Abstract
Public health faces unprecedented challenges in its efforts to control COVID-19 through a national vaccination campaign. Addressing these challenges will require fundamental changes to public health data systems. For example, of the core data systems for immunization campaigns is the immunization information system (IIS); however, IISs were designed for tracking the vaccinated, not finding the patients who are high risk and need to be vaccinated. Health systems have this data in their electronic health records (EHR) systems and often have a greater capacity for outreach. Clearly, a partnership is needed. However, successful collaborations will require public health to change from its historical hierarchical information supply chain model to an ecosystem model with a peer-to-peer exchange with population health providers. Examples of the types of informatics innovations necessary to support such an ecosystem include a national patient identifier, population-level data exchange for immunization data, and computable electronic quality measures. Rather than think of these components individually, a comprehensive approach to rapidly adaptable tools for collaboration is needed.
Keywords: public health informatics, population health, national patient identifier, Fast Healthcare Interoperability Resource, electronic clinical quality measure
INTRODUCTION: PUBLIC HEALTH AND POPULATION HEALTH EFFORTS FOR PANDEMIC CONTROL
In the previous century, healthcare providers looked after the care of individuals, and public health looked after the care of populations. However, this paradigm has changed. Health systems now practice population health,1 caring for groups of patients who are “at-risk” through value-based reimbursement. A recent survey suggests that about 53% of care is value-based.2 There are recognized quality metrics that reward health systems for performance of essential tasks at a population level, with ongoing efforts to compute these quality metrics, such as rates of vaccination of patients for influenza, from data in electronic health records systems (EHRs).3 Many health systems and other healthcare providers, such as pharmacies, have data warehouses linked to electronic dashboards that show the health system’s day-to-day performance on other population health measures. These systems offer advanced capabilities that would be the envy of many public health practitioners.
The events of the past year have revealed fundamental weaknesses in public health data systems due to years of under funding. As a foundation for efforts for the next phase of the pandemic and future preparedness, we need to make significant national investments in public health data systems. But what kind of investments? Rather than invest in purpose-built systems that address the issues of the most recent public health disaster, we need an “all hazards” approach. In addition, the next generation of public health data systems needs to be designed for collaboration. Traditional public health data management models placed public health providers at the top of a hierarchical information “supply chain,” supporting policy decisions.4,5 COVID-19, and many other public health problems, require public health to move beyond its vertically oriented tools to establish an information “ecosystem” with n-direction communication among public health and population health providers,6,7 with the goal of an independent but coordinated response to the challenges of the pandemic or other public health emergency at a population level.
COVID-19 AND POPULATION HEALTH INFRASTRUCTURE
COVID-19, like most infectious diseases, is an illness that disproportionately affects vulnerable populations: the aged, those with serious prior illnesses, minorities, and individuals with health disparities.8 It also selectively affects individuals in work environments where social distancing and mask use is difficult such as in meatpacking and service industries.9 Fighting the pandemic requires a population health perspective. Who are the vulnerable? How do we reach them? As this pandemic has revealed, sometimes the vulnerable are persons supporting critical infrastructure such as teachers or food processors.10 As we move into the next phase of care of COVID-19, vaccination of the vulnerable populations based on risk and vaccine availability is critical to mitigating loss of life and health.11 The providers caring for populations must be able to carefully track and target for intervention-specific subpopulations of patients, based on CDC and jurisdictional guidelines. But, knowing who in a provider’s population has, and perhaps more importantly, who has not been vaccinated will be difficult.
Involving providers in vaccination campaigns is critical because vaccinating a population as diverse as the United States will be difficult. Even with wide availability, achieving uptake of the vaccines may experience difficult grassroots resistance.12 Many persons may need outreach and intervention from a trusted party, such as a healthcare provider, to accept vaccination. So systems for getting data back to healthcare practitioners, in the long run, will be critical. Moreover, when vaccines become widely available, events could make them scarce again. The evolution of Sars-COV-2 has not so far required reengineering of existing vaccines,13 but this is possible and may result in a need for ongoing revaccination, keeping vaccines a scarce commodity.
