Abstract
Compared with other countries, a more substantial decrease in the incidence of invasive pneumococcal disease was observed in Hong Kong, which is most likely attributable to the proactive mass adoption of face masks by the public. Human behavioral changes, particularly mask wearing, should be considered as an additional preventive strategy against invasive pneumococcal disease.
Keywords: COVID-19, invasive pneumococcal disease, Hong Kong
The coronavirus disease 2019 (COVID-19) pandemic has resulted in dramatic human loss worldwide. The first COVID-19 case was confirmed in Hong Kong on 23 January 2020 and was followed by several waves of the disease. As of 31 December 2020, Hong Kong had recorded 8847 confirmed cases, with 26.7% being locally acquired [1]. Overall, Hong Kong has kept a relatively flatter epidemic curve than most other places. This is quite remarkable considering that Hong Kong is an international transport hub, in close proximity to China, and one of the most densely populated areas in the world. The city also did not enter any stage of complete lockdown. Hong Kong is one of the locations most affected by the severe acute respiratory syndrome (SARS) outbreak in 2003 and aggregated a total of 299 deaths, representing the second highest mortality rate, after China. It is believed that the SARS experience largely influenced the personal behavioral changes of citizens in response to the COVID-19 epidemic. In fact, the psychological impact of the SARS outbreak was so huge that hygiene became second nature, and Hong Kong was among the first places to initiate proactive mass adoption of face masks in public areas as personal protection, many months before they were made compulsory by the government in July 2020.
Invasive pneumococcal disease (IPD) is caused by Streptococcus pneumoniae and transmitted via respiratory droplets. Carriage of S. pneumoniae is a prerequisite for developing IPD and is commonly found in young children who are considered the source of pneumococcal infections and spread in the community. Since IPD is a leading cause of death and disease in our locality, it was listed as a statutory notifiable disease in 2015 [2]. Pneumococcal vaccination is one means of preventing IPD, and Hong Kong was among the first Asian cities to include pneumococcal conjugate vaccine in its childhood immunization program in 2009 [2]. The latest recommendation is the 13-valent pneumococcal conjugate vaccine, with a vaccination rate of 99.5% in children. However, vaccination coverage in persons aged ≥65 years remained low, only 45.8% in this high-risk category. Before the COVID-19 pandemic, the IPD incidence in Hong Kong was still high. IPD also causes significant burden of illness in Singapore and Taiwan and was listed as a statutory disease in 2010 and 2007 respectively [3, 4]. Studies in Singapore and Taiwan reported reductions in IPD cases during the first few months of the COVID-19 pandemic [5, 6]. In Singapore, a 42.9% decline of IPD cases in an institution was recorded in the first 27 weeks of 2020, while Taiwan recorded a 50.9% nationwide reduction in IPD cases during the first 8 months of 2020. We hypothesized that the marked behavioral changes among Hong Kong citizens, particularly the proactive mass adoption of face masks, should have a more prominent effect on reducing IPD cases during the COVID-19 pandemic. To test the hypothesis, we analyzed IPD case numbers in 2020 and compared the monthly and yearly trends with the data in the previous 5 years in Hong Kong. We also extended the analysis of IPD case numbers in Singapore and Taiwan to the entire 12-month period in 2020 and compared these numbers with trends from the previous 5 years in Singapore, Taiwan, and Hong Kong.
METHODS
The number of IPD cases before (2015–2019) and during (2020) the COVID-19 pandemic was obtained from the open databases at the Hong Kong Centre of Health Protection, the Ministry of Health of Singapore, and the Taiwan Centers for Disease Control [7–9], respectively. Because IPD is a serious disease that can become life threatening if untreated, individuals would seek prompt medical attention when infected. Therefore, data collected through reportable disease registries truly reflect the actual number of IPD cases in the respective countries. Seasonal autoregressive integrated moving average models were applied to monthly IPD cases in 2015–2019 inclusively to predict those of 2020. We performed stepwise model selection based on the Akaike information criterion (Supplementary Table 1), generating 12-step predictions and prediction intervals for each location to forecast the respective monthly cases in 2020.
