Abstract
Aims
Multiparametric remote monitoring of patients with heart failure (HF) has the potential to mitigate the health risks of lockdowns for COVID-19. We aimed to compare healthcare use, physiological variables, and HF decompensations during 1 month before and during the first month of the first French national lockdown for COVID-19 among patients undergoing remote monitoring.
Methods and results
Transmitted vital parameters and data from cardiac implantable electronic devices were analysed in 51 patients. Medical contact was defined as the sum of visits and days of hospitalization. The lockdown was associated with a marked decrease in cardiology medical contact (118 days before vs. 26 days during, −77%, P = 0.003) and overall medical contact (180 days before vs. 79 days during, −58%, P = 0.005). Patient adherence with remote monitoring was 84 ± 21% before and 87 ± 19% during lockdown. The lockdown was not associated with significant changes in various parameters, including physical activity (2 ± 1 to 2 ± 1 h/day), weight (83 ± 16 to 83 ± 16 kg), systolic blood pressure (121 ± 19 to 121 ± 18 mmHg), heart rate (68 ± 10 to 67 ± 10 b.p.m.), heart rate variability (89 ± 44 to 78 ± 46 ms, P = 0.05), atrial fibrillation burden (84 ± 146 vs. 86 ± 146 h/month), or thoracic impedance (66 ± 8 to 66 ± 9 Ω). Seven cases of HF decompensations were observed before lockdown, all but one of which required hospitalization, vs. six during lockdown, all but one of which were managed remotely.
Conclusions
The lockdown restrictions caused a marked decrease in healthcare use but no significant change in the clinical status of HF patients under multiparametric remote monitoring.
Keywords: Remote monitoring, Heart failure, COVID-19, Telemedicine
Graphical Abstract
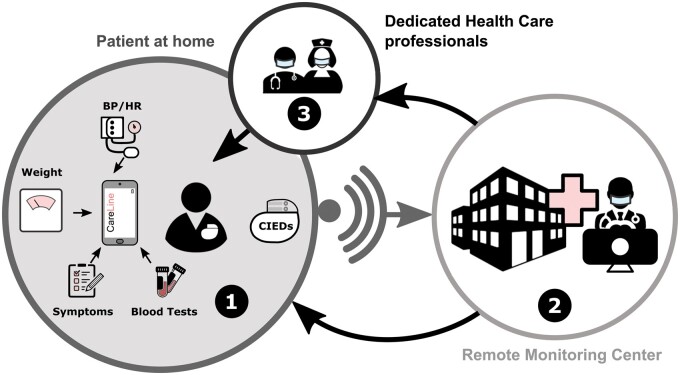
Heart failure multiparametric remote monitoring. (1) Patients were equipped with a multiparametric remote monitoring system that incorporates daily blood pressure (BP), heart rate (HR), body weight, and symptom status. The receiving server could additionally incorporate blood test results. Cardiac implantable electronic devices (CIEDs) were remotely monitored, when applicable. (2) Collected data were monitored by a specialized team of nurses and physicians (the remote monitoring centre). (3) Relevant and actionable information could be communicated to the patient and their healthcare professionals.
Lay Summary
The first French COVID-19 lockdown had a huge detrimental impact on conventional healthcare use (−78% in cardiology medical contact). However, the lockdown had little impact over the short-term, if any, on vital parameters and the clinical status of patients with heart failure (HF) who were adherent to multiparametric remote monitoring. This remote monitoring strategy allowed early identification and home management of most of the HF decompensations during the lockdown.