Further, the United States’ approach to delivering vaccinations is disjointed. Many providers are being engaged to administer vaccines, including nontraditional ones such as pharmacy chains. New approaches are being implemented, such as drive-through sites for mass vaccinations.14 Patients, freed of the responsibility for payment, are seeking vaccinations where it is convenient for them and when they decide to participate.15,16 As a result, no single provider is likely to hold comprehensive vaccination data on its population of patients. Providers need to look to public health data systems for this information. But there are a number of barriers. Three important ones that have informatics solutions are discussed below.
A COVID-19 SPECIFIC NATIONAL PATIENT IDENTIFIER AND DISAMBIGUATION TECHNOLOGY
First and foremost, a national vaccination campaign needs consistent national-level tools for disambiguation of patients’ identity. A single national medical identifier would be a useful approach but is still a controversial issue because of privacy concerns.17–19 During the pandemic, the Office of the National Coordinator for Health Information Technology has accelerated its research to develop other approaches for disambiguating patient identities.20 However, both public health and healthcare providers urgently need an operational solution. One option might be a pandemic-specific-identifier based on the best available technology. Such a solution might not need to be as precise as a permanent identifier and could be discarded after the resolution of the pandemic. The identifier should be a health identifier, under the legal protection of the Health Insurance Portability and Accountability Act (HIPAA), and authorized only for use by public health officials and providers for outreach to patients where they have existing relationships, to protect privacy. Whether permanent or temporary, only with adequate infrastructure for patient identity resolution, linked to public health data, can we know who has and has not been vaccinated and conduct systematic, risk-based individual outreach to those who have not.
DATA SYSTEMS DESIGNED FOR RAPIDLY EVOLVING COLLABORATION ON POPULATION HEALTH
Data systems for public health are siloed by jurisdiction (by law), but also by program (as a result of federal funding restrictions.) However, effective data systems could share many components, making them more interoperable and flexible.7 One such component could be the identity disambiguation tools described above. A second might be a database designed to support population health level queries that allow a healthcare system to know what public health knows about its patients. Basic components such as these could be assembled into program-specific systems that are cost-effective, interoperable, and adaptable to new challenges, as described in Lenert and Sundwall.7
Applying these principles to vaccination campaigns, the primary tool public health has for assessing the effectiveness of vaccine campaigns are state and regional immunization information systems (IIS).21 These systems, in turn, provide data to the Centers for Disease Control and Prevention (CDC) for national statistics and policy formation. There are approximately 60 disparate states and jurisdictional IIS systems that are linked only at the CDC (national level). IIS systems functions include: 1) tracking administration of vaccine supplies to authorized providers and to support the logistics of vaccine distribution; 2) ongoing population-level assessment on the effectiveness of immunization campaigns (by race, ethnicity, gender, and geolocation); and 3) provision of information to clinicians on the vaccine status of individuals. IIS capabilities have advanced under Meaningful Use regulations.22 Most EHR systems now automatically send standardized HL7 version 2.X vaccination messages to state IIS systems.23,24 Many IIS provide web interfaces for patient-level or clinical provider level queries on the vaccination status of individuals and some provide recommendations for future vaccinations.22
IISs are unique in public health data systems because they are among the most collaborative of public health data systems with existing capabilities for 2-way communication with healthcare providers. IISs were created to send population-level data back “upstream” to the CDC. Their uniqueness comes from how they obtained this data. Prior to Meaningful Use, healthcare providers voluntarily contributed patient data to vaccination registries to be part of a community maintaining accurate records for patients across healthcare systems. By meeting the information needs of healthcare providers, public health acquired the data it needed for operations.
Our present circumstances require similar collaborations but scaled for population health practice—moving from collaboration 1 patient at a time to large groups of patients at a time. From an informatics standpoint, a population-based program within a healthcare provider would require the creation of a registry of targeted patients which might be very large—tens of thousands of patients or more at later stages in vaccine distribution. A team of population health specialists might prioritize that provider’s patients by their risk and try to contact patients, in order of risk, to help them “navigate” access to vaccination appointments.25,26 To do this in an efficient manner, the registry software might need to check on the vaccination status of hundreds or even tens of thousands of patients every day. As a result, a jurisdictional IIS might need to be able to respond to potentially millions of queries a day. Operationally, processing this number of data requests, 1 at a time, would be challenging even for the most technically sophisticated IISs.
