Abstract
The COVID-19 pandemic has had profound health and social impacts. COVID-19 also affords opportunities to study the emergence of prejudice as a factor in taking protective actions. This study investigated the association of COVID-19 concerns, prejudicial beliefs, and personal actions that involve life disruptions among people not living with and people living with HIV. 338 Black/African American men not living with HIV who reported male sex partners and 148 Black/African American men living with HIV who reported male sex partners completed a confidential survey that measured COVID-19 concern, COVID-19 prejudice, and personal action and institutionally imposed COVID-19 disruptions. Participants reported having experienced multiple social and healthcare disruptions stemming from COVID-19, including reductions in social contacts, canceling medical appointments, and inability to access medications. Mediation analyses demonstrated that COVID-19 concerns and COVID-19 prejudice were associated with personal action disruptions, indicating that these social processes are important for understanding how individuals modified their lives in response to COVID-19. It is imperative that public health efforts combat COVID-19 prejudice as these beliefs undermine investments in developing healthcare infrastructure to address COVID-19 prevention.
Keywords: COVID-19, HIV, Risks, Prejudice, Life disruptions
Implications.
Research: Protective behaviors against perceived health threats are mediated by prejudicial beliefs among both more and less vulnerable populations.
Practitioners: Patients may express prejudicial beliefs against populations associated with COVID-19 in their efforts to psychologically distance themselves from the threat of disease.
Policymakers: Public health messaging to mitigate the spread of COVID-19 should consider potential impacts of messages on propagating disease-related prejudices.
Introduction
The SARS-CoV-2 (the virus that causes COVID-19) pandemic rapidly amplified to become the greatest threat to global health in the modern era. The only means of mitigating the spread of this highly contagious respiratory virus in its first year, before safe and effective vaccines were available, was through strict social distancing practices, including the avoidance of close shared spaces, wearing facial coverings and practicing hand-washing hygiene [1]. Although social distancing effectively slows the spread of COVID-19, limiting social contacts comes with social, emotional, economic, and other costs [2]. The widespread direct impacts of COVID-19 on health, as well as the direct and indirect impacts resulting from life disruptions, may have their greatest impact on people at high-risk for severe complications of COVID-19, especially older persons and those with underlying health conditions [2–5].
Life disruptions that accompany social distancing restrictions include limiting contact with personal relationships, diminishing social support, and impeding access to essential resources such as food, medicine, and healthcare [4,6]. Personally initiating and complying with social distancing restrictions are motivated by concerns for contracting and transmitting COVID-19 [7,8]. Individuals who express greater concern about contracting COVID-19 may also be among those most affected by social distancing and therefore experience more life disruptions [9]. In addition to motivating protective behaviors, increased perceived threat (e.g., personal concerns) of contracting COVID-19 may have the unintended consequences of stigmatizing and fostering prejudice against people who have contracted the virus [10,11]. Stigmatization of COVID-19 arises out of the perceived threats posed by the disease itself and are fueled by attitudes and perceptions that attribute blame for COVID-19 to individuals, social groups, and even countries [12–15].
Prejudice is often defined by generally negative attitudes toward groups [16] and is theorized to serve as a social mechanism to prompt emotional and behavioral reactions in response to perceived threats [16]. A threat-based approach to prejudice posits that concerns regarding physical well-being, including health threats, activate stereotypes toward targeted groups, which in turn elicit emotional responses, including reactions related to prejudice [17]. From an evolutionary perspective, prejudice can function as a mechanism against pathogen threats in a behavioral immune system [18]. The role of disease prejudice in self-protection, including practicing disease avoidance mitigation strategies, poses a potential public health dilemma [19]. Public health messaging to communicate the threat of an infectious disease may promote prejudice, whereas efforts to reduce prejudice could unintentionally undermine threat-heightening messaging [20]. The degree to which COVID-19 prejudice contributes to disease concerns and personal actions against COVID-19 among persons at greater risk for more severe disease outcomes has not yet been reported.
Among those at greatest risk for severe COVID-19 disease are individuals with underlying chronic health conditions, including people with compromised immune systems [21–23]. While the factors and combinations of underlying conditions that determine COVID-19 severity are under investigation, it is now established that immune system disorders, including diseases that suppress the immune system such as HIV infection, potentially contribute to greater risks for COVID-19 severity [24–27]. People with HIV, therefore, may have a heightened sense of concern for contracting COVID-19 [28–30]. Threat response perspectives of prejudice suggest that prejudice will motivate threat management to a greater degree among individuals at greater risk for a disease [16,20]. Thus, the implications for considering prejudice in COVID-19 public health messaging may differ for those at greater risk for severe COVID-19 (i.e., people living with HIV) and those at lower-risk (people not living with HIV).
