Abstract
Background
COVID-19 has impacted more than 200 countries. However in the USA, the response to the COVID-19 pandemic has been politically polarized. The objective of this study is to investigate the association between political partisanship and COVID-19 deaths rates in the USA.
Methods
This study used longitudinal county-level panel data, segmented into 10 30-day time periods, consisting of all counties in the USA, from 22 January 2020 to 5 December 2020. The outcome measure is the total number of COVID-19 deaths per 30-day period. The key explanatory variable is county political partisanship, dichotomized as Democratic or Republican. The analysis used a ZINB regression.
Results
When compared with Republican counties, COVID-19 death rates in Democratic counties were significantly higher (IRRs ranged from 2.0 to 18.3, P < 0.001) in Time 1–Time 5, but in Time 9–Time10, were significantly lower (IRRs ranged from 0.43 to 0.69, P < 0.001).
Conclusion
The reversed trend in COVID-19 death rates between Democratic and Republican counties was influenced by the political polarized response to the pandemic. The findings support the necessity of evidence-based public health leadership and management in maneuvering the USA out of the current COVID-19 pandemic and prepare for future public health crises.
Introduction
COVID-19 has had a devastating impact on countries globally, spreading to more than 200 countries.1 While some countries have been able to control and gradually recover from the outbreak, the USA has been unsuccessful in containing the effects of the COVID-19 pandemic. Although the USA has about 4.2% of the world’s population, it has 19% of the world’s total COVID-19 deaths.2 As of 31 December 2020, the USA leads the world with both the highest recorded confirmed COVID-19 cases (20 026 231 confirmed cases) and confirmed deaths due to COVID-19 (345 866 deaths).1 In 2021, the COVID-19 pandemic is predicted to get worse in the USA, with expected increases in the rates of both the number of confirmed cases and deaths.
In an attempt to contain the spread and reduce the direct risk of exposure to COVID-19, the Centers for Disease Control and Prevention (CDC) and public health state agencies recommended preventive behaviors, such as wearing masks, voluntary social distancing, cleaning guidelines, hand washing and shelter-in-place orders, to protect individuals until the availability of a vaccine.3 Compliance with these preventive behaviors not only protects individuals themselves but also creates positive externalities by slowing the spread of the virus, lowering the risk of infecting others and significantly curtailing deaths.4,5
However, the extent to which states and individuals adhere to the COVID-19 guidelines has become politically polarized, furthering the divide between partisan groups. For instance, a state’s political orientation appears to determine the timing and duration of shelter-in-place orders, business lockdowns and mask mandates in response to COVID-19.6,7 Media outlets further influenced partisan behaviors, by delivering mixed messages about the seriousness of COVID-19 and importance of preventive behaviors, which have biased individual attitudes and responses to the COVID-19 virus.8,9 Individuals who identify as Democrats are more willing to comply with COVID-19 guidelines versus individuals who identify as Republicans.10–12 Given the variation in response to the COVID-19 pandemic due to political party affiliation, partisanship may be a risk factor for the rising rates of the COVID-19 pandemic in 2020 and in the future.
This study proposes to investigate the trend in COVID-19 death rates between Democratic and Republican counties. The authors hypothesize that the county political party affiliation is associated with the disparities in county-level COVID-19 death rates. As the political divide has deepened in recent decades,13 the results from this study will emphasize the public health implications of managing a pandemic under a political polarized environment.
Methods
Data sources and study sample
The study utilized county-level data. COVID-19 confirmed cases and deaths at the county-level were downloaded from USAFacts from 22 January 2020 through 5 December 2020.14 County-level political partisan was determined using the 2016 U.S. presidential election results available from The New York Times.15 County-level demographics and characteristics were obtained from the Area Health Resource File.16 All data sets were merged using the 5-digit County Federal Information Processing Standard code identifiers.
The study sample was a longitudinal, balanced panel consisting of all counties in the 50 US states and the District of Columbia. The data were segmented into 10 30-day time periods: (i) Time 1: 10 February 2020 to 10 March 2020, (ii) Time 2: 11 March 2020 to 9 April 2020, (iii) Time 3: 10 April 2020 to 9 May 2020, (iv) Time 4: 10 May 2020 to 8 June 2020, (v) Time 5: 9 June 2020 to 8 July 2020, (vi) Time 6: 9 July 2020 to 7 August 2020, (vii) Time 7: 8 August 2020 to 6 September 2020, (viii) Time 8: 8 August 2020 to 6 September 2020, (ix) Time 9: 7 October 2020 to 5 November 2020 and (x) Time 10: 6 November 2020 to 5 December 2020. Since the first death from COVID-19 was recorded on 10 February 2020, the time period prior to this date (22 January 2020 to 9 February 2020) was excluded from the analysis. Counties with no residents were excluded from the final sample. The final study sample consisted of 3140 counties (31 400 county-month observations).
