Abstract
OBJECTIVE
To assess the effect of a supportive educational intervention on the psychological wellbeing of mothers whose babies were admitted to Neonatal Care Unit (NCU) in Nigeria.
METHODS
Controlled trial involving 41 mothers whose babies were consecutively admitted into two NCUs (21 in the intervention group and 19 controls). The intervention group received two group-based sessions which included psychological coping strategies, and familiarity with NCU environment, equipment, personnel and procedures. The control group received usual care. Outcome measures were depressive symptoms (Edinburg Postnatal Depression Scale—EPDS), stress-related to NCU (Parental Stressor Scale: Neonatal Intensive Care Unit—PSS: NICU) and post-traumatic symptoms (Impact Event Scale-Revised—IES-R).
RESULTS
Difference-in-Differences (DiD) analysis showed a difference of −4.70 in PSS: NICU score in favour of the intervention group which was statistically significant [F(3, 75) = 9.47, p < 0.0001, R2 = 0.28]. The differences in EPDS (0.91) and IES-R (2.55) were not statistically significant [F(3, 75) = 10.10, p = 0.74] and [F(3, 75) = 10.13, p = 0.73], respectively. All the mothers in the treatment group expressed satisfaction with the intervention.
CONCLUSION
This brief group-based supportive educational intervention for mothers with babies in NCU was feasible, acceptable and helpful in reducing stress related to NCU. Larger controlled trials are recommended to establish the generalizability of these findings in this region.
LAY SUMMARY
Babies born too early and or with complications require admission to special hospital called Neonatal Care Unit (NCU) to help them to survive. However, parents whose babies are admitted to NCU can find the experience frightening. We examined how to reduce the fear and stress mothers in Nigeria experience when their babies are admitted to NCU.
We had two groups of mothers. The first group made up of 21 mothers was taught how to cope with the stress of having a baby in NCU. They were also shown how the various equipment in the NCU work, what the staff in NCU do and what types of things need to be done to help their babies. The second group of 19 mothers received usual care but did not have the extra teaching the first group received. After 2 weeks, we checked the level of depression and stress the mothers in both groups had compared with the level before the first group received the extra teaching.
We found that mothers in the first group who received the extra teaching were less stressed about having their babies in the NCU compared with the mothers that did not receive the teaching.
Keywords: neonatal intensive care unit (NCU), post-natal depression, parental stress, educational intervention, supportive counselling
INTRODUCTION
Fifteen million babies are born prematurely every year and Nigeria has the third highest number of premature births in the world [1]. Prematurity accounts for 1 million deaths annually [2] making it a leading cause of under-five mortality. Also, the surviving premature babies are at increased risk of medical and developmental complications associated with long term learning disabilities, hearing and visual impairments [3]. Specialist care in Neonatal Care Units (NCU) can greatly improve the survival of babies born pre-term. Low cost options such as Kangaroo mother care can also be helpful in regions with limited access to NCU [4]. In addition to prematurity, new born babies can also require admission to NCU due to respiratory distress syndrome, sepsis, hypoglycaemia, jaundice and asphyxia [5].
Parents who are not used to NCU are likely to find the environment ‘unusual’ and even frightening [6]. This potentially distressing experience can occur for the following reasons [7]. First, the atypical appearance of the preterm infant can challenge the parent’s pre-birth expectations. Second, the sight of babies in incubators or on mechanical ventilators and the acute realization of the baby’s vulnerability can be distressing to parents. Third, the frequent and varied sounds of monitors can be disconcerting for parents who being unfamiliar with the significance may assume the worst with each beep. Fourth, the baby’s admission is often unexpected which means there is little time to prepare parents for the experience. Finally, parents may feel inadequate because a large proportion of their baby’s care is being provided by medical and nursing staff who may be too busy to involve the parents. In countries like Nigeria where some of the cost of NCU care has to be funded out-of-pocket, the unexpected financial burden can be a further stress for the family [8]. Thus some parents whose babies are admitted to NCU may have difficulties coping with these stressful experiences; hence a recent systematic review [7] found increased prevalence of anxiety, depression and post-traumatic stress disorder among such parents. These findings indicate the need for psychosocial support tailored towards the unique situation of parents whose babies are admitted to NCU [9].