The current study tested the hypothesis that COVID-19 prejudice would be associated with personal action COVID-19 disruptions and would account for the association (e.g., mediate) between personal concerns for contracting COVID-19 and personal action COVID-19 disruptions. Our study was conducted in a high-COVID-19 prevalence setting and focused on both men who are living with and not living with HIV. We restricted our sample to Black/African American men who have sex with men because they are disproportionately impacted by both HIV and COVID-19 [31,32]. We used a moderated mediation model to test the hypothesis that COVID-19 concerns would be associated with personal action COVID-19 disruptions, and that this association would be accounted for, at least in part, by COVID-19 prejudices. In this model, we also examined whether the direct and indirect effects of COVID-19 concerns and prejudice varied by HIV status. We hypothesized that prejudice would mediate the association between COVID-19 concerns and disruptions to a greater degree among men living with HIV relative to men not living with HIV.
METHODS
Participants and procedures
Participants were 338 men not living with HIV and 148 men living with HIV recruited through online advertisements and chain referrals. Advertisements were placed within a 50-mile radius of Atlanta, GA, an area of the country with among the highest HIV infection rates [33] and among the earliest high-rates of COVID-19 in the United States [34]. Participants were recruited through social media outlets and snowball chain referrals. Eligibility criteria included age 18 and older, identifying as African-American/Black, and having had at least one male sex partner in the previous 6-months. Participants were interpersonally screened through a video-chat platform. Participants were asked their HIV status and those who reported living with HIV were asked to confirm their status by showing a name-matching HIV test result, HIV viral load report, or antiretroviral therapy (ART) medication bottle. All participants were aware of COVID-19 at the time of the study.
Following a phone conducted enrollment interview for informed consent, participants were sent a link to complete a self-administered survey on an internet-connected device of the participant’s choosing. The measures were programmed using the REDcap automated survey collection tool. Measures were delivered in two assessments in order to reduce time burden. Data collection occurred between April 13 and July 2, 2020. The University of Connecticut Institutional Review Board approved all study procedures.
Measures
Demographic and health characteristics
Participants reported their basic demographic information, including age, marital status, race, education, and income. Participants also reported the last time they had been tested for HIV and their results. We asked participants living with HIV whether they were currently receiving HIV care, receiving ART, and their most recent HIV viral load.
Concern about COVID-19
We assessed participant concern that they may contract COVID-19 using a 100-point rating scale in response to the question: “From 0 to 100, how concerned are you about catching COVID-19,” with 0 = “Not at all concerned” and 100 = “Extremely concerned.”
COVID-19 prejudice
This scale was constructed for the current study using 7-items that were derived from media accounts of COVID-19 acts of prejudice, discrimination and xenophobia in the early months of the COVID-19 pandemic [12,14,35] as well as conceptual bases for prejudicial beliefs directed toward people living with HIV [36]. Consistent with previous research, prejudice in our measure refers to negative emotions such as anger and fear that people who are not diagnosed with a communicable disease may hold against people who have been diagnosed with a disease [36]. Example items include “It should be a crime for people who know they have the virus but do not take steps to prevent from spreading it,” “People who test positive for the new virus should be required to wear identification tags,” “I am afraid of people who have this new virus,” and “People who have been to China in the past year should not be allowed into the United States.” Items were responded to on 6-point scales, from 0 = “Strongly disagree” to 5 = “Strongly agree.” Mean scores ranged from 0 to 5 and the measure was internally consistent (Cronbach’s α = .87).
COVID-19 life disruptions
Participants reported whether they had experienced 12 disruptions to social relationships and healthcare as a result of COVID-19. Disruptions included five personal actions taken by individuals to mitigate risk for contracting COVID-19 and seven disruptions resulting from institutional responses intended to slow the spread of COVID-19. The items are shown in the results section. The COVID-19 disruptions were responded to using 3-options to indicate whether the participant had experienced each: 0 = “No,” 1 = “Yes, a little,” and 2 = “Yes, a lot.” We formed an index of personal actions to avoid COVID-19 by summing the five personal action items, with a possible range of 0 to 10 and sample range of 0 to 9, median = 6.
Data analyses
We conducted descriptive analyses for demographic and health characteristics and COVID-19 life disruptions on the sample partitioned by HIV status using contingency table X2 tests for categorical variables and independent t-tests for continuous variables. We examined the bivariate correlations among participant age, COVID-19 concerns, COVID-19 prejudice, and personal action COVID-19 disruptions using Pearson Correlation coefficients. Separate correlation matrixes were constructed for participants living with and not living with HIV, with differences between correlation coefficients tested using z-tests.