Variable definitions
Dependent variable
The outcome measure is the total number of COVID-19 deaths for each county for each respective 30-day time period. The COVID-19 deaths are confirmed by laboratory evidence for COVID-19 or by meeting clinical criteria and epidemiological evidence as established by the CDC.17 For the study period, there were a total of 275 861 COVID-19 deaths.
Key explanatory variable
There are three key explanatory variables: (i) a dichotomous variable for Democratic counties that had the majority of votes for Hilary Clinton in 2016, with the counties that had the majority of votes for Donald Trump as the reference group; (ii) a set of time dummies for Time 2–Time 10 (30 days in length each Time), with Time 1 as the reference group; and (iii) an interaction between Democratic counties and each time period indicator, which provides the change in the number of COVID-19 deaths for each time period between Democratic and Republican counties.
Confounding variables
A series of county-level characteristics were included in the model: two dichotomous variables for Micropolitan and rural counties (Metropolitan counties as the referent category) as measures of geography; the total number of confirmed COVID-19 cases for each county for each of the 10 time periods, which provides a measure of magnitude and spread of the disease over the study time period; population density, calculated as the number of people per square mile,18 which has been theorized to influence the rate of spread of infection and eventually increasing the likelihood of dying from COVID-19;19 and the total hospital beds per 1000 population measures access and available healthcare resources to respond to increasing demand of COVID-19 patients and mitigating preventable deaths.20 Since COVID-19 has a disproportionate impact on deaths for the elderly, impoverished people, racial and ethnic minorities, and individuals with underlying conditions,21,22 the percent seniors (age ≥ 65 years), median household income, percentage of African Americans and Hispanic/Latino population, and the Centers for Medicare and Medicaid Services (CMS) Hierarchical Condition Category (HCC) risk scores23 at the county level were used as indicators of sociodemographic and clinical factors.
Statistical analysis
Descriptive statistics were used to summarize the county-month level data. Bivariate analyses (t-tests for continuous variables and chi-square tests for categorical variables) were used to test the differences on each measure between Democratic and Republican counties. Statistical significance was set at α < 0.05 for all analyses. The data management and analysis were performed using Stata 14.0 (College Station, TX).
A zero-inflated negative binomial (ZINB) regression was used for the analysis because there are a large proportion of counties with no deaths during the study time period and the number of COVID-19 deaths per county are highly skewed and over-dispersed.24,25 This model considers two pathways. One pathway uses the negative binomial regression model. The interaction between the county political partisanship variable and each time period measures the difference in COVID-19 deaths between Democratic and Republican counties during the each time period. This part of the regression included county-level confounders. The other pathway uses a logistic regression model to estimate the likelihood of no deaths from COVID-19, commonly referred to as ‘excess zeros’ (e.g. survival due to not contracting COVID-19). This part of the regression included population density and the county-level confirmed COVID-19 cases. The number of county-level confirmed COVID-19 cases is negatively associated with ‘excess zero’ deaths, while the population density is positively associated with ‘excess zero’ deaths.19
Finally, states implemented policies and deployed resources to control the pandemic, which influence residents’ likelihood of exposure and death from COVID-19.12 To control for the state-level fixed effects, the ZINB model included clustering at the state-level. To ease interpretation, the ZINB model coefficients are presented as incidence rate ratios (IRRs) for the negative binomial regression part of the analysis and odds ratios for the logistic regression part of the analysis.
Results
For the 10 time periods, the final study sample included 31 400 county-month observations (3140 counties). There were 4860 Democratic county-month observations (486 counties) and 26 540 Republican county-month observations (2654 counties).
Figure 1 displays the average COVID-19 mortality per 100 000 population per time period for Democratic and Republican counties. The average COVID-19 mortality rate in Democratic counties initially increases, reaching the highest rate in Time 3 (16.4 per 100 000), followed by an overall gradual decrease for the remaining time periods. During the same time period, in Republican counties, the average COVID-19 mortality rate progressively increased, reaching the highest rates in Time 10 (27.4 per 100 000). During the first 7 time periods, Democratic counties have a higher average COVID-19 mortality rate compared with Republican counties. This trend reverses in Time 9 and Time 10, where Republican counties experience a higher average COVID-19 mortality rate than Democratic counties.