Introduction
Numerous countries have implemented movement restrictions and physical distancing measures to reduce viral transmission during the coronavirus disease 2019 (COVID-19) pandemic. In France, the first lockdown was strict and enforced, including a maximum allotment of 1 h outside the home for selected activities, exercise restrictions to 1 km from one’s home, and mandatory time-stamped forms when doing so. This lockdown was accompanied by national guidelines on medical countermeasures, including cancelling non-urgent medical and surgical activities to preserve intensive care capacity for potential surges in COVID-19 patients and to limit viral spread between hospitals.1 Patients with heart failure (HF) are a particularly vulnerable population in this context: HF decompensation and hospitalization can occur because of their heightened susceptibility to infection but also because of potential lockdown-related reductions in physical activity, withdrawal from psychosocial support networks, and disruptions in healthcare delivery.2–4 Remote monitoring of patients with HF using home sensors or cardiac implantable electronic devices (CIEDs) has proven to be effective when added to standard care in randomized controlled trials.5,6 However, whether remote monitoring can mitigate the health risks of lockdowns—in particular restrictions in conventional measures of care provision—is unknown. We therefore examined the impact of the first national lockdown for COVID-19 in France on the healthcare use and the clinical status of patients with HF under multiparametric remote monitoring.
Materials and methods
Physiological variables, HF decompensations, and healthcare use were retrospectively examined 1 month before and 1 month after the beginning of the first French lockdown for COVID-19 (17 March 2020) in a sample of patients with chronic HF who were remotely monitored. All patients were enrolled in the French HF remote monitoring programme Experimental Telemedicine And Provision of Enhanced Services (ETAPES)7 at least 1 month before the beginning of the national lockdown and were followed at the Bordeaux University Hospital. Patients were eligible for enrolment in the ETAPES programme if they had symptomatic HF (with or without reduced left ventricular ejection fraction) and had been hospitalized for acute HF within the preceding 12 months. Consent: all patients provided informed consent for study participation.
Multiparametric remote monitoring
All patients were equipped with a multiparametric remote monitoring system (CareLine Solutions™, Mérignac, France), which includes either a tablet or smartphone connected via Bluetooth to a body weight scale and a blood pressure monitor. This system allows for daily transmissions of weight, blood pressure, heart rate, and responses to questions relating to five HF symptoms to a remote monitoring server, which is also capable of importing blood test results. These parameters were subject to 17 programmable alerts based on critical absolute values or changes over time. All participants were concomitantly enrolled in an HF education programme. Triggered alerts from the system were reviewed during office hours by specialized nurses and physicians of the Bordeaux University Hospital cardiac remote monitoring centre. This centre was also responsible for remote monitoring of CIEDs.
Lockdown measures
Between 17 March and 11 May 2020, all residents in France were instructed to stay home as much as possible and to venture outside only for essential errands or approved work. When outside the home, all residents were required to carry a signed and time-stamped document justifying the reason. Failure to produce a valid form could result in a fine. Hospitals were instructed to cancel all non-urgent medical or surgical activities.1
Study periods and variables of interest
Variables of interest were compared between two periods: before lockdown from 15 February to 16 March 2020 (31 days) and during lockdown from 17 March to 17, April 2020 (31 days).8 The CareLine Solutions™ remote monitoring platform was used to collect data on weight, blood pressure, heart rate, symptoms, blood tests, alerts, HF decompensation events, medical changes, consultations, and details of hospitalizations (including the number, length of stay, and reason for admission). Measures of healthcare use were cross-checked using patient medical records and phone calls to patients and practitioners. We defined the medical contact index as the sum of in-person visits and days of hospitalization for each 31-day period (i.e. the number of days during which the patient was medically assessed in person). Cardiology specific and overall medical contact indices were calculated. We retrieved the following CIED parameters from the Biotronik Home Monitoring service centre (Biotronik, Berlin, Germany) and the Medtronic CareLink website: daily mean heart rate, daily heart rate variability, daily atrial fibrillation burden, daily activity, and daily thoracic impedance. Heart failure decompensations were reported by the cardiologists from the remote monitoring centre and resulted in an increase in diuretic treatment.