RESULTS
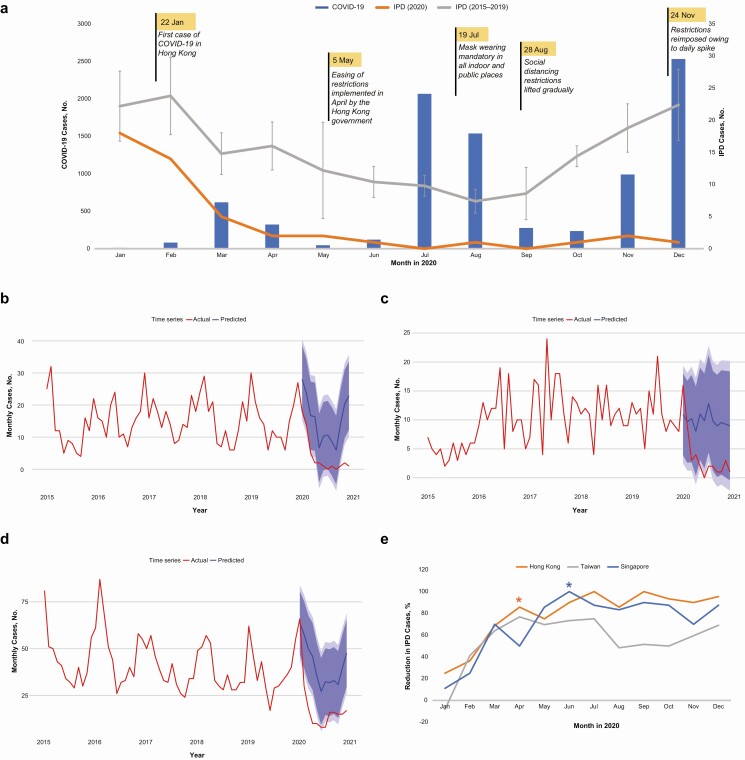
In Hong Kong, a total of 47 IPD cases were reported in 2020, compared with 162–190 yearly cases in 2015–2019 (Supplementary Table 2), for an overall decline of 74.7% (Figure 1A and 1E). Monthly cases in all 12 months during the pandemic were below expectation (Figure 1B and Supplementary Table 3). The dominant S. pneumoniae serotype found was serotype 3, accounting for 45.7% of the total cases in 2020, compared with 44.4%–52.9% in 2015–2019. Similarly, Singapore recorded an overall decrease of 67.2% in IPD cases (Figure 1E). Monthly cases in Singapore were below expectation in 11 of the 12 months (Figure 1C and Supplementary Table 3); 44 cases were reported in 2020, compared with 125–149 yearly in 2015–2019 (Supplementary Table 2). Conversely, Taiwan recorded a less pronounced overall reduction of 47.5% in IPD cases (Figure 1E). Monthly cases in Taiwan were below expectation in 11 of the 12 months (Figure 1D and Supplementary Table 3); 229 cases were reported in 2020, compared with 448–592 yearly in 2015–2019 (Supplementary Table 2). Further statistical analysis revealed that the first significant drops (<95% prediction interval) in IPD cases were observed in April and June for Hong Kong and Singapore, respectively (Figure 1E and Supplementary Table 3).
Figure 1.
A, Numbers of coronavirus disease 2019 (COVID-19) cases (blue bars) and invasive pneumococcal disease (IPD) cases reported in the same monthly periods in Hong Kong in 2020 (orange line) and on average in the years 2015–2019 (black line). Error bars represent 95% confidence intervals for 2015–2019 data. Some important infection control measures and policies implemented by the Hong Kong government are flagged according to their effective dates. B–D, Forecasting monthly IPD cases in 2020 using corresponding fitted seasonal AutoRegressive Integrated Moving Average (ARIMA) models for Hong Kong (B), Singapore (C), and Taiwan (D). Actual monthly cases (red lines) are compared with predicted monthly cases (blue lines) with 90% (dark-blue shading) and 95% (light-blue shading) prediction intervals. E, Percentage reduction in IPD cases in 2020, compared with median number of cases in 2015–2019 in Hong Kong (orange line), Singapore (blue line), and Taiwan (gray line). Asterisks indicate first month (April for Hong Kong and June for Singapore) with a significant drop in IPD cases compared with the corresponding monthly cases in 2015–2019.
DISCUSSION
The marked decline in IPD cases in Hong Kong in 2020 is likely attributable to mask wearing during the COVID-19 pandemic. A marked decrease was observed as early as March (Figure 1A and 1E). This corresponded to the time when Hong Kong citizens responded to the COVID-19 outbreak in China and began to proactively follow a mask-wearing practice, resulting in the first significant drop in IPD cases in April (Figure 1E and Supplementary Table 3). Given the experience learned from SARS, mask wearing was recognized by Hong Kong citizens as an undeniably important means of self-protection and a collective responsibility for reducing COVID-19 transmission. In February 2020, we conducted surveillance on the percentage of mask wearers in public by observing visitors at 3 shopping malls in 3 geographic regions of Hong Kong. Visitors were monitored at the main entrances during lunchtime, the busiest hour of the venues. We found that >99% of people wore masks, including children (Supplementary Figure 1A), consistent with findings reported in previous studies [10]. In addition to mask wearing, hygiene awareness was raised, including increased use of hand sanitizers, improved protection for high-contact surfaces, temperature checking, social distancing and limiting restaurant dining services and gathering sizes (Supplementary Figure 1). In May and August, when the numbers of confirmed local COVID-19 cases were kept low for >3 weeks, restrictions such as limits on gathering sizes and various commercial activities were lifted, and schools reopened. However, the mask-wearing practice was continued, and the number of IPD cases remained low (Figure 1A). Considering that no changes had been made to the pneumococcal vaccination strategy or the reporting requirements, and there was no change of dominant serotype, it is highly likely that proactive actions of the public in response to the COVID-19 pandemic, particularly mask wearing, contributed to the decline in IPD incidence in 2020. This is further supported by a similar marked decline in IPD cases observed in Singapore. After an initial surge in mask usage in January, the Singapore government in February advocated that its citizens use masks only if unwell. In March 2020, measures were reviewed, and masks were made mandatory in April, resulting in a rise in mask wearers from 23% in March to 90% in April [11]. The response in mask wearing was reflected in Singapore’s monthly IPD case numbers, with an average reduction of 39% in January–April, followed by a marked