Abstract
Aims: The aim of this study was to test a Child-Centred Health Dialogue model for primary prevention of obesity for 4-year-old children in Child Health Services, for its feasibility and the responsiveness of its outcomes. Methods: A feasibility study was set up with a non-randomised quasi-experimental cluster design comparing usual care with a structured multicomponent Child-Centred Health Dialogue consisting of two parts: (1) a universal part directed to all children and (2) a targeted part for families where the child is identified with overweight. Results: In total, 203 children participated in Child-Centred Health Dialogue while 582 children received usual care. Nurses trained in the model were able to execute both the universal health dialogue and the targeted part of the intervention. Tutorship enabled the nurses to reflect on and discuss their experiences, which strengthened their confidence and security. One year after the intervention fewer normal-weight 4-year-olds in the intervention group had developed overweight at the age of five compared with the control group, and none had developed obesity. The difference in overweight prevalence at follow-up did not reach statistical significance. Conclusions: This study demonstrates that a child-centred, multicomponent, interactive intervention for the promotion of healthy lifestyles and primary prevention of obesity for all 4-year-old children participating in Child Health Services is feasible on a small scale. As almost all caregivers make use of Child Health Services in Sweden, the findings should be confirmed in a randomised controlled trial before the intervention can be implemented on a larger scale.
Keywords: Primary care, preschool, primary prevention obesity, health promotion, child-centred, health literacy, family therapy
Background
The rise in child obesity challenges global health as it results in various health and social consequences. The number of obese children has increased tenfold in the last 40 years [1]. The World Health Organization estimated that in 2016, approximately 42 million children under 5 years worldwide were overweight or obese, and that this number is likely to increase to at least 50 million by 2030 [2]. Globally the percentage of children under five with overweight and obesity is estimated to be 6.0% [2]. In Sweden the prevalence of increased body mass index (BMI) in 4-year-olds born 2013 was 11.7% (9.4% overweight and 2.3% obesity) [3].
The evidence is strong that, once a preschool child has obesity, it tracks through to adulthood and is difficult to reverse [4]. Therefore, primary prevention and lifestyle interventions are important in order to promote a healthy lifestyle and reduce the likelihood of later obesity. Studies indicate that young age at intervention is a strong predictor for positive outcome, in both the short and the long term [4]. Caregivers even ask for early interventions that focus on the preschool years, a period when behaviours and habits are shaped [5]. Previous research shows that, in order to prevent obesity in early age, family-based interventions are more effective, especially when multicomponent (targeting healthy eating and physical activity) and interactive [4, 6]. It is essential that these interventions are universal and can be implemented in the real-world environment into routine practices [7, 8].
The Swedish Child Health Services (CHS), which are free of charge and attended by nearly all families, irrespective of social position or ethnicity [9], provide a package of health care universally to all children and extra health visits according to need. Nurses together with physicians are responsible for health surveillance of children from birth up to the age of five (18 scheduled health visits, 14 with the nurse and four with the nurse and physician together) and work at Child Health Centres (CHCs). One of the aims of CHS is to promote a healthy lifestyle through regular health dialogues. These health dialogues are led by a salutogenic approach which promotes protective factors in order to maintain and strengthen health and a supportive environment approach to support participation and empowerment [9]. Another aim of CHS is to prevent obesity through early identification of risk factors including overweight. The most widely used method of measuring and identifying overweight and obesity is BMI using the age-standardised International Obesity Task Force (IOTF) cut-off points [10].
Evidence-based models that can be used in CHS for the promotion of healthy lifestyle and prevention of obesity are lacking [9]. Research shows that professionals working within CHS pay infrequent attention to health behaviours in dialogues with caregivers of 4-year-olds, and nurses find it delicate to talk about dietary behaviours and overweight [11, 12]. Another complicating factor is that caregivers and even health professionals have difficulty identifying overweight in a pre-schooler without using a BMI growth chart, which means that most caregivers presumably will be surprised when their children are identified as overweight [13].