Statistical analysis
Categorical variables are expressed as absolute numbers (percentages); continuous variables are expressed as mean ± standard deviation. Adherence with remote monitoring was calculated as the percentage of days that patients transmitted body weight data out of all effective surveillance days. The number of days spent in hospital was subtracted from all possible surveillance days to calculate the number of days of effective surveillance in each study period. The dependent t-test or the Wilcoxon signed rank test was used to compare continuous data, with a significance level of 0.05. Statistical analyses were performed using SPSS software, version 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Population
A total of 53 patients with HF were eligible for the study; however, two patients were excluded because data were missing for the periods of interest. One of these patients was hospitalized for an orthopaedic condition for over 60 days soon after the start of the pre lockdown period; another was already hospitalized at the beginning of the before lockdown period and was not discharged until after the lockdown had been implemented. Patient characteristics and HF therapies at inclusion of the treatment group are summarized in Table 1.
Table 1.
Baseline patient characteristics
| Characteristic | |
|---|---|
| Male sex | 43 (84) |
| Age, years | 72 ± 11 |
| ≥80 years | 14 (27) |
| NYHA classification | |
| NYHA 2 | 19 (37) |
| NYHA 3 | 26 (51) |
| NYHA 4 | 6 (12) |
| HF aetiology | |
| Ischaemic | 22 (43) |
| Dilated cardiomyopathy | 15 (29) |
| Valvular | 5 (10) |
| Tachyarrhythmia | 4 (8) |
| Other | 5 (10) |
| Comorbidities | |
| Atrial fibrillation | 36 (70) |
| Overweight/obesity | 31 (61) |
| Hypertension | 35 (69) |
| Diabetes mellitus | 23 (45) |
| Dyslipidaemia | 33 (65) |
| eGFR, mL/min/1.73 m2 | 49 ± 25 |
| BNP, pg/mL | 591 ± 614 |
| LVEF, % | 35 ± 12 |
| ≤35% | 31 (61) |
| Treatments | |
| ACEi/ARB* <50% | 10 (20) |
| ACEi /ARB* ≥50% | 12 (24) |
| Sacubitril/Valsartan* <50% | 6 (12) |
| Sacubitril/Valsartan* ≥50% | 15 (29) |
| Beta blockers* >50% | 13 (25) |
| Beta blockers* ≥50% | 29 (57) |
| Aldosterone antagonist* <50% | 18 (35) |
| Aldosterone antagonist* ≥50% | 5 (10) |
| Furosemide, mg | 142 ± 122 |
| Cardiac implantable electronic devices | |
| Implantable cardioverter-defibrillator | 27 (53) |
| Permanent pacemaker | 12 (24) |
| Cardiac resynchronization therapy | 18 (35) |
| CRT-D | 14 (27) |
| CRT-P | 4 (8) |
ACEi, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; BNP, B-type natriuretic peptide; eGFR, glomerular filtration rate.
* % of target dose. Patients can have mixed aetiologies.
Healthcare use
The cardiology contact index markedly decreased from 118 days (28 visits and 90 days of hospitalization) before lockdown to 26 days (6 visits and 20 days of hospitalization) during the lockdown (−77%, P = 0.003). The overall medical contact index also decreased from 180 days (80 visits and 100 days of hospitalization) before lockdown to 79 days (52 visits and 27 days of hospitalization) during the lockdown (−58%, P = 0.005). Three virtual visits were performed before vs. 12 during the lockdown.
Physiologic parameters
Adherence with remote monitoring was high and similar before and during lockdown (84 ± 21% and 87 ± 19%, respectively). The overall observance was similar between patients older than 80 (90 ± 16%) and the younger patients (84 ± 18%; P = 0.13). There were no significant changes in weight, blood pressure, or heart rate between the two study periods. Data from remote CIEDs interrogations corroborated these findings, with no significant change observed in heart rate, heart rate variability, atrial fibrillation burden, thoracic impedance, or daily activity (Table 2). No sustained ventricular arrhythmia occurred during any of the study periods.
Table 2.