Systematic reviews have shown that a range of psychosocial interventions can reduce distress and depression among mothers or both parents whose babies are admitted to NCU [9, 10]. These systematic reviews examined studies that varied in terms of modality of intervention, delivery by professionals or by peer mentors, in group or individual formats, focused on mothers or both parents, and duration. The review by Mendelson, et al. [10] used narrow selection criteria to identify 12 studies. They found that cognitive behavioural therapy (CBT) was effective in reducing maternal depressive symptoms but not anxiety. On the other hand, Sabnis, et al. [9] used broader criteria and included 23 randomized and 10 non-randomized studies in their review. They found that studies that included an educational component significantly reduced parental distress. The aims of educational intervention include helping parents to become familiar with the NCU environment, equipment and the essentials of neonatal care. This educational component addresses the element of ‘fear of the unknown’ about the NCU environment. It has been postulated that ‘fear of the unknown’ is the fundamental basis for anxiety disorders [11].
Despite the high prevalence of premature births in Africa, there is limited research on the psychosocial needs of parents with babies in NCU and interventions to support them [12]. A scoping survey of clinicians providing neonatal services in Nigeria identified a range of medical expertise and interventions but did not mention psychosocial support [13]. Also, none of the studies reviewed by Mendelson, et al. [10] or Sabnis, et al. [9] was from Africa. The severe lack of material and human resources in sub-Saharan Africa, coupled with huge infrastructural challenges all suggest that interventions that are effective in other countries may not be feasible or scalable in the region. Tackling this huge knowledge-gap about potentially helpful interventions in Africa will require large scale studies. However, such studies need to be preceded by smaller feasibility studies to scope important factors such as the potentially helpful components, duration and acceptability of such interventions, as well as the reliability of potential outcome measures. This study aimed to start fillings these gaps by evaluating the feasibility and effect of a brief educational and supportive intervention for mothers whose babies were admitted to an NCU in a Tertiary Hospital in South-western Nigeria. Given the severe resource limitation in Nigeria, studies in the region require short, easy-to-complete but reliable outcome measures. Therefore, this study also assessed the potential usefulness of a very short subscale of a measure of stress associated with NCU [Parental Stressor Scale—Neonatal Intensive Care Unit (PSS: NICU)] [14]. Although the stress of NCU admission can affect both mothers and fathers, the current study focused on mothers because they provide the bulk of newborn care in Nigeria [15].
METHODS
Study design and location
This was a controlled two-group intervention study conducted in two NCUs at the University College Hospital (UCH), Ibadan, Nigeria. Ibadan is the third most populous metropolis in Nigeria with a population of 5 million. The UCH is the oldest University Teaching Hospital in Nigeria. It is a tertiary referral centre for primary and secondary health facilities in a large region of South-western Nigeria. The hospital admits pre-term babies into one of two Wards namely, Special Care Baby Unit (SCBU) which admits babies born in UCH within 24 − 48 h, and C12nd Ward which admits newborns delivered outside UCH. Both wards can admit up to 20 babies and they provide similar levels and acuity of neonatal care including ventilatory support. The average duration of admission is 2 weeks. Ethical approval was given by the University of Ibadan/University College Hospital Institutional Review Board.
