Abstract
Background
Many injection drug users (IDUs) seek care at emergency departments and some require hospital admission because of late presentation in the course of their illness. We determined the predictors of frequent emergency department visits and hospital admissions among community-based IDUs and estimated the incremental hospital utilization costs incurred by IDUs with early HIV infection relative to costs incurred by HIV-negative IDUs.
Methods
The Vancouver Injection Drug User Study (VIDUS) is a prospective cohort study involving IDUs that began in 1996. Our analyses were restricted to the 598 participants who gave informed consent for our study. We used the participants' responses to the baseline VIDUS questionnaire and, from medical records at St. Paul's Hospital, Vancouver, we collected detailed information about the frequency of emergency department visits, hospital admissions and the primary diagnosis for all visits or hospital stays between May 1, 1996, and Aug. 31, 1999. The incremental difference in hospital utilization costs by HIV status was estimated, based on 105 admissions in a subgroup of 64 participants.
Results
A total of 440 (73.6%) of the 598 IDUs made 2763 visits to the emergency department at St. Paul's Hospital during the study period. Of these 440, 265 (60.2%) made frequent visits (3 or more). The following factors were associated with frequent use: HIV-positive status (seroprevalent: adjusted odds ratio [OR] 1.7, 95% confidence interval [CI] 1.2–2.6; seroconverted during study period: adjusted OR 3.0, 95% CI 1.6–5.7); more than 4 injections daily (adjusted OR 1.5, 95% CI 1.1–2.1); cocaine use more frequent than use of other drugs (adjusted OR 2.0, 95% CI 1.2–3.6); and unstable housing (adjusted OR 1.5, 95% CI 1.1–2.2). During the study period 210 of the participants were admitted to hospital 495 times; 118 (56.2%) of them were admitted frequently (2 or more admissions). The 2 most common reasons for admission were pneumonia (132 admissions among 79 patients) and soft-tissue infections (cellulitis and skin abscess) (90 admissions among 59 patients). The following factors were independently associated with frequent hospital admissions: HIV-positive status (seroprevalent: adjusted OR 5.4, 95% CI 3.4–8.6; seroconverted during study period: adjusted OR 2.9, 95% CI 1.4–6.0); and female sex (adjusted OR 1.8, 95% CI 1.1–3.1). The incremental hospital utilization costs incurred by HIV-positive IDUs relative to the costs incurred by HIV-negative IDUs were $1752 per year.
Interpretation
Hospital utilization was significantly higher among community-based IDUs with early HIV disease than among those who were HIV negative. Much of the hospital use was related to complications of injection drug use and may be reduced with the establishment of programs that integrate harm reduction strategies with primary care and addiction treatment.
Many injection drug users (IDUs) use emergency departments as a regular source of care because of the lack of accessible primary care services or their inability to attend set appointment times.1,2,3,4 Poor health status among IDUs because of drug use, HIV infection or hepatitis C is common, and some IDUs present later in the course of an illness and thus require hospital admission.4,5,6,7,8 IDUs at all stages of HIV infection are admitted to hospital significantly more often than non-IDUs with HIV infection.9
Because hospital admissions among HIV-positive IDUs are largely attributable to complications of injection drug use10 that are not directly related to the HIV infection, it is unclear whether community-based HIV-negative IDUs have similar hospital utilization patterns as IDUs with early HIV disease. Other studies of health care use by IDUs have been in the setting of drug treatment or clinics and reflect a highly selected population.11,12 We therefore conducted this study to determine the predictors of frequent emergency department use among community-based IDUs. We also examined the predictors of frequent hospital admission and reviewed the primary diagnosis for each encounter. To assess whether there was a difference in hospital utilization costs according to HIV status, we estimated the incremental costs incurred by IDUs with early stage disease relative to costs incurred by HIV-negative IDUs. With the rising prevalence of HIV infection among IDUs in many Canadian cities, including Vancouver,13,14 these data may be crucial for planning and evaluating programs that provide appropriate health care services to reduce drug-related harm among active IDUs with or at risk of HIV infection.