Details of data from home sensors and cardiac implantable electronic devices
| Before LD | During LD | ||
|---|---|---|---|
| Home sensors data (N = 51) | |||
| Days of remote monitoring | 28 ± 6 | 31 ± 1 | <0.01 |
| Days of transmissions | 24 ± 8 | 27 ± 6 | 0.01 |
| Adherence, % | 84 ± 21 | 87 ± 19 | 0.08 |
| Weight, kg | 83 ± 16 | 83 ± 16 | 0.12 |
| SBP, mmHg | 121 ± 19 | 121 ± 18 | 0.91 |
| DPB, mmHg | 73 ± 9 | 73 ± 9 | 0.86 |
| Heart rate, b.p.m. | 68 ± 10 | 67 ± 10 | 0.36 |
| Device data (N = 21) | |||
| Activity, h/day | 2 ± 1 | 2 ± 1 | 0.27 |
| Heart rate, b.p.m. | 71 ± 5 | 70 ± 6 | 0.08 |
| Heart rate variability, ms | 89 ± 44 | 78 ± 46 | 0.05 |
| AF burden, h | 84 ± 146 | 86 ± 146 | 0.72 |
| Thoracic impedance, Ohms | 66 ± 8 | 66 ± 9 | 0.61 |
AF burden, atrial fibrillation burden (total hours/31 days); DBP, diastolic blood pressure; LD, lockdown; SBP, systolic blood pressure.
Alerts and telephone calls
Details of CareLine alerts before and during lockdown are shown in Table 3. Overall, the remote monitoring centre received fewer alerts during lockdown than before it, although the numbers of telephone calls emitted by the remote monitoring centre were similar between the two periods (3.6 ± 4.1 per patient before lockdown vs. 2.9 ± 3.2 during lockdown). Blood test alerts were significantly reduced during the lockdown due to the strong decrease in medical analysis laboratory frequentation. Figure 1 shows trends in weight, heart rate, and systolic blood pressure (from home sensors) and in activity and thoracic impedance (Optivol™ index) from CIEDs during the two study periods in a patient with chronic HF who clinically decompensated on the second day of the lockdown (18 March 2020, red arrow) and was managed at home with an increase in their diuretic.
Table 3.
Details of alerts transmitted before and during lockdown
| Before LD | During LD | ||
|---|---|---|---|
| Weight alerts, n | 95 | 76 | 0.60 |
| Blood pressure alerts, n | 20 | 7 | 0.46 |
| Heart rate alerts, n | 11 | 13 | 0.10 |
| Symptom alerts, n | 53 | 26 | 0.15 |
| Blood test alerts, n | 27 | 7 | 0.01 |
| Total alerts, n | 206 | 139 | 0.12 |