Fig. 1.
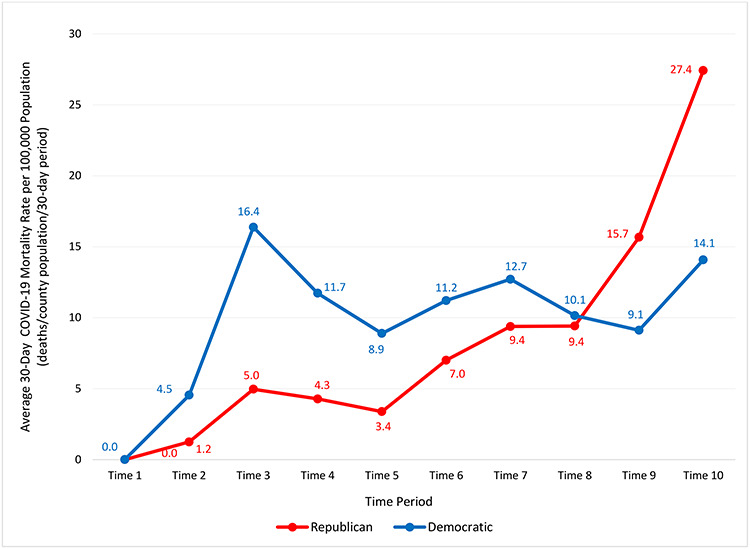
Average COVID-19 mortality rate per 100 000 population per time period for Democratic and Republican Counties. (Time 1: 10 February 2020 to 10 March 2020; Time 2: 11 March 2020 to 9 April 2020; Time 3: 10 April 2020 to 9 May 2020; Time 4: 10 May 2020 to 8 June 2020; Time 5: 9 June 2020 to 8 July 2020; Time 6: 9 July 2020 to 7 August 2020; Time 7: 8 August 2020 to 6 September 2020; Time 8: 7 September 2020 to 6 October 2020; Time 9: 7 October 2020 to 5 November 2020; Time 10: 6 November 2020 to 5 December 2020).
Figure 2 displays the unadjusted total number of COVID-19 deaths for Democratic and Republican counties during the 10-month time period. While the total number of COVID-19 deaths is higher for Democratic counties in the first 7 time periods, from Time 8 through Time 10, the trend in total number of COVID-19 deaths reverses with Republican counties experiencing a higher total number of COVID-19 deaths. Both Figures 1 and 2 confirm the study hypothesis that county-level political partisanship is associated with COVID-19 deaths.
Fig. 2.
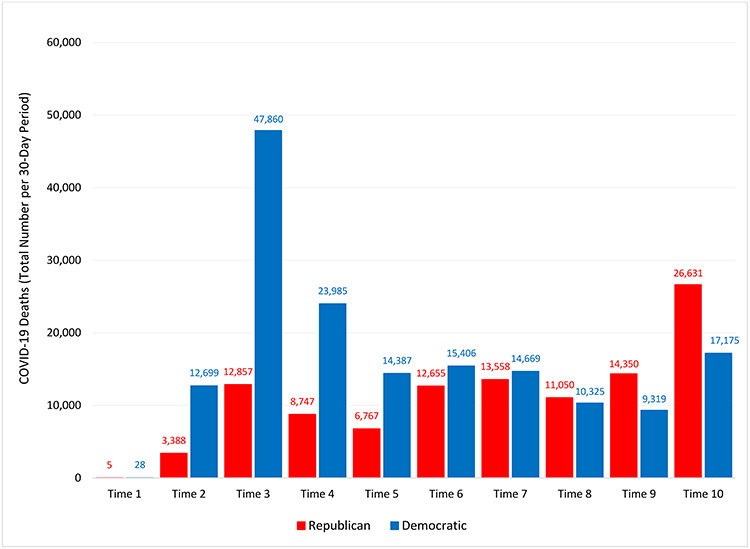
Total COVID-19 deaths for Republican and Democratic Counties (Time 1: 10 February 2020 to 10 March 2020; Time 2: 11 March 2020 to 9 April 2020; Time 3: 10 April 2020 to 9 May 2020; Time 4: 10 May 2020 to 8 June 2020; Time 5: 9 June 2020 to 8 July 2020; Time 6: 9 July 2020 to 7 August 2020; Time 7: 8 August 2020 to 6 September 2020; Time 8: 7 September 2020 to 6 October 2020; Time 9: 7 October 2020 to 5 November 2020; Time 10: 6 November 2020 to 5 December 2020).
