Abstract
Background:
Adverse Childhood Experiences (ACEs) are potentially traumatic childhood events associated with negative health outcomes. Limited data on ACEs exists from low- and middle-income countries (LMICs). No ACEs studies have been done in Honduras.
Objective:
This study assessed the prevalence of ACEs in Honduras and associated health risks and risk behaviors among young adults.
Participants and setting:
Data from the 2017 Honduras Violence Against Children and Youth Survey (VACS) were used. Analyses were restricted to participants ages 18–24 years (n = 2701).
Methods:
This study uses nationally representative VACS data to estimate the weighted prevalence of ACEs (physical, emotional, and sexual violence; witnessing violence; parental migration). Logistic regression analyses assessed the relationship between individual ACEs, cumulative ACEs, and health risks and risk behaviors (psychological distress; suicide ideation or self-harm; binge drinking; smoking; drug use; STIs; early pregnancy). Chi-square tests examined differences by sex.
Results:
An estimated 77 % of 18–24 year olds in Honduras experienced at least 1 ACE and 39 % experienced 3+ ACEs. Women experienced significantly more sexual, emotional, and physical violence compared to men. Compared to youth with no ACEs, those with 1–2 ACEs and 3+ ACEs had 1.8 and 2.8 increased odds for psychological distress, 2.3 and 6.4 increased odds for suicidal ideation and self-harm, and 1.7 and 1.9 increased odds for smoking, respectively, adjusting for age, education, and food insecurity. Physical violence victimization and witnessing violence in the community were associated with increased odds of all health risks and risk behaviors.
Conclusions:
The high prevalence of ACEs and associated negative health risks and risk behaviors in this population support the need for prevention and early intervention for ACEs.
Keywords: Adverse Childhood Experiences, Violence prevention, Violence against children, Child abuse, Health risks
1. Introduction
Adverse Childhood Experiences (ACEs) are potentially traumatic events that occur in childhood. ACEs are of great public health concern globally. Violence against children, one type of ACE, is currently a target of the United Nation’s 2030 Agenda for Sustainable Development (United Nations General Assembly, 2015). Globally, over half of all children experience physical, sexual, and/or emotional violence each year (Hillis, Mercy, Amobi, & Kress, 2016). A systematic review of the global prevalence of violence against children calculated that in Latin America, at least 33 % of 15–17 year olds experienced violence in the past year (Hillis et al., 2016). Few studies have attempted to estimate the prevalence of ACEs globally (Hughes et al., 2017). Most ACE studies to date have been in high-income countries, with estimates suggesting about 61 % of adults in the United States have experienced at least one ACE and 16 % have experienced four or more before age 18 (Merrick et al., 2019). Limited ACEs data exists from low- and middle-income countries (LMICs).
Although some data exist on the prevalence of violence in Central America, no nationally representative studies have been published on the prevalence of ACEs or violence in this region or in specific countries in the region. Studies in Honduras suggest youth ages 15–24 years are at elevated risk for fatal and non-fatal injuries due to violence (Yacoub, Sergio, & Padgett-Moncada, 2006). Violence against women is also prevalent in Honduras with almost one in four women (22 %) reporting lifetime physical and/or sexual intimate partner violence (Secretaría de Salud [Honduras], Instituto Nacional de Estadística (INE) e ICF International, 2013). This high prevalence of violence against women puts children at an increased risk of witnessing or being exposed to intimate partner violence both in the home and in the community. Violence in Honduras is part of a complex, recurring cycle with prevalent gang activity, drug trafficking, and challenges in the law enforcement and criminal justice systems (Landa-Blanco, Cheon, Flores, Spohn, & Katz, 2020; Ransford, Decker, Cruz, Sanchez, & Slutkin, 2017). High levels of poverty, food insecurity, and a lack of access to basic services in Honduras are associated with crime and violence, often out of necessity in order to meet basic needs (The World Bank in Honduras, 2019).