Little is known about the participation of the child itself in the primary prevention of obesity. Research suggests that children as young as 2 years old are able to communicate their needs and opinions in health care settings [14] and generally prefer to be included in health care interactions [15]. Since the endorsement of the Swedish Patient Law that reinforces the rights of the child as stated in the United Nations Convention on the Rights of the Child, children must be given the opportunity to participate in health dialogues as active agents expressing their needs based on their competence [16]. Therefore, there is a need for a child-centred, multicomponent, interactive intervention that includes the family of the child and can be executed universally within CHS. The aim of this study was to test a Child-Centred Health Dialogue model for primary prevention of obesity for 4-year-old children in CHS, for its feasibility and the responsiveness of its outcomes.
Methods
Design
The study was guided by the Medical Research Council’s framework for complex interventions [17], which serves to systematically develop an intervention using the best available evidence and appropriate theory and then test for feasibility before evaluation in a full-scale randomised control trial (RCT). A feasibility study was set up with a non-randomised quasi-experimental cluster design. The study was planned and carried out in compliance with the ethical principles of the Declaration of Helsinki. Approval was obtained from the Regional Ethical Review Board in Lund (2015/223).
Setting
The study was conducted in the southern county of Sweden, which has 146 CHCs where about 96,000 children between 0 and 6 years of age are registered [18]. An intervention was tested at three CHCs in two municipalities and compared with eight CHCs matched in non-randomised fashion regarding Care Need Index (CNI) and residential area. CNI is a socioeconomic need index that aims to measure individuals need for health care based on various socioeconomic factors and is calculated for each CHC based on the enrolled patient population [19]. Six nurses working with intervention care received 2 days of training for the Child-Centred Health Dialogue model (CCHD). They were also offered tutorial sessions during the time of intervention from a nurse educated in family therapy with long experience of working with child obesity and the later described Standardized Obesity Family Therapy (SOFT). Thirteen nurses working at the eight control CHCs executed usual care. Two qualitative studies exploring the perspectives of nurses and caregivers participating in the universal part of the Health Dialogue were performed simultaneously with the present study [20, 21].
Child-Centred Health Dialogue
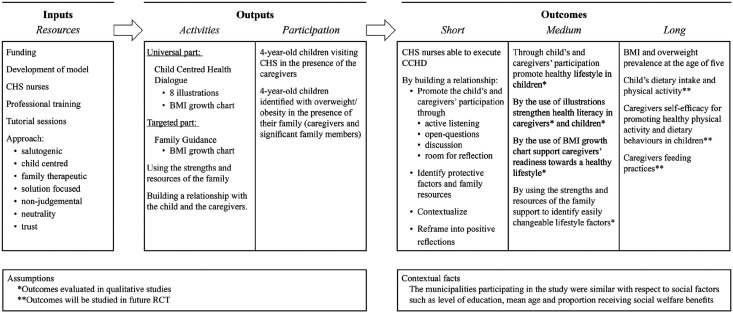
CCHD is a structured child-centred health dialogue that consists of two parts: (1) a universal part directed to all 4-year-olds and their caregiver visiting CHS and (2) a targeted part for families where the 4-year-old is identified with overweight (Figure 1).
Figure 1.
Logic model for the Child-Centred Health Dialogue.
CCHD was developed based on the best available evidence by nurses and paediatricians, including one of the authors (MD) supported by professionals responsible for the national handbook for CHS in Sweden [22]. The overarching theoretical basis of the intervention is Child-Centred Care, which puts the child in the centre and includes the child as an independent actor supported by the family [15]. To be able to promote a healthy lifestyle it is important that the child and its caregivers are given easily accessible information [23]. In this way Health Literacy is another concept used for the development of CCHD, as it attempts to meet the health literacy needs of children and their caregivers [21]. The BMI growth chart was used to help caregivers gain an accurate weight perception in order to support readiness for a healthy lifestyle [13, 24].
The universal part of CCHD
The universal part of CCHD contained, on the one hand, a structured dialogue using eight illustrations based on the most important modifiable feeding and related practices associated with overweight in preschool children (Table I) and, on the other hand, an evaluation of the child’s growth development using the BMI chart.
Table I.