| Telephone calls, n (com) | 183 (53) | 148 (38) | 0.34 |
Telephone calls, N = total, com = calls for absence of communication.
Figure 1.
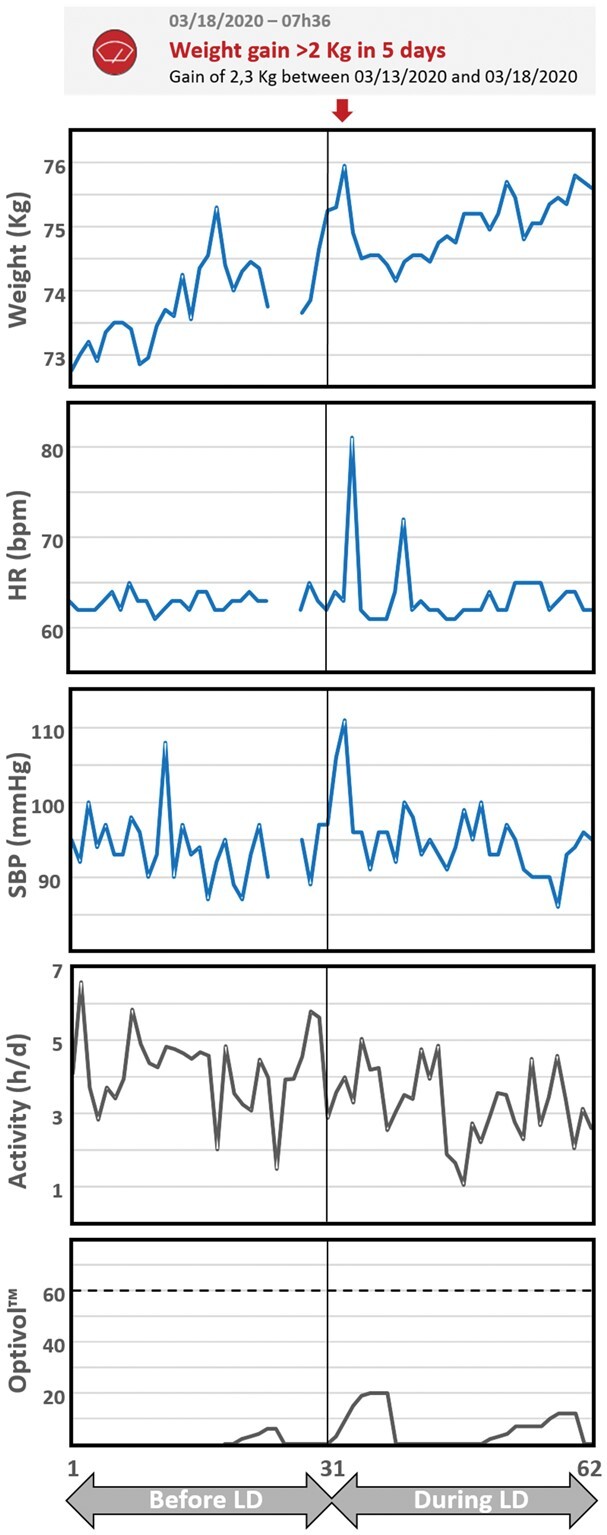
Multiparametric remote monitoring in a patient with heart failure. Trends in vital parameters from a 72-year-old patient with non-ischaemic cardiomyopathy with a left ventricular ejection fraction of 25% and a dual-chamber implantable cardioverter-defibrillator (Medtronic Evera XT DR). Each panel demonstrates is divided by a vertical line into the period before lockdown (days 1–31) and during lockdown (days 32–62). On day 33 (second day of the lockdown), a weight alert was received (gain of 2.3 kg in 5 days, red arrow). The patient complained of worsening dyspnoea and abdominal bloating. The patient was asked to double his dose of furosemide and continued to be remotely monitored at home. Another alert was received 36 days after lockdown implementation, which prompted a further increase in diuretic for few days until a blood test alert was triggered for an increase in creatinine and urea levels, then the patients stabilized. This patient was fully managed remotely and did not require hospitalization during the following 9 months. Home sensor-derived trends are depicted in blue [weight, heart rate (HR), and systolic blood pressure (SBP)]; activity and OptiVol trends from the CIED are depicted in black.
HF decompensation
The number of HF decompensations was similar during lockdown compared to before: six events in five patients vs. seven events in six patients, respectively. Table 4 presents and overview of HF decompensations with related triggered alerts and medical interventions. Before the lockdown, all but one episode required hospitalization. Conversely, during the lockdown, all but one HF decompensation were managed at home. Among these four patients with HF decompensations managed at home, three remained free from hospitalization over the subsequent 3 months. One patient was hospitalized for decompensated HF after an in-person consultation during lockdown. None of the patients reported symptoms suggestive of COVID-19 nor tested positive for SARS-CoV-2.
Table 4.