Participants
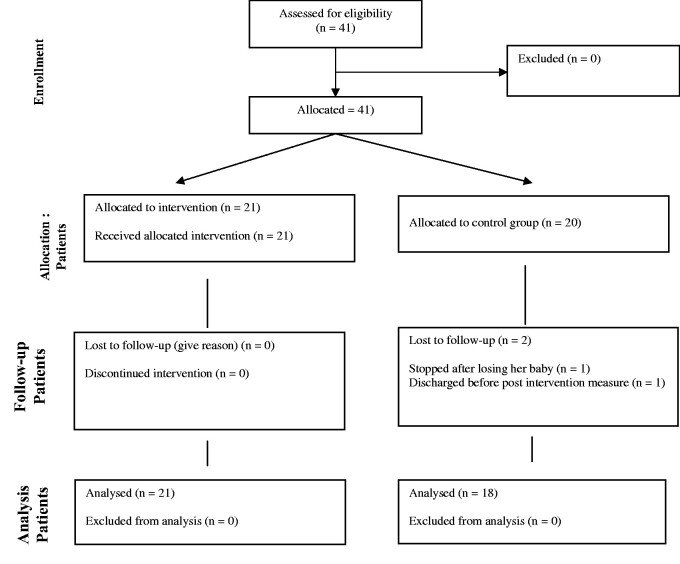
Participants were mothers above 18 years of age whose babies were admitted into the NCU in the preceding 48 h. Consenting mothers whose babies were admitted to the SCBU Ward were the intervention group while mothers of babies in C12nd Ward were controls. The respective Wards were randomly assigned to ‘intervention’ or ‘control’ by balloting. Consecutive admissions that met the inclusion criteria were recruited until the target sample of 20 mothers in each group was reached. A sample of 16 in each group was calculated a priori as adequate to detect a reduction of one standard deviation in maternal stress in the intervention group compared with the control group with 80% power and 5% two-sided alpha [16]. This was increased to 20 in each group to account for potential attrition. The plan was to exclude mothers who were medically unstable, severely depressed or psychotic, but none of the eligible mothers had these problems. Similarly, no mothers declined consent. For the intervention ward, two mothers consented simultaneously to be the 20th participant. Thus, both mothers were recruited to avoid disappointing either of them. One mother in the control group was discharged shortly after recruitment and before completing the baseline measures. A second mother in the control group lost her baby before completing the post-intervention measures. She was therefore excluded to allow her to grieve. Thus, the baseline sample consisted of 21 mothers in the intervention group and 19 mothers in the control group. Twenty-one mothers in the intervention group and 18 controls completed the post-intervention measures (Fig. 1).
Fig. 1.
CONSORT flow diagram of study participants.
Procedure
Intervention
This was a manualized intervention delivered by the first author and supervised by the other authors. The intervention was delivered in groups of five mothers per session. The content had a core of supportive and educational framework intended to de-mystify the NCU environment for the mothers. The intervention was developed by merging evidence from the literature and the lived-experience of three parents with previous experience of NCU admission for their babies. These parents were not part of the current study.
The first session involved introductions and ground rules. This was followed by explanation of the equipment and environment in the NCU. The themes covered included functions of the incubator and other equipment, staff of the NCU, procedures (e.g. venipuncture), characteristics of premature infants (e.g. appearance, behaviour and physical signs), possible fears and worries of parents during their infant's hospitalization, and methods of participation in their infant’s care (e.g. kangaroo mother care). The first session was also used to discuss problem-solving techniques and self-care strategies for the mothers. The mothers were encouraged to identify and use coping self-talks. The latter included religious-based coping talks which were encouraged to reflect the existing high level of religious coping in the culture [17, 18]. The session lasted 60 min. At the end of the session, the mothers were encouraged to practice the self-care and self-talk strategies discussed before the next session.
The second session which took place a week later was used to reinforce the themes discussed in the first session. The session was also used to problem-solve specific difficulties interfering with the mothers’ ability to practice the strategies discussed in the first session. The outcome measures were re-administered to both groups immediately after the intervention group completed the second session. The intervention was limited to two sessions because babies are admitted to the neonatal wards for an average duration of 2 weeks. The post-intervention measures were completed after the second session in order to avoid ‘loss to follow up’ as many infants were discharged shortly after. The option of obtaining a second post-intervention measure was not viable because it would have required community follow-up of discharged infants/mothers which was not feasible due to time and logistical constraints.