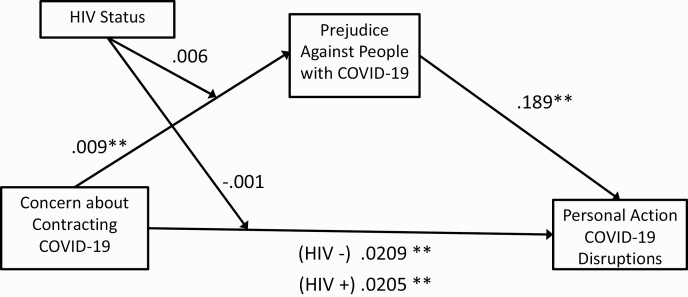
Our main analyses tested the moderated mediation model shown in Fig. 1, specifying the associations between COVID-19 concerns → COVID-19 prejudice → personal action COVID-19 disruptions. HIV status was included as a moderator of the effects of COVID-19 concerns. We used the SPSS mediation macro designed by Hayes [37] to test the direct and indirect effects using bootstrap statistical techniques. Mediation models are appropriately analyzed using regression when data are cross-sectional [38]. The macro estimates all direct paths designated in the model. For this analysis we used the model 8 template to test moderated mediation in an x–y relationship [37]. The model tests the association between the predictor variable (COVID-19 concerns) and the mediator variable (COVID-19 prejudice, a path), the association between the mediator and the outcome (personal action COVID-19 disruptions, b path), and the conditional direct effects of the predictor variable on the outcome for participants living with and not living with HIV (the c paths). We also computed 95% confidence intervals (CI) for the conditional indirect effects of COVID-19 concerns on personal action COVID-19 disruptions through COVID-19 prejudice for participants that were and were not living with HIV estimated from 5,000 bootstrap resamples.
Fig 1.
Moderated mediation model testing for the association of COVID-19 concerns and COVID-19 life disruptions through COVID-19 prejudice. Note: ** p < .01.
There were no missing items or scales for variables included in the model. We conducted a sensitivity analysis with four participants reporting having been diagnosed with COVID-19 removed. In addition, we repeated the mediation model with participant age, education, and income included as covariates because older age is associated with greater risk for severe COVID-19 health outcomes and there were education and income differences between the HIV status groups. All analyses used p < .05 as the criterion for statistical significance.
RESULTS
Table 1 shows the demographic and health characteristics of men participating in the study partitioned by HIV status. Compared to men who were not living with HIV, participants living with HIV reported being older in age, having fewer years of education, lower incomes, and greater unemployment. In addition, participants living with HIV were more likely to believe they had contracted the virus that causes COVID-19, were more likely tested for COVID-19, more concerned about COVID-19, and had higher COVID-19 prejudice scores. Nearly all participants living with HIV were taking HIV medications and 88% reported having undetectable HIV viral loads.
Table 1.
Demographic and health characteristics of participants not living with HIV and participants living with HIV
| Not living with HIV (N =338) | Living with HIV (N = 148) | ||||
|---|---|---|---|---|---|
| Characteristic | N | % | N | % | X 2 |
| Education | |||||
| Less than high school | 5 | 2 | 10 | 34 | 33.5** |
| Graduated high school | 55 | 16 | 50 | 59 | |
| At least some college | 278 | 82 | 88 | 70 | |
| Annual income < $25,000 | 176 | 52 | 103 | 70 | 19.7** |
| Currently unemployed | 90 | 27 | 52 | 35 | 14.8** |
| Currently in HIV care | 139 | 94 | |||
| Currently taking antiretroviral therapy | 141 | 96 | |||
| Most recent HIV viral load | |||||
| Detectable | 10 | 7 | |||
| Undetectable | 130 | 88 | |||
| Does not know | 8 | 5 | |||
| Believe they have had COVID-19 | 4 | 1 | 21 | 14 | 35.6** |
| Has been tested for COVID-19 | 46 | 14 | 41 | 47 | 13.9** |
| Tested positive for COVID-19 | 0 | 4 | 3 | ||
| M | SD | M | SD | t | |
| Age in years | 29.3 | 5.5 | 33.8 | 8.2 | 7.0** |
| Concerned about contracting COVID-19 | 63.4 | 31.8 | 70.9 | 33.0 | 2.3* |
| Personal action COVID-19 disruptions | 6.2 | 2.1 | 6.4 | 2.0 | 0.9 |
| COVID-19 prejudice score | 2.9 | 1.2 | 3.3 | 1.7 | 3.1** |
Note: * p < .05, ** p < .01
COVID-19 personal action and institution-imposed disruptions
Table 2 shows the frequencies of COVID-19 disruptions as indicated by responding “Yes, a lot,” for participants not living with and living with HIV. With respect to personal action COVID-19 disruptions, a sizable majority of the sample reported staying home and away from others to avoid contracting COVID-19. A majority (60%) of participants also indicated avoiding public transportation. Disruptions also included interference with healthcare, with 45% of men living with HIV having canceled care appointments. For institutionally imposed COVID-19 disruptions, more than one in five participants were unable to get the food they needed because of COVID-19. As would be expected given greater regularly utilizing health services among people living with HIV, interruptions to healthcare occurred more often for participants living with HIV.
