Abstract
Background
We aimed to investigate the association between institution trust and public responses to the coronavirus disease 2019 (COVID-19) outbreak.
Methods
An Internet-based, cross-sectional survey was administered on 29 January 2020. A total of 4393 adults ≥18 y of age and residing or working in the province of Hubei, central China were included in the study.
Results
The majority of the participants expressed a great degree of trust in the information and preventive instructions provided by the central government compared with the local government. Being under quarantine (adjusted odds ratio [OR] 2.35 [95% confidence interval {CI} 1.80 to 3.08]) and having a high institutional trust score (OR 2.23 [95% CI 1.96 to 2.53]) were both strong and significant determinants of higher preventive practices scores. The majority of study participants (n=3640 [85.7%]) reported that they would seek hospital treatment if they suspected themselves to have been infected with COVID-19. Few of the participants from Wuhan (n=475 [16.6%]) and those participants who were under quarantine (n=550 [13.8%]) expressed an unwillingness to seek hospital treatment.
Conclusions
Institutional trust is an important factor influencing adequate preventive behaviour and seeking formal medical care during an outbreak.
Keywords: China, COVID-19, Hubei, institutional trust, preventive, treatment-seeking behaviour
Introduction
On 8 December 2019, several cases of pneumonia were reported in Wuhan, Hubei province, China.1,2 Subsequently, on 7 January 2020, the Chinese Center for Disease Control and Prevention (CDC) identified a novel coronavirus linked to the outbreak, which was subsequently named the 2019 novel coronavirus (2019-nCoV) by the World Health Organization (WHO).3 On 23 January 2020, the central government of the People's Republic of China imposed a lockdown in Wuhan in an effort to quarantine the epicentre of the outbreak to prevent an epidemic. On 11 February 2020, the WHO declared an official name for the new coronavirus disease as coronavirus disease 2019 (COVID-19). In this ongoing pandemic, healthcare providers in China have been working around the clock treating patients and preventing casualties, while scientists in China and around the globe have been racing to find out more about the coronavirus. Published studies have led to a better worldwide understanding of the epidemiology and clinical and genomic characteristics of COVID-19.4,5 However, counteracting COVID-19 will entail multifaceted control strategies. Global outbreaks like the severe acute respiratory syndrome (SARS) epidemic and the 2009 influenza A (H1N1) pandemic have brought attention to the importance of understanding community responses in outbreak control.6 Understanding local community responses is vital to provide insights into the development of risk communication messages to the general public for outbreak prevention and control.6,7 Therefore, investigating the public response to the outbreak is as important as epidemiological, clinical and genomic research.
Trust in public institutions, both government and healthcare, has been investigated in previous infectious disease outbreaks but has not been studied in the early stage of the COVID-19 epidemic in Wuhan, China. The lessons learned from the 2018–2019 Ebola outbreak suggest that institutional trust is of central importance in effective public health intervention.8 Lack of institutional trust may lead to refusal to comply with a preventive or curative intervention, which may result in an increased risk of both acquiring and spreading the disease.8 As noted in the statement from the second meeting of the Emergency Committee on 30 January regarding the outbreak of COVID-19, the implementation of comprehensive risk communication strategies to enhance public health measures for containment of the outbreak is vital.9 Therefore it is of utmost importance that people in Wuhan, the epicentre of COVID-19, have full trust in public institutions to enable successful delivery of risk communication and practice of health protection behaviours. As in many countries, the federal structure in China divides the country into three spheres of governance—central, provincial and local. A previous study reported that the general public in China has a higher level of trust in the national or central government due to political control and cultural and performance reasons.10 It is unknown whether, during a period of uncertainty, the level of public trust remains similar.
The importance of trust in healthcare institutions is also well established. In China, most of the hospitals are public healthcare institutions owned and run by the government. During the ongoing COVID-19 pandemic, healthcare providers engaged in healthcare activities that involved face-to-face interaction with patients. Public trust in healthcare providers during a healthcare crisis is imperative in promoting care-seeking and behavioural competence. Understanding public trust in the different levels of governments and the healthcare authorities during the outbreak of infectious diseases is undeniably important and warrants rigorous investigation. Such information may help to tailor and implement programs effectively, as well as facilitate policy compliance.