Heart failure decompensation details
| CareLine alert | Device Alert | Action |
||
|---|---|---|---|---|
| Home | Hospital | |||
| Before LD | ||||
| Patient 1 | Weight gain >2 kg/5days | NA | IV diuretics | |
|
| ||||
|
|
No | ↑ oral diuretics | Hospitalization 7 days after |
|
| ||||
| Patient 3 |
|
NA | Hospitalization | |
|
| ||||
|
|
No | ↑ oral diuretics | Hospitalization 7 days after |
|
| ||||
|
No | TriageHF™ index high for 9 days | Hospitalization | |
|
| ||||
| Patient 1 | Weight gain >2 kg/5days | NA | IV diuretics | Hospitalization |
|
| ||||
|
|
NA | ↑ oral diuretics | Hospitalization 3 days after |
| During LD | ||||
|
|
No | ↑ oral diuretics | |
|
| ||||
|
|
|
|
|
|
| ||||
|
|
No | ↑ oral diuretics | |
|
| ||||
| Patient 1 | Weight gain >2 kg/5days | NA | IV diuretics | |
|
| ||||
|
No | No | Hospitalization | |
|
| ||||
| Patient 1 | Weight gain >2 kg/5days | NA | IV diuretics | |
Overview of the nine patients with heart failure decompensations under remote monitoring presented in chronological order. The first column indicates the patient’s number and the device model. PM VR BS, pacemaker VR Boston Scientific; CRTD bio, CRT-Defibrillator Biotronik; ICD DR Med, ICD DR Medtronic; CRT-D Ab, CRT-Defibrillator Abbott; CRT-P Ab, CRT-Pacemaker Abbott. The second column depicts the CareLine Solutions alerts at the time of HF decompensation diagnosis. Weight gain >4 kg/Ref: weight gain in comparison to the weight patient’s reference. Weight gain >2 kg/5days: gain of more than 2 kg in five consecutive days. Δ Symptoms: worsening of symptoms based on the questionnaire. HR > 100 b.p.m./3 days: mean heart rate above 100 b.p.m. on three consecutive days. Δ Blood urea >20% and Δ NT-proBNP >20%: increase >20% of the last known value. The third column depicts the CIEDs remote monitoring alerts at the time of HF decompensation diagnosis. The last columns indicate the medical interventions required.
Discussion
Lockdowns could theoretically have a detrimental impact on HF patient outcomes due to disrupted contact with healthcare professionals, lifestyle changes, and loss of social support networks. However, our data suggest that the first national lockdown in France had little short-term impact, if any, on vital parameters and clinical measures of patients with HF who were adherent to multiparametric remote monitoring despite a significant reduction in conventional measures of healthcare access.
Consequences of the lockdown restrictions
Strict government health mandates aimed at limiting the spread of COVID-19 were associated with a reluctance among patients to attend hospitals and resulted in a marked reduction in medical contact and in admissions to hospital for cardiovascular disease.8–10 In line with previous reports, we observed a two-thirds reduction in cardiology appointments and a greater than 50% reduction in overall medical contact associated with lockdown measures—findings that could be expected to favour HF destabilization.11,12
There exist several potential explanations for the stability observed in the clinical status of patients with HF during lockdown in our study. It could be that patients with symptomatic HF lead relatively sedentary lifestyles and are relatively ‘homebound’ at baseline, therefore lockdowns do not impose a marked change in their daily lives. The unchanged activity level seen in our study sample during lockdown could support this explanation. However, this is an inconsistent observation: in a similar population of patients implanted with cardiac resynchronization therapy devices but without dedicated remote monitoring, Al Fagih et al.13 observed a significant decrease in activity level during lockdown, suggesting that lockdowns could meaningfully impact such patients’ lifestyles. This is further supported by the results of a French survey of patients with HF but without remote monitoring that found that during the same lockdown 42% exhibited a decrease in physical activity, 14.5% had a decrease in dietary adherence, 22% had a decrease in well-being, and 27% reported weight gains of >2 kg, coinciding with 72% of their medical appointments being cancelled.11 An alternate explanation is that the remote monitoring programme, which includes patient education, mitigated the impact of lockdown measures, allowing for ongoing surveillance of vital parameters, preserving patients’ contact with their medical team (via telephone calls), and providing opportunities to reinforce lifestyle counselling and to make timely treatment adjustments.