Methods
We obtained informed consent from 598 participants of the Vancouver Injection Drug User Study (VIDUS) to review their medical records at St. Paul's Hospital, the main teaching hospital for IDUs and HIV care in Vancouver. The hospital's Committee on Human Experimentation approved the study. The research design and methods of the VIDUS have been previously described;13 the primary aim was to determine the risk practices associated with HIV seroconversion. In brief, subjects were eligible to participate in the VIDUS if they had injected illicit drugs in the month before enrolment and resided in the Greater Vancouver region. Most participants (82%) were recruited through word of mouth and street outreach programs. Participants provided blood samples for HIV antibody testing and responded to an interviewer-administered questionnaire semi-annually. Responses from the baseline survey were used for our analyses. We reviewed medical records from St. Paul's Hospital for the 598 participants to determine the frequency of emergency department use and hospital admissions as well as the presenting problem for each emergency department visit and the primary diagnosis for each hospital admission between May 1, 1996, and Aug. 31, 1999.
Hospital utilization costs were estimated according to the inpatient resource-utilization profiles of a random sample of 64 participants who were admitted to hospital during the study period. Our cost estimates were for the first 105 admissions. For each admission, information was abstracted from the medical records, including the nursing ward, medications received, investigations, physicians' visits and length of stay. To distinguish between costs and charges,15 we estimated inpatient unit costs using a model of simultaneous allocation16 of all expenditures including overhead, opportunity cost of hospital resources as well as a 5% global depreciation of capital equipment.
Contingency tables were used to examine associations between frequent users and nonfrequent users of the emergency department and hospital by their HIV status and other sociodemographic and behavioural characteristics. We defined a priori frequent emergency department use as 3 or more visits and frequent hospital admission as 2 or more stays during the study period. We classified HIV status as seroprevalent (n = 166), seroconverted (for HIV seroconversions that occurred during the study period) (n = 51) and negative (n = 381). Unstable housing was defined as living in a single-occupancy room hotel, boarding room, hostel, transition house, jail or on the street in the 6 months before enrolment in the study.3,13 The Wilcoxon rank-sum test was used to compare continuous variables.
To identify independent predictors of frequent emergency department use, variables significant at the 0.05 level in the univariate analysis were entered into logistic regression models in a stepwise, hierarchical fashion. In the final model, all relevant 2-way interactions were considered. This procedure was also performed to identify predictors of frequent hospital admission. We also compared self-reported hospital admissions in the 6 months before entry into the study and at follow-up (1999) by HIV status to assess the extent to which HIV-negative IDUs could have been admitted to hospital elsewhere.
To estimate the incremental difference in hospital utilization costs between IDUs with early HIV infection and HIV-negative IDUs, the average daily cost was multiplied by the median length of stay and then the annualized frequency of hospital admission per person by HIV status.17 We performed 2-way sensitivity analyses using the lower and upper limits of the 95% confidence interval (CI) for the hospital utilization costs and simultaneously varying the length of stay by calculating the difference in length of stay by HIV status using the 25th and 75th percentiles.
Results
Hospital utilization
Of the 598 participants included in our analysis, 440 (73.6%) of them visited the emergency department a total of 2763 times during the 39-month study period. Of these 440 IDUs, 265 (60.2%) visited the emergency department frequently and 91 (20.7%) visited more than 10 times. The annualized frequency of emergency department use by HIV status was 2.6 for the IDUs with seroprevalent HIV infection (1171 visits among 137 patients), 2.9 for the IDUs with seroconverted HIV infection (387 visits among 41 patients) and 1.4 for the HIV-negative IDUs (1205 among 262 patients). The 2 most common reasons for visiting the emergency department were soft-tissue infections (cellulitis and skin abscess) and problems directly related to illicit drug use (e.g., drug intoxication, overdose and drug withdrawal) (Table 1).