In consideration of the importance of understanding community responses, this study aimed to investigate the role of institutional trust in individual preventive and treatment-seeking intentions during the COVID-19 outbreak, which as of 23 February, the confirmed cases had reached >70 000 and >2000 deaths had been reported in China.
Methods
Study design and participants
An anonymous Internet-based, cross-sectional survey commenced on 29 January 2020. The study population was adults ≥18 y of age and residing or working in the province of Hubei, where Wuhan is the capital city. This cross-sectional study was performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.
Procedures
A snowball sampling technique was used to recruit the participants. The web link to the survey was first circulated to the academic staff and students of Ningbo Medical University, who are from diverse geographic locations of origin. They were instructed to employ their social networks to circulate the link to people residing or working in the province of Hubei. Upon completing the survey, a note to encourage participants to disseminate the survey link to all known contacts in Hubei province was included. Participants were remunerated 5 Chinese yuan for each complete response.
The questionnaire was developed in English and translated into the Han language (Mandarin). Independent experts reviewed and validated the translation. The questionnaire was also face validated by local experts and pilot tested. The survey consisted of sections that assessed sociodemographic background, locality, mandatory home quarantine status, institutional trust and COVID-19-related preventive practices and health-seeking intentions. A question on locality assessed the participants’ current place of residence (whether in the epicentre of Wuhan or other cities in Hubei province). Questions on mandatory quarantine status queried participants whether they were currently under mandatory home quarantine or placed under quarantine in a government facility.
Institutional trust was assessed using a series of questions (eight items) that assessed participants’ trust in COVID-19-related information (i.e. the reported number of confirmed cases, deaths, etc.) and preventive instructions (i.e. self-quarantine, provincial quarantine, extended time off, etc.) given by the governments (local, provincial and central) and healthcare institutions. The questions were adapted from Vinck et al.8 The response options were recorded on a 4-point Likert scale with items scored as either 0 (not at all), 1 (a small extent), 2 (moderate) or 3 (a great extent). Both government and healthcare institutions are public institutions, hence the scores for trust in local, provincial and central government and healthcare providers were totalled. The possible score ranged from 0 to 24, with higher scores indicating higher levels of trust.
The section on preventive practices consisted of five parts (14 items): direct avoidance, social interaction avoidance, physical contact avoidance, public space avoidance and personal protection. The preventive questions were also adapted from Vinck et al.8 The response options were recorded on a 3-point Likert scale with items scored as 0 (never), 1 (occasionally) or 2 (frequently). The possible score ranged from 0 to 28, with higher scores indicating higher levels of preventive behaviours.
The section on health-seeking intentions asked participants about the health-seeking intentions that they would adopt if they suspected themselves to have been infected with COVID-19. The health-seeking intentions included seeking treatment in the hospital, traditional healing and self-healing (i.e. exercise, high dose of vitamins, plenty of fresh fruits and vegetables). The answers included two options, ‘yes’ and ‘no’.
Statistical analyses
Normality testing was performed using the Kolmogorov–Smirnov test. The scores of institutional trust and preventive practices were not normally distributed, therefore all results were expressed as the median and interquartile range (IQR). Other descriptive statistics, such as frequency tables, charts and proportions, were used for data summarization. The reliability of the institutional trust and preventive practices items was evaluated by assessing the internal consistency of the items representing the scores. The 8-item institutional trust and the 14-item preventive practices had a reliability (Cronbach's α) of 0.944 and 0.653, respectively. Multivariable logistic regression was used to determine factors influencing preventive practices scores and conventional treatment-seeking intentions. The prevention practices scores was categorized into two ranges based on the median split; the higher score range was coded as 1 and the lower score range was coded as 0. The independent variables for both multivariable logistic regressions predicting prevention practices and treatment seeking were sociodemographic characteristics, locality, quarantine status and institutional trust score.
Variables that were significant on a χ2 test were selected for multivariable logistic regression analysis and included in the model using a simultaneous forced-entry method. Odds ratios (ORs), 95% confidence intervals (CIs) and p-values were calculated for each independent variable. The model fit was assessed using the Hosmer–Lemeshow goodness-of-fit test.11 All statistical analyses were performed using the Statistical Package for the Social Sciences, version 20.0 (IBM, Armonk, NY, USA). P-values <0.05 were considered statistically significant.