Table 1 presents descriptive statistics for study variables between Democratic or Republican counties. The average COVID-19 deaths and confirmed cases per month were higher for Democratic counties (34.1 deaths and 1536.1 confirmed cases) compared with Republican counties (4.1 deaths and 257.5 confirmed cases). Additionally, several county characteristics between Democratic counties and Republican counties are different. For example, Democratic counties, compared with Republican counties, have a higher population density per square mile (1149.8 versus 96.2), more total hospital beds per 1000 population (3.3 versus 2.9), higher unemployment rate (4.4 versus 4.1%) and higher median household income ($55 530 versus $50 290), as well as a larger percentage of African Americans (21.3 versus 6.5%) and the population ≥ 65 years (19.3 versus16.2%).
Table 1.
Summary statistics of the study variables by county political partisanship (N = county-month observations)
| All Counties (N = 31 400 county-month observations based on 3140 counties) | Democratic Counties (4860 county-month observations based on 486 counties) | Republican Counties (26 540 county-month observations based on 2654 counties) | P-value | |
|---|---|---|---|---|
| Death COVID-19 Cases [Mean (SD)] | 8.8 (61.0) | 34.1 (146.4) | 4.1 (18.7) | <0.001 |
| Confirmed COVID-19 Cases [Mean (SD)] | 455.4 (2186.8) | 1536.1 (4893.7) | 257.5 (1010.1) | <0.001 |
| Metropolitan Counties [n (%)] | 11 810 (37.6) | 3090 (63.6) | 8720 (32.9) | <0.001 |
| Micropolitan Counties [n (%)] | 6600 (21.0) | 870 (17.9) | 5730 (21.6) | |
| Rural Counties [n (%)] | 13 010 (41.4) | 900 (18.5) | 12 090 (45.6) | |
| Population density per square mile [Mean (SD)] | 259.3 (1724.7) | 1149.8 (4238.8) | 96.2 (240.5) | <0.001 |
| Total hospital beds (per 1000 population) [Mean (SD)] | 3.0 (4.9) | 3.3 (6.5) | 2.9 (4.6) | <0.001 |
| Health status (CMS HCC score) [Mean (SD)] | 1.0 (.1) | 1.0 (.1) | 0.9 (.1) | <0.001 |
| Percent population ≥ 65 years [Mean (SD)] | 18.8 (4.7) | 16.2 (4.1) | 19.3 (4.6) | <0.001 |
| Unemployment rate [Mean (SD)] | 4.1 (1.5) | 4.4 (1.7) | 4.1 (1.4) | <0.001 |
| Percent population Black or African American [Mean (SD)] | 8.8 (14.4) | 21.3 (23.9) | 6.4 (10.3) | <0.001 |
| Percent population Hispanic/Latino [Mean (SD)] | 8.3 (13.2) | 14.9 (21.3) | 7.1 (10.7) | <0.001 |
| Percent population Other Race [Mean (SD)] | 0.1 (.1) | .2 (.3) | .1 (.1) | <0.001 |
| Median household income (/$1000) [Mean (SD)] | 51.1 (13.5) | 55.5 (20.2) | 50.3 (11.7) | <0.001 |
| Time Period: | 1.00 | |||
| Time 1 (10 February 2020 to 10 March 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 2 (11 March 2020 to 9 April 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 3 (10 April 2020 to 9 May 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 4 (10 May 2020 to 8 June 020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 5 (9 June 2020 to 8 July 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 6 (9 July 2020 to 7 August 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 7 (8 August 2020 to 6 September 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 8 (7 September 2020 to 6 October 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 9 (7 October 2020 to 5 November 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
| Time 10 (6 November 2020 to 5 December 2020) [n (%)] | 3140 (10.0) | 486 (10.0) | 2654 (10.0) | |
Table 2 presents the adjusted IRR for each time period between the Democratic and Republican counties after controlling for confounders. The IRR was calculated using the regression coefficients from county political partisanship and the interaction between the time periods and county political partisanship from the ZINB regression model (full model available in Supplemental Appendix). From Time 1 through Time 5, the IRR of COVID-19 deaths is significantly higher (IRR ranged from 2.0–18.3, P < 0.001) for Democratic counties compared with Republican counties. However, the IRR of COVID-19 deaths gradually decreased and became non-significant between both counties from Time 6 through Time 8 (P > 0.05). In Time 9 and Time 10, the IRR of COVID-19 death is significantly lower (P < 0.001) for Democratic counties compared with Republican counties, and the difference in the IRR between the Democratic and Republican counties has steadily increased.