Table 1
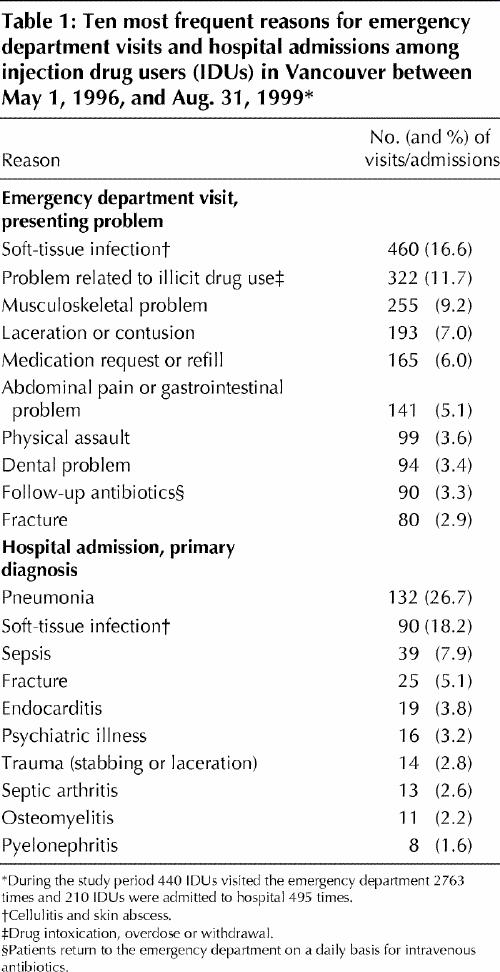
Overall, 210 (35.1%) of the 598 participants were admitted to the hospital 495 times during the study period. Of these 210, 118 (56.2%) were admitted frequently and 21 (10.0%) had 5 or more admissions. The annualized frequency of hospital admissions by HIV status was 0.89 for the IDUs with seroprevalent HIV infection (294 admissions among 102 patients), 0.80 for the IDUs with seroconverted HIV infection (52 admissions among 20 patients) and 0.52 for the HIV-negative IDUs (149 admissions among 88 patients). The 2 most common reasons for admission were pneumonia (132 admissions among 79 patients) and soft-tissue infections (cellulitis and skin abscess, 90 admissions among 59 patients) (Table 1). The HIV-negative IDUs were less likely than the HIV-positive IDUs to report hospital admissions in the 6 months before entry into the study (odds ratio [OR] 0.43, 95% CI 0.29–0.67) and in the 6 months before follow-up (OR 0.48, 95% CI 0.29–0.77).
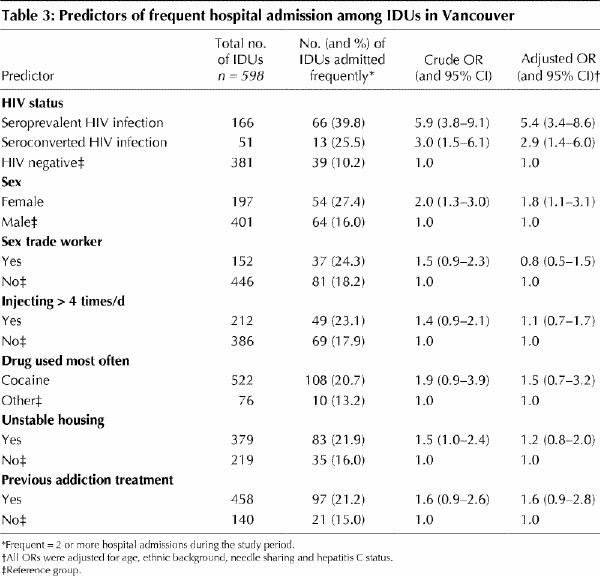
The crude and adjusted ORs for the predictors of frequent emergency department use and frequent hospital admission are shown in Tables 2 and 3 respectively. Logistic regression analysis showed that frequent emergency department use was associated with HIV infection (seroprevalent: adjusted OR 1.7, 95% CI 1.2–2.6; seroconverted: adjusted OR 3.0, 95% CI 1.6–5.7), injection more than 4 times daily (adjusted OR 1.5, 95% CI 1.1–2.1), cocaine use more frequent than use of other drugs; adjusted OR 2.0, 95% CI 1.2–3.6) and unstable housing (adjusted OR 1.5, 95% CI 1.1–2.2). The following factors were independently associated with frequent hospital admission: HIV infection (seroprevalent: adjusted OR 5.4, 95% CI 3.4–8.6; seroconverted: adjusted OR 2.9, 95% CI 1.4–6.0) and female sex (adjusted OR 1.8, 95% CI 1.1–3.1).