Substantial evidence documents the relationship between ACEs and negative health outcomes into adulthood (Felitti et al., 2019; Kalmakis & Chandler, 2015; Petruccelli, Davis, & Berman, 2019). This evidence suggests a dose-response relationship, so as the number and severity of ACEs increase so does the risk of negative health outcomes, including poor mental health (Bellis et al., 2014), chronic illnesses (Felitti et al., 1998), infectious diseases like HIV (Reisner, Falb, & Mimiaga, 2011), and reproductive health (Ramiro, Madrid, & Brown, 2010). Exposure to more ACEs has also been linked to health-risk behaviors including drug use, alcoholism, intimate partner violence perpetration for men, infrequent condom use, and crime (Broidy & Agnew, 1997; Leban & Gibson, 2020; VanderEnde et al., 2018). Other traumatic childhood experiences, such as the loss of a parent due to parental migration or orphanhood, can result in an increased risk for mental health disorders (depression, anxiety, conduct disorder), suicidal ideation, substance use, and infectious disease (Fellmeth et al., 2018). While it is important to understand the cumulative risk of ACEs, further research needs to be done to understand whether specific adverse experiences represent different levels of risk for specific health consequences (Lanier, Maguire-Jack, Lombardi, Frey, & Rose, 2018).
Sex differences have been observed in both exposure to ACEs (Baglivio et al., 2014; Felitti et al., 1998) and in the outcomes associated with these exposures (Cavanaugh, Petra, & Martins, 2015; Duke, Pettingell, McMorris, & Borowsky, 2010). Generally, females experience more ACEs than their male counterparts (Felitti et al., 1998; Merrick et al., 2019) and different types of ACEs compared to males (Baglivio et al., 2014). Specifically, sexual violence is more prevalent among females (Baglivio et al., 2014) and physical abuse tends to be more prevalent among males (Kilpatrick & Saunders, 1997). There are also sex differences in how boys and girls cope with and react to adverse events. Females are more likely than males to experience depression following a traumatic experience (Piccinelli & Wilkinson, 2000) whereas males are more likely than females to engage in criminal or delinquent behaviors (Broidy & Agnew, 1997). As with most ACEs literature, however, these studies have largely been conducted in high-income western countries. Therefore, it is not possible to know whether these patterns in sex differences are also evident in LMICs.
Honduras has experienced extremely high levels of violence in the last decade. Several factors have driven violence to high levels in this country and the surrounding region. Shifts in the transnational drug trade have fueled organized crime in Honduras (Berg & Carranza, 2018). Economic instability has contributed to the vulnerabilities of Honduran youth and hampered the reduction of gang activities. In addition, violence and economic instability have fueled population movements either through internal displacement or through emigration (Berg & Carranza, 2018; Moser & McIlwaine, 2006). Several studies have documented increased risk for vulnerability and violence in Honduras (Hansen-Nord et al., 2014; Solberg & Peters, 2019; Yacoub, Arellano, & Padgett-Moncada, 2006), but research has largely assessed individual types of violence, and studies have relied on convenience samples so it is not possible to know whether they are nationally representative. Furthermore, studies have focused mostly on adult populations and have not measured violence or other adverse experiences among children. No studies have systematically assessed population-level prevalence of ACEs or documented associations with health risks.
The purpose of this study is to assess the prevalence of and health risks and risk behaviors associated with ACEs in Honduras. This study provides the first-ever national estimates of ACEs in the Central America region and examines associations of ACEs with health risks and risk behaviors among young adults in Honduras. Health risks and risk behaviors assessed included psychological distress, suicide ideation and self-harm, substance abuse, sexually transmitted infections (STIs), and early pregnancy. This study also aims to establish whether a dose-response relationship exists between ACEs and health risks and risk behaviors, and the individual associations between each ACE type and each modeled outcome. In addition, sex differences in prevalence of ACEs were examined.
2. Methods
2.1. Design
The Honduras 2017 Violence Against Children and Youth Survey (VACS) is a nationally representative, cross-sectional, household survey conducted in Honduras between August and September 2017. VACS uses a standardized methodology to measure physical, emotional, and sexual violence in childhood (before age 18). It includes a short questionnaire for an adult in the household to obtain household consent and build rapport with the family and to determine current household socioeconomic conditions. The longer questionnaire is administered to participants 13–24 years old who are eligible and consent to participating. In addition to questions about sexual, physical, and emotional violence, the survey also collects data on health conditions, risk and protective factors for violence, and service utilization. Questionnaire adaptation for the Honduras context was led by technical working groups under the guidance of a steering committee represented by the Gabinete de Prevención and the Children and Youth Prevention Council (COPREV). Data collection was conducted by interviewers who received comprehensive training, interview practice, and training on building rapport and creating a comfortable environment for disclosure (for more details, see Centers for Disease Control & Prevention, 2019). Field implementation for the 2017 Honduras VACS was led by the National Institute of Statistics (INE), in collaboration with the International Office on Migration and funding by the US Agency for International Development (USAID). CDC trained interview teams, conducted quality control of data collection, data cleaning, and statistical weighting of the data and led the main analysis of findings. Detailed information on the methodology and procedures for the 2017 Honduras VACS is available in the full survey report (Government of Honduras, 2019).