Results
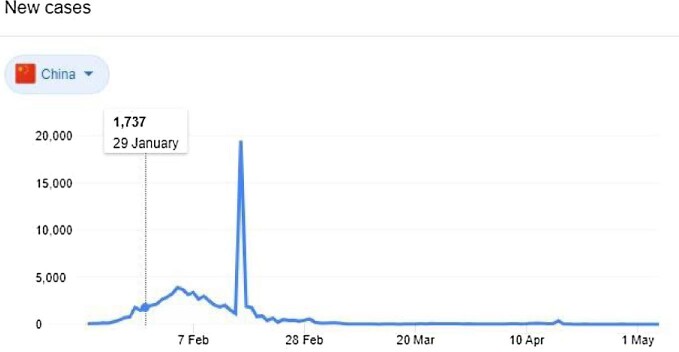
Figure 1 showed the number of confirmed cases in China was 1737 on the date of the onset of data collection. The survey link was disseminated on 29 January 2020 and by 30 January a total of 4393 responses were received. The final number of responses included in the data analyses was 4245, after data cleaning to remove invalid responses. The demographic characteristics of the participants are shown in the first column of Table 1. Most of the participants were from the city of Wuhan (67.3%) and the remaining 32.7% were from other cities in Hubei province. The majority of the participants (93.6%) reported that they were currently under mandatory quarantine. The study participants’ ages ranged from 18 to 70 y. The majority of the study participants (35.7%) were 26–35 y of age. A total of 7.3% of participants were of the oldest age group (56–70 y).
Figure 1.
The number of confirmed COVID-19 cases in China and the date of data collection.
Table 1.
Demographic characteristics and factors associated with preventive practices (N=4245).
| Univariate analysis | Multivariable analysisa | ||||
|---|---|---|---|---|---|
| Preventive practices score | Preventive practices score, 27–28 vs 7–26 | ||||
| Covariates | n (%) | 27–28 (n=2321) | 7–26 (n=1924) | p-Value | OR (95% CI) |
| Demographic characteristics | |||||
| Age group (years) | |||||
| 18–25 | 782 (18.4) | 380 (48.6) | 402 (51.4) | 1.25 (0.91 to 1.71) | |
| 26–35 | 1515 (35.7) | 893 (58.9) | 622 (41.1) | <0.001 | 1.64 (1.24 to 2.16)*** |
| 36–45 | 953 (22.4) | 532 (55.8) | 421 (44.2) | 1.30 (0.98 to 1.73) | |
| 46–55 | 685 (16.1) | 361 (52.7) | 324 (47.3) | 1.09 (0.82 to 1.46) | |
| 56–70 | 310 (7.3) | 155 (50.0) | 155 (50.0) | Reference | |
| Gender | |||||
| Male | 1754 (41.3) | 975 (55.6) | 779 (44.4) | 0.332 | |
| Female | 2491 (58.7) | 1346 (54.0) | 1145 (46.0) | ||
| Highest education level | |||||
| Middle school and below | 380 (9.0) | 215 (56.6) | 165 (43.4) | Reference | |
| High school/technical secondary school | 783 (18.4) | 472 (60.3) | 311 (39.7) | <0.001 | 1.22 (0.94 to 1.57) |
| Junior college/vocational college | 1117 (26.3) | 626 (56.0) | 491 (44.0) | 1.05 (0.82 to 1.35) | |
| Bachelor/master's degree and above | 1965 (46.3) | 1008 (51.3) | 957 (48.7) | 0.94 (0.73 to 1.21) | |
| Occupation | |||||
| Government staff/civil servants | 1324 (31.2) | 681 (51.4) | 643 (48.6) | 1.12 (0.84 to 1.50) | |
| Ordinary worker | 1260 (29.7) | 768 (61.0) | 492 (39.0) | 1.54 (1.13 to 2.09)** | |
| Business/service personnel | 823 (19.4) | 455 (55.3) | 368 (44.7) | <0.001 | 1.24 (0.91 to 1.69) |
| Housewife/retiree | 504 (11.9) | 266 (52.8) | 238 (47.2) | 1.20 (0.85 to 1.70) | |
| Student | 334 (7.9) | 151 (45.2) | 183 (54.8) | Reference | |
| Current location | |||||
| Wuhan | 2855 (67.3) | 1562 (54.7) | 1293 (45.3) | 0.948 | |
| Other | 1390 (32.7) | 759 (54.6) | 631 (45.4) | ||
| Quarantine status | |||||
| Yes | 3974 (93.6) | 2233 (56.2) | 1741 (43.8) | <0.001 | 2.35 (1.80 to 3.08)*** |
| No | 271 (6.4) | 88 (32.5) | 183 (67.5) | Reference | |
| Total score of institutional trust in information provision and preventive behaviours | |||||
| 0–21 | 2037 (48.0) | 895 (43.9) | 1142 (56.1) | <0.001 | Reference |
| 21–24 | 2208 (52.0) | 1426 (64.6) | 782 (35.4) | 2.22 (1.96 to 2.52)*** | |
*p<0.05, **p<0.01, ***p<0.001.