Table 2.
COVID-19 disruptions among participants not living with HIV and participants living with HIV
| Not living with HIV (N =338) | Living with HIV (N = 148) | ||||
|---|---|---|---|---|---|
| Personal actions | N | % | N | % | X 2 |
| Staying indoors and away from public places | 247 | 73 | 116 | 78 | 1.6 |
| Canceled plans that involved other people | 245 | 73 | 103 | 70 | 1.5 |
| You cancelled a clinic or doctor’s appointment because of the coronavirus. | 100 | 30 | 67 | 45 | 11.2** |
| You asked others to stay away to avoid getting the coronavirus. | 156 | 46 | 72 | 49 | 0.3 |
| You avoided public transportation because of the coronavirus. | 206 | 61 | 88 | 60 | 0.4 |
| Institutionally imposed | |||||
| A clinic or doctor closed or canceled your appointment because of the coronavirus. | 112 | 33 | 94 | 63 | 38.9** |
| A service provider of any type closed or canceled your appointment because of the coronavirus. | 139 | 41 | 96 | 65 | 23.2** |
| Been unable to get the food that you need. | 68 | 20 | 40 | 27 | 3.3 |
| Been unable to get to the pharmacy because of the coronavirus. | 36 | 11 | 27 | 18 | 5.6 |
| Been unable to get the medicine you need because of the coronavirus. | 30 | 9 | 23 | 16 | 4.7 |
| You were asked by others to stay away to protect them from getting the coronavirus. | 147 | 44 | 74 | 50 | 3.2 |
| You were told not to come to work or school because of the coronavirus. | 192 | 57 | 75 | 5 | 2.3 |
Note: “Yes, a lot” response category shown, ** p < .01.
Bivariate correlations
Table 3 shows the Pearson correlations among COVID-19 concern, prejudice and personal action disruptions for participants living with HIV (above the diagonal) and participants not living with HIV (below the diagonal). All three COVID-19 variables were significantly correlated with each other for both participants not living with and living with HIV. Results from z-tests for differences between the pairs of correlation coefficients for participants not living with and living with HIV indicated that there were no differences in the magnitude of the associations; concern – prejudice, z =.541, ns; concern – disruptions z =.462, ns; and prejudice – disruptions, z = .846, ns.
Table 3.
Pearson correlation coefficients for COVID-19 concern, prejudice and personal action disruptions among participants living with HIV (above diagonal) and participants not living with HIV (below diagonal)
| COVID-19 concern | COVID-19 prejudice | COVID-19 disruptions | |
|---|---|---|---|
| COVID-19 Concern | − | .29** | .38** |
| COVID-19 Prejudice | .24** | − | .26** |
| COVID-19 Disruptions | .34** | .18** | − |
Note: ** p < .01.
COVID-19 concern, prejudice, and personal action COVID-19 disruptions
We tested the moderated mediation model shown in Fig. 1 using multiple regression analyses that included COVID-19 concerns as the independent variable and personal action COVID-19 disruptions as the dependent variable, with COVID-19 prejudice entered as the mediator variable, and HIV status as the moderator. The model was significant in predicting personal action COVID-19 disruptions, model F = 19.38, p < .001, accounting for 13.9% of the variance. Results showed that the direct effect of COVID-19 concerns on COVID-19 prejudice was significant, B = .009 (SE =.002), t = 3.98, p < .001. The HIV status × COVID-19 concerns interaction on COVID-19 prejudice was not significant, B = .006 (SE = .004), t = 1.51, p > .10. The direct effect of COVID-19 prejudice on COVID-19 disruptions was significant, B = .189, (SE = .066), t = 2.87, p < .001. In addition, the conditional direct effect of COVID-19 concerns on COVID-19 disruptions was significant for participants not living with HIV, B = .020 (SE =.003), t = 6.11, p < .001, and the conditional direct effect of COVID-19 concerns on COVID-19 disruptions was also significant for participants living with HIV, B = .020 (SE =.005), t = 4.08, p < .001. The HIV status × COVID-19 concerns interaction on COVID-19 disruptions was not significant, B = −.001 (SE = .006), t = 0.07, p > .10.