Overview of the illustrations.
| 1 | Fruit and vegetables | Children with higher consumption of fruit and/or vegetables consume less total energy and have been associated with a more desirable body weight during preschool years. |
| 2 | The ‘Plate model’ | Total energy intake and portion size negatively affect weight in children of 4 years and older and research suggests that parents can be encouraged to monitor the portion sizes of foods that children are offered at home. |
| 3 | Portion size | |
| 4 | Sugar-sweetened beverages | Intake of sugar-sweetened beverages has been positively related to overweight or obesity in preschool children. |
| 5 | Active playtime | Time spent in physical activity or active play has been inversely associated with risk of overweight among preschool children. |
| 6 | Sedentary behaviours | Sedentary viewing has been positively associated with overweight or obesity in preschool children. |
| 7 | Sleeping routines | Sleep duration has been inversely associated with overweight and obesity in preschool children. |
| 8 | Tooth brushing | The prevalence of caries is correlated with intake of sweetened beverages. |
The interactive illustrations were developed by a professional illustrator and included animated characters as a strategy to engage preschool children [25]. In the structured dialogue the nurse first introduced each illustration to the child in the presence of its caregiver. Each illustration was then followed by an open dialogue with the child and the caregiver to ensure caregiver involvement. Finally, the nurse summarised the conversation and recapped the health message. To standardise the health dialogue an instruction guide was made available, although the nurse was encouraged to listen carefully to the child and the caregiver and follow up what was said. The universal part of CCHD was completed by demonstrating the BMI growth chart for the caregivers to show BMI development and to identify overweight or obesity.
The targeted part of CCHD
Children identified with overweight and obesity and their caregivers or other important family members were invited to the targeted part of CCHD, Family Guidance, taking place 1–3 weeks after the universal 4-year health visit. The Family Guidance is a family consultation with a solution-focussed approach grounded on the evidence-based SOFT [26]. SOFT is a low-intensity treatment which has shown positive effects in the treatment of child obesity [27]. SOFT empowers family members to carry out lifestyle changes by themselves by influencing the context of change through collaborative family support and by adopting a normalising and non-blaming position [26]. The BMI chart was used to identify habits that might have driven BMI upwards and could guide family members to choose habits that seem easiest for them to change. Children with obesity were also referred to a multidisciplinary treatment team consisting of a specialised nurse, a dietician and a paediatrician at the nearest outpatient clinic for lifestyle changing support according to regional guidelines.
Usual care
Usual care involved a 4-year health visit to all 4-year-olds where nurses were recommended to talk with caregivers about the child’s eating habits and physical activity. The professionals were aware of the importance of promoting health lifestyles, but they did not receive any specific training regarding overweight prevention as was provided in CCHD.
Data collection
Between June 2015 and June 2016 nurses working at the intervention CHCs invited all 4-year-olds to participate in CCHD. After the consent of both caregivers the age of the child, sex, weight and height were registered directly after the 4-year health visit on a case report form for children in the intervention. At follow-up, 1 year after CCHD age, sex, weight and height at the age of 5 were registered. In the control group age, sex, weight and height at the age of 4 and 5 were collected retrospectively from Profdoc Medical Office for all children that had visited one of the eight control CHCs for their 5-year health visit between June 2016 and July 2017.
Measurements and statistical analysis
The number and the duration of the tutorial sessions were measured and the scope of content was passed on to the researcher (MD). In order to describe usual care an anonymous questionnaire was distributed among all nurses working within CHS in the south of Sweden in May 2016. BMI and BMI standard deviation score (SDS) were calculated at the age of 4 (baseline) and 5 (follow-up). Each child’s BMI was then categorised into underweight, normal weight, overweight and obesity using the IOTF standard definitions [10]. We matched the children in the intervention group with three times as many in the register control group to identify differences in mean absolute change BMI SDS at the age of five. A two-sample t-test was used to compare the mean absolute change in the intervention and control group. As an important aim of the intervention is to prevent overweight, we also compared the prevalence of overweight at the age of 5 among the normal-weight 4-year-olds in the intervention and control group using Fisher’s exact test. Results were also reported for the overweight, obese and underweight children at baseline but were not subjected to statistical significance testing.