Table 2.
Adjusted IRR for each time period between the Democratic and Republican Counties
| Time period | IRR | 95% Confidence interval |
|---|---|---|
| Time 1 (10 February 2020 to 10 March 2020) | 18.3*** | (2.5, 131.4) |
| Time 2 (11 March 2020 to 9 April 2020) | 2.2*** | (1.8, 2.7) |
| Time 3 (10 April 2020 to 9 May 2020) | 2.0*** | (1.6, 2.6) |
| Time 4 (10 May 2020 to 8 June 2020) | 2.2*** | (1.7, 2.9) |
| Time 5 (9 June 2020 to 8 July 2020) | 2.4*** | (1.7, 3.2) |
| Time 6 (9 July 2020 to 7 August 2020) | 1.1 | (8.5 × 10−1, 1.4) |
| Time 7 (8 August 2020 to 6 September 2020) | 9.7 × 10−1 | (7.9 × 10−1, 1.2) |
| Time 8 (7 September 2020 to 6 October 2020) | 1.1 | (8.9 × 10−1, 1.3) |
| Time 9 (7 October 2020 to 5 November 2020) | 6.9 × 10−1*** | (5.8 × 10−1, 8.3 × 10−1) |
| Time 10 (6 November 2020 to 5 December 2020) | 4.3 × 10−1*** | (3.7 × 10−1, 5.2 × 10−1) |
* = P < 0.05; ** = P < 0.010; *** = P < 0.001
Adjusted IRR for each time period between the Democratic and Republican counties are calculated using the ZINB regression results from Appendix by  .
.
Discussion
Main finding of this study
The results confirm the research hypothesis that after controlling for confounders, COVID-19 deaths vary by county-level political partisanship. At the start of the COVID-19 pandemic, higher COVID-19 death rates were recorded in Democratic versus Republican counties. As the pandemic progressed, the trend in county-level COVID-19 death rates reversed, with Republican county rates surpassing Democratic county rates. By the end of the study period, Republican counties recorded higher COVID-19 death rates compared with Democratic counties, with expectations that differences in rates will widen in the future if evidence-based interventions are not implemented.
What is already known on this topic
The response to the COVID-19 pandemic has been politically polarized,6,7,10–12 which has resulted in differences in COVID-19 mortality rates between Democratic and Republican counties. It has been reported that Republican-led states experienced lower mortality rates compared with Democratic-led states from March to the beginning of July, but then Republican-led states experienced higher mortality rates than Democratic-led states after the beginning of July.26 At the county level, a similar trend was observed—the number of COVID-19 deaths was rising faster in Republican counties than in Democratic counties. These results were either based on data reported before June11 or were not adjusted for county-level risk factors.27 The adjusted differences in COVID-19 mortality rates between county level partisanship affiliations are unknown.
What this study adds
This study used 10 months of data at the county level from February 2020 to December 2020 and includes county-level risk factors, which may influence COVID-19 mortality. In addition, this study applies a longitudinal panel design with a difference-in-difference framework. This framework estimates the differences in COVID-19 mortality trends between Democratic and Republican counties for every 30-day period during the study period.
If states and individuals, regardless of political partisanship, implemented and adhered to evidenced-based approaches to manage the COVID-19 pandemic, theoretically, mortality rates in Republican counties may have had a lower likelihood of exceeding rates in Democratic counties. Unfortunately, mortality rates in Republican counties have surpassed rates in Democratic counties, and the partisan variation continues to widen. This outcome may be explained by the divided responses to the pandemic at individual and state levels due to political affiliations.6,7,10,11
The observed trend in COVID-19 death rates between Democratic and Republican counties may be attributed to the externalities associated with state-level public health interventions. Negative externalities result from non-compliance with preventive behaviors, resulting in COVID-19 spreading quickly through communities, leading to increases in confirmed cases and subsequent deaths.28 The observed upward trend in COVID-19 death rates in Republican counties may be due to negative externalities related to non-compliance with preventive behaviors. Positive externalities result from implementation of evidence-based policies and individual compliance with guidelines, reducing the spread of the virus and negative outcomes.5 The observed downward trend in COVID-19 death rates in Democratic counties may be due to positive externalities related to compliance with preventive behaviors.