2.2. Participant selection
The sample was selected using a multistage, geographically clustered design (see Fig. 1) that included the following steps: 1) randomly selecting geographic areas within the country, 2) randomly selecting a sample of households from a list of all households within each selected area, and 3) randomly selecting one eligible individual from each selected household to participate. For the first stage, enumeration areas (EAs), the smallest geographical unit used for the census, were used as the primary sampling units. A split sample approach was used, in which the survey for females is conducted in different EAs than the survey for males. This approach serves to protect the confidentiality and safety of participants. In the second stage, 21 households within each EA were randomly selected using equal probability systematic sampling. In the third stage, at each selected household interviewers identified the head of the household to introduce the study and determine eligibility of household members for study participation. Females and males ages 13–24 years who lived in a sampled household were eligible to participate. Individuals were excluded if they were in the military, institutionalized (i.e. in hospitals, prisons, nursing homes), or had a severe mental or physical disability that would preclude participation in the one-on-one interview. One eligible resident (female or male, depending on the selected EA) was randomly selected from each household to participate in the interview. Interviews were completed face-to-face in the participant’s native language and participant responses were recorded electronically on netbooks by interviewers. The interviewers conducted the interview in a safe and private space, such as outside, or in an appropriate place in the home or yard, to ensure confidentiality. Additional information about interviewer training and other procedures to increase disclosure and ensure participant safety and confidentiality are described in Centers for Disease Control and Prevention (2017).
Fig. 1.
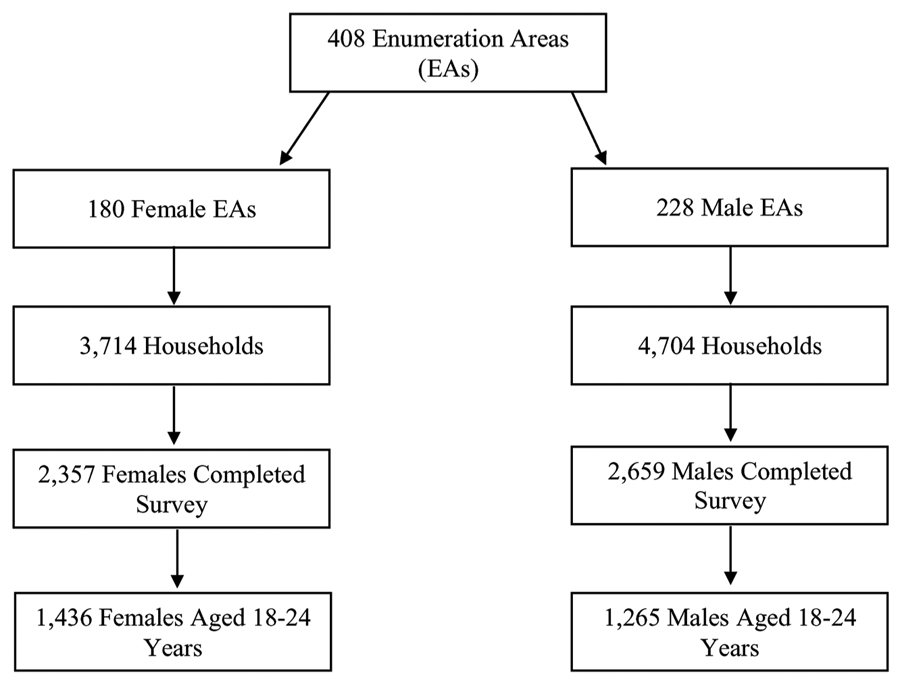
Three-Stage Stratified Random Sampling Method.