Results
Feasibility
Testing the research protocol in the clinical setting of CHS showed that 203 children received the universal part of CCHD and 20 families in which the child was identified with overweight received the targeted part. A total of 194 children participated in follow-up 1 year after the intervention (Figure 2). The rate of recruitment was 94% and the rate of retention was 95.6%. Of the nine children lost to follow-up, eight had normal weight and one had obesity at the age of four.
Figure 2.
Flowchart describing the inclusion of children.
The nurses working at the intervention CHCs received six tutorial sessions of 1 hour once every 2 months during the duration of the study. In the sessions nurses were able to discuss and reflect on their experiences, which made them feel more comfortable in CCHD. They felt stimulated using CCHD and described the illustrations as a way to gain the child’s confidence triggering them to talk about healthy habits [20]. During tutorship the nurses described how they considered it easier to talk about overweight and said that the BMI chart was helpful in explaining trends in BMI.
The questionnaire describing usual care was answered by 229 out of 351 nurses (65%) working in the south of Sweden and showed that many (55%) did not have a structured health dialogue at the 4-year health visit and the majority thought it was difficult to talk to caregivers about healthy eating (>70%) and overweight (>90%). Only 10% of the nurses used illustrations to support the health conversation. Many nurses showed the BMI chart to caregivers (45% always and 24% often), but the BMI chart was seldom used as a tool to promote a healthy lifestyle (0.5%).
Responsiveness of outcomes
The prevalence of overweight and obesity at baseline (9.9%) was lower in the intervention group than in the control group (12.7%). Conversely, there was a higher prevalence of underweight (13.3%) in the intervention group at baseline compared with the control group (10.0%). Mean BMI in both groups was similar 15.9 [sd: 1.4] compared with 16.1 [sd: 1.4] (Table II).
Table II.
Data at baseline and follow-up.
| Baseline | Intervention (n=203) | Usual care (n=582) |
|---|---|---|
| Age (years) | 4.1±0.1 | 4.1±0.1 |
| BMI | 15.9±1.4 | 16.1±1.4 |
| BMI SDS | 0.09±1.0 | 0.23±1.0 |
| Girls | 106 (52.2) | 299 (51.4) |
| Normal weight** | 156 (76.8) | 450 (77.3) |
| Overweight and obesity | 20 (9.9) | 74 (12.7) |
| Overweight | 16 (7.9) | 65 (11.2) |
| Obesity | 4 (2.0) | 9 (1.5) |
| Underweight | 27 (13.3) | 58 (10.0) |
| Follow-up | Intervention (n=194) | Usual care (n=582) |
| Age (years) | 5.4±0.18 | 5.1±0.14 |
| BMI | 15.7±1.6 | 16.0±1.7 |
| BMI SDS | 0.15±1.1 | 0.31±1.1 |
| Abs change BMI SDS | 0.01±1.42 | 0.05±0.44 |
| Girls | 102 (52.6) | 299 (51.4) |
| Normal weight | 151 (77.8) | 439 (75.4) |
| Overweight and obesity | 25 (12.9) | 100 (17.1) |
| Overweight | 18 (9.3) | 75 (11.2) |
| Obesity | 7 (3.6) | 25 (4.2) |
| Underweight | 18 (9.3) | 43 (7.4) |
Data are presented as mean ± SD values or n (%).
Each child’s BMI was categorised into underweight, normal weight, overweight and obesity using the IOTF standard definitions.
At follow-up there was no significant difference in absolute change BMI SDS between the children in the intervention group compared with the control group: 0.01 [sd: 0.42] and 0.05 respectively [sd: 0.44] (p=0.23; 95% CI −0.03 to 0.11) (Table II).
Of the normal-weight children in the intervention at baseline, at follow-up 6.1% became overweight, none became obese and 93.9% retained normal weight. In the control group among the children that had normal weight at baseline, the prevalence of overweight at follow-up was 8.9% (8.0% for overweight and 0.9% for obesity) and 91.1% remained normal weight. None of the normal weight children in either the intervention or the control group were categorised as underweight at follow-up. The difference in overweight prevalence at follow-up among normal-weight children at baseline did not reach statistical significance (p=0.18) (Table III).
Table III.