Limitations of the study
This study has few limitations. First, county-level political partisanship was determined using the 2016 election results and considered a proxy for COVID-19 guideline compliance. Counties were identified as Democratic or Republican according to the majority of votes in the 2016 federal election. County-level political partisanship cannot be generalized to all county residents, since a proportion of residents may have voted for other political parties. However, according to research regarding the politically polarized response to COVID-19, the 2016 federal election results are an acceptable proxy for the variation in compliance and county-level policies between political parties. Second, county-level HCC risk scores were used as a measure of the county’s underlying health conditions. The HCC risk scores are based on Medicare population,23 which do not reflect the underlying health conditions of the county population.
Regardless of these limitations, the findings from this study have important public health implications. First, evidence-based public health leadership and management without political interference is the ideal approach to lead the USA out of the COVID-19 pandemic since the virus affects individuals irrespective of their political affiliations. Current efforts focusing on transparency of COVID-19 facts and data, accessibility of vaccines and a top-down coordinated approach led by the federal government are moving in the right direction. However, a collaborative approach involving partnerships with federal, state and local public health agencies is necessary.
Second, politically polarized attitudes and behaviors have created challenges in controlling the spread of the COVID-19 pandemic. While the US Constitution protects individuals’ liberties and rights, exercising these liberties and rights during a pandemic compromises the health and safety of the country’s residents, creating unnecessary harm. In order to protect the safety of the public and promote adherence to preventive behaviors, implementation of regulations and fines, such as mandating facemasks in public areas, may be warranted to ensure compliance and contain the spread of infection at the individual levels.
Lastly, the K-12 education system provides an ideal platform to educate younger generations about the implications of public health strategies on population health. The experience from the COVID-19 pandemic provides a window of opportunity to educate students about the value and significance of evidenced-based approaches to managing public health emergencies. Educators, public health officials and other professionals should form partnerships and collaborate to create a curriculum that may be implemented at various stages in the K-12 education system. The challenges of leading public health practices under a political polarized environment becomes a reality, especially when the political polarization has been further divided in the recent decades.13 Educating the next generation provides a chance to manage the political influence while controlling the impact of contiguous diseases in the future.
In conclusion, COVID-19 pandemic has brought public health to the forefront. Public health participation and leadership is recognized as an essential component to successfully manage a public health crisis. In past events, public health has played a role in eradicating and controlling spread of diseases such as smallpox, polio and HIV. Evidence-based public health leadership and management is essential to lead the USA out of the current COVID-19 crisis and to prepare for future public health crises.
Saleema A. Karim, Associate Professor
Hsueh-Fen Chen, Associate Professor
Contributor Information
Hsueh-Fen Chen, Department of Healthcare Administration and Medical Informatics, Kaohsiung Medical University, 100, Shih-Chuan 1st Road, Kaohsiung 80708, Taiwan.
Saleema A Karim, Department of Health Policy and Management, University of Arkansas for Medical Sciences, Little Rock, AR 72205, USA.
Reference
- 1. World Health Organization . WHO Coronavirus Disease (COVID-19) Dashboard. World Health Organization. https://covid19.who.int/ (Published 2021; 5 January 2021, date last accessed).
- 2. The United States Census Bureau . U.S. and World Population Clock. https://www.census.gov/popclock/ (5 January 2021, date last accessed).
- 3. Centers for Disease Control and Prevention . How COVID-19 Spreads. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html (Published 2020; 5 July 2020, date last accessed).