Table 2
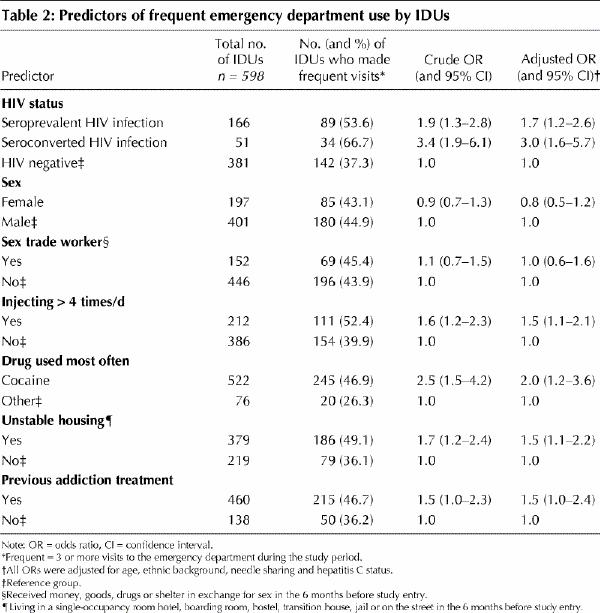
Table 3
Utilization costs
The 64 IDUs included in the subgroup cost analysis were admitted to hospital 184 times during the study period. Of the 64 participants, 33 had seroprevalent HIV infection at baseline and 5 became HIV positive during the study period, with a median CD4 count of 389 х 106/L (interquartile range [IQR] 216–592 х 106/L) at their first hospital admission. The 5 who became HIV positive during the study period had not been admitted to hospital when they were HIV negative. The IDUs who were HIV-positive had a longer length of stay (median 7 days, IQR 5–12 days) than the HIV-negative IDUs (median 5 days, IQR 4–8 days). The annualized frequency of hospital admissions was 0.96 among the seroprevalent HIV-positive IDUs and 0.77 among the HIV-negative IDUs. The fully allocated average hospital utilization cost per day was $610.33 (95% CI $575.70–$644.96). The incremental hospital utilization cost incurred by the HIV-positive IDUs relative to the HIV-negative IDUs was $1752 per year (the sensitivity analyses showed that the incremental cost varied from $990 to $3457 per year).
Interpretation
We found that the HIV-positive IDUs visited the emergency department and were admitted to hospital substantially more often than the HIV-negative IDUs. This may have been due to continued high-risk injection behaviours, particularly among the IDUs who became HIV positive during the study period. Our annualized frequency of emergency department use among the HIV-negative IDUs was higher than the estimate reported by French and associates4 (1.4 v. 0.78); the same was true for the annualized frequency of hospital admissions (0.52 v. 0.32). These differences may have been due to differences in population, health care systems and ascertainment of health care use (self-report versus actual).
Our finding that female sex was an independent predictor of frequent hospital admission is consistent with previous findings.6,18,19 The recent HIV Costs and Services Utilization Study in the United States reported that the suboptimal pattern of care among women and IDUs was largely mitigated by adjusting for insurance coverage and race or ethnic background.20 Comparisons with US findings are difficult given differences in the health care systems and the demographic composition of the study populations. The association between the use of cocaine and unstable housing with frequent emergency department use has been noted elsewhere.21,22,23,24
The predominant reasons for hospital admission (pneumonia and soft-tissue infections) in our study are directly and indirectly related to needle use and highlight the importance of counselling and providing the tools necessary to practise safe injection techniques. In a study by Stein,10 HIV-positive IDUs were admitted to an urban hospital primarily because of injection-related complications. In another study, involving IDUs in drug treatment, those with early HIV infection used more ambulatory and inpatient services than HIV-negative IDUs.12 An increased biological susceptibility to bacterial infections8,25 or poor hygiene and high-risk drug injection practices13,26 are possible explanations for the higher frequency of hospital admissions among HIV-positive IDUs.
Our study had several limitations. First, we may have underestimated the emergency department and hospital use because the participants may have received care from other hospitals. Second, we did not capture outpatient clinic visits. Third, we used a relatively small sample of IDUs to estimate the hospital utilization costs. Finally, the study participants may not be representative of all IDUs, because those in the lowest socioeconomic group may have been overrepresented in our study population.
Our cost analysis builds on previous work in that we examined actual hospital costs for IDUs by assigning fully allocated costs of actual resource use. In other studies costs were derived from charge data,4,10,27 or aggregated service utilization costs were used to calculate costs per patient-year.28,29 The incremental hospital utilization costs incurred by the HIV-positive IDUs relative to the costs incurred by the HIV-negative IDUs were $1752 per person; this translates into an additional $197 976 per year for hospital care for the 113 HIV-positive IDUs who were admitted to hospital during our study period.
A recent study reported high hospital use and costs among poor people in Toronto.30 Our results provide some reasons for their findings among the IDU subgroup. Much of the health care use was largely attributable to complications of injection drug use, regardless of HIV status. The use of sterile injecting equipment and safe injection practices might have prevented many of these conditions and, thus, reduced the need for emergency department visits or hospital admissions.31,32 Programs that integrate harm reduction strategies with primary care and addiction treatment33,34 should be considered by jurisdictions serving this vulnerable population.