Development of BMI categories from baseline to follow-up.
| Normal weight at baseline | At follow-up | Total | ||
|---|---|---|---|---|
| Normal weight | Overweight | Obesity | ||
| Intervention | 139 (93.9) | 9 (6.1) | 148 (100) | |
| Control | 410 (91.1) | 36 (8.0) | 4 (0.9) | 450 (100) |
| Overweight at baseline | At follow-up | |||
| Normal weight | Overweight | Obesity | ||
| Intervention | 3 (18.8) | 9 (56.3) | 4 (25.0) | 16 (100) |
| Control | 14 (21.5) | 38 (58.5) | 13 (20.0) | 65 (100) |
| Obesity at baseline | At follow-up | |||
| Normal weight | Overweight | Obesity | ||
| Intervention | 3 (100) | 3 (100) | ||
| Control | 1 (11.1) | 8 (88.9) | 9 (100) | |
| Underweight at baseline | At follow-up | |||
| Normal weight | Overweight | Underweight | ||
| Intervention | 9 (33.3) | 18 (66.7) | 27 (100) | |
| Control | 15 (25.9) | 43 (74.1) | 58 (100) | |
Data are presented as n (%)
Of the 16 overweight children in the intervention group at baseline, three (18.8%) had become normal weight, nine (56.3%) remained overweight and four (25%) children had obesity at follow-up. Of the three children with obesity at baseline, all continued to be obese at follow-up (one lost to follow-up). In the control group 21.5% of the overweight children at baseline had become normal weight at follow-up, 58.5% stayed overweight at follow-up and 20% had developed obesity. For children with obesity at baseline, one child became overweight (11.1%) and eight continued to have obesity (88.9%) (Table III). We did not calculate any statistical tests because we considered that 19 children with either overweight or obesity was too small a number to compare with.
Of the 27 underweight children in the intervention at baseline, at follow-up nine (33.3%) had become normal weight and 18 (66.7%) remained underweight. In the control group among the children that were underweight at baseline, the prevalence of normal weight and underweight was 25.9% and 74.1%, respectively, at follow-up. None of the underweight children in both the intervention and the control group were categorised as overweight at follow-up (Table III).
Discussion
This study shows that CCHD is feasible on a small scale. Nurses trained in CCHD were able to execute the universal health dialogue using the illustrations as well as the BMI chart to identify overweight. The nurses felt stimulated using a new health conversation model and felt more comfortable in the universal part of CCHD [20]. They even performed 20 Family Guidances using concepts of family therapy. In Family Guidance the nurse helps the family to identify their strengths and resources in order to empower the family and to help them develop healthy routines on their own without frequent contact with the health care system [26]. Although the number of children with overweight was low, the nurses said that the training and tutorship provided them with skills to bring up the subject of overweight. This is an important finding, especially since caregivers of preschool-age children do not recognise their children as overweight and prevention may not be a relevant issue [28]. The qualitative study describing caregivers’ experiences of CCHD indicated that the caregivers wanted to promote a healthy lifestyle for their children and experienced guidance and understanding. They felt the dialogue focussed on their own strengths and abilities and created supportive conditions for family members’ active participation in the visits, promoting empowerment and strengthening health literacy [21].
The present feasibility study did not reveal significant effects of the intervention on absolute BMI SDS change or the prevalence of overweight/obesity. However, it showed trends in the development of BMI among normal-weight 4-year-olds, which were more favourable in the intervention. Fewer normal-weight 4-year-olds in the intervention group had developed overweight compared with normal-weight 4-year-olds in the control group and none had developed obesity. This trend, although not significant, is important in an intervention that primarily aims to prevent overweight in children that have not yet developed overweight, and it should be further evaluated in a subsequent adequately powered trial. This future RCT will include evaluation of both the universal and the targeted part of CCHD as research shows that health professionals not only want to be trained in preventing overweight but also desire to receive training in the guidance that is given when overweight is identified, as they experience this condition as delicate to address [29].
Another interesting trend was that a higher proportion of underweight children had attained normal weight in the intervention group compared with the underweight children in the control group. This trend might be explained by the fact that CCHD promotes a healthy lifestyle for all children. A recent study showed that both overweight and underweight were associated with low health literacy [30]. The use of illustrations in CCHD might be an explanation for this trend as an attempt to meet the health literacy needs of children and their caregivers [25].