Hosmer–Lemeshow test, χ2=8.096, p=0.424; Nagelkerke R2=0.086.
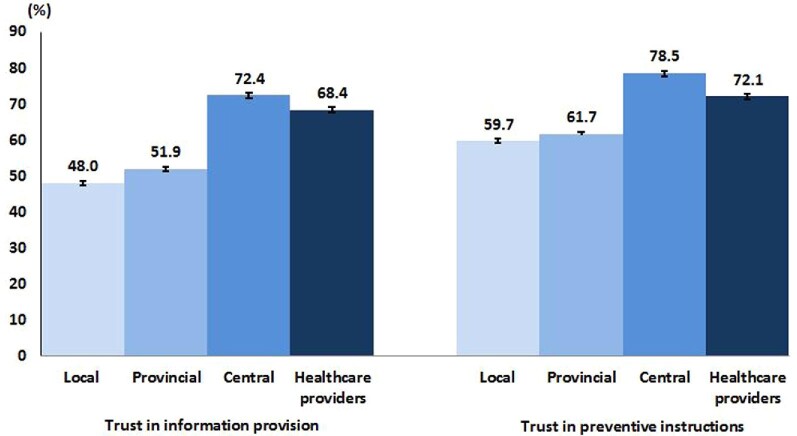
Figure 2 shows the results of institutional trust for both information provision and preventive instruction. The majority of the participants expressed great trust in the information provision (72.4%) and preventive instructions (78.5%) from the central government authority. The level of trust in the information provision (68.4%) and preventive instruction (72.1%) from healthcare providers was lower than that of the central government authority. The lowest levels of trust in information provision and preventive instruction were for the local and provincial government authorities. An even lower proportion expressed a great extent of trust in information provision (48.0%) and preventive instructions (59.7%) given by the local authority. There were no significant associations between score differences in information provision and preventive measures. The total scores of institutional trust for information provision and preventive instruction ranged from 0 to 24. The median score was 22 (IQR 18–24). The total score was categorized into two groups—22–24 and 0–21—based on the median split; as such, a total of 2208 (52.0%) were categorized as having a score of 22–24 and 2037 (48.0%) had a score of 0–21.
Figure 2.
Institutional trust for information provision and preventive instruction (N=4245).
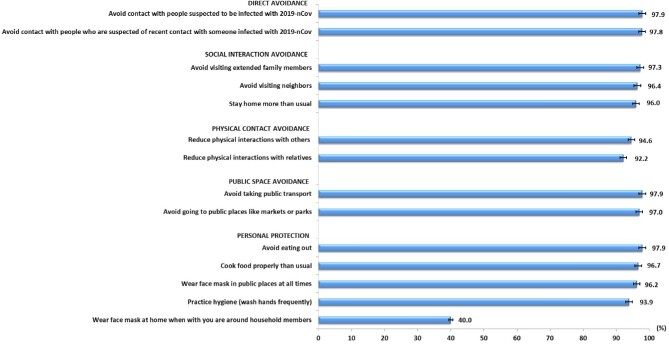
Figure 3 shows the distribution of self-reported preventive practices. The uptake of preventive practices was high in the study population. However, only 40% reported wearing a face mask at home when they were with other household members. The scores of preventive practices in the study population ranged from 7 to 28. The median score was 27 (IQR 26–28). The preventive practices scores were categorized as a score of 27–28 or 7–26 based on the median split; as such, a total of 2321 (54.7%) were categorized as having a score of 27–28 and 1924 (45.3%) had a score of 7–26.
Figure 3.
Proportion of ‘frequent’ responses for preventive practices (N=4245).