There is a potentially rapidly deployable solution that might also serve as the foundation for the next generation of public health systems: “wrapping” existing IIS systems in interoperable database technology designed for “bulk” queries. Does such a database architecture exist and do standards for this type of communication (bulk queries on populations) exist? The short answer is yes. While these standards are not fully mature, efforts with Fast Healthcare Interoperability Resource standards have produced clinical data repositories based on this standard that can receive HL7 messages, map them to FHIR data standards, and respond to population-level queries using the evolving Flat FHIR protocols for bulk transfer of data. Implementers include Amazon Web Services, Cerner, Firefly, Microsoft Azure, Smile CDR, and several government agencies. There is a large ongoing effort to pilot bulk data exchange between payers and healthcare providers, and the Office of the National Coordinator has funded further development of Flat FHIR by HL7.27 These efforts should be extended to joint work on Flat FHIR for data exchange between public health and population health providers from IIS.
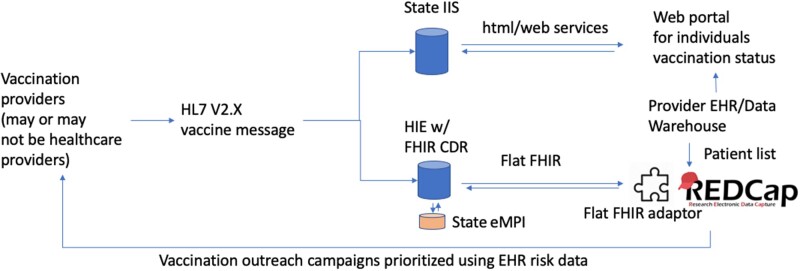
Figure 1 illustrates a conceptual architecture for wrapping IIS with Flat FHIR interoperability that we call VACTRAC. Key features of the model include: replication of the existing HL7 V2.X vaccine message stream with storage of this data; an FHIR clinical data repository; a regional, state, or national electronic master person index to disambiguate patients; and a provider data system, for bulk query of a population, that is flat FHIR-enabled. A dedicated facility for independent population data exchange with scalable capacity would be an important step in the transformation of public health data systems from legacy hierarchical information models to a more collaborative ecosystem model. A state or regional health information exchange might be a reasonable home for this infrastructure, but it could also be hosted by a public health agency.
Figure 1.
Architecture for VacTrac, a Flat FHIR system for making data in state immunization registries more available for collaboration with health systems.
Can this be done fast enough to have an impact on the pandemic? Data standards, standardized development components, and cloud-based infrastructure make it possible to rapidly adapt existing data platforms for collaboration in response to emergencies. Health Sciences South Carolina, Medical University of South Carolina, and Smile CDR (Toronto, Canada) over a few weeks developed a prototype population health management tool based on Figure 1 called VacTrac. It allows a provider to upload a list of patients to an open-source Health Insurance Portability and Accountability Act-compliant database (REDCap) from an EHR or to enter it manually. The database performs a daily check of the COVID-19 vaccination status of these patients, using the flat FHIR protocol to access an FHIR CDR and also prioritizes and tracks contacts. The Flat FHIR-enabled REDCap instance described can be downloaded at Github.28
MEASURING PROGRESS: THE NEED FOR COMPUTABLE CLINICAL QUALITY MEASURES
A critical aspect of any public–private collaboration is reliable benchmarks of performance. Targeting populations and measuring the effectiveness of providers in reaching the right segments of a population is difficult. Current CDC data shows that only 6.3% of the vaccine-receiving patients report African American race and only 11.1% report Hispanic ethnicity despite both groups having higher risks of infection (12.2% and 21.2%, respectively29) potentially exacerbating health disparities with COVID-19. We currently lack tools to access the effectiveness of COVID-19 vaccination campaigns within subpopulations or by risk level. A critical gap is the lack of computable definitions of the population segments of interest. Computable denominator definitions could be combined with vaccination data to build electronic computable quality measures that track and reward providers for success in their outreach to the most vulnerable populations. Computable quality measures exist for influenza30 and pneumococcal vaccination31 and could be readily adapted to make COVID-19 vaccination programs more equitable.
CONCLUSIONS
As outlined in this article, informatics at the interface between public health and population health will play a critical role in our response to the COVID-19 pandemic and for “all hazards” responses to further public health challenges. Rather than anticipate every use case, public health data systems should adopt a flexible, scalable approach, enabled by a foundation of standardized foundational components. With the rise of population health capabilities in health systems, public health data systems must meet not only their own needs but work collaboratively with those of population health providers. Only through consistent architecture and standardized components such as COVID-19 emergency medical identifier, population-level interoperability with public health systems, and electronic clinical quality measures for programs can we create the comprehensive data ecosystem we need to address the challenges of this pandemic and the next one.
FUNDING
This publication was supported, in part, by the National Center for Advancing Translational Sciences of the National Institutes of Health under Grant Number UL1 TR001450 and from The Duke Endowment. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or The Duke Endowment.
AUTHOR CONTRIBUTIONS
LL conceived of the study design, obtained funding, and wrote this manuscript. WD designed and implemented the described software application and contributed to the manuscript. JJ implemented the described database and contributed to the manuscript.
ACKNOWLEDGMENTS
The authors acknowledge Smile CDR for its work in optimizing the described database.
DATA AVAILABILITY STATEMENT
Not applicable.
CONFLICT OF INTEREST STATEMENT
Leslie Lenert is an unpaid member of the Scientific Advisory Board of a company, Smile CDR, that develops FHIR clinical data repositories and supports data operations with “flat FHIR” whose product was described in this manuscript.
References
- 1. Kindig D, Stoddart G.. What is population health? Am J Public Health 2003; 93 (3): 380–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.HealthPayerIntelligence. Value-Based Reimbursements Hit 53% in 2017, Reform Slows. 2019. https://healthpayerintelligence.com/news/value-based-reimbursements-hit-53-in-2017-reform-slowsAccessed March 25, 2021
- 3. McClure RC, Macumber CL, Skapik JL, et al. Igniting harmonized digital clinical quality measurement through terminology, CQL, and FHIR. Appl Clin Inform 2020; 11 (1): 23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lee LM, Thacker SB, St. Louis ME.. Principles and Practice of Public Health Surveillance. New York, NY: Oxford University Press; 2010. [Google Scholar]
- 5. Thacker SB, Qualters JR, Lee LM, Centers for Disease Control and Prevention. Public health surveillance in the United States: evolution and challenges. MMWR Suppl 2012; 61 (3): 3–9. [PubMed] [Google Scholar]
- 6. Savel T, Hall K, Lee B, et al. A Public Health Grid (PHGrid): architecture and value proposition for 21st century public health. Int J Med Inform 2010; 79 (7): 523–9. [DOI] [PubMed] [Google Scholar]
- 7. Lenert L, Sundwall DN.. Public health surveillance and meaningful use regulations: a crisis of opportunity. Am J Public Health 2012; 102 (3): e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Killerby ME, Link-Gelles R, Haight SC, et al. ; CDC COVID-19 Response Clinical Team. Characteristics associated with hospitalization among patients with COVID-19 - Metropolitan Atlanta, Georgia, March–April 2020. MMWR Morb Mortal Wkly Rep 2020; 69 (25): 790–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Baker MG, Peckham TK, Seixas NS.. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One 2020; 15 (4): e0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CDC. When Vaccine is Limited, Who Should Get Vaccinated First? 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations.htmlAccessed January 30, 2021
- 11. Jean-Jacques M, Bauchner H.. Vaccine distribution-equity left behind? JAMA 2021; 325 (9): 829. [DOI] [PubMed] [Google Scholar]
- 12. Coustasse A, Kimble C, Maxik K.. COVID-19 and vaccine hesitancy: a challenge the United States must overcome. J Ambul Care Manage 2021; 44 (1): 71–5. [DOI] [PubMed] [Google Scholar]
- 13. Kupferschmidt K. New mutations raise specter of ‘immune escape’. Science 2021; 371 (6527): 329–30. [DOI] [PubMed] [Google Scholar]
- 14. Schaffer DeRoo S, Pudalov NJ, Fu LY.. Planning for a COVID-19 vaccination program. JAMA 2020; 323 (24): 2458–9. [DOI] [PubMed] [Google Scholar]
- 15. Elizabeth Findell JSH, Frosch D. Covid-19 Vaccines Are Getting Stuck at the Last Step. WSJ Online. 2021. https://www.wsj.com/articles/covid-19-vaccines-are-getting-stuck-at-the-last-step-11610892001Accessed January 17, 2021
- 16. Tompkins L, Walker AS, Lee JC, et al. More Than Half of States Widen Access to Vaccine, Raising Hopes as Well as Chaos. The New York Times. 2021. https://www.nytimes.com/2021/01/15/us/coronavirus-vaccine-states.htmlAccessed January 17, 2021
- 17. Sood HS, Bates DW, Halamka JD, et al. Has the time come for a unique patient identifier for the US? NEJM Catalyst 2018; 4 . https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0252 Accessed March 1, 2021. [Google Scholar]
- 18. Appavu SI. Analysis of Unique Patient Identifier Options. The Department of Health and Human Services.1997. https://ncvhs.hhs.gov/wp-content/uploads/2018/03/APPAVU-508.pdf Accessed March 1, 2021.
- 19. Yasnoff WA, Humphreys BL, Overhage JM, et al. A consensus action agenda for achieving the national health information infrastructure. J Am Med Inform Assoc 2004; 11 (4): 332–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patient Identity and Patient Record Matching. https://www.healthit.gov/topic/patient-identity-and-patient-record-matchingAccessed March 24, 2021
- 21. Martin DW, Lowery NE, Brand B, et al. Immunization information systems: a decade of progress in law and policy. J Public Health Manag Pract 2015; 21 (3): 296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kempe A, Hurley LP, Cardemil CV, et al. Use of immunization information systems in primary care. Am J Prev Med 2017; 52 (2): 173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dixon GN. Making vaccine messaging stick: perceived causal instability as a barrier to effective vaccine messaging. J Health Commun 2017; 22 (8): 631–7. [DOI] [PubMed] [Google Scholar]
- 24.Immunization Information System (IIS) Functional Standards, v4.1. 2020. https://www.cdc.gov/vaccines/programs/iis/functional-standards/func-stds-v4-1.htmlAccessed January 30, 2021
- 25. Schutt RK, Siegfriedt J, Fawcett J.. Who cares? Case management and patient navigation in a public health programme. International Journal of Care and Caring 2017; 1 (3): 367–87. [Google Scholar]
- 26. Paskett ED, Harrop JP, Wells KJ.. Patient navigation: an update on the state of the science. CA Cancer J Clin 2011; 61 (4): 237–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pop Health on FLAT FHIR: A SMART Approach to Universal Healthcare Reporting. https://www.healthit.gov/topic/scientific-initiatives/leap/pop-health-flat-fhir Accessed January 30, 2021
- 28.VATRAC documentation. Github. https://github.com/vactraccovid/vactrac Accessed May 14, 2021.
- 29.CDC. COVID Data Tracker. https://covid.cdc.gov/covid-data-tracker/#vaccination-demographicAccessed February 20, 2021
- 30.Preventive Care and Screening: Influenza Immunization (eCQM). https://ecqi.healthit.gov/ecqm/ep/2020/cms147v9Accessed March 27, 2021
- 31.Immunization, Administered: Pneumococcal Vaccine. https://ecqi.healthit.gov/mcw/2020/ecqm-dataelement/immunizationadministeredpneumococcalvaccine.htmlAccessed January 30, 2021
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.