- 4. Cato S, Iida T, Ishida K et al. Social distancing as a public good under the COVID-19 pandemic. Public Health 2020;188:51–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Okyere MA, Forson R, Essel-Gaisey F. Positive externalities of an epidemic: the case of the coronavirus (COVID-19) in China. J Med Virol 2020;92(9):1376–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dave D, Friedson AI, Matsuzawa K, Sabia JJ. When do shelter-in-place orders fight COVID-19 best? Policy heterogeneity across states and adoption time. Econ Inq 2021;59(1):29–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Adolph C, Amano K, Bang-Jensen B et al. Pandemic politics: timing state-level social distancing responses to COVID-19. J Health Polit Policy Law 2021;46(2):211–33. [DOI] [PubMed] [Google Scholar]
- 8. Simonov A, Sacher SK, Dube’ JBS. The persuasive effect of fox news: non-compliance with social distancing during the COVID-19 pandemic. 1050 Massachusetts Avenue Cambridge, MA 02138: https://www.nber.org/system/files/working_papers/w27237/w27237.pdf. [Google Scholar]
- 9. Zhao E, Wu Q, Crimmins EM, Ailshire JA. Media trust and infection mitigating behaviours during the COVID-19 pandemic in the USA. BMJ Glob Heal 2020;5(10):e003323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Allcott H, Boxell L, Conway J et al. Polarization and public health: partisan differences in social distancing during the coronavirus pandemic. J Public Econ 2020;191:104254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gollwitzer A, Martel C, Brady WJ et al. Partisan differences in physical distancing are linked to health outcomes during the COVID-19 pandemic. Nat Hum Behav 2020;4(11):1186–97. [DOI] [PubMed] [Google Scholar]
- 12. Grossman G, Kim S, Rexer JM, Thirumurthy H. Political partisanship influences behavioral responses to governors’ recommendations for COVID-19 prevention in the United States. Proc Natl Acad Sci U S A 2020;117(39):24144–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jong A. Ideological divides among partisans deepen: ABC news polling analysis. https://abcnews.go.com/Politics/ideological-divides-partisans-deepen-abc-news-polling-analysis/story?id=71718386 (28 February 2021, date last accessed).
- 14. USAFACTS . US Coronavirus Cases & Deaths by State: track COVID-19 data daily by state and county. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/ (Published 2021; 6 January 2021, date last accessed).
- 15. The New York Times . Presidential Election Results. The New York Times, 2016. [Google Scholar]
- 16. Department of Health Resources and Services Administration . County-Level Data: Area Health Resources File 2018–2019. https://data.hrsa.gov/data/download (2 June 2019, date last accessed).
- 17. Centers for Disease Control and Prevention . FAQ: COVID-19 Data and Surveillance. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/faq-surveillance.html#Understanding-the-Data (Published 2020; 27 January 2021, date last accessed).
- 18. Cohen D. Understanding Population Density. The United Census Bureau. https://www.census.gov/newsroom/blogs/random-samplings/2015/03/understanding-population-density.html (Published 2015; 20 January 2021, date last accessed). [Google Scholar]
- 19. Hamidi S, Sabouri S, Ewing R. Does Density Aggravate the COVID-19 Pandemic? J Am Plan Assoc. 2020;86(4):495–509. [Google Scholar]
- 20. Son K-B, Lee T, Hwang S. Does the health system’s response matter to cope with the COVID-19 outbreak? Recent evidence from South Korea. Bulletin of the World Health Organization. https://www.who.int/bulletin/online_first/20-257758.pdf (Published 2020). [Google Scholar]
- 21. Chen T, Wu DI, Chen H et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tai DB, Shah A, Doubeni CA et al. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis 2021;72(4):703–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. The Centers for Medicare and Medicaid Services . Advance Notice of Methodological Changes for Calendar Year (CY) 2020 for the Medicare Advantage (MA) CMS-HCC Risk Adjustment Model. https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/Downloads/Advance2020Part1.pdf (27 January 2021, date last accessed).
- 24. Tang W, Lu N, Chen T et al. On performance of parametric and distribution-free models for zero-inflated and over-dispersed count responses. Stat Med 2015;34(24):3235–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. He H, Wang W, Hu J et al. Distribution-free inference of zero-inflated binomial data for longitudinal studies. J Appl Stat 2015;42(10):2203–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Neelon B, Mutiso F, Mueller NT et al. Associations between governor political affiliation and COVID-19 cases, deaths, and testing in the US. American Journal of Preventive Medicine 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bump P. The shift of the coronavirus to primarily red states is complete — but it’s not that simple. The Washington Post. https://www.washingtonpost.com/politics/2020/06/24/shift-coronavirus-primarily-red-states-is-complete-its-not-that-simple/ (Published 2020). [Google Scholar]
- 28. Lee JN, Mahmud M, Morduch J et al. Migration, externalities, and the diffusion of COVID-19 in South Asia☆. J Public Econ 2021;193:104312. [DOI] [PMC free article] [PubMed] [Google Scholar]


