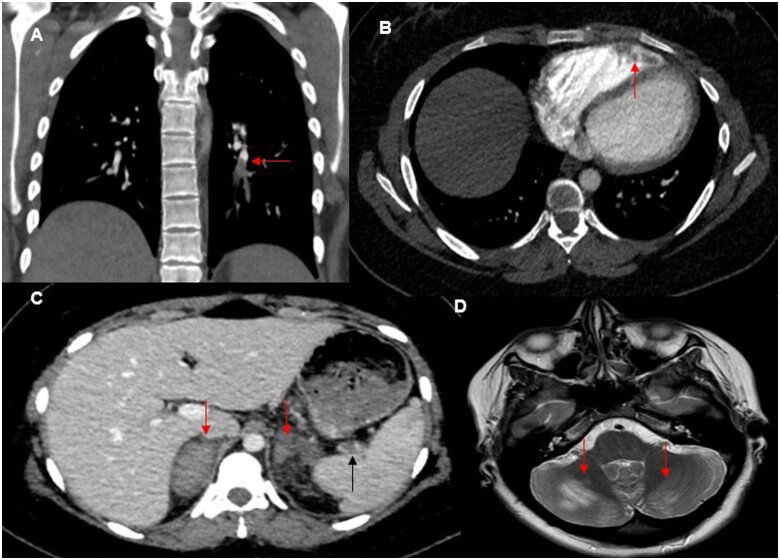
A 23-year-old patient without any risk factor of thromboembolic disease presented with chest pain and breathlessness within 1 week of receiving the COVID-19 vaccine. The patient’s CT revealed pulmonary emboli (Panel A) and she was treated with Apixaban. Despite treatment, her condition deteriorated. Her blood results identified thrombocytopenia (73 × 109/L), elevated D-dimer (17 548 μg/L), and normal haemoglobin, clotting and troponin. SARS-CoV-2 polymerase chain reaction and antibody tests were consistent with vaccination rather than recent infection (anti-S IgG positive, anti-Spike positive, and anti-Nucleocapsid negative). A repeat CT showed right ventricle (RV) thrombus (Panel B), splenic vein thrombus (Panel C, black arrow), and bilateral adrenal haemorrhage (Panel C, red arrows). Echocardiogram confirmed the RV thrombus. The patient’s brain MRI showed high T2 areas in the cerebellum (Panel D) with restricted diffusion, which could represent embolic infarcts or posterior reversible encephalopathy syndrome. The initial working diagnoses included infection, catastrophic antiphospholipid syndrome, and vaccine-triggered immune reaction. Investigations including broncho-alveolar lavage for viral/bacterial/fungal infections, anti-phospholipid, and lupus anticoagulant screens were all negative. The patient required intubation and ventilation with plasma exchange, intravenous methylprednisolone, and heparin infusion. She made a full recovery. Based on our experience, patients could also present with headache/seizures due to cerebral venous sinus thrombosis, and/or intra-parenchymal brain haemorrhage. The syndrome is rare but as the vaccination rollout becomes global, early recognition of the syndrome among clinicians is key for prompt treatment to minimize morbidity and mortality.
Conflict of interest: The authors have submitted their declaration which can be found in the article Supplementary Material online.