Table 1 shows the univariate and multivariable analyses of factors associated with preventive practices scores. In the univariate analysis there were significant associations between the preventive practices scores and age group, highest educational attainment, occupational type, quarantine status and the total score of institutional trust. In the multivariate analysis, under quarantine (adjusted OR 2.35 [95% CI 1.80 to 3.08]) and having a high institutional trust score (OR 2.23 [95% CI 1.96 to 2.53]) were two strong significant determinants of higher preventive practices scores. Participants in the age group 26–35 y (OR 1.64 [95% CI 1.24 to 2.16]) and 36–45 y (OR 1.30 [95% CI 0.98 to 1.73]) had significantly higher preventive practices scores than those in the age group 56–70 y.
Figure 4 shows the treatment-seeking intention of the study population. Most participants (85.7% [n=3640]) reported that they would seek treatment at the hospital, whereas 42% (n=1782) reported that they would seek traditional healing and 62.4% (n=2651) reported a preference for self-treatment. A total of 462 (46.3%) participants >45 y of age reported a preference for using traditional healing (χ2=13.649, degrees of freedom=3, p=0.011). There was no significant difference in the use of self-healing by participants’ age. Table 2 shows the univariate and multivariable analyses of factors associated with intention to seek treatment in the hospital. In the univariate analysis, all of the factors studied, except for the age group, were significantly associated with intention to seek treatment in the hospital. Of note, 16.6% (n=475) of the participants from the city of Wuhan reported no intention of seeking treatment in the hospital, whereas 13.8% (n=550) of participants who were in the quarantine area reported no intention of seeking treatment in the hospital. Similarly, in the multivariable analysis, being quarantined (OR 2.36 [95% CI 1.80 to 3.09]) and having a high institutional trust score (OR 2.20 [95% CI 1.96 to 2.49]) were two strong significant determinants of intention to seek treatment in the hospital.
Figure 4.
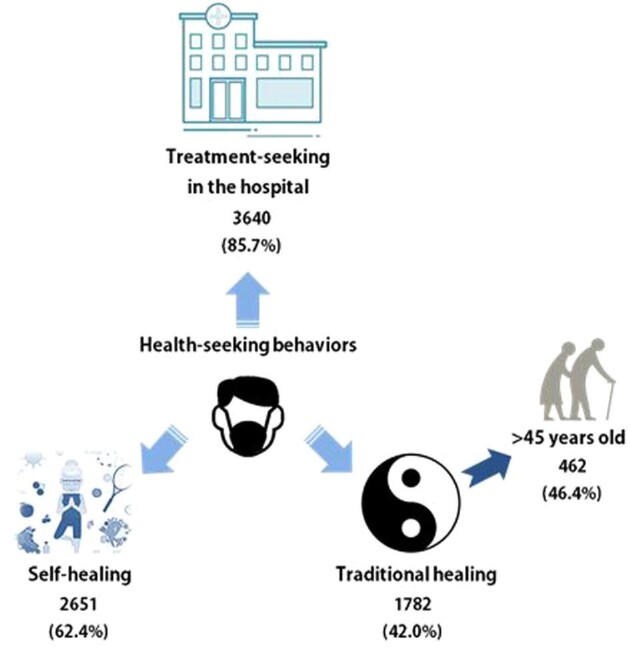
Treatment-seeking intentions (N=4245).
Table 2.