average reduction of 86.4% in May–December (Figure 1B). This corresponded to the first significant drop in IPD cases observed in June (Figure 1E and Supplementary Table 3). Comparatively, Taiwan recorded a relatively smaller reduction of IPD cases compared to Hong Kong and Singapore (Figure 1E). Although initial proactive use of masks in Taiwan was rapid, we speculate that owing to early success (with no local COVID-19 cases for >8 months in 2020) through strict border controls, people in Taiwan were not as compliant with mask usage, and face masks were not mandatory until December 2020. Social distancing restrictions were also eased since June 2020. A recent study in England demonstrated a 30% decline in IPD cases in 2020 compared with 2000–2019 [12]. While England has enforced 3 national lockdowns, only 38% of Britons wear masks in public [11]. Other possible factors leading to reduced host susceptibility may also contribute to the decline in IPD. It is known that viral infections can create favorable conditions in the nasopharyngeal mucosa for colonizing pneumococci to invade, leading to IPD; therefore, reduced influenza transmission during the pandemic may also contribute to the decline in IPD. Further studies can be performed to investigate the pneumococcal carriage and other confounding factors that may contribute to the IPD incidence in Hong Kong.
In conclusion, the current study findings suggest that, in addition to vaccination, human behavioral changes, particularly mask wearing, play key roles in reducing the transmission of S. pneumoniae. These measures should be considered as an additional preventive strategy against IPD.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgment. The authors thank Hwei Huih Lee and Tsz Tuen Li for allowing the use of their images.
Disclaimer. The funding sources had no role in study design, data collection, analysis, interpretation, or writing of the report. The authors alone are responsible for the content and the writing of the manuscript.
Financial support. This work was supported by the Health and Medical Research Fund, the Food and Health Bureau, The Government of the Hong Kong Special Administrative Region, China
Potential conflicts of interest. J. L. L. T. has provided scientific advisory/laboratory services for Pfizer. P. C. Y. W. has provided scientific advisory/laboratory services for Gilead Sciences, International Health Management Associates, Merck, Micología Molecular, and Pfizer. All other authors report no potential conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Centre for Health Protection, Department of Health, Hong Kong. The latest situation of cases of COVID-19. Available at: https://www.chp.gov.hk/files/pdf/local_situation_covid19_en.pdf. Accessed 31 December 2020.
- 2. Ho PL, Law PY, Chiu SS. Increase in incidence of invasive pneumococcal disease caused by serotype 3 in children eight years after the introduction of the pneumococcal conjugate vaccine in Hong Kong. Hum Vaccin Immunother 2019; 15:455–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Eng P, Lim LH, Loo CM, et al. Role of pneumococcal vaccination in prevention of pneumococcal disease among adults in Singapore. Int J Gen Med 2014; 7:179–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wei SH, Chiang CS, Chen CL, Chiu CH. Pneumococcal disease and use of pneumococcal vaccines in Taiwan. Clin Exp Vaccine Res 2015; 4:121–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lim RH, Chow A, Ho HJ. Decline in pneumococcal disease incidence in the time of COVID-19 in Singapore. J Infect 2020; 81:e19–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Juan HC, Chao CM, Lai CC, Tang HJ. Decline in invasive pneumococcal disease during COVID-19 pandemic in Taiwan. J Infect 2020; 82:282–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centre for Health Protection, Department of Health, Hong Kong. Report on IPD. Available at https://www.chp.gov.hk/en/resources/29/636.html. Accessed 31 December 2020.
- 8. Ministry of Health, Singapore. Resources & statistics. Available at https://www.moh.gov.sg/resources-statistics. Accessed 31 December 2020.
- 9. Taiwan Centers for Disease Control. Available at https://www.cdc.gov.tw/. Accessed 31 December 2020.
- 10. Chan KH, Lee PW, Chan CY, Lam KBH, Ho PL. Monitoring respiratory infections in COVID-19 epidemics. BMJ 2020; 369:m1628. [DOI] [PubMed] [Google Scholar]
- 11. He E, Laurent L.. The world is masking up, some are opting out. Bloomberg. 2020. Available at: https://www.bloomberg.com/graphics/2020-opinion-coronavirus-global-face-mask-adoption/. Accessed 31 December 2020. [Google Scholar]
- 12. Amin-Chowdhury Z, Aiano F, Mensah A, Sheppard CL, et al. Impact of the coronavirus disease 2019 (COVID-19) pandemic on invasive pneumococcal disease and risk of pneumococcal coinfection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): prospective national cohort study, England. Clin Infect Dis 2021; 72:e65-e75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.