In the male sample, 4704 households were surveyed in 228 randomly selected EAs, including 2659 completed individual interviews. The household response rate was 89.5 % and the individual response rate was 83.4 %, resulting in an overall response rate of 74.6 % for males. In the female sample, 3714 households were surveyed in 180 EAs, resulting in 2357 completed individual interviews. The household response rate was 93.7 % for females, the individual response rate was 89.4 %; the overall response rate was 83.8 % for females. In order to assess ACEs before age 18 in the present study, data are restricted to only participants ages 18–24 years old, resulting in a final analytic sample size of 1265 males and 1436 females.
2.3. Ethical procedures
The Honduras VACS was reviewed and approved by the CDC’s Institutional Review Board and the Ethics Committee on Biomedical Research of the Universidad Nacional Autónoma de Honduras. The VACS protocol is consistent with the WHO ethical recommendations for research on violence against women (World Health Organization, 2016). Field staff followed protocol and offered direct referrals for counseling to participants who requested them. Additional information about ethics and privacy protections is available in separate publications (Centers for Disease Control & Prevention, 2017; Government of Honduras, 2019). IRB approval was waived for this secondary data analysis.
2.4. Measures
The Honduras VACS used the standardized VACS questionnaire, which has been used to measure violence, risk and protective factors, and health risks in similar settings across multiple surveys (Nguyen, Kress, Villaveces, & Massetti, 2019). Measures in VACS were selected from a range of well-established and respected survey tools with demonstrated validity and reliability, and the Honduras version was pilot-tested to ensure appropriateness to the local context in Latin America.
2.4.1. Demographic characteristics and covariates
Demographic characteristics included current age, completed level of schooling, and food insecurity. Current age was measured based on the participant’s age at the time of the interview. Participants were asked to report the highest level of schooling they completed, and the variable was dichotomized to categorize those who had less than a secondary school education and those who completed secondary school or higher. Food insecurity was evaluated based on a yes or no response to the question, “Do you think your household has enough money for food?” Level of schooling and food insecurity were chosen as covariates for the analyses as a proxy for socio-economic status, which has been associated with both exposure to ACEs and lifetime health outcomes (Nurius, Green, Logan-Greene, Longhi, & Song, 2016).
2.4.2. Adverse Childhood Experiences
ACEs assessed include the following experiences before age 18: 1) sexual violence, 2) physical violence, 3) emotional violence, 4) witnessed physical violence in the home, 5) witnessed physical violence in the community, 6) orphan status, and 7) parental migration. Items measuring ACEs in VACS were selected from the ISPCAN Child Abuse Screening Tool-Retrospective (ICAST-R; for parent physical violence, and emotional violence; Dunne et al., 2009) and the Juvenile Victimization Questionnaire (JVQ; for peer, intimate partner, and adult physical violence, sexual violence, witnessing physical violence in the home, and witnessing physical violence in the community; Finkelhor, Hamby, Ormrod, & Turner, 2005). Published studies have demonstrated the psychometric properties, reliability, and validity of both the ICAST-R (Dunne et al., 2009; Zolotor et al., 2009) and the JVQ (Finkelhor et al., 2005; Pereda, Gallardo-Pujol, & Guilera, 2018). Questions about parental migration were constructed for this survey. Sexual violence included experiences of unwanted sexual touching, attempted sex, physically forced sex, or any pressured or coerced sex. Physical violence included having been slapped, pushed, shoved, shook, intentionally thrown at, punched, kicked, whipped, beaten with an object, choked, smothered, intentionally burned, attempted drowning, attacked or threatened with a knife, and attacked or threatened with a gun. These questions were asked about experiences of physical violence perpetrated by intimate partners, peers, parents, or other adults in the community. Emotional violence was measured by asking participants if a parent, adult caregiver, or other adult relative ever told them that they were not loved, wished they had never been born, or ever ridiculed or put them down. Witnessing physical violence in the home included seeing or hearing one’s mother or step-mother being punched, kicked, or beaten up by one’s father or step-father and/or seeing or hearing a parent punch, kick, or beat up one’s brothers or sisters. Witnessing physical violence in the community included seeing anyone get attacked outside of the home and family environment. Orphan status was defined as the death of one or both parents prior to age 18 years. For parental migration, participants were asked “has your biological mother ever lived away from you for 6 months or more before you were 18 years old?”, and the same question about his or her biological father. Participants were considered to have experienced parental migration if one or both parents lived away from them for 6 months or more before age 18. A summative ACEs score was also created to categorize the ACEs count as none, one or two, or three or more. These ACEs count categorical cutoffs were chosen based on existing cumulative ACEs research (Dube et al., 2009; VanderEnde et al., 2018).