Factors associated with intention to seek treatment in the hospital (N=4245)
| Univariate analysis | Multivariable analysisa | ||||
|---|---|---|---|---|---|
| Treatment-seeking in hospital | Treatment seeking in hospital, yes vs no | ||||
| Covariates | n (%) | Yes (n=3640) | No (n=605) | p-Value | OR (95% CI) |
| Demographic characteristics | |||||
| Age group (years) | |||||
| 18–25 | 782 (18.4) | 655 (83.8) | 127 (16.2) | ||
| 26–35 | 1515 (35.7) | 1297 (85.6) | 218 (14.4) | 0.346 | |
| 36–45 | 953 (22.4) | 824 (86.5) | 129 (13.5) | ||
| 46–55 | 685 (16.1) | 591 (86.3) | 94 (13.7) | ||
| 56–70 | 310 (7.3) | 273 (88.1) | 37 (11.9) | ||
| Gender | |||||
| Male | 1754 (41.3) | 1549 (88.3) | 205 (11.7) | 1.01 (0.89 to 1.15) | |
| Female | 2491 (58.7) | 2091 (83.9) | 400 (16.1) | <0.001 | Reference |
| Highest education level | |||||
| Middle school and below | 380 (9.0) | 340 (89.5) | 40 (10.5) | Reference | |
| High school/technical secondary school | 783 (18.4) | 709 (90.5) | 74 (9.5) | <0.001 | 1.22 (0.94 to 1.58) |
| Junior college/vocational college | 1117 (26.3) | 977 (87.5) | 140 (12.5) | 1.12 (0.87 to 1.43) | |
| Bachelor/master's degree and above | 1965 (46.3) | 1614 (82.1) | 351 (17.9) | 1.04 (0.81 to 1.32) | |
| Occupation | |||||
| Government staff/civil servant | 1324 (31.2) | 1105 (83.5) | 219 (16.5) | 1.18 (0.92 to 1.52) | |
| Ordinary worker | 1260 (29.7) | 1110 (88.1) | 150 (11.9) | 1.66 (1.28 to 2.16)*** | |
| Business/service personnel | 823 (19.4) | 718 (87.2) | 105 (12.8) | 0.002 | 1.38 (1.06 to 1.81)* |
| Housewife/retiree | 504 (11.9) | 434 (86.1) | 70 (13.9) | 1.19 (0.88 to 1.61) | |
| Student | 334 (7.9) | 273 (81.7) | 61 (18.3) | Reference | |
| Current location | |||||
| Wuhan | 2855 (67.3) | 2380 (83.4) | 475 (16.6) | <0.001 | Reference |
| Other | 1390 (32.7) | 1260 (90.6) | 130 (9.4) | 0.94 (0.82 to 1.08) | |
| Quarantine status | |||||
| Yes | 3974 (93.6) | 3424 (86.2) | 550 (13.8) | 0.005 | 2.36 (1.80 to 3.09)*** |
| No | 271 (6.4) | 216 (79.7) | 55 (20.3) | Reference | |
| Total score of institutional trust in information provision and preventive behaviours | |||||
| 0–21 | 2037 (48.0) | 1604 (78.7) | 433 (21.3) | <0.001 | Reference |
| 21–24 | 2208 (52.0) | 2036 (92.2) | 172 (7.8) | 2.20 (1.94 to 2.49)*** | |
*p<0.05, **p<0.01, ***p<0.001.
Hosmer–Lemeshow test, χ2=2.231, p=0.973; Nagelkerke R2=0.079.
Discussion
This study was conducted during the early onset of the COVID-19 outbreak in China. With the aim of understanding public behaviour in prevention measures in this crisis that has now become a worldwide concern, this study collected data at the COVID-19 outbreak epicentre during a period of exponential growth of the epidemic. This study found a considerably high level of institutional trust in both information provision and recommendations among the public. However, trust (both information provision and recommendations) in the local authority was lower than that in the provincial and central government. The cause of lack of trust in local authorities during the COVID-19 outbreak is unknown and beyond the scope of this present study. Future studies should consider investigating the lack of public trust towards local authority. This finding is in contrast to the study on the Ebola outbreak in the Democratic Republic of Congo, where their public expressed higher trust in local authorities.8 Local governments are key agencies that play an important role in the management of COVID-19 at the community level. They are also the front line in service delivery during the outbreak. The low level of trust in local governments warrants considerable attention and there is a need to enhance public trust in local authorities. Lack of trust in local authorities results in poor cooperation, thus undermining contact tracing and adherence to recommended public health interventions.12,13 The high level of public trust in the central government found in this study shows the importance of informing the public of central–local government relationships in handling the crisis and the consistency of enforcement at all levels of government. Healthcare providers can be strong advocates for outbreak prevention efforts in the communities, and many expressed a high level of trust in them.
On a positive note, this study revealed that the people in the epicentres adopted a high level of prevention measures. As noted, however, only a relatively small proportion reported using face masks at home when they were around household members. During the study period, wearing a mask at home was not obligatory in China. People with symptoms were advised to wear masks to prevent transmission between family members and face masks were only compulsory in public places. However, wearing a face mask in public places and at home when around other household members is advisable based on the CDC recommendation and the Australian Department of Health.14,15 Considering that human-to-human transmission among close family members has been reported in countries such as Germany, Japan and Vietnam, the community in Hubei province and the epicentres should be made aware of the essential importance of wearing face masks when they are around other household members.
The main strength of this study is the finding of the strong influence of institutional trust on overall preventive behaviours, in good agreement with previous studies.8,12 As the COVID-19 pandemic is still growing exponentially, continued strengthening of institutional trust, and in particular increasing the trust in the local authority, is essential for emergency management. The study also found that uptake of prevention practices was poorer among older members of the public, which warrants serious attention. It has been found that older adults affected by COVID-19 are likely to have a higher risk of complications and mortality.4 There is a need to find out whether a lack of appropriate prevention practices among people of older age is due to knowledge deficiency or to their being out-of-reach of current public health intervention.
The finding that nearly 15% of people would be reluctant to seek treatment in the hospital if they were suspected to have been infected with COVID-19 is clinically important and worrisome. Of utmost importance, a proportion of those participants are in the city of Wuhan and currently under quarantine. The preference for using traditional healing among a minority of the older respondents is also of concern. Refusal to seek hospital treatment not only leads to serious respiratory distress and can be life-threatening, but also increases the chances of spreading the disease. People who favour traditional healing should be made aware that seeking conventional treatment in the hospital and obeying the quarantine order are the most appropriate actions in containing this outbreak. Finally, the finding of the strong influence of institutional trust on seeking conventional treatment again amplifies the immense importance of building trust between the public and government authorities.
This study has several limitations that should be considered. The first pertains to the cross-sectional nature of the study. Thus it cannot be used to infer causality. Second, the responses were based on self-reports and may be subject to biases in self-reported demographics and a tendency to report socially desirable prevention practices and treatment-seeking intentions. Therefore the results should be interpreted with caution. Third, the snowball data collection method via mobile phone used in this study can lead to selection bias. The sample may not be representative of the population in Hubei, as reflected in the large number of females, people in the younger age groups and those with higher education. However, using mobile phones as a survey tool enables rapid collection of data, as well as wide coverage of responses, as smartphone ownership in China is reported to be as high as 96%.16 Despite these limitations, the study data contribute tremendously to understanding public responses.
In conclusion, bridging the trust gaps between the public and local authorities in the epicentres is crucial. It is of utmost urgency to carry out public health interventions to reach out to individuals with poor adherence to preventive measures and who are reluctant to seek conventional medical care. Considering the extremely contagious nature of COVID-19, non-compliance by even a small portion of the population may have grave consequences and contribute to the continued increase in cases.
Acknowledgements
We would like to express our special appreciation to all the study participants.
Contributor Information
Li Ping Wong, HwaMei Hospital, University of Chinese Academy of Sciences; Ningbo Institute of Life and Health Industry, University of Chinese Academy of Sciences; Centre for Epidemiology and Evidence-Based Practice, Department of Social and Preventive Medicine, Faculty of Medicine, University of Malaya 50603, Kuala Lumpur, Malaysia.
Qunhong Wu, Department of Social Medicine, Health Management College, Harbin Medical University, Harbin, Heilongjiang Province, China.
Yanhua Hao, Department of Social Medicine, Health Management College, Harbin Medical University, Harbin, Heilongjiang Province, China.
Xi Chen, Yale School of Public Health, PO Box 208034, New Haven, CT 06520, USA.
Zhuo Chen, College of Public Health, University of Georgia, Athens, GA 30602, USA; School of Economics, University of Nottingham Ningbo China, 315100 Ningbo, Zhejiang Province, China.
Haridah Alias, Centre for Epidemiology and Evidence-Based Practice, Department of Social and Preventive Medicine, Faculty of Medicine, University of Malaya 50603, Kuala Lumpur, Malaysia.
Mingwang Shen, Department of Epidemiology and Biostatistics, School of Public Health, Xi'an Jiaotong University Health Science Center, Xi'an, Shanxi 710061, China.
Jingcen Hu, Department of Epidemiology, Zhejiang Provincial Key Laboratory of Pathophysiology, School of Medicine, Ningbo University, Ningbo, Zhejiang, China.
Shiwei Duan, HwaMei Hospital, University of Chinese Academy of Sciences.
Jinjie Zhang, College of Food and Pharmaceutical Sciences, Ningbo University, Ningbo 315000, China.