One of the limitations of this feasibility study was that there was no random assignment and that the number of children with overweight and obesity at baseline was too small to consider calculating any statistical tests. Another limitation is that weight and height were only collected prospectively in the intervention group but not in the control group, and that BMI was the only long-term outcome measurement. The present study did not measure changes in dietary intake and physical activity, caregivers’ self-efficacy for promoting healthy lifestyle and caregivers feeding practices (Figure 1). These outcomes, however, will be evaluated in an RCT as well as the cost-effectiveness, which is recommended [4]. Lastly, the children’s experiences of CCHD, which are of utmost importance in a child-centred intervention, were not evaluated in the feasibility phase but will be explored during the RCT.
However, the study also had considerable strengths: first, the theoretical foundation in Child-Centred Care that respects the child, belonging to the family, as an active agent in the promotion of a healthy lifestyle which is in line with the Swedish Patient Law [16], and second, the use of tutorial sessions as a way to teach a new model. The tutorship enabled the nurses to reflect upon and discuss their experiences, which strengthened their confidence and security in the model [20].
Conclusions
This study demonstrates that a child-centred, interactive, multicomponent intervention for the promotion of healthy lifestyles and for the primary prevention of obesity for all 4-year-old children participating in CHS visited by almost all caregivers is feasible on a small scale. Effectiveness and cost-effectiveness of both the universal and the targeted part of CCHD need to be tested in a subsequent full-scale RCT before the intervention can be implemented on a larger scale.
Acknowledgments
Special thanks to the children and caregivers that participated in the study and the nurses executing CCHD. Thanks to Linda Håkansson for managing the project and to Ulla Börjeson Munk for supporting the nurses in the tutorial sessions.
Footnotes
Declaration of conflicting interests: The authors declare that there is no conflict of interest.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by The Swedish Research Council for Health, Working Life and Welfare (FORTE), Region Skåne and Föreningen Mjölkdroppen Helsingborg.
ORCID iDs: Mariette Derwig  https://orcid.org/0000-0002-9087-0506
https://orcid.org/0000-0002-9087-0506
Jonas Björk  https://orcid.org/0000-0003-1883-2000
https://orcid.org/0000-0003-1883-2000
Availability of data and materials: The data set generated and analysed during the current study will not be shared to maintain participants’ anonymity and confidentiality, but are available from the corresponding author on reasonable request.
References
- [1]. Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017; 390: 2627–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. World Health Organization. Report of the Commission on Ending Childhood Obesity: Implementation plan: Executive summary, 2017. [Google Scholar]
- [3]. Nylander C, Miregård J. Overweight and obesity in four year olds in Sweden. Poster presented on National Conference on Child Health Services. In Swedish. 2018. https://edilprod.dll.se/GetPublicFile.ashx?docid=409659 (accessed 10 September 2019).
- [4]. Waters E, de Silva-Sanigorski A, Hall BJ, et al. Interventions for preventing obesity in children. Cochrane Database Syst Rev 2011; 12. [DOI] [PubMed] [Google Scholar]
- [5]. Stenhammar C, Wells M, Ahman A, et al. ‘Children are exposed to temptation all the time’- parents’ lifestyle-related discussions in focus groups. Acta Paediatr 2012; 101: 208–215. [DOI] [PubMed] [Google Scholar]
- [6]. Yavuz HM, van IJzendoorn MH, Mesman J, et al. Interventions aimed at reducing obesity in early childhood: A meta-analysis of programs that involve parents. J Child Psychol Psychiatry 2015; 56: 677–692. [DOI] [PubMed] [Google Scholar]
- [7]. Enö Persson J, Bohman B, Tynelius P, et al. Prevention of childhood obesity in Child Health Services: Follow-up of the PRIMROSE Trial. Childhood Obes 2018; 14: 99–105. [DOI] [PubMed] [Google Scholar]
- [8]. Matwiejczyk L, Mehta K, Scott J, et al. Characteristics of effective interventions promoting healthy eating for pre-schoolers in childcare settings: An umbrella review. Nutrients 2018; 10: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. The National Board of Health and Welfare, Socialstyrelsen. Guidelines for Child Health Services. In Swedish. 2014. [Google Scholar]
- [10]. Cole TJ, Bellizzi MC, Flegal KF, et al. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000; 7244: 1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Bohman B, Eriksson M, Lind M, et al. Infrequent attention to dietary and physical activity behaviours in conversations in Swedish child health services. Acta Paediatr 2013; 102: 520–524. [DOI] [PubMed] [Google Scholar]
- [12]. Ljungkrona-Falk L, Brekke H, Nyholm M. Swedish nurses encounter barriers when promoting healthy habits in children. Health Promot Int 2014; 29: 730–738. [DOI] [PubMed] [Google Scholar]
- [13]. Regber S, Novak M, Eiben G, et al. Parental perceptions of and concerns about child’s body weight in eight European countries – the IDEFICS study. Pediatr Obes 2013; 8: 118–129. [DOI] [PubMed] [Google Scholar]
- [14]. Stålberg A, Sandberg A, Söderbäck M. Younger children’s (three to five years) perceptions of being in a health-care situation. Early Child Develop Care 2016; 186: 832–844. [Google Scholar]
- [15]. Coyne I, Hallström I, Söderbäck M. Reframing the focus from a family-centred to a child-centred care approach for children’s healthcare. J Child Health Care 2016; 20: 494–502. [DOI] [PubMed] [Google Scholar]
- [16]. Swedish Government, Patient Law (Patientlagen). 2014; 821: 2015. [Google Scholar]
- [17]. Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008; 337: a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. County of Scania, Region Skåne, Annual Report Child Health Services County of Scania 2017. In Swedish. 2018. [Google Scholar]
- [19]. SCB, Statistiska Centralbyrån Statistics Sweden. Care Need Index – a socioeconomic need index. Before Vårdval 2010. In Swedish. 2009. [Google Scholar]
- [20]. Håkansson L. Nurses experiences on the health dialogue concerning healthy eating in Child Health Service. In Swedish. Student Thesis, Department of Health Sciences, Mid Sweden University, Sweden, 2015. [Google Scholar]
- [21]. Håkansson L, Derwig M, Olander E. Parents’ experiences of a health dialogue in Child Health Services: A qualitative study. BMC Health Serv Res 2019; 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Digital National Handbook for Child Health Services, http://www.rikshandboken-bhv.se/.
- [23]. Velardo S, Drummond M. Emphasizing the child in child health literacy research. J Child Health Care 2016; 21: 5–13. [DOI] [PubMed] [Google Scholar]
- [24]. Börnhorst C, Siani A, Tornaritis M, et al. Potential selection effects when estimating associations between the infancy peak or adiposity rebound and later body mass index in children. Int J Obes (Lond) 2017; 41(4) 518–526. [DOI] [PubMed] [Google Scholar]
- [25]. LaSala KB, Abbot Eng CR. Effectiveness of a child’s fable on the cognition of preschools when used to address childhood obesity. J Pediatr Nurs 2014; 29: 547–554. [DOI] [PubMed] [Google Scholar]
- [26]. Nowicka P, Flodmark C. Family therapy as a model for treating childhood obesity: Useful tools for clinicians. Clin Child Psychol Psychiatry 2011; 16: 129–145. [DOI] [PubMed] [Google Scholar]
- [27]. Nowicka P, Pietrobelli A, Flodmark C-E. Low-intensity family therapy intervention is useful in a clinical setting to treat obese and extremely obese children. Int J Pediatr Obes 2007; 2: 211–217. [DOI] [PubMed] [Google Scholar]
- [28]. Sherwood NE, JaKa MM, Crain AL, et al. Pediatric primary care-based obesity prevention for parents of preschool children: A pilot study. Child Obes 2015; 11: 674–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29]. Lind BM. CHS nurses’ experiences of Bamse’s Health Conversation during the 4 year health visit at the CHC. In Swedish. Student Thesis, Department of Health Sciences, University West, Sweden: 2017. [Google Scholar]
- [30]. Shih S-F, Liu C-H, Liao L-L, et al. Health literacy and the determinants of obesity: A population-based survey of sixth grade school children in Taiwan. BMC Public Health 2016; 16: 280. [DOI] [PMC free article] [PubMed] [Google Scholar]