Remote management of HF decompensation
The TIM-HF2 (Telemedical Interventional Monitoring in Heart Failure) randomized trial suggested that multiparametric remote management of patients with HF could reduce unplanned cardiovascular hospitalization or death.5 We studied a similar strategy in combination with CIED remote monitoring in the unique context of a national lockdown for COVID-19, during which in-person contact with the hospital and healthcare providers was discouraged. With this strategy, most of the decompensations were remotely identified (6/7 before and 5/6 during the lockdown) and more importantly, four of five patients with HF decompensation during lockdown could be managed at home, avoiding hospitalization. We have learned from this unique experience, that when detected earlier, HF decompensations do not need to be systematically hospitalized. Although the number of events is low, these findings suggest that remote monitoring can be an effective strategy during lockdowns, while also suggesting that its value may be underappreciated in non-lockdown settings.
Limitations
This is a single-centre retrospective study with a limited number of patients and events. However, we evaluated a large number of parameters with few missing data. Unlike other monitoring strategies that rely on direct-to-consumer technologies (e.g. smartphones), which are more likely to appeal to younger patient populations, the system used in this study was provided and supported by healthcare professionals. In our study design, the 1-month period before to lockdown served as a control. We could not exclude that some patients already applied some form of self-quarantine. However, Vetrovsky et al.4 showed a rather stable activity in HF patients among the 3 weeks before, and a drop clearly delimited by the start of the lockdown restrictions. The positive predictive value of the alert system could not be assessed because multiple alerts could occur for the same event and reoccur if not suspended by the user. Because the present findings were obtained with a multiparametric approach in a structured remote monitoring centre they represent a complex intervention and their generalizability to different technologies or other organizations is unknown.
Perspective
The COVID-19 pandemic and associated lockdowns have forced healthcare teams to rapidly adopt remote monitoring and telehealth strategies.14 Until recently, the lack of consistent benefits observed in randomized trials with remote monitoring in patients with HF had hindered widespread adoption of this approach. In light of the TIM-HF2 results, however, the French government launched the ETAPES programme to explore this strategy at a national level. The programme is still under evaluation, but the COVID-19 crisis and national lockdowns have created unique opportunities to examine its potential. Our findings suggest that a combination of home sensors and CIED remote interrogation capabilities represent a method of complying with public health measures while preserving the care and safety of patients with chronic HF. Our experience therefore argues for the benefits of this strategy in this patient population and supports larger studies to confirm our findings.
Conclusion
The clinical status of HF patients under multiparametric remote monitoring was minimally affected by lockdown restrictions despite a marked decrease in conventional measures of healthcare use. This strategy, combined with patient education, may mitigate the health risks associated with strict lockdowns for COVID-19.
Acknowledgements
The authors wish to acknowledge the kind collaboration of Aurélie Chamouleau, Sylvie Delor, Estel Hugot, Mélissa Lavevre, Maïder Piquet, and Mélanie Vergne.
Funding
This study received financial support from the French Government as part of the ‘Investments of the Future’ programme managed by the National Research Agency (ANR), grant reference ANR-10-IAHU-04. S.A.-A. has received a research grant from the CHU Clermont-Ferrand.
Conflict of interest: S.P. and R.E. are co-founders and stock owners of the CareLine Solutions Company.
Data availability
Data will be made available upon reasonable request.
References
- 1.Guide méthodologique ‘préparation à la phase épidémique de COVID-19 des établissements de santé, de la médecine de ville et des établissements et services médico-sociaux’ du 16 mars 2020. http://www.nouvelle-aquitaine.ars.sante.fr/guide-methodologique-preparation-la-phase-epidemique-de-covid-19-des-etablissements-de-sante-de-la (last accessed 05/26/2021).