2.4.3. Health risks and risk behaviors
Health risks and risk behaviors included: psychological distress, suicide ideation and self-harm, binge drinking, smoking, drug use, sexually transmitted infections (STIs), and early pregnancy. Psychological distress was assessed using the Kessler Screening Scale for Psychological Distress (K6) and includes six questions about feeling nervous, hopeless, restless, sad, and worthless in the past 30 days (Kessler et al., 2002). The K6 is sum scored and then categorized into low (K6 < 5), moderate (5 ≤ K6 < 13), and severe mental health risk categories (K6> = 13; Kessler et al., 2008). The Kessler scale has demonstrated good internal consistency and reliability (Cronbach α = 0.83; Kessler et al., 2002). If a participant’s K6 score indicated moderate or severe distress, they were coded as having experienced psychological distress in the past 30 days. The suicide ideation and self-harm variable was coded by combining responses from two separate items: “have you ever thought about killing yourself?” and “have you ever intentionally hurt yourself?” A dichotomous suicide ideation/self-harm variable was coded to capture individuals who reported yes to one or both of the suicide/self-harm-related questions. Three behaviors were included that assessed substance misuse: binge drinking, smoking, and drug use. For binge drinking, females were asked, “in the past 30 days, on how many days did you have 4 or more drinks of alcohol in a row?” and males were asked, “in the past 30 days, on how many days did you have 5 or more drinks of alcohol in a row?” This binge drinking question was only asked of individuals who said yes to ever having a drink of alcohol that was more than a few sips. This variable was then recoded into a binary variable in which any response of one day or more of binge drinking in the past month was considered binge drinking. Participants were asked if they currently smoke tobacco on a daily basis, less than daily, or not at all. Responses of “daily basis” or “less than daily” were recoded as affirmative for smoking in the past 30 days. For drug use, participants were asked if they used drugs such as marijuana, pills, ecstasy, or sniffed any chemical such as petrol or glue in the last 30 days, with yes or no response options. STIs were measured by asking participants if they had ever been diagnosed with a sexually transmitted infection or had a genital sore, ulcer, or abnormal genital discharge. Lastly, if female participants reported they had ever been pregnant, then a follow up question asked, “how old were you the first time that you got pregnant?” Early pregnancy was coded as any pregnancy before age 18 years.
Psychometric properties for suicide measures, substance use measures, STI, and early pregnancy were not available. The VACS questionnaire asks discrete questions for each health outcome and did not ask additional questions to establish a measure of internal consistency (i.e., reliability). Nonetheless, the instrument asked questions that were incorporated from well-established tools for health risk and health behavior ascertainment among youth, including the Youth Risk Behavior Surveillance System (YRBSS; https://www.cdc.gov/healthyyouth/data/yrbs/index.htm), the Global School-Based Student Health Survey (GSHS; https://www.who.int/ncds/surveillance/gshs/en/), and the Demographic and Health Surveys (DHS; https://dhsprogram.com/).
2.5. Data analysis
The study included only participants who were ages 18–24 years and completed the interview in order to estimate the weighted prevalence of demographic characteristics, ACEs, and health risks and risk behaviors among 18–24-year-olds in Honduras. Means, frequencies, weighted percentages, and 95 % confidence intervals were calculated for all variables of interest, including demographic characteristics, individual ACEs, ACEs count, and health risks and risk behaviors. Both prevalence overall and estimates stratified by sex were reported. Chi-square tests were used to examine if observed differences by sex were statistically significant. Additionally, we estimated weighted prevalence and 95 % confidence intervals of the co-occurrence of individual health risks and risk behaviors by ACEs count. A three-step weighting procedure was used to obtain parameters from the data set resulting from sampling in order to represent the total population. These steps included 1) computation of base weight for each sample participant, 2) adjustment of the base weights for differential non-response, and 3) post-stratification calibration adjustment of weights to known population totals. The final weights assigned to each responding unit were computed as the product of the base weights, the non-response adjustment factors, and post-stratification calibration adjustment factors. The Taylor Series Method (Taylor Linearization) variance estimation technique accounted for the complex survey design. Detailed technical information about the development of survey weights is available in the Honduras VACS final report (Government of Honduras, 2019) and in Nguyen et al. (2019).