Footnotes
This article has been peer reviewed.
Acknowledgements: We thank Kathy Li for the statistical analyses, Laura Kuyper for database management, the Vancouver Injection Drug User Study (VIDUS) staff and the VIDUS Community Advisory Board.
This research was funded by the British Columbia Health Research Foundation, the National Institutes of Health (grant R01 DA11591-01), the British Columbia Ministry of Health and Health Canada. Anita Palepu was supported by a National Health Research Scholar Award from the National Health Research and Development Program of Health Canada, and Martin Schechter was supported by a National AIDS Research Scientist Award.
Competing interests: None declared.
Correspondence to: Dr. Anita Palepu, Rm. 620B, St. Paul's Hospital, 1081 Burrard St., Vancouver BC V6Z 1Y6; fax 604 806-8005; anita@hivnet.ubc.ca
References
- 1.Solomon L, Frank R, Vlahov D, Astemborski J. Utilization of health services in a cohort of intravenous drug users with known HIV-1 serostatus. Am J Public Health 1991;81:1285-90. [DOI] [PMC free article] [PubMed]
- 2.Markson LE, Houchens R, Fanning TR, Turner BJ. Repeated emergency department use by HIV-infected persons: effect of clinic accessibility and expertise in HIV care. J Acquir Immune Defic Syndr Hum Retrovirol 1998;17:35-41. [DOI] [PubMed]
- 3.Palepu A, Strathdee SA, Hogg RS, Anis AH, Rae S, Cornelisse PG, et al. The social determinants of emergency department and hospital use by injection drug users in Canada. J Urban Health 1999;76:409-18. [DOI] [PMC free article] [PubMed]
- 4.French MT, McGeary KA, Chitwood DD, McCoy CB. Chronic illicit drug use, health services utilization and the cost of medical care. Soc Sci Med 2000;50:1703-13. [DOI] [PubMed]
- 5.Weber AE, Yip B, O'Shaughnessy MV, Montaner JS, Hogg RS. Determinants of hospital admission among HIV-positive people in British Columbia. CMAJ 2000;162(6):783-6. Available: www.cma.ca/cmaj/vol-162/issue-6/0783.htm [PMC free article] [PubMed]
- 6.Aday L. Health status of vulnerable populations. Annu Rev Public Health 1994;15:487-509. [DOI] [PubMed]
- 7.Guydish J, Bucardo J, Clark G, Bernheim S. Evaluating needle exchange: a description of client characteristics, health status, program utilization, and HIV risk behavior. Subst Use Misuse 1998;33:1173-96. [DOI] [PubMed]
- 8.Stein MD. Medical complications of intravenous drug use. J Gen Intern Med 1990;5:249-57. [DOI] [PubMed]
- 9.Brettle RP, Willcocks L, Cowan FM, Richardson AM. Inpatient health care utilization for patients with HIV and AIDS in the Edinburgh City Hospital. Int J STD AIDS 1994;5:194-201. [DOI] [PubMed]
- 10.Stein MD. Injected-drug use: complications and costs in the care of hospitalized HIV-infected patients. J Acquir Immune Defic Syndr 1994;7:469-73. [PubMed]
- 11.Umbricht-Schneiter A, Ginn DH, Pabst KM, Bigelow GE. Providing medical care to methadone clinic patients: referral versus on-site care. Am J Public Health 1994;84:207-10. [DOI] [PMC free article] [PubMed]
- 12.Stein MD, O'Sullivan PS, Ellis P, Perrin H, Wartenberg A. Utilization of medical services by drug abusers in detoxification. J Subst Abuse 1993;5:187-93. [DOI] [PubMed]
- 13.Strathdee SA, Patrick DM, Currie SL, Cornelisse PG, Rekart ML, Montaner JS, et al. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS 1997;11:F59-65. [DOI] [PubMed]
- 14.Patrick DM, Strathdee SA, Archibald CP, Ofner M, Craib KJ, Cornelisse PG, et al. Determinants of HIV seroconversion in injection drug users during a period of rising prevalence in Vancouver. Int J STD AIDS 1997;8:437-45. [DOI] [PubMed]
- 15.Finkler SA. The distinction between cost and charges. Ann Intern Med 1982; 96:102-9. [DOI] [PubMed]
- 16.Drummond M. Methods for the evaluation of health care programmes. Oxford: Oxford University Press; 1996.
- 17.Anis AH, Hogg RS, Wang XH, Yip B, Palepu A, Montaner JS, et al. Modelling the potential economic impact of viral load-driven triple drug combination antiretroviral therapy. Pharmacoeconomics 1998;13:697-705. [DOI] [PubMed]
- 18.Solomon L, Stein M, Flynn C, Schuman P, Schoenbaum E, Moore J, et al. Health services use by urban women with or at risk for HIV-1 infection: the HIV Epidemiology Research Study (HERS). J Acquir Immune Defic Syndr Hum Retrovirol 1998;17:253-61. [DOI] [PubMed]
- 19.Hulka B, Wheat J. Patterns of utilization: the patient perspective. Med Care 1985;23:438-60. [DOI] [PubMed]
- 20.Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, et al. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA 1999;281:2305-15. [DOI] [PubMed]
- 21.Padgett DK, Struening EL. Influence of substance abuse and mental disorders on emergency room use by homeless adults. Hosp Community Psychiatry 1991;42:834-8. [DOI] [PubMed]
- 22.Bangsberg D, Tulsky JP, Hecht FM, Moss AR. Protease inhibitors in the homeless. JAMA 1997;278:63-5. [PubMed]
- 23.Smith MY, Rapkin BD, Winkel G, Springer C, Chabra R, Feldman IS. Housing status and health care service utilization among low-income persons with HIV/AIDS. J Gen Intern Med 2000;15:731-8. [DOI] [PMC free article] [PubMed]
- 24.Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA 2001;285:200-6. [DOI] [PubMed]
- 25.Selwyn PA, Alcabes P, Hartel D, Buono D, Schoenbaum EE, Klein RS, et al. Clinical manifestations and predictors of disease progression in drug users with human immunodeficiency virus infection. N Engl J Med 1992;327:1697-703. [DOI] [PubMed]
- 26.Archibald CP, Ofner M, Strathdee SA, Patrick DM, Sutherland D, Rekart ML, et al. Factors associated with frequent needle exchange program attendance in injection drug users in Vancouver, Canada. J Acquir Immune Defic Syndr Hum Retrovirol 1998;17:160-6. [DOI] [PubMed]
- 27.Bentham WD, Cai L, Schulman KA. Characteristics of hospitalizations of HIV-infected patients: an analysis of data from the 1994 healthcare cost and utilization project. J Acquir Immune Defic Syndr 1999;22(5):503-8. [DOI] [PubMed]
- 28.Beck EJ, Whitaker L, Kennelly J, McKevitt C, Wadsworth J, Miller DL, et al. Changing presentation and survival, service utilization and costs for AIDS patients: insights from a London referral centre. AIDS 1994;8:379-84. [DOI] [PubMed]
- 29.Beck EJ, Kennelly J, McKevitt C, Whitaker L, Wadsworth J, Miller DL, et al. Changing use of hospital services and costs at a London AIDS referral centre, 1983–1989. AIDS 1994;8:367-77. [DOI] [PubMed]
- 30.Glazier RH, Badley EM, Gilbert JE, Rothman L. The nature of increased hospital use in poor neighbourhoods: findings from a Canadian inner city. Can J Public Health 2000;91:268-73. [DOI] [PMC free article] [PubMed]
- 31.Vlahov D, Sullivan M, Astemborski J, Nelson KE. Bacterial infections and skin cleaning prior to injection among intravenous drug users. Public Health Rep 1992;107:595-8. [PMC free article] [PubMed]
- 32.Van Haastrecht HJ, Bindels PJ, Sluijs TA, Van den Hoek AA, Reijneveld SA, Coutinho RA. The impact of drug users on inpatient hospital care during the human immunodeficiency virus epidemic in Amsterdam. Int J Epidemiol 1996;25:846-53. [DOI] [PubMed]
- 33.McGeary KA, French MT. Illicit drug use and emergency room utilization. Health Serv Res 2000;35:153-69. [PMC free article] [PubMed]
- 34.Laine C, Hauck WW, Gourevitch MN, Rothman J, Cohen C, Turner BJ. Regular outpatient medical and drug abuse care and subsequent hospitalization of persons who use illicit drugs. JAMA 2001;285:2355-62. [DOI] [PubMed]