- 2. Reza N, DeFilippis EM, Jessup M.. Secondary impact of the COVID-19 pandemic on patients with heart failure. Circ Heart Fail 2020;13:e007219. [DOI] [PubMed] [Google Scholar]
- 3. Mattioli AV, Ballerini Puviani M, Nasi M, Farinetti A.. COVID-19 pandemic: the effects of quarantine on cardiovascular risk. Eur J Clin Nutr 2020;74:852–855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vetrovsky T, Frybova T, Gant I, Semerad M, Cimler R, Bunc V, Siranec M, Miklikova M, Vesely J, Griva M, Precek J, Pelouch R, Parenica J, Belohlavek J.. The detrimental effect of COVID-19 nationwide quarantine on accelerometer-assessed physical activity of heart failure patients. ESC Heart Fail 2020;7:2093–2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koehler F, Winkler S, Schieber M, Sechtem U, Stangl K, Böhm M, Boll H, Baumann G, Honold M, Koehler K, Gelbrich G, Kirwan B-A, Anker SD; Telemedical Interventional Monitoring in Heart Failure Investigators. Impact of remote telemedical management on mortality and hospitalizations in ambulatory patients with chronic heart failure: the telemedical interventional monitoring in heart failure study. Circulation 2011;123:1873–1880. [DOI] [PubMed] [Google Scholar]
- 6. Hindricks G, Taborsky M, Glikson M, Heinrich U, Schumacher B, Katz A, Brachmann J, Lewalter T, Goette A, Block M, Kautzner J, Sack S, Husser D, Piorkowski C, Søgaard P, IN-TIME study group. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet Lond Engl 2014;384:583–590. [DOI] [PubMed] [Google Scholar]
- 7.DGOS. ÉTAPES: Expérimentations de Télémédecine pour l’Amélioration des Parcours En Santé. Ministère Solidar. Santé. 2020. https://solidarites-sante.gouv.fr/soins-et-maladies/prises-en-charge-specialisees/telesante-pour-l-acces-de-tous-a-des-soins-a-distance/article/la-telesurveillance-etapes (last accessed 05/26/2021).
- 8. Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, Thuaire C, Angoulvant D, Cayla G, Bouleti C, Gallet de Saint Aurin R, Goube P, Lhermusier T, Dillinger J-G, Paganelli F, Saib A, Prunier F, Vanzetto G, Dubreuil O, Puymirat E, Boccara F, Eltchaninoff H, Cachanado M, Rousseau A, Drouet E, Steg P-G, Simon T, Danchin N.. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health 2020;5:e536–e542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, Hollings S, Roebuck C, Gale CP, Mamas MA, Deanfield JE, de Belder MA, Luescher TF, Denwood T, Landray MJ, Emberson JR, Collins R, Morris EJA, Casadei B, Baigent C.. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet Lond Engl 2020;396:381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Frankfurter C, Buchan TA, Kobulnik J, Lee DS, Luk A, McDonald M, Ross HJ, Alba AC.. Reduced rate of hospital presentations for heart failure during the COVID-19 pandemic in Toronto, Canada. Can J Cardiol 2020;36:1680–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chagué F, Boulin M, Eicher J-C, Bichat F, Jalmes MS, Cransac‐Miet A, Soudry‐Faure A, Danchin N, Cottin Y, Zeller M.. Impact of lockdown on patients with congestive heart failure during the coronavirus disease 2019 pandemic. ESC Heart Fail 2020;7:4420–4423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sankaranarayanan R, Hartshorne-Evans N, Redmond-Lyon S, Wilson J, Essa H, Gray A, Clayton L, Barton C, Ahmed FZ, Cunnington C, Satchithananda DK, Murphy CL.. The impact of COVID-19 on the management of heart failure: a United Kingdom patient questionnaire study. ESC Heart Fail 2021;8:1324–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Al Fagih A, Al Onazi M, Al Basiri S, Al-Kaf F, Dagriri K, Al Hebaishi Y, Samargandy S, Al Shengeiti L.. Remotely monitored inactivity due to COVID-19 lockdowns. Potential hazard for heart failure patients. Saudi Med J 2020;41:1211–1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cleland JGF, Clark RA, Pellicori P, Inglis SC.. Caring for people with heart failure and many other medical problems through and beyond the COVID‐19 pandemic: the advantages of universal access to home telemonitoring. Eur J Heart Fail 2020;22:995–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available upon reasonable request.