Logistic regression models were used to estimate the relationship between ACEs and each health outcome. While differential effects by gender were of substantive interest, we were not well powered to estimate them with these data. Therefore, the overall relationships, for both males and females, between the ACEs count and each health outcome were estimated. Additionally, to assess whether specific ACEs were associated with specific risks and risk behaviors, a series of models were run to look at the relationship between each individual ACE and each outcome. For all sets of models, both crude and adjusted models were estimated comparing each ACE relative to the absence of that ACE (for example, sexual violence compared to no sexual violence) to each outcome (psychological distress, suicide ideation or self-harm, binge drinking, smoking, drug use, STIs, and early pregnancy). The adjusted models included age, food insecurity, and schooling as covariates. All prevalence estimates and models were estimated using the SURVEYLOGISTIC procedure in SAS version 9.4 to account for the complex survey design of VACS.
3. Results
3.1. Population characteristics
Table 1 includes population characteristics overall and by sex, 95 % Confidence Intervals (CIs) and p-values of chi square tests comparing males and females. The mean age was 20.7 years old. Fifty-two percent (52.6 %) of 18–24-year-olds completed secondary school or higher. Thirty-four percent (34.3 %) of the population experienced food insecurity. There were no statistically significant differences between males and females on education completion (females, 53.6 %; males, 51.5 %; p = 0.56) or food insecurity (females, 33.8 %; males, 34.9 %; p = 0.66).
Table 1.
Background Characteristics and Prevalence of Adverse Childhood Experiences (ACEs) and Health Risks and Risk Behaviors Among Males and Females aged 18 to 24 years, Honduras, 2017.
| Combined (n = 2701) |
Males (n = 1265) |
Females (n = 1436) |
Chi-square p value |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | Weighted % |
(95 % CI) |
n | Weighted % |
(95 % CI) |
n | Weighted % |
(95 % CI) |
||
| Demographic Characteristics | ||||||||||
| Mean age in years | 2701 | 20.7 | (20.7, 20.8) | 1265 | 20.7 | (20.5, 20.8) | 1436 | 20.8 | (20.7, 20.9) | |
| Completed secondary school or higher | 1428 | 52.6 | (49.2, 56.0) | 660 | 51.5 | (46.4, 56.6) | 768 | 53.6 | (48.8, 58.4) | 0.5645 |
| Experienced food insecurity | 870 | 34.3 | (31.7, 36.9) | 415 | 34.9 | (31.2, 38.7) | 455 | 33.8 | (30.2, 37.4) | 0.6630 |
| Adverse Childhood Experiences (ACEs) | ||||||||||
| Childhood sexual violence | 373 | 13.3 | (11.9, 14.8) | 135 | 9.9 | (8.2, 11.6) | 238 | 16.2 | (14.0, 18.5) | <0.0001* |
| Childhood physical violence | 845 | 30.8 | (28.4, 33.2) | 382 | 29.5 | (26.1, 32.9) | 463 | 31.9 | (28.4, 35.3) | 0.3459 |
| Childhood emotional violence | 311 | 11.5 | (10.0, 12.9) | 98 | 7.7 | (6.1, 9.3) | 213 | 14.7 | (12.5, 17.0) | <0.0001* |
| Witnessed physical violence in the home | 548 | 19.7 | (17.9, 21.5) | 201 | 15.8 | (13.5, 18.1) | 347 | 23.0 | (20.5, 25.5) | <0.0001* |
| Witnessed physical violence in the community | 993 | 35.4 | (33.0, 37.9) | 501 | 37.6 | (33.8, 41.4) | 492 | 33.6 | (30.2, 37.0) | 0.1302 |
| Orphaned (one or both parents died) | 329 | 12.0 | (10.4, 13.5) | 147 | 11.3 | (9.2, 13.3) | 182 | 12.5 | (10.3, 14.8) | 0.4183 |
| Migration by one or both parents (for 6 months or more) | 963 | 42.1 | (39.2, 45.0) | 433 | 39.0 | (35.0, 43.0) | 530 | 44.8 | (40.7, 48.9) | 0.0446* |
| ACE Exposures | 0.0012* | |||||||||