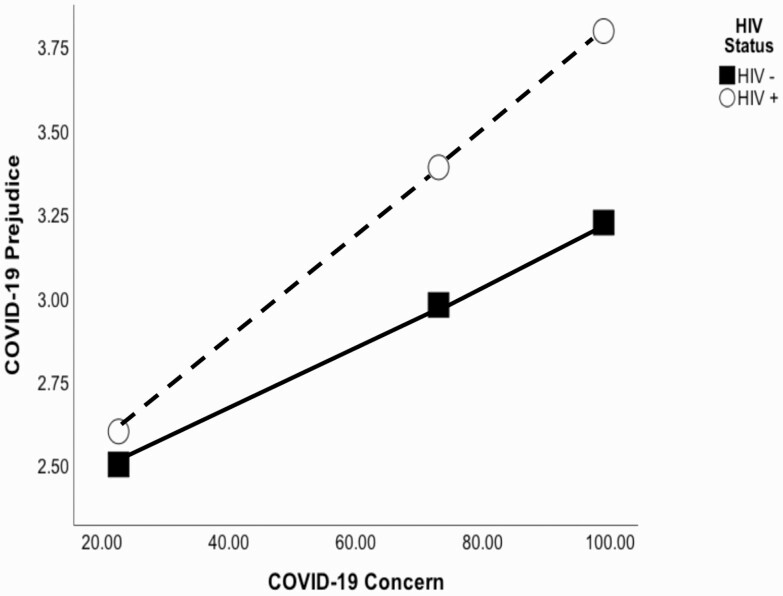
The conditional indirect effect of COVID-19 concerns on COVID-19 disruptions through prejudice (COVID-19 concerns → COVID-19 prejudice → COVID-19 disruptions) was significant for men not living with HIV, B = .0018 (SE = .0008), 95% CI .0004−.0035, as it was for men living with HIV, B = .0029, (SE =.0015) 95% CI .0006−.0063. Tests for HIV status as a moderating variable did not indicate significant moderator effects; the index of moderated mediation was not significant, B =.0012 (SE = .0011), 95% CI −.0005 to .0037. Figure 2 shows the associations between COVID-19 concerns (X axis set at the median = 73 and 16th and 84th percentiles, 23 and 99, respectively), and mean COVID-19 prejudice scores. As shown in the figure, higher COVID-19 concerns were related to greater prejudice and the differences between participants not living with and living with HIV at each level of concern and prejudice were not significant.
Fig 2.
Relationships between COVID-19 concerns and prejudice for participants not living with HIV (HIV -) and participants living with HIV (HIV+).
Adjusting the model for covariates did not change the results. Age and income were not significant in any model effects. However, education was significantly related to COVID-19 prejudice, B = −.282 (SE = .084), t = 3.33, p < .001, and education was related to personal action COVID-19 disruptions, B = .386, (SE = .124), t = 3.11, p < .01. The model remained significant, model F = 12.71, p < .001, accounting for 15.7% of the variance. The direct effects all remained significant: concerns on prejudice, B = .010 (SE =.002), t = 4.37, p < .001, prejudice on disruptions, B = .217 (SE = .066), t = 3.27, p < .001, concerns on disruptions for participants not living with HIV, B = .0207 (SE =.003), t = 6.00, p < .001, and concerns on disruptions for participants living with HIV, B = .0212 (SE =.005), t = 4.24, p < .001. The conditional indirect effect for men not living with HIV, B = .0022 (SE = .0009), 95% CI .0008−.0041, and men living with HIV, B = .0031 (SE =.0014) 95% CI .0007−.0063, were also significant. The adjusted index of moderated mediation remained non-significant, B =.0009 (SE = .0012), 95% CI −.0012 to .0035. Finally, we repeated all analyses with the four participants who had been diagnosed with COVID-19 removed and there were no changes in the results.
Discussion
Results found that a sizable majority of participants reported having experienced multiple social and healthcare disruptions stemming from COVID-19, including reductions in social contacts, canceled medical appointments, and inability to access medications. It was common for participants to experience multiple disruptions related to their personal actions and stemming from institutional responses to COVID-19 that spanned across social relationships and healthcare. It is notable that both personal actions and institutionally imposed restrictions were associated with cancellation of medical services, indicating substantial impacts of COVID-19 on the healthcare of people living with HIV. COVID-19 disruptions were associated with the degree of concern participants expressed about contracting COVID-19, with greater concern indicating greater disruptions. Furthermore, we found that COVID-19 concerns and disruptions were significantly associated with COVID-19 prejudice. Results illustrate one potential route for how prejudice may function in a new communicable disease [18]. The paths that we constructed in our model imply that disease concerns are a precursor to prejudice. Alternatively, prejudicial beliefs may emerge in parallel to, or as a part of, disease concerns. It is also possible that prejudice precedes disease concerns. Our data do not allow for us to determine the temporality of associations between concerns, prejudice and personal actions, indicating a need for future longitudinal studies.
Results of the moderated mediation model confirmed our hypothesis that concern for contracting COVID-19 would predict personal action COVID-19 disruptions and that this association would be mediated by prejudicial beliefs. However, we did not confirm our hypothesis that the mediation model would be moderated by HIV status. We found that for both participants not living with and living with HIV, COVID-19 concerns predicted life disruptions through COVID-19 prejudice. The observed mediation was, however, only partial in that the direct effect of COVID-19 concern on life disruptions remained significant after accounting for COVID-19 prejudice. Results support the notion that prejudicial beliefs may have a role in response to perceived health threats [16,20]. One potential reason why there were no differences in the mediation model by HIV status is that the risks for severity among people living with HIV are uncertain, especially earlier in the COVID-19 crisis when these data were collected. In addition, the degree to which participants in this study personally experienced stigma and discrimination themselves, based on race, sexual orientation as well as HIV status may have influenced the results. Conceptualized as stressful life events, stigma experiences can lead to coping responses with positive outcomes, including responses to future stigma events [39–41]. For example, people living with HIV commonly experience stigma and discrimination related to their HIV diagnosis and these experiences may have buffered the predicted mediation effects of COVID-19 prejudice.
The current findings should be interpreted in light of their methodological limitations. The sample for this study was one of convenience and cannot be considered representative of any particular population. In addition, the sample was male and African-American/Black and therefore limited in its generalizability to women and people of various other racial backgrounds. It should also be noted that we recruited several participants from social media websites which may have influenced responses. The cross-sectional design of the study also precludes drawing any causal or directional conclusions. Our measures of social and healthcare disruptions were not exhaustive and we did not measure several individual behaviors that can be undertaken to reduce the spread of SARS-CoV-2, such as mask wearing and hand-washing hygiene. The study was undertaken in response to the early months of the COVID-19 public health crisis and our findings may therefore be transient and specific to this time period. With the exception of HIV status which was verified for people living with HIV, our study measures relied entirely on self-report instruments and were therefore subject to social response biases. Nevertheless, these findings have implications for public health communications and messaging in response to COVID-19.
One avenue for reducing prejudice is to diminish the perceived threat of COVID-19. By casting blame on those who contract COVID-19, people who have not been infected distance themselves from the disease through the social process of “othering” [42,43]. Prejudice therefore may function as a psychological dimension of social distancing, explaining its associations to concerns for contracting COVID-19 as well as personal action COVID-19 disruptions. Prejudice, in other words, may add to a sense of safety and security in the face of an invisible threat posed by a virus. Prejudice, however, fuels discrimination, inequity, and social injustice. Political rhetoric that tags a disease with a group affiliation, such as referring to the 1917 influenza as “Spanish Flu,” AIDS as “Gay Related Immune Deficiency (GRID),” and COVID-19 as the “China Virus,” is inflammatory, xenophobic and runs counter to a unified public health response. Furthermore, stigmatization of a disease itself undermines prevention and treatment [44,45]. Public health messaging is needed to actively counter the sources of prejudicial beliefs and ultimately squelch prejudicial rhetoric while simultaneously sustaining physical distancing and collective actions that render reduced risk for community spread of disease. Research has shown that messaging that emphasizes empathy and concern for those affected by COVID-19, and believing that collectively people can reduce the spread of the virus, results in greater compliance with social distancing [46]. Several approaches to prejudice reduction messaging have been found effective and should be incorporated into public health education around COVID-19. Interventions that include cooperative learning, collectivism, peer influence, and personal contact have all been shown to reduce prejudicial beliefs in experimental and field research [47]. Research is needed to determine whether public health messaging that aims to heighten concern and increase disease mitigation practice can also effectively deliver evidence-based approaches to reducing prejudice.
Funding: Research was supported by the National Institute of Mental Health grant R21-MH121314.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards: All authors declare that they have no conflicts of interest.
Human Rights All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent All participants provided written informed consent prior to data collection.
Ethical Statement The study procedures were approved by the University of Connecticut Institutional Review Board.
Author Contributions SCK, BS, MOK and LAE contributed to the conceptual development and execution of the study. SCK conducted the data analyses and all authors contributed to the preparation of the final manuscript.
Transparency Statements: This study was not formally registered. The analysis plan was not formally preregistered.
Data Availability: Deidentified data from this study are not available in public archive. Deidentified data from this study will be made available (as allowable according to institutional IRB standards) by emailing the corresponding author. Analytic code used to conduct the analyses presented in this study are not available in a public archive. They may be available by emailing the corresponding author. There is not analytic code associated with this study. Materials used to conduct the study are not publicly available.
References
- 1. Walensky RP, Del Rio C. From mitigation to containment of the COVID-19 pandemic: Putting the SARS-CoV-2 genie back in the bottle. JAMA. 2020;323(19):1889–1890. [DOI] [PubMed] [Google Scholar]
- 2. Moirano G, Schmid M, Barone-Adesi F. Short-term effects of mitigation measures for the containment of the COVID-19 outbreak: An experience from Northern Italy. Disaster Med Public Health Prep. 2020;14(4):e3–e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Akseer, N., et al. , COVID-19 pandemic and mitigation strategies: Implications for maternal and child health and nutrition. Am J Clin Nutr, 2020;112(2): 251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cawthon, P., et al. , Assessing the impact of the COVID-19 pandemic and accompanying mitigation efforts on older adults. J Gerontol A Biol Sci Med Sci, 2020;75(9):e123–e125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Melamed OC, Hahn MK, Agarwal SM, Taylor VH, Mulsant BH, Selby P. Physical health among people with serious mental illness in the face of COVID-19: Concerns and mitigation strategies. Gen Hosp Psychiatry. 2020;66:30–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marziali ME, Card KG, McLinden T, Wang L, Trigg J, Hogg RS. Physical distancing in COVID-19 may exacerbate experiences of social isolation among people living with HIV. AIDS Behav. 2020;24(8):2250–2252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weinstein N, Nguyen TV. Motivation and preference in isolation: A test of their different influences on responses to self-isolation during the COVID-19 outbreak. R Soc Open Sci. 2020;7(5):200458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gibson Miller J, Hartman TK, Levita L, et al. . Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. Br J Health Psychol. 2020;25(4):856–864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhang SX, Wang Y, Rauch A, Wei F. Unprecedented disruption of lives and work: Health, distress and life satisfaction of working adults in China one month into the COVID-19 outbreak. Psychiatry Res. 2020;288:112958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. St Lawrence JS, Husfeldt BA, Kelly JA, Hood HV, Smith S Jr. The stigma of AIDS: fear of disease and prejudice toward gay men. J Homosex. 1990;19(3):85–101. [DOI] [PubMed] [Google Scholar]
- 11. Gebbie KM. Open the door. AIDS Read. 1999;9(6):373–374. [PubMed] [Google Scholar]
- 12. Dyer O. Covid-19: Trump stokes protests against social distancing measures. BMJ. 2020;369:m1596. [DOI] [PubMed] [Google Scholar]
- 13. Budhwani H, Sun R. Creating COVID-19 stigma by referencing the novel coronavirus as the “Chinese virus” on Twitter: Quantitative analysis of social media data. J Med Internet Res. 2020;22(5):e19301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rzymski P, Nowicki M. Preventing COVID-19 prejudice in academia. Science. 2020;367(6484):1313. [DOI] [PubMed] [Google Scholar]
- 15. Habibi R, Burci GL, de Campos TC, et al. . Do not violate the International Health Regulations during the COVID-19 outbreak. Lancet. 2020;395(10225):664–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cottrell CA, Neuberg SL. Different emotional reactions to different groups: A sociofunctional threat-based approach to “prejudice”. J Pers Soc Psychol. 2005;88(5):770–789. [DOI] [PubMed] [Google Scholar]
- 17. Pirlott AG, Cook CL. Prejudices and discrimination as goal activated and threat driven: The affordance management approach applied to sexual prejudice. Psychol Rev. 2018;125(6):1002–1027. [DOI] [PubMed] [Google Scholar]
- 18. Kusche I, Barker JL. Pathogens and immigrants: A critical appraisal of the behavioral immune system as an explanation of prejudice against ethnic outgroups. Front Psychol. 2019;10:2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Logie CH, Turan JM. How do we balance tensions between COVID-19 public health responses and stigma mitigation? Learning from HIV research. AIDS Behav. 2020;24(7):2003–2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cook CL, Li Y, Newell M, Cottrell C, Neel R. The world is a scary place: Individual differences in belief in a dangerous world predict specific intergroup prejudices. Group Process Intergroup Relat, 2018; 21(4):584–596. [Google Scholar]
- 21. Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. Lancet HIV. 2020;7(5):e308–e309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Blanco, J, Ambrosioni, J, Garcia, F, Martínez, E, Soriano, A, Mallolas, J, Miro, JM; on behalf the COVID-19 in HIV Investigators . COVID-19 in patients with HIV: Clinical case series. Lancet HIV, 2020;7:E314–E316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Adepoju P, Tuberculosis and HIV responses threatened by COVID-19. Lancet HIV, 2020;7:E319–E320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang R, Pan, M, Zhang, X, Han, M, Fan, X, Zhao, F, Miao, M, Xu, J, Guan, M, Deng, X, Chen, X, Shen, L. Epidemiological and clinical features of 125 hospitalized patients with COVID-19 in Fuyang, Anhui, China, Int J Infect Dis. 2020; 95:421–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Harris OO, Leblanc N, McGee K, Randolph S, Wharton MJ, Relf M. Alarm at the gate-health and social inequalities are comorbid conditions of HIV and COVID-19. J Assoc Nurses AIDS Care. 2020;31(4):367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Laurence J. Why aren’t people living with HIV at higher risk for developing severe coronavirus disease 2019 (COVID-19)? AIDS Patient Care STDS. 2020;34(6):247–248. [DOI] [PubMed] [Google Scholar]
- 27. Del Amo J, Polo R, Moreno S, et al. ; The Spanish HIV/COVID-19 Collaboration . Incidence and severity of COVID-19 in HIV-positive persons receiving antiretroviral therapy: A cohort study. Ann Intern Med. 2020;173(7):536–541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Algarin AB, Varas-Rodríguez E, Valdivia C, et al. . Symptoms, stress, and HIV-related care among older people living with HIV during the COVID-19 pandemic, Miami, Florida. AIDS Behav. 2020;24(8):2236–2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Edelman EJ, Aoun-Barakat L, Villanueva M, Friedland G. Confronting another pandemic: Lessons from HIV can inform our COVID-19 response. AIDS Behav. 2020;24(7):1977–1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Harkness A, Behar-Zusman V, Safren SA. Understanding the impact of COVID-19 on Latino sexual minority men in a US HIV hot spot. AIDS Behav. 2020;24(7):2017–2023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Borno HT, Zhang S, Gomez S. COVID-19 disparities: An urgent call for race reporting and representation in clinical research. Contemp Clin Trials Commun. 2020;19:100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Centers for Disease Control and and Prevention. HIV Surveillance Report, 2018. (Updated). Atlanta, GA: Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 34. CDC COVID-19 Response Team. Geographic Differences in COVID-19 Cases, Deaths, and Incidence — United States, February 12–April 7, 2020 Morb Mortal Wkly Rep, 2020;69(15):465–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rzymski P, Nowicki M. COVID-19-related prejudice toward Asian medical students: A consequence of SARS-CoV-2 fears in Poland. J Infect Public Health. 2020;13(6):873–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hayes AF. Model Templates for Process for SPSS and SAS. 2013: Guilford Press, New York: Guilford Press. [Google Scholar]
- 38. Judd CM, Kenny DA. Process analysis: Estimating mediation in treatment evaluations. Eval Rev, 1981;5(5):602–619. [Google Scholar]
- 39. Frost DM. Stigma and intimacy in same-sex relationships: A narrative approach. J Fam Psychol. 2011;25(1):1–10. [DOI] [PubMed] [Google Scholar]
- 40. Jewkes R. Beyond stigma: Social responses to HIV in South Africa. Lancet. 2006;368(9534):430–431. [DOI] [PubMed] [Google Scholar]
- 41. Frost DM. Social stigma and its consequences for the socially stigmatized. Soc Personality Psych Compass, 2011;5(11):824–839. [Google Scholar]
- 42. Walton JA, Lazzaro-Salazar M. Othering the chronically ill: a discourse analysis of New Zealand health policy documents. Health Commun. 2016;31(4):460–467. [DOI] [PubMed] [Google Scholar]
- 43. Johnson JL, Bottorff JL, Browne AJ, Grewal S, Hilton BA, Clarke H. Othering and being othered in the context of health care services. Health Commun. 2004;16(2):255–271. [DOI] [PubMed] [Google Scholar]
- 44. Dalbeth N, Douglas M, MacKrill K, Te Karu L, Kleinstäuber M, Petrie KJ. The impact of the illness label ‘gout’ on illness and treatment perceptions in Māori (Indigenous New Zealanders). BMC Rheumatol. 2020;4:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Krasnoryadtseva A, Derksen C, Dalbeth N, Petrie KJ. Not every picture tells a story: A content analysis of visual images in patient educational resources about gout. J Rheumatol. 2020;47(12):1815–1821. [DOI] [PubMed] [Google Scholar]
- 46. Chomaa B, Hodson G, Sumantrya D, Hanoch., Gummerum M. Ideological and psychological predictors of COVID-19-related collective action, opinions, and health compliance across three nations. J Soc Personality Psych 2021;9(1):123–143. [Google Scholar]
- 47. Paluck EL, Green DP. Prejudice reduction: what works? A review and assessment of research and practice. Annu Rev Psychol. 2009;60:339–367. [DOI] [PubMed] [Google Scholar]