In 2019, the pandemic induced by the rapid spread of the severe acute respiratory syndrome coronavirus-2 'SARS-CoV-2', also named coronavirus disease 'COVID-19', has rapidly caused serious health, economic, social, and political issues worldwide. This has been accentuated by asymptomatic carriers, fast viral mutations, incoherent lockdown policies, and limited methods of detection and treatment. Nucleic acid tests for COVID-19 are lengthy and complicated, and the rapid antibody tests produce false-negative diagnoses, particularly in the early stage of infection. Moreover, there are no specific and effective medicines available for treatment. Therefore, rapid diagnostics and therapeutics are urgently required. Here, we argue that nanozymes—enzyme-mimicking nanoparticles—could be used for faster, more sensitive, and accurate detection and treatment of the COVID-19. Indeed, nanozymes have high surface areas allowing easier bioconjugation for detection, and nanozymes possess integrated drug-functionalization for treatment. Moreover, the size, composition, and surface chemistry of nanozymes can be rationally designed for improved theranostic applications.
COVID-19 history
The COVID-19 appeared in Wuhan, China, due to emergence of a novel strain of coronavirus (Sallard et al. 2021), which was provisionally named ‘2019-nCoV’ by the World Health Organization (WHO). Later, the virus was renamed 'SARS-CoV-2' by the International Committee on Taxonomy of Viruses based on the phylogeny and taxonomy (Gorbalenya et al. 2020). Genetic analysis has confirmed the resemblance of the key genes of SARS-CoV-2 with other coronaviruses causing respiratory diseases (Zhou et al. 2020). Further, the genes of SARS-CoV-2 are undergoing frequent mutations, and several new variants have been reported: B.1.351 in South Africa, B.1.1.7 in the UK, B.1.427 and B.1.429 in the USA, and B.1.617 in India (Kemp et al. 2020). Moreover, a new strain S-614G showing increased replication, transmission and survival following a D614G substitution was recently identified (Zhou et al. 2021).
Due to rapid mutations, SARS-CoV-2 is displaying higher pathogenicity and virulence compared to previous strains, namely the severe acute respiratory syndrome (SARS) and the Middle East respiratory syndrome (MERS-CoV2, Paliwal et al. 2020). The rapid air transmission of the virus has induced the contagious spread, leading to the ongoing pandemic. This pandemic has been amplified by the potency of the virus to remain viable on surfaces for several hours, and in some cases several days (Sharma et al. 2020). The major symptoms of COVID-19 are variable, and the patients may have fever, headache, cough, fatigue, loss of smell and taste or breathing difficulties. After recovery, some patients still experience various adverse effects, including damage to organs due to inflammation, hypercoagulability, endotheliitis, vasoconstriction or oedema (Jain 2020). Since there is no effective and specific treatment for infected cases, prevention and vaccination are actually the sole means to control the pandemic.
Prevention and treatment
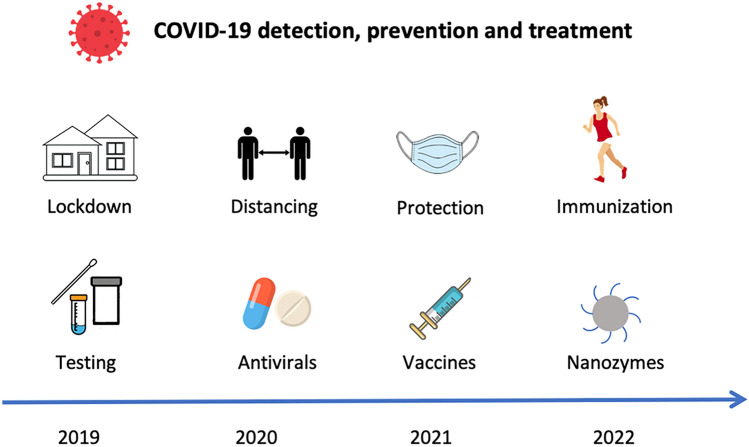
Numerous and sometimes contradictory policies have been issued by nations and health agencies to reduce transmission from infected persons to healthy individuals (Fig. 1). Policies include physical distancing of two meters, frequent hand washing, and personal hygiene, according to the US Centre of Disease Control and Prevention (CDC). These recommendations are based on respiratory studies carried out in 1930s (Shope 1931; Smith et al. 1933). Self-isolation has also been advocated for COVID-19 patients or infected suspects. Health agencies have provided directives for self-isolation and strict self-quarantine instructions to high-risk groups. Another policy was the use of personal protective equipment such as masks and respirators, in particular by healthcare professionals. Face coverings with masks are advised, in particular when social distancing is challenging to maintain, e.g. in transportations.
Fig. 1.
Approximate history of policies and means taken to decline the COVID-19 pandemic. Nanozymes are actually promising for detection, disinfection and treatment. Nanozymes are artificial enzymes made with nanomaterials (https://en.wikipedia.org/wiki/Artificial_enzyme)
Lockdown has also been imposed in many countries, yet strict lockdown of groups and families in densely populated cities has probably favoured viral transmission within families. In other words, lockdown has sometimes concentrated the population, and this is contradictory to physical distancing. In addition, ventilation and air filtration in hospitals and other public buildings have been recommended to clear out infectious aerosols. Lastly, improving immunity by eating nutritious food, doing daily physical activity, stress management and enough sleep are advised (Ibarra-Coronado et al. 2015; Dai et al. 2021). All these practices have found to be effective in controlling viral dissemination to some extent. Nonetheless, timely detection and specific medications are urgently needed.
Limits of actual diagnostics
Early diagnosis of any disease is crucial for an appropriate treatment, yet actual testing methods to identifying SARS-CoV-2 are limited. Table 1 compares diagnostic techniques which are currently applied for COVID-19 detection (Chakraborty et al. 2020). Here, it is challenging to develop effective diagnostics and therapeutics against SARS-CoV-2 due to the lack of validated biomarkers, frequent mutations, and unknown functional mechanisms of the virus (Paliwal et al. 2020). Nevertheless, diagnostic instrumentation such as single-photon emission computed tomography (SPECT) could be explored to diagnose the SARS-CoV-2 (Zavaleta et al. 2018). Several techniques such as L-surface plasmon resonance (LSPR) or field effector transition-based biosensing are available for detecting the viral load (Qiu et al. 2020; Seo et al. 2020). Similarly, there are few tests based on the molecular, immunological, clustered regularly interspaced short palindromic repeats (CRISPR) or serological methods with limit of detection ranging from 10 copies/µL to 100 copies/mL.
Table 1.
Available diagnostic methods for the detection of the coronavirus disease that has appeared in 2019 (COVID-19), their principle, assay time, advantages, constraints, and detection limits. Reprinted with permission from Chakraborty et al. (2020) under the Creative Commons Attribution License (CC BY)
| Method | Principle | Assay time | Advantage | Limitation | Detection limit |
|---|---|---|---|---|---|
| Reverse transcription polymerase chain reaction (RT-PCR) | Primer and fluorescent marker-based | 3–4 h | Reliable, detects current viral infection | Requires sophisticated instrument, and cannot detect already recovered patients | 100 copies/mL |
| Reverse transcription loop-mediated isothermal amplification (RT-LAMP) | Primer-based, two to three pairs of primer can be used | 2–3 h | Highly sensitive, conducted at constant temperature of 60–65 °C | Optimizing the primer and sample run | 80 copies of viral RNA/mL sample |
| Clustered regularly interspaced short palindromic repeats (CRISPR)-based assay | Gene editing | 1 h | Highly sensitive, low-resource settings | Many CRISPR kits are in the development stage and need more clinical validation | RT-LAMP/ Cas12 10 copies/µl input |
| Serological assay, enzyme-linked immunosorbent assay, neutralizing, chemiluminescent immunoassay | Antigen–antibody based | 30 min-4 h | Sensitive or good specificity | Depends on host antibody response, false positive | Enzyme-linked immunosorbent assay—5 IU/mL |
| Nanoparticle-based methods: gold nanoparticles, graphene oxide | Gold nanoparticles-nucleic acid hybridization via thermoplasmonic heating: graphene oxide-field effect transistor | Not specified | High specificity and sensitivity | Requires expertise in nanoparticle synthesis and sensor fabrication | Gold nanoparticles -0.22 pM: graphene oxide—1 fg/mL |
Specific methods based on quantitative fluorescence polymerase chain reaction (QF-PCR) or isothermal nucleic acid amplification have also been developed (Bustin and Nolan 2020; Varlamov et al. 2020). Nucleic acid amplification tests (NAAT) are highly recommended by the World Health Organization, and they are based on reverse transcription-polymerase chain reaction (RT-PCR). However, nucleic acid-based testing is time-consuming and complicated, and host antibodies-based serological testing may lead to false-negatives during the initial viral infection. Moreover, paper-based testing is restricted to point-of-care testing due to the lower precision of detection. Paper-based tests include Feluda, E25Bio, and direct antigen rapid test (DART).