The outcome measures were translated into Yoruba which is the local language in the area. The translation was carried out by a qualified linguist at University of Ibadan using iterative back translation procedure. A trained research assistant who was blinded to group-assignment supported the administration of the outcome measures.
Measures
Sociodemographic questionnaire
This was adapted from a sociodemographic questionnaire previously used in the setting [19]. The questionnaire sought background characteristics and medical information as shown in Table 1. In line with previous studies in Nigeria [18, 20, 21], ownership of valued household possessions was used to create a ‘wealth rating’ as surrogate for socioeconomic status.
Table 1.
Background characteristics of mothers in the intervention group and control group
| Variables | Intervention group N (%) or mean (SD) N = 21 | Control group N (%) or mean (SD) N = 19 | p value | |
|---|---|---|---|---|
| Years of marriage | ||||
| 2 years and below | 6 (30.0) | 9 (45.0) | 0.96 | 0.33 |
| >2 years | 14 (70.0) | 11 (55.0) | ||
| Mother’s level of education | ||||
| Secondary and below | 11 (55.0) | 6 (30.0) | 2.56 | 0.11 |
| More than secondary | 9 (45.0) | 14 (70.0) | ||
| Mother’s occupation | ||||
| Artisan | 5 (25.0) | 7 (35.0) | 7.41 | 0.06 |
| Civil servant | 0 (0.0) | 4 (20.0) | ||
| Trader | 8 (40.0) | 5 (25.0) | ||
| Others | 7 (35.0) | 4 (20.0) | ||
| Spouses’ level of education | ||||
| Secondary and below | 7 (35.0) | 6 (30.0) | 0.11 | 0.74 |
| More than Secondary | 13 (65.0) | 14 (70.0) | ||
| Spouses’ occupation | ||||
| Artisan | 6 (30.0) | 6 (30.0) | 0.23 | 0.97 |
| Civil servant | 5 (25.0) | 5 (25.0) | ||
| Trader | 3 (15.0) | 4 (20.0) | ||
| Others | 6 (30.0) | 5 (25.0) | ||
| Age at first pregnancy | ||||
| ≤20 years | 4 (20) | 4 (20) | 0.00 | 1.00 |
| >20 years | 16 (80) | 16 (80) | ||
| Parity (mean, SD) | 2.38 (1.28) | 1.79 (0.92) | 1.66 (38) | 0.11 |
| Mental health difficulty during pregnancy | ||||
| Yes | 3 (15) | 5 (25) | 0.63 | 0.43 |
| No | 17 (85) | 15 (75) | ||
| Mode of delivery | ||||
| Vaginal | 13 (62) | 14 (73.6) | 0.11 | 0.74 |
| Caesarean section | 8 (38) | 5 (26.3) |
Edinburg Postnatal Depression Scale
This is a ten-item self-report scale used to measure the level of depression in the postpartum period with a cut-off of 11 and above considered significant [22]. Respondents selected one of four possible answers that were closest to how they felt during the past week. Responses were scored 0, 1, 2 and 3 (reversed for some items), and summed. The Edinburg Postnatal Depression Scale (EPDS) has been standardized among Nigerian women [23]. The internal consistency in the current study was good (Cronbach’s α 0.84).
Impact of Event Scale—Revised (IES-R)
The Impact of Event Scale—Revised (IES-R) [24] assesses subjective distress following a potentially traumatic event which in this study is birth of a child requiring admission to NCU. It consists of 22 items divided into 3 clusters (‘avoidance’, ‘intrusion’ and ‘hyperarousal’) and rated on a five-point Likert scale ranging from 0 (not at all) to 4 (extremely) [24]. The IES-R has been used previously in Nigeria [25], and the internal consistencies for the sub-scales in the current study were good (Cronbach’s α 0.79, 0.70 and 0.82).
PSS: NICU (sight and sounds subscale)
The full PSS: NICU is a long instrument with three subscales namely, ‘Parental Role Alterations’, ‘Infant Behaviour and Appearance’, and ‘Sights and Sounds of the Unit’ [14]. However, the current study required, a short, easy-to-complete measure of NCU-related stress. Thus, a panel of a neonatologist, a neonatal nurse and a child psychiatrist reviewed the PSS: NICU and recommended adoption of the five-item ‘Sight and Sounds’ subscale for this study as it has the most face validity and closest match with the content of the intervention. The items in the subscale are (i) seeing many monitors and equipment; (ii) hearing regular/common sounds made by monitors and equipment; (iii) seeing sick babies; (iv) hearing sudden ‘alarm’ noises and (v) seeing large numbers of nurses and doctors. A sixth item ‘seeing babies using a ventilator/machine to breathe’ was added to reflect the fact that this is an uncommon and potentially disconcerting sight for the average parent in that setting. Each item was rated on a four-point Likert scale (1 = not worried, 2 = a bit worried, 3 = very worried and 4 = frightened). The internal consistency of this instrument in the current study was good (Cronbach’s α 0.85).
Client satisfaction questionnaire
Participants in the intervention group were asked to indicate how satisfied or dis-satisified they were with the intervention [26]. They were further asked three open-ended questions to elicit what they liked or did not like about the intervention and their suggestions for improvement. The qualitative comments were analysed thematically.
Data management
These data were analysed using SPSS version 22. Categorical variables were presented as frequencies and percentages. EPDS, IES-R and PSS: NICU scores were summarized using Means and Standard Deviations. Between-group differences were examined with t-test for continuous variables and Chi-square test for categorical variables. Difference-in-Differences (DiD) analysis [27] was used to determine the treatment effect on EPDS, IES-R and PSS: NICU scores because individual participants were neither randomized to the intervention or control groups nor assigned based on similar baseline scores. Linear regression was used to assess the statistical significance of the calculated DiD for each outcome. Level of significance was set at 0.05 two-tailed.
RESULTS
Sociodemographic and clinical characteristics at baseline
The two groups were comparable in their sociodemographic and baseline clinical characteristics (Table 1). The mean ages for the intervention group and control groups were 31.55 (SD 5.88) years and 28.70 (SD 4.60), respectively, and was not statistically significantly different (t = 1.69, df = 38, p = 0.11). All mothers in both groups were married and most had been married for over 2 years. The intervention and control groups were similar in Parity [Mean 2.38 SD 1.28) vs. Mean 1.79 (SD 0.92), t = 1.66, df 38, p = 0.11], and in ‘wealth rating’ [Mean 5.15 (SD 3.05) vs. Mean 4.95 (SD 2.86), t = 0.22, df 38, p = 0.83]. Baseline scores on the outcome measures were not statistically significantly different between the intervention and control groups, except for PSS: NICU scores which were higher among the intervention group (Table 2). At baseline, 29% of mothers in the intervention group scored 11 and above on the EPDS compared with 63% in the control group (Fisher’s Test p = 0.06).
Table 2.
Comparisons between intervention group and control group on outcome measures
| Intervention group (n = 21 at baseline and post-intervention) M (SD) |
Control group (n = 19 at baseline) (n = 18 at post-intervention) M (SD) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Baseline | Post | Difference | Baseline | Post | Difference | DiD (β) | F value (3.75) | p value |
| EPDS | 8.20 (6.86)a | 2.29 (2.95)d | 5.91 | 11.81 (5.50)a | 6.81 (6.63)d | 5.0 | −0.91 | 10.10 | 0.74 |
| IESR | 32.45 (17.46)b | 15.05 (9.05)e | 17.4 | 34.85 (13.12)b | 20.0 (14.9)e | 14.85 | −2.55 | 10.13 | 0.73 |
| PSS: NICU | 16.30 (5.78)c | 8.82 (3.74)f | 7.48 | 12.50 (5.83)c | 9.72 (4.73)f | 2.78 | −4.70 | 9.47 | 0.0001 |
T tests for between group comparisons at baseline and post-intervention.
t(df) = 1.83 (38), p = 0.08.
t(df) = 0.41 (38), p = 0.63.
t(df) = 2.07 (38), p = 0.05.
t(df) = 2.84 (37), p = 0.04.
t(df) = 1.20 (37), p = 0.26.
t(df) = 0.21 (37), p = 0.03.
In relation to the infants’ characteristics, babies born to mothers in the intervention group had significantly lower birth weight [Mean 1.92 (SD 0.77) vs. Mean 2.96 (SD 0.63), t = −4.59, df 38, p = 0.0001] and lower gestation age [Mean 32.23 (SD 4.56) vs. Mean 37.15 (SD 2.21), t = −4.38, df 38, p = 0.0001]. Other baby characteristics were similar between the intervention and control groups such as: ventilatory support (48% vs. 21%, Fisher’s test, p = 0.18), blood transfusion (48% vs. 58%, p = 0.53), jaundiced (85% vs. 56% p = 0.51), and duration of admission for <2 weeks (67% vs. 67%).
Effect of the intervention
The between-group comparison of post-intervention scores (Table 2) shows that the intervention group had significantly EPDS and PSS: NICU scores than the control group, but no significant difference in IES-R scores. However, for EPDS, no mother in the intervention group scored 11 or above while only 3 mothers in the control group did (p = 0.09). The DiD analysis used to ascertain treatment effect showed a DiD of −4.70 in PSS: NICU in favour of the intervention group. This DiD was statistically significant [F(3, 75) = 9.47, p < 0.0001, R2 = 0.28]. Controlling for birth weight improved the R2 to 0.30. The DiD for EPDS (−0.91) and IES-R (−2.55) were not statistically significant [F(3, 75) = 10.10, p = 0.74] and [F(3, 75) = 10.13, p = 0.73], respectively.
Client satisfaction with the intervention
All the mothers in the intervention group were ‘satisfied’ (70%) or very satisfied (30%) with the programme. The positive aspects of the intervention most frequently cited by the mothers were the explanation of the equipment in NCU (35% of all comments), and being taught coping strategies some of which re-enforced their existing religious coping (e.g. ‘counting your blessings’) (25% of all comments). The mothers’ suggestions for improving the intervention included making the sessions longer, having follow-up sessions post-discharge, and extending the intervention to their spouses.
DISCUSSION
This brief controlled educational and supportive intervention for mothers whose babies were admitted to NCU resulted in significant reduction in stress related to NCU in the intervention group. Also, the intervention was well received by the participants. The positive treatment effect based on DiD analysis indicate that the change was unlikely to be attributable to spontaneous improvement or regression to the mean. To the best of our knowledge, this is the first study of its kind in sub-Saharan Africa.
The findings of the current study are consistent with recent systematic reviews [9, 10] which showed that CBT and interventions that included education elements showed reductions in the stress experienced by parents with babies in NCU. The reduction in maternal stress directly related to NCU in the current study supports the hypothesis that helping the mothers to understand the unusual NCU environment could reduce the stress related to that setting [28]. Qualitative comments by the mothers in the current study provide further support for this hypothesis in that the most commonly reported positive aspect of the intervention was the explanation regarding the NCU equipment. These findings are thus consistent with the postulation that ‘fear of the unknown’ is fundamental to anxiety [11]. The fact that this successful intervention was brief, educational and reinforced pre-existing religious coping strategies suggest that it could be easier to deliver, and more affordable in LMICs where the human and material resources to support lengthy and complex interventions are limited.
As a feasibility study, one of the aims of the current study was to explore the possibility of using a very brief subscale of the PSS: NICU as an effective measure of stress related to NCU. The study showed that a modified six-item version of the original PSS-NICU measure was sensitive enough to identify a treatment difference despite the small sample size and brief duration of the intervention. Although this short subscale of the PSS: NICU has not been validated in Nigeria, the internal consistency in the current study (0.85) was good. This finding is encouraging because long and time-consuming outcome measures are of less practical use in resource-poor settings like Nigeria.
The intervention was hypothesized to reduce maternal post-partum depressive and post-traumatic stress symptoms but this was not the case. The absence of treatment effect on EPDS scores may be because the questionnaire was administered <2 weeks post-partum; hence it might have captured general distress and post-partum blues, rather than post-partum depression [22]. The null finding on IES-R scores could be because difficulties associated with birth and admission of a baby to NCU are perceived in this setting as not particularly ‘traumatic’. Furthermore, the intervention did not include specific strategies for managing post-traumatic symptoms. These null findings could also be Type II Errors due to the small sample size.
The strengths of the study include the quasi-experimental design with a control group, and the novelty of the intervention in this setting. However, the findings need to be interpreted with the following limitations in mind. First, participants were not individually randomized; hence there may be other unknown factors that are different between the two groups. Second, it was not possible to blind the participants although the research assistant who facilitated completion of outcome measures was blinded. Third, administration of EPDS within 2 weeks of birth may have captured general distress and post-partum blues rather than post-partum depression. Fourth, the short time scale for the post-intervention outcome measure means that sustainability of the treatment benefit is uncertain. Fifth, the small sample size limits the generalizability of the finding. Finally, the current intervention focused on mothers but it is recognized that fathers can also benefit and wish to be included [12].
CONCLUSION
This study suggests that group-based supportive and educational intervention for mothers with babies in NCU is feasible and acceptable in this setting. Also, the intervention reduced maternal stress related to NCU. Larger randomized controlled trials are recommended to establish the validity and generalizability of these findings in this region. Future studies should consider including fathers and use mixed-method approaches to also explore potential barriers and facilitators to wider implementation.
ACKNOWLEDGEMENTS
The authors thank the mothers who participated in the intervention, and the staff in the two NCUs who supported and facilitated the study.
FUNDING
This work was supported by the John D. and Catherine T. Mac-Arthur Foundation through the University of Ibadan Centre for Child and Adolescent Mental Health.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
REFERENCES
- 1. Chawanpaiboon S, Vogel JP, Moller AB, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health 2019;7:e37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet 2016;388:3027–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mwaniki MK, Atieno M, Lawn JE, et al. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet 2012;379:445–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chan GJ, Labar AS, Wall S, et al. Kangaroo mother care: a systematic review of barriers and enablers. Bull World Health Organ 2016;94:130–141J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Parkash J, Das N.. Pattern of admissions to neonatal unit. J Coll Physicians Surg Pak 2005;15:341–4. [PubMed] [Google Scholar]
- 6. Altimier L, Phillips R.. The neonatal integrative developmental care model: advanced clinical applications of the seven core measures for neuroprotective family-centered developmental care. Newborn Infant Nurs Rev 2016;16:230–44. [Google Scholar]
- 7. Loewenstein K. Parent psychological distress in the neonatal intensive care unit within the context of the social ecological model: a scoping review. J Am Psychiatr Nurses Assoc 2018;24:495–509. [DOI] [PubMed] [Google Scholar]
- 8. Enweronu-Laryea CC, Andoh HD, Frimpong-Barfi A, et al. Parental costs for in-patient neonatal services for perinatal asphyxia and low birth weight in Ghana. PloS One 2018;13:e0204410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sabnis A, Fojo S, Nayak SS, et al. Reducing parental trauma and stress in neonatal intensive care: systematic review and meta-analysis of hospital interventions. J Perinatol 2019;39:375–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mendelson T, Cluxton-Keller F, Vullo GC, et al. NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics 2017;139:e20161870. [DOI] [PubMed] [Google Scholar]
- 11. Carleton RN. Fear of the unknown: one fear to rule them all? J Anxiety Disord 2016;41:5–21. [DOI] [PubMed] [Google Scholar]
- 12. Opara PI, Alinnor EA.. Experiences of fathers of babies admitted into a neonatal unit in a tertiary hospital in Port Harcourt. JAMMR 2019;29. [Google Scholar]
- 13. Okonkwo IR, Abhulimhen-Iyoha BI, Okolo AA.. Scope of neonatal care services in major Nigerian hospitals. Nig J Paed 2016;43:8–13. [Google Scholar]
- 14. Miles MS, Funk SG, Carlson J.. Parental Stressor Scale: neonatal intensive care unit. Nurs Res 1993;42:148–52. [PubMed] [Google Scholar]
- 15. Iganus R, Hill Z, Manzi F, et al. Roles and responsibilities in newborn care in four African sites. Trop Med Int Health 2015;20:1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Noordzij M, Tripepi G, Dekker FW, et al. Sample size calculations: basic principles and common pitfalls. Nephrol Dial Transplant 2010;25:1388–93. [DOI] [PubMed] [Google Scholar]
- 17. Ani CC, Kinanee JO, Ola BO.. Psychological distress among trainee teachers in Nigeria: association with religious practice. Eur J Educ Stud 2011;3:163–72. [Google Scholar]
- 18. Bella‐Awusah T, Ani C, Ajuwon A, et al. Effectiveness of brief school‐based, group cognitive behavioural therapy for depressed adolescents in south west Nigeria. Child Adolesc Ment Health 2016;21:44–50. [DOI] [PubMed] [Google Scholar]
- 19. Omigbodun O, Dogra N, Esan O, et al. Prevalence and correlates of suicidal behaviour among adolescents in southwest Nigeria. Int J Soc Psychiatry 2008;54:34–46. [DOI] [PubMed] [Google Scholar]
- 20. Ani CC, Grantham-McGregor S.. Family and personal characteristics of aggressive Nigerian boys: differences from and similarities with Western findings. J Adolesc Health 1998;23:311–7. [DOI] [PubMed] [Google Scholar]
- 21. Ola B, Suren R, Ani C.. Depressive symptoms among children whose parents have serious mental illness: association with children’s threat related beliefs about mental illness. S Afr J Psych 2015;21:5– 8. [Google Scholar]
- 22. Levis B, Negeri Z, Sun Y, et al. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ 2020;2020:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adewuya AO, Ola BA, Dada AO, Fasoto OO.. Validation of the Edinburgh Postnatal Depression Scale as a screening tool for depression in late pregnancy among Nigerian women. J Psychosom Obstet Gynaecol 2006;27:267–72. [DOI] [PubMed] [Google Scholar]
- 24. Weiss DS, Marmar CR.. Assessing psychological trauma and PTSD. In: Wilson JP, Keane TM (eds). The Impact of Event Scale—Revised. New York: Guildford Press, 1997, 399–411. [Google Scholar]
- 25. Mosaku K, Akinyoola A, Olasinde A, et al. Predictors of posttraumatic stress in patients admitted to a trauma unit following road traffic accident (RTA). J Psychiatry 1997;17:121. [Google Scholar]
- 26. Attkisson C, Greenfield T.. The USCF client satisfaction scales: 1. The client satisfaction Questionnaire – 8. In: Maruish M (ed). The Use of Psychological Testing for Treatment Planning and Outcome Assessment, 3rd edn.Mahwah, NJ: Lawrence Erlbaum Associates, 2004, 799–812. [Google Scholar]
- 27. Wing C, Simon K, Bello-Gomez RA. (Designing difference in difference studies: best practices for public health policy research. Annu Rev Public Health 2018;39:453–69. [DOI] [PubMed] [Google Scholar]
- 28. Abdeyazdan Z, Shahkolahi Z, Mehrabi T, et al. A family support intervention to reduce stress among parents of preterm infants in neonatal intensive care unit. Iran J Nurs Midwifery Res 2014;19:349. [PMC free article] [PubMed] [Google Scholar]