Liyuan Han, HwaMei Hospital, University of Chinese Academy of Sciences; Ningbo Institute of Life and Health Industry, University of Chinese Academy of Sciences; College of Food and Pharmaceutical Sciences, Ningbo University, Ningbo 315000, China.
Authors’ contributions
QW, XC, ZC, MS, JH, SD, JZ and LYH conceived and designed the study. LPW and HA analysed the data. LPW wrote the first draft of the manuscript. All authors interpreted the data and contributed to subsequent drafts of the manuscript. All authors have read and approved the final version..
Funding
This work is supported by the National Key R&D Program of China (grants 2017YFC1310902 and 2018YFC1315305), Ningbo Health Branding Subject Fund (grant PPXK2018-02), Sanming Project of Medicine in Shenzhen (grant SZSM201803080), K.C. Wong Magna Fund in Ningbo University, National Natural Science Foundation of China (grant 11801435 [to MS]), Fundamental Research Funds for the Central Universities (grant xjh012019055), China Postdoctoral Science Foundation (grant 2018M631134) and Natural Science Basic Research Program of Shanxi Province (grant 2019JQ-187).
Competing interests
None declared.
Ethical approval
Not required. This survey was part of a continuing public health outbreak investigation during the state of emergency in Wuhan and the need for ethical approval was waived by the institutional review board.
Data availability
The authors have the research data, which are available upon reasonable request.
References
- 1. Lu H, Stratton CW, Tang YW.. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. J Med Virol. 2020;92(4):401–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hui DS, Azhar IE, Madani TAet al. . The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264––6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Clinical management of severe acute respiratory infection when novel coronavirus (nCoV) infection is suspected: interim guidance. Available from: https://www.who.int/internalpublications-detail/clinical-management-of-severe-acute-respiratoryinfection-when-novel-coronavirus-(ncov)-infection-is-suspected[accessed 30 January 2020]. [Google Scholar]
- 4. Chen N, Zhou M, Dong Xet al. . Epidemiological and clinical characteristics of 99 cases of 2019-novel coronavirus (2019-nCoV) pneumonia in Wuhan, China. Lancet. 2020;395(10223):507–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lu R, Zhao X, Li Jet al. . Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leung GM, Ho LM, Chan SKet al. . Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin Infect Dis. 2005;40(12):1713–20. [DOI] [PubMed] [Google Scholar]
- 7. Vaughan E, Tinker T.. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Public Health. 2009;99(Suppl 2):S324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vinck P, Pham PN, Bindu KKet al. . Institutional trust and misinformation in the response to the 2018–19 Ebola outbreak in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis. 2019;19(5):529–36. [DOI] [PubMed] [Google Scholar]
- 9. World Health Organization . Statement on the second meeting of the International Health Regulations. Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) [accessed 31 January 2020].
- 10. Wu C, Wilkes R.. Local–national political trust patterns: why China is an exception. Int Polit Sci Rev. 2018;39(4):436–54. [Google Scholar]
- 11. Hosmer DW Jr, Lemeshow S, Sturdivant RX. Applied logistic regression. Hoboken, NJ: John Wiley & Sons; 2013 [Google Scholar]
- 12. Kutalek R, Wang S, Fallah Met al. . Ebola interventions: listen to communities. Lancet Glob Health. 2015;3(3):e131. [DOI] [PubMed] [Google Scholar]
- 13. Meredith LS, Eisenman DP, Rhodes H. et al. Trust influences response to public health messages during a bioterrorist event. J Health Commun. 2007;12(3):217–32. [DOI] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention. Influenza (Flu). Interim guidance for the use of masks to control seasonal influenza virus transmission. Available from: https://www.cdc.gov/flu/professionals/infectioncontrol/maskguidance.htm [accessed 1 February 2020].
- 15. Australian Government Department of Health . Home isolation guidance when unwell (suspected or confirmed cases). Available from: https://www.health.gov.au/sites/default/files/documents/2020/03/coronavirus-covid-19-information-about-home-isolation-when-unwell-suspected-or-confirmed-cases.pdf [accessed 7 May 2020]. [Google Scholar]
- 16. Delloite . Chinese consumers at the forefront of digital technologies: 2018 Deloitte China Mobile Consumer Survey. Available from: https://www2.deloitte.com/cn/en/pages/technology-media-and-telecommunications/articles/2018-deloitte-china-mobile-consumer-survey.html [assessed 9 December 2020]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors have the research data, which are available upon reasonable request.