Preanalytical bias
Another issue is the preanalytical bias, which includes difficulties to scale-up, purify, store samples and to select the best body location from which the sample is collected. Indeed, biases have been observed for 93% of samples of bronchoalveolar lavage fluids, 72% for sputum, 63% for nasopharyngeal swabs, 46% for fibrobronchoscope brush biopsy, 32% for pharyngeal swabs, 29% for stools and 1% for blood, making the site of collection of high importance (Wang et al. 2020a, b). In addition, samples may be collected before development of the viral load, thus escaping detections. Overall, low viral loads and inappropriate specimen collection may give false results, and each technique has a different limit of detection. To conclude, a rapid, sensitive, and effective diagnosis strategy is urgently required.
Variants complicate detection and treatment
COVID-19 variants are formed under selective pressure in the convalescent plasma therapy, thus inducing the rapid development of antibiotic-resistant mutations (Kemp et al. 2020; Dai et al. 2021). Selective pressure is a natural phenomenon in which the drug-survived COVID-19 variants pass on the resistant gene to the subsequent generation, whereas the drug-susceptible variants perish and do not produce offspring. Due to the process of the selective pressure, the newer COVID-19 variants show higher pathogenicity and virulence. Consequently, the actual therapeutic strategies are based on drug repositioning or drug repurposing, which encompasses scrutinizing available drugs for new therapeutic purposes. Moreover, though drugs such as remdesivir, hydroxychloroquine and chloroquine have been approved, their mechanism of action against COVID-19 remains unclear. In such a complicated scenario, rapid testing and isolating COVID-19 positive cases could prevent progression of COVID-19. Moreover, scientific characterization and identification of different COVID-19 variants should reduce the prescription of antibiotics or antivirals and, in turn, diminish antibiotic resistance. Lastly, it is noteworthy that medical diagnosis generally guides the choice of the therapy. Therefore, the lack of effective diagnostics of different variants has highly challenged the management of the pandemic.
Why nanomaterials are highly relevant?
Viruses and nanomaterials have similar dimensions, of about 20–300 nm for the most studied viruses and 1–100 nm for nanomaterials (Singh et al. 2017). Since viruses possess designed strategies to infect all living organisms, scientists have been inspired by viruses to design nanomaterials, in particular for targeted drug and gene delivery (Wen and Steinmetz 2016). In particular, it has been predicted that nanotechnology-based pharmaceutical formulations could be powerful to limit the COVID-19 pandemic (Campos et al. 2020; Khan et al. 2021; Rangayasami et al. 2021). Nanoparticles can be tailored for prevention, diagnosis and treatments of the COVID-19 (Vahedifard and Chakravarthy 2021). Concerning prevention, colloidal solutions of silver, copper or zinc nanoparticles can be used as disinfectant, and gold nanoparticles can be designed for rapid detection of the coronavirus. Similarly, plastics containing antimicrobial silver nanoparticles, graphene or carbon nanotubes provide better safety to healthcare workers or healthy individuals.
Concerning diagnosis, nanoparticles can be used for biomarker-based, single-cell tracking because nanoparticles may have enzymatic and electric properties, chemical stability, and surface plasmon resonance (Navya and Daima 2016; Umapathi et al. 2018; Navya et al. 2019). In particular, enzyme-like properties can be fine-tuned for virus detection, drug or gene delivery, and even to impart therapeutic potentials against SARS-CoV-19. Concerning treatments, effective nanomedicines can be formulated to cure COVID-19 patients. For instance, a lipid nanoparticle–encapsulated mRNA-based vaccine has already been developed against SARS-CoV-2 to prevent secondary adverse effects of vaccines (Baden et al. 2020). Moreover, conventional issues of targeting, pharmacokinetics and compartmentalisation can be solved through tailored nanoparticles (Varahachalam et al. 2021). For example, nanoparticles used as drug carriers can decrease the toxicity of raw active substances such as zidovudine, dapivirine or efavirenz antivirals (Cojocaru et al. 2020).
Nanozymes can be tuned for biomedical applications
Nanoparticles bearing enzyme-like characteristics are named ‘nanozymes’ or ‘artificial enzymes’ (https://en.wikipedia.org/wiki/Artificial_enzyme). They have found applications for the detection of metal ions, small biomolecules, and cancer cells (Sharma, et al. 2014; Wang et al. 2020a, b; Daima et al. 2021). Nanozymes display several advantages over natural enzymes. Nanozymes can be easily manufactured and stored for longer periods, they are cost-effective and recyclable, whereas natural enzymes are often highly biodegradable and sensitive to heat, pH and pressure (Daima 2013; Daima 2014; Shankar et al. 2015; Sanjana et al. 2019). Moreover, nanozymes exhibit larger surface areas allowing easy bioconjugation, surface modification and integrated multi-functionalization, which are not possible using natural enzymes or small chemical catalysts. Due to their size, composition and surface corona activity, nanozymes can be tuned for specific biomedical applications just by varying their size, composition and surface chemistry (Matur et al. 2020), as detailed below.
Nanozymes for detection of chemicals, viruses and cells
Nanozymes can be used for detection. For instance, cerium oxide nanoparticles are used to monitor superoxide dismutase- and catalase-mimic activities, whereas ferric-based nanoparticles detect peroxidase- and oxidase-mimic actions (Yang et al. 2017; Bhagat et al. 2018). Nanomaterials have been used for the detection of glucose, cholesterol, organophosphorous neurotoxins, DNA, c-reactive proteins, viruses, stem cell, and cancer cells (Liang et al. 2013; Maji et al. 2015; Nirala et al. 2018; Jansman and Hosta-Rigau 2019; Sun et al. 2020; Gupta et al. 2021). Signals are detected and imaged using properties such as electrochemical, chemiluminescence, fluorescence, calorimetry, surface plasmon resonance and thermoplasmonic. Platinum-based nanomaterials show pH- and temperature-dependent enzyme-mimetic behaviour, and manipulating their size, shape, surface chemistry and surface charge allows to improve their medicinal potency.
Gold nanoparticles have been explored to detect mumps and zika virus (Hsu et al. 2020; Long et al. 2020). Gold nanozymes have been employed in rapid detection of SARS-CoV-19 (Pramanik et al. 2021). Indeed, samples taken in positive patients contain nucleocapsid phosphoprotein oligonucleotides that combine with thiol-functionalized gold nanozymes, which allow detection in 10 min by calorimetry (Kamaraj 2020). Compared to the traditional calorimetric methods using natural enzymes such as horseradish peroxidases and alkaline phosphatase, nanozymes display better sensitivity by involving chromogenic and fluorogenic substrates such as 3,3’,5,5’-tetramethylbenzidine, 2,2’-azinobis-(3-ethylbenzothiazoline-6-sulfonic acid, 3-(4-dihydroxy phenyl) propionic acid, and 2,3-diaminophenazine. Rapid and sensitive chemiluminescence kits have been developed to detect the virus spike proteins using a Co–Fe@hemin-peroxidase nanozyme at levels of 0.1 ng/mL (Liu et al. 2020). Furthermore, the use of magnetic iron oxide nanoparticles at the pre-diagnosis stage should help to isolate viruses specifically with a magnet (Jindal and Gopinath 2020).
Nanozymes for treatment
Nanozymes can be functionalized for therapeutic purposes. For instance, virus mitochondrial proteins can be degraded by multivalent silver nanozymes (Vahedifard and Chakravarthy 2021). The silver ions bind to the RNA viral genome to activate the mitochondrial proteins exhibiting an anti-viral effect (Galdiero et al. 2011). Gold nanozymes have the ability to mimic the binding receptor of viruses, thus leading to viral deformation (Huang et al. 2019). Zinc oxide nanozymes are also able to reduce viral infection by boosting T cell and antibody-mediated response (Antoine et al. 2012; Tabish and Hamblin 2020). Overall, nanozymes appear as an effective alternative to detect and target coronaviruses, yet catalytic mechanisms are poorly known, requiring research in nanotechnology, computational engineering, machine learning, artificial intelligence, and informatics.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Eric Lichtfouse, Email: eric.lichtfouse@gmail.com.
Hemant Kumar Daima, Email: hkdaima@jpr.amity.edu, Email: hkdaima@gmail.com.
References
- Antoine TE, Mishra YK, Trigilio J, Tiwari V, Adelung R, Shukla D. Prophylactic, therapeutic and neutralizing effects of zinc oxide tetrapod structures against herpes simplex virus type-2 infection. Antivir Res. 2012;96(3):363–375. doi: 10.1016/j.antiviral.2012.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baden LR, Sahly HME, Essink B, Kotloff K, Frey S, Novak R, Diemert D, Spector SA, Rouphael N, Creech BC, McGettigan J, Khetan S, Segall N, Solis J, Brosz A, Fierro C, Schwartz H, Neuzil K, Corey L, Gilbert P, Janes H, Follmann D, Marovich M, Mascola J, Polakowski L, Ledgerwood J, Graham BS, Bennett H, Pajon R, Knightly C, Leav B, Deng W, Zhou H, Han S, Ivarsson M, Miller J, Zaks T. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. New Engl J Med. 2020;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhagat S, Vallabani NVS, Shutthanandan V, Bowden M, Karakoti AS, Singh S. Gold core/ceria shell-based redox active nanozyme mimicking the biological multienzyme complex phenomenon. J Colloid Inter Sci. 2018;513:831–842. doi: 10.1016/j.jcis.2017.11.064. [DOI] [PubMed] [Google Scholar]
- Bustin SA, Nolan T. RT-qPCR Testing of SARS-CoV-2: A Primer. Int J Mol Sci. 2020 doi: 10.3390/ijms21083004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos EVR, Pereira AES, Oliveira JLD, Carvalho LB, Guilger-Casagrande M, Lima RD, Fraceto LF. How can nanotechnology help to combat COVID-19? Opportunities Urgent Need J Nanobiotechnol. 2020;18(1):125. doi: 10.1186/s12951-020-00685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakraborty D, Kumar S, Chandrasekaran N, MukherjeeA, Viral diagnostics and preventive techniques in the era of COVID-19: role of nanoparticles. Front Nanotechnol. 2020;2:7. doi: 10.3389/fnano.2020.588795. [DOI] [Google Scholar]
- Cojocaru FD, Botezat D, Gardikiotis I, Uritu C-M, Dodi G, Trandafir L, Rezus C, Rezus E, Tamba B-I, Mihai C-T. Nanomaterials designed for antiviral drug delivery transport across biological barriers. Pharmaceutics. 2020;12(2):171. doi: 10.3390/pharmaceutics12020171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Han J, Lichtfouse E. Smarter cures to combat COVID-19 and future pathogens: a review. Environ Chem Lett. 2021 doi: 10.1007/s10311-021-01224-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daima HK, Selvakannan PR, Shukla R, Bhargava SK, Bansal V. Fine-tuning the antimicrobial profile of biocompatible gold nanoparticles by sequential surface functionalization using polyoxometalates and lysine. PLoS ONE. 2013;8(10):1–14. doi: 10.1371/journal.pone.0079676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daima HK, Selvakannan PR, Kandjani AE, Shukla R, Bhargava SK, Bansal V. Synergistic influence of polyoxometalate surface corona towards enhancing the antibacterial performance of tyrosine-capped Ag nanoparticles. Nanoscale. 2014;6(2):758–765. doi: 10.1039/C3NR03806H. [DOI] [PubMed] [Google Scholar]
- Daima HK, Navya PN, Lichtfouse E. Nanozymes Environ Eng. 2021;1:1–241. doi: 10.1007/978-3-030-68230-9. [DOI] [Google Scholar]
- Galdiero S, Falanga A, Vitiello M, Cantisani M, Marra V, Galdiero M. Silver nanoparticles as potential antiviral agents. Molecules. 2011;16(10):8894–8918. doi: 10.3390/molecules16108894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorbalenya AE, Baker SC, Baric RS, Groot RJD, Drosten C, Gulyaeva AA, Haagmans BL, Lauber C, Leontovich AM, Neuman BW, Penzar D, Perlman S, Poon LLM, Samborskiy DV, Sidorov IA, Sola I, Ziebuhr J. Coronaviridae study group of the international committee on taxonomy of viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nature Microbiol. 2020;5(4):536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta PK, Son SE, Seong GH. Functionalized ultra-fine bimetallic PtRu alloy nanoparticle with high peroxidase-mimicking activity for rapid and sensitive colorimetric quantification of C-reactive protein. Mikrochim Acta. 2021;188(4):119. doi: 10.1007/s00604-021-04775-4. [DOI] [PubMed] [Google Scholar]
- Hsu Y-P, Li N-S, Chen Y-T, Pang H-H, Wei K-C, Yang H-W. A serological point-of-care test for Zika virus detection and infection surveillance using an enzyme-free vial immunosensor with a smartphone. Biosens and Bioelectron. 2020;151:111960. doi: 10.1016/j.bios.2019.111960. [DOI] [PubMed] [Google Scholar]
- Huang X, Li M, Xu Y, Zhang J, Meng X, An X, Sun L, Guo L, Shan X, Ge J, Chen J, Luo Y, Wu H, Zhang Y, Jiang Q, Ning X. Novel gold nanorod-based HR1 peptide inhibitor for middle east respiratory syndrome coronavirus. ACS Appl Mate Inter. 2019;11(22):19799–19807. doi: 10.1021/acsami.9b04240. [DOI] [PubMed] [Google Scholar]
- Ibarra-Coronado EG, Pantaleón-Martínez AM, Velazquéz-Moctezuma J, Prospéro-García O, Méndez-Díaz M, Pérez-Tapia M, Pavón L, Morales-Montor J. The bidirectional relationship between sleep and immunity against infections. J Immunol Res. 2015 doi: 10.1155/2015/678164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain U. Effect of COVID-19 on the organs. Cureus. 2020;12(8):e9540. doi: 10.7759/cureus.9540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jansman M, Hosta-Rigau L. Cerium- and iron-oxide-based nanozymes in tissue engineering and regenerative medicine. Catalysts. 2019;9(8):691. doi: 10.3390/catal9080691. [DOI] [Google Scholar]
- Jindal S, Gopinath P. Nanotechnology based approaches for combatting COVID-19 viral infection. Nano Express. 2020 doi: 10.1088/2632-959X/abb714. [DOI] [Google Scholar]
- Kamaraj S-K. The perspective on bio-nano interface technology for covid-19. Front Nanotechnol. 2020;2:18. doi: 10.3389/fnano.2020.586250. [DOI] [Google Scholar]
- Kemp SA, Collier DA, Datir R, Gayed S, Jahun A, Hosmillo M, Ferreira I, Rees-Spear C, Mlcochova P, Lumb IU, Roberts D, Chandra A, Temperton N. Neutralising antibodies drive Spike mediated SARS-CoV-2 evasion. Nature. 2020 doi: 10.1101/2020.12.05.20241927. [DOI] [Google Scholar]
- Khan AH, Tirth V, Fawzy M, Mahmoud AED, Khan NA, Ahmed S, Ali SS, Akram M, Hameed L, Islam S, Das G, Roy S, Dehghani MH. COVID-19 transmission, vulnerability, persistence and nanotherapy: a review. Environ Chem Lett. 2021 doi: 10.1007/s10311-021-01229-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang M, Fan K, Pan Y, Jiang H, Wang F, Yang D, Lu D, Feng J, Zhao J, Yang LA, Yan X. Fe3O4 magnetic nanoparticle peroxidase mimetic-based colorimetric assay for the rapid detection of organophosphorus pesticide and nerve agent. Anal Chem. 2013;85(1):308–312. doi: 10.1021/ac302781r. [DOI] [PubMed] [Google Scholar]
- Liu D, Ju C, Han C, Shi R, Chen X, Duan D, Yan J, Yan X. Ultra-sensitive nanozyme-based chemiluminescence paper test for rapid diagnosis of SARS-CoV-2 infection. Biosens Bioelectron. 2020;173:112817. doi: 10.1101/2020.06.05.131748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long L, Cai R, Liu J, Wu X. A novel nanoprobe based on core–shell Au@ Pt@ mesoporous SiO2 nanozyme with enhanced activity and stability for mumps virus diagnosis. Front Chem. 2020;8:463. doi: 10.3389/fchem.2020.00463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maji SK, Mandal AK, Nguyen KT, Borah P, Zhao Y. Cancer cell detection and therapeutics using peroxidase-active nanohybrid of gold nanoparticle-loaded mesoporous silica-coated graphene. ACS Appl Mater inter. 2015;7(18):9807–9816. doi: 10.1021/acsami.5b01758. [DOI] [PubMed] [Google Scholar]
- Matur M, Madhyastha H, Shruthi TS, Madhyastha R, Srinivas SP, Navya PN, Daima HK. Engineering bioactive surfaces on nanoparticles and their biological interactions. Sci Rep. 2020;10(1):19713. doi: 10.1038/s41598-020-75465-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navya PN, Daima HK. Rational engineering of physicochemical properties of nanomaterials for biomedical applications with nanotoxicological perspectives. Nano Converg. 2016;3(1):1–14. doi: 10.1186/s40580-016-0064-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navya PN, Kaphle A, Daima HK. Nanomedicine in sensing, delivery, imaging and tissue engineering: advances, opportunities and challenges. Nanoscience: Volume 5. The Royal Society of Chemistry. 2019;5:30–56. doi: 10.1039/9781788013871-00030. [DOI] [Google Scholar]
- Nirala NR, Saxena PS, Srivastava A. Colorimetric detection of cholesterol based on enzyme modified gold nanoparticles. Spectrochim Acta A. 2018;190:506–512. doi: 10.1016/j.saa.2017.09.058. [DOI] [PubMed] [Google Scholar]
- Paliwal P, Sargolzaei S, Bhardwaj SK, Bhardwaj V, Dixit C, Kaushik A. Grand challenges in bio-nanotechnology to manage COVID-19 pandemic. Front Nanotechnol. 2020 doi: 10.3389/fnano.2020.571284. [DOI] [Google Scholar]
- Pramanik A, Gao Y, Patibandla S, Mitra D, McCandless MG, Fassero LA, Gates K, Tandon R, Ray PC. The rapid diagnosis and effective inhibition of coronavirus using spike antibody attached gold nanoparticles. Nanoscale Adv. 2021;3(6):1588–1596. doi: 10.1039/d0na01007c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu G, Gai Z, Tao Y, Schmitt J, Kullak-Ublick G-A, Wang J. Dual-functional plasmonic photothermal biosensors for highly accurate severe acute respiratory syndrome coronavirus 2 detection. ACS Nano. 2020;14(5):5268–5277. doi: 10.1021/acsnano.0c02439. [DOI] [PubMed] [Google Scholar]
- Rangayasami A, Kannan K, Murugesan S, Radhika D, Sadasivuni KK, Reddy KR, Raghu AV. Influence of nanotechnology to combat against COVID-19 for global health emergency: a review. Sens Int. 2021 doi: 10.1016/j.sintl.2020.100079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallard E, Halloy J, Casane D, Decroly E, Helden JV. Tracing the origins of SARS-COV-2 in coronavirus phylogenies: a review. Environ Chem Lett. 2021;19(2):769–785. doi: 10.1007/s10311-020-01151-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanjana S, Medha MU, Meghna MR, Shruthi TS, Srinivas SP, Madhyastha H, Navya PN, Daima HK. Enzyme immobilization on quercetin capped gold and silver nanoparticles for improved performance. Mater Today: Proc. 2019;10(1):92–99. doi: 10.1016/j.matpr.2019.02.193. [DOI] [Google Scholar]
- Seo G, Lee G, Kim MJ, Baek S-H, Choi M, Ku KB, Lee C-S, Jun S, Park D, Kim HG, Kim S-J, Lee J-O, Kim BT, Park EC, Kim SI. Rapid Detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano. 2020;14(4):5135–5142. doi: 10.1021/acsnano.0c02823. [DOI] [PubMed] [Google Scholar]
- Shankar S, Soni SK, Daima HK, Selvakannan PR, Khire JM, Bhargava SK, Bansal V. Charge-switchable gold nanoparticles for enhanced enzymatic thermostability. Phys Chem Chem Phys. 2015;17(33):21517–21524. doi: 10.1039/C5CP03021H. [DOI] [PubMed] [Google Scholar]
- Sharma TK, Ramanathan R, Weerathunge P, Mohammadtaheri M, Daima HK, Shukla R, Bansal V. Aptamer-mediated ‘turn-off/turn-on’nanozyme activity of gold nanoparticles for kanamycin detection. Chem Commun. 2014;50(100):15856–15859. doi: 10.1039/C4CC07275H. [DOI] [PubMed] [Google Scholar]
- Sharma VK, Jinadatha C, Lichtfouse E. Environmental chemistry is most relevant to study coronavirus pandemics. Environ Chem Lett. 2020;18(4):993–996. doi: 10.1007/s10311-020-01017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shope RE. Swine influenza : III. Filtration experiments and etiology. J Exp Med. 1931;54(3):373–385. doi: 10.1084/jem.54.3.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh L, Kruger HG, Maguire GEM, Govender T, Parboosing R. The role of nanotechnology in the treatment of viral infections. Ther Adv Infect Dis. 2017;4(4):105–131. doi: 10.1177/2049936117713593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith W, Andrewes CH, Laidlaw PP. A virus obtained from influenza patients. The Lancet. 1933;222(5732):66–68. doi: 10.1016/S0140-6736(00)78541-2. [DOI] [Google Scholar]
- Sun H, Cai S, Wang C, Chen Y, Yang R. Recent progress of nanozymes in the detection of pathogenic microorganisms. ChemBioChem. 2020;21(18):2572–2584. doi: 10.1002/cbic.202000126. [DOI] [PubMed] [Google Scholar]
- Tabish TA, Hamblin MR. Multivalent nanomedicines to treat COVID-19: a slow train coming. Nano Today. 2020 doi: 10.1016/j.nantod.2020.100962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umapathi A, Kaphle A, Nagraju NP, Monnappa S, Firdose N, Jain D, Sangly SP, Madhyastha H, Madhyastha R, Daima HK (2018). Impact of physicochemical properties and surface chemistry of nanomaterials on toxicity. Nanotoxicology: Toxicity Evaluation, Risk Assessment and Management. CRC Press 35–61. doi: 10.1201/b21545-3
- Vahedifard F, Chakravarthy K. Nanomedicine for COVID-19: the role of nanotechnology in the treatment and diagnosis of COVID-19. Emerg Mater. 2021;4(1):75–99. doi: 10.1007/s42247-021-00168-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varahachalam SP, Lahooti B, Chamaneh M, Bagchi S, Chhibber T, Morris K, Bolanos JF, Kim N-Y, Kaushik A. Nanomedicine for the SARS-CoV-2: state-of-the-art and future prospects. Int J Nanomed. 2021;16:539. doi: 10.2147/IJN.S283686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varlamov DA, Blagodatskikh KA, Smirnova EV, Kramarov VM, Ignatov KB. Combinations of PCR and Isothermal Amplification Techniques Are Suitable for Fast and Sensitive Detection of SARS-CoV-2 Viral RNA. Front Bioeng Biotech. 2020 doi: 10.3389/fbioe.2020.604793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang P, Wang T, Hong J, Yan X, Liang M. Nanozymes: a new disease imaging strategy. Front Bioeng Biotech. 2020 doi: 10.3389/fbioe.2020.00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323(18):1843–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen AM, Steinmetz NF. Design of virus-based nanomaterials for medicine, biotechnology, and energy. Chem Soc Rev. 2016;45(15):4074–4126. doi: 10.1039/C5CS00287G. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H, Xiao J, Su L, Feng T, Lv Q, Zhang X. Oxidase-mimicking activity of the nitrogen-doped Fe3C@C composites. Chem Commun. 2017;53(27):3882–3885. doi: 10.1039/C7CC00610A. [DOI] [PubMed] [Google Scholar]
- Zavaleta C, Ho D, Chung E. Theranostic nanoparticles for tracking and monitoring disease state. SLAS Technol. 2018;23(3):281–293. doi: 10.1177/2472630317738699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD, Chen J, Luo Y, Guo H, Jiang R-D, Liu M-Q, Chen Y, Shen XR, Wang X, Zheng XS, Zhao K, Chen QJ, Deng F, Liu LL, Yan B, Zhan FX, Wang YY, Xiao GF, Shi ZL. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;588(7836):270–273. doi: 10.1038/s41586-020-2951-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou B, Thao TTN, Hoffmann D, Taddeo A, Ebert N, Labroussaa F, Pohlmann A, King J, Steiner S, Kelly JN, Portmann J, Halwe NJ, Ulrich L, Trueb BS, Fan X, Hoffman B, Wang L, Thomann L, Lin X, Stalder H, Pozzi B, Brot SD, Jiang N, Cui D, Hossain J, Wilson MM, Keller MW, Stark TJ, Barnes JR, Dijkman R, Jores J, Benarafa C, Wentworth DE, Theil V, Beer M. SARS-CoV-2 spike D614G change enhances replication and transmission. Nature. 2021;592:121–127. doi: 10.1038/s41586-021-03361-1. [DOI] [PubMed] [Google Scholar]