| None | 585 | 22.9 | (20.6, 25.2) | 309 | 26.1 | (22.6, 29.6) | 276 | 20.2 | (17.1, 23.3) | |
| One or two | 1041 | 38.0 | (35.8, 40.2) | 507 | 39.5 | (36.3, 42.6) | 534 | 36.7 | (33.6, 39.7) | |
| Three or more | 1075 | 39.1 | (36.6, 41.6) | 449 | 34.4 | (30.9, 37.9) | 626 | 43.1 | (39.6, 46.6) | |
| Health Risks and Risk Behaviors | ||||||||||
| Psychological distress in the past 30 days | 1396 | 52.3 | (49.9, 54.6) | 575 | 47.1 | (43.5, 50.7) | 821 | 56.6 | (53.6, 59.6) | <0.0001* |
| Suicide ideation or self-harm (ever) | 418 | 15.6 | (14.0, 17.2) | 144 | 11.3 | (9.3, 13.4) | 274 | 19.3 | (17.0, 21.5) | <0.0001* |
| Binge drinking in the past 30 days | 393 | 28.9 | (25.7, 32.1) | 282 | 35.8 | (31.8, 39.9) | 111 | 19.4 | (15.1, 23.7) | <0.0001* |
| Current smoking | 368 | 13.5 | (11.4, 15.5) | 300 | 23.8 | (20.6, 26.9) | 68 | 4.8 | (3.3, 6.2) | <0.0001* |
| Drug use in the past 30 days | 76 | 2.9 | (2.1, 3.7) | 59 | 4.6 | (3.2, 6.0) | 17 | 1.5 | (0.7, 2.3) | 0.0001* |
| STI | 127 | 4.5 | (3.6, 5.4) | 20 | 1.4 | (0.8, 2.0) | 107 | 7.1 | (5.6, 8.6) | <0.0001* |
| Early pregnancy (before age 18) | 370 | 34.0 | (30.7, 37.2) | |||||||
Note. STI = Sexually Transmitted Infection.
Indicates p < 0.05 for the chi-square p value comparing males and females.
Thirty percent (30.8 %) of the population experienced physical violence in childhood, 35.4 % witnessed community violence in childhood, and 19.7 % witnessing violence in the home in childhood. Additionally, 13.3 % experienced childhood sexual violence and 11.5 % experienced childhood emotional violence. Forty-two percent (42.1 %) of young men and women experienced parental migration in childhood and 12.0 % experienced orphanhood. Significantly more females than males experienced sexual violence (females, 16.2 %; males, 9.9 %; p < 0.001), emotional violence (females, 14.7 %; males, 7.7 %; p < 0.001), and witnessing physical violence in the home (females, 23.0 %; males, 15.8 %; p < 0.001) in childhood. There were no statistically significant differences between males and females on childhood physical violence, witnessing violence in the community, or orphanhood (Table 1). Significantly more females (44.8 %) than males (39.0 %; p < 0.05) experienced parental migration in childhood. Overall, 77.1 % of 18–24-year-olds in Honduras experienced at least one ACE, with 38.0 % experiencing one or two ACEs, and 39.1 % experiencing three or more ACEs. The difference between males and females in ACE scores was statistically significant, with more females in the 3 or more ACE group (none, 20.2 %; 1–2, 36.7 %; 3+, 43.1 %) compared to males (none, 26.1 %; 1–2, 39.5 %; 3 or more, 34.4 %; p < 0.01).
Fifty-two percent (52.3 %) of youth experienced psychological distress in the past 30 days, 15.6 % ever experienced suicide ideation or self-harm, 28.9 % binge drank in the past 30 days, 13.5 % smoked, 2.9 % used illicit drugs in the past 30 days, and 4.5 % had ever had an STI. Females were significantly more likely than males to have psychological distress (p < 0.001), suicide ideation or self-harm (p < 0.001), and STIs (p < 0.001; estimates in Table 1). Males were significantly more likely than females to binge drink (p < 0.001), smoke (p < 0.001), and use illicit drugs (p < 0.001; estimates in Table 1). An estimated 34.0 % of females got pregnant before age 18 years.
3.2. Cumulative ACEs and health risks and risk behaviors
Table 2 includes results of logistic regression models assessing the relationship between ACEs exposures (none, 1–2, 3+) and health risks and risk behaviors among young adults. These results suggest a dose-response relationship between ