncol. 2004;40(4):440–3. doi: 10.1016/j.oraloncology.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Feller L, Wood NH, Raubenheimer EJ. Proliferative verrucous leukoplakia and field cancerization: report of a case. J Int Acad Periodontol. 2006;8(2):67–70. [PubMed] [Google Scholar]
- 7.Upadhyaya JD, Fitzpatrick SG, Islam MN, Bhattacharyya I, Cohen DM. A retrospective 20-year analysis of proliferative verrucous leukoplakia and its progression to malignancy and association with high-risk human papillomavirus. Head Neck Pathol. 2018;12(4):500–10. doi: 10.1007/s12105-018-0893-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Upadhyaya JD, Fitzpatrick SG, Cohen DM, et al. Inter-observer variability in the diagnosis of proliferative verrucous leukoplakia: clinical implications for oral and maxillofacial surgeon understanding: a collaborative pilot study. Head Neck Pathol. 2020;14(1):156–65. doi: 10.1007/s12105-019-01035-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cerero-Lapiedra R, Balade-Martinez D, Moreno-Lopez LA, Esparza-Gomez G, Bagan JV. Proliferative verrucous leukoplakia: a proposal for diagnostic criteria. Med Oral Patol Oral Cir Bucal. 2010;15(6):e839–45. [PubMed] [Google Scholar]
- 10.Carrard VC, Brouns ER, van der Waal I. Proliferative verrucous leukoplakia; a critical appraisal of the diagnostic criteria. Med Oral Patol Oral Cir Bucal. 2013;18(3):e411–3. doi: 10.4317/medoral.18912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fleiss JL. Statistical Methods for Rates and Proportions. London: Wiley; 1981. [Google Scholar]
- 12.Villa A, Menon RS, Kerr AR, et al. Proliferative leukoplakia: proposed new clinical diagnostic criteria. Oral Dis. 2018;24(5):749–60. doi: 10.1111/odi.12830. [DOI] [PubMed] [Google Scholar]
- 13.Karabulut A, Reibel J, Therkildsen MH, et al. Observer variability in the histologic assessment of oral premalignant lesions. J Oral Pathol Med. 1995;24(5):198–200. doi: 10.1111/j.1600-0714.1995.tb01166.x. [DOI] [PubMed] [Google Scholar]
- 14.Abbey LM, Kaugars GE, Gunsolley JC, et al. Intraexaminer and interexaminer reliability in the diagnosis of oral epithelial dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(2):188–91. doi: 10.1016/s1079-2104(05)80201-x. [DOI] [PubMed] [Google Scholar]
- 15.van der Meij EH, Reibel J, Slootweg PJ, et al. Interobserver and intraobserver variability in the histologic assessment of oral lichen planus. J Oral Pathol Med. 1999;28(6):274–7. doi: 10.1111/j.1600-0714.1999.tb02038.x. [DOI] [PubMed] [Google Scholar]
- 16.Fischer DJ, Epstein JB, Morton TH, Schwartz SM. Interobserver reliability in the histopathologic diagnosis of oral pre-malignant and malignant lesions. J Oral Pathol Med. 2004;33(2):65–70. doi: 10.1111/j.1600-0714.2004.0037n.x. [DOI] [PubMed] [Google Scholar]
- 17.Kujan O, Khattab A, Oliver RJ, et al. Why oral histopathology suffers inter-observer variability on grading oral epithelial dysplasia: an attempt to understand the sources of variation. Oral Oncol. 2007;43(3):224–31. doi: 10.1016/j.oraloncology.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 18.Manchanda A, Shetty DC. Reproducibility of grading systems in oral epithelial dysplasia. Med Oral Patol Oral Cir Bucal. 2012;17(6):e935–42. doi: 10.4317/medoral.17749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geetha KM, Leeky M, Narayan TV, Sadhana S, Saleha J. Grading of oral epithelial dysplasia: points to ponder. J Oral Maxillofac Pathol. 2015;19(2):198–204. doi: 10.4103/0973-029X.164533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Speight PM, Abram TJ, Floriano PN, et al. Interobserver agreement in dysplasia grading: toward an enhanced gold standard for clinical pathology trials. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):474–82. doi: 10.1016/j.oooo.2015.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krishnan L, Karpagaselvi K, Kumarswamy J, et al. Inter- and intra-observer variability in three grading systems for oral epithelial dysplasia. J Oral Maxillofac Pathol. 2016;20(2):261–8. doi: 10.4103/0973-029X.185928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.B RSA, Hegde NP, et al. Inter- and intra-observer variability in diagnosis of oral dysplasia. Asian Pac J Cancer Prev. 2017;18(12):3251–4. doi: 10.22034/APJCP.2017.18.12.3251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zain RB, Kallarakkal TG, Ramanathan A, et al. Exophytic verrucous hyperplasia of the oral cavity—application of standardized criteria for diagnosis from a consensus report. Asian Pac J Cancer Prev. 2016;17(9):4491. doi: 10.7314/APJCP.2016.17.(9).4491. [DOI] [PubMed] [Google Scholar]
- 24.Müller S. Oral epithelial dysplasia, atypical verrucous lesions and oral potentially malignant disorders: focus on histopathology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125(6):591–602. doi: 10.1016/j.oooo.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 25.Müller S. Oral lichenoid lesions: distinguishing the benign from the deadly. Mod Pathol. 2017;30(s1):S54–S67. doi: 10.1038/modpathol.2016.121. [DOI] [PubMed] [Google Scholar]
- 26.Cheng YS, Gould A, Kurago Z, Fantasia J, Muller S. Diagnosis of oral lichen planus: a position paper of the American Academy of Oral and Maxillofacial Pathology. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;122(3):332–54. doi: 10.1016/j.oooo.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Mignogna MD, Fortuna G, Leuci S, et al. Frictional keratoses on the facial attached gingiva are rare clinical findings and do not belong to the category of leukoplakia. J Oral Maxillofac Surg. 2011;69(5):1367–74. doi: 10.1016/j.joms.2010.05.087. [DOI] [PubMed] [Google Scholar]
- 28.Woo SB, Lin D. Morsicatio mucosae oris—a chronic oral frictional keratosis, not a leukoplakia. J Oral Maxillofac Surg. 2009;67(1):140–6. doi: 10.1016/j.joms.2008.08.040. [DOI] [PubMed] [Google Scholar]
- 29.Müller S. Frictional keratosis, contact keratosis and smokeless tobacco keratosis: features of reactive white lesions of the oral mucosa. Head Neck Pathol. 2019;13(1):16–24. doi: 10.1007/s12105-018-0986-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Woo SB, Grammer RL, Lerman MA. Keratosis of unknown significance and leukoplakia: a preliminary study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118(6):713–24. doi: 10.1016/j.oooo.2014.09.016. [DOI] [PubMed] [Google Scholar]
- 31.Almazyad A, Li CC, Woo SB. Benign alveolar ridge keratosis: clinical and histopathologic analysis of 167 cases. Head Neck Pathol. 2020;14(4):915–922. doi: 10.1007/s12105-020-01151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Natarajan E, Woo SB. Benign alveolar ridge keratosis (oral lichen simplex chronicus): a distinct clinicopathologic entity. J Am Acad Dermatol. 2008;58(1):151–7. doi: 10.1016/j.jaad.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 33.Chi AC, Lambert PR, Pan Y, et al. Is alveolar ridge keratosis a true leukoplakia?: A clinicopathologic comparison of 2,153 lesions. J Am Dent Assoc. 2007;138(5):641–51. doi: 10.14219/jada.archive.2007.0236. [DOI] [PubMed] [Google Scholar]
- 34.Rosebush MS, Briody AN, Cordell KG. Black and brown: non-neoplastic pigmentation of the oral mucosa. Head Neck Pathol. 2019;13(1):47–55. doi: 10.1007/s12105-018-0980-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Behura SS, Masthan MK, Narayanasamy AB. Oral mucosal lesions associated with smokers and chewers—a case–control study in chennai population. J Clin Diagn Res. 2015;9(7):Zc17–22. doi: 10.7860/JCDR/2015/14008.6169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saraswathi TR, Ranganathan K, Shanmugam S, et al. Prevalence of oral lesions in relation to habits: cross-sectional study in South India. Indian J Dent Res. 2006;17(3):121–5. doi: 10.4103/0970-9290.29877. [DOI] [PubMed] [Google Scholar]
- 37.van der Waal I. Potentially malignant disorders of the oral and oropharyngeal mucosa; terminology, classification and present concepts of management. Oral Oncol. 2009;45(4–5):317–23. doi: 10.1016/j.oraloncology.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 38.Fitzpatrick SG, Honda KS, Sattar A, Hirsch SA. Histologic lichenoid features in oral dysplasia and squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(4):511–20. doi: 10.1016/j.oooo.2013.12.413. [DOI] [PubMed] [Google Scholar]
- 39.Iocca O, Sollecito TP, Alawi F, et al. Potentially malignant disorders of the oral cavity and oral dysplasia: a systematic review and meta-analysis of malignant transformation rate by subtype. Head Neck. 2020;42(3):539–55. doi: 10.1002/hed.26006. [DOI] [PubMed] [Google Scholar]
- 40.Woo SB. Oral epithelial dysplasia and premalignancy. Head Neck Pathol. 2019;13(3):423–39. doi: 10.1007/s12105-019-01020-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Akrish S, Eskander-Hashoul L, Rachmiel A, Ben-Izhak O. Clinicopathologic analysis of verrucous hyperplasia, verrucous carcinoma and squamous cell carcinoma as part of the clinicopathologic spectrum of oral proliferative verrucous leukoplakia: a literature review and analysis. Pathol Res Pract. 2019;215(12):152670. doi: 10.1016/j.prp.2019.152670. [DOI] [PubMed] [Google Scholar]
- 42.Capella DL, Gonçalves JM, Abrantes AAA, Grando LJ, Daniel FI. Proliferative verrucous leukoplakia: diagnosis, management and current advances. Braz J Otorhinolaryngol. 2017;83(5):585–93. doi: 10.1016/j.bjorl.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Celentano A, Glurich I, Borgnakke WS, Farah CS. World Workshop on Oral Medicine VII: Prognostic biomarkers in oral leukoplakia and proliferative verrucous leukoplakia—A systematic review of retrospective studies. Oral Dis. 2020 doi: 10.1111/odi.13363. [DOI] [PubMed] [Google Scholar]
- 44.Pentenero M, Meleti M, Vescovi P, Gandolfo S. Oral proliferative verrucous leucoplakia: are there particular features for such an ambiguous entity? A systematic review. Br J Dermatol. 2014;170(5):1039–47. doi: 10.1111/bjd.12853. [DOI] [PubMed] [Google Scholar]
- 45.Gillenwater AM, Vigneswaran N, Fatani H, Saintigny P, El-Naggar AK. Proliferative verrucous leukoplakia: recognition and differentiation from conventional leukoplakia and mimics. Head Neck. 2014;36(11):1662–8. doi: 10.1002/hed.23505. [DOI] [PubMed] [Google Scholar]
- 46.Davidova LA, Fitzpatrick SG, Bhattacharyya I, Cohen DM, Islam MN. Lichenoid characteristics in premalignant verrucous lesions and verrucous carcinoma of the oral cavity. Head Neck Pathol. 2019;13(4):573–9. doi: 10.1007/s12105-019-01006-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Montague LJ, Bhattacharyya I, Islam MN, Cohen DM, Fitzpatrick SG. Direct immunofluorescence testing results in cases of premalignant and malignant oral lesions. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119(6):675–83. doi: 10.1016/j.oooo.2015.02.478. [DOI] [PubMed] [Google Scholar]
- 48.González-Moles M, Ruiz-Ávila I, González-Ruiz L, et al. Malignant transformation risk of oral lichen planus: a systematic review and comprehensive meta-analysis. Oral Oncol. 2019;96:121–30. doi: 10.1016/j.oraloncology.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 49.Shear M, Pindborg JJ. Verrucous hyperplasia of the oral mucosa. Cancer. 1980;46(8):1855–62. doi: 10.1002/1097-0142(19801015)46:8<1855::aid-cncr2820460825>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 50.Ackerman LV. Verrucous carcinoma of the oral cavity. Surgery. 1948;23(4):670–8. [PubMed] [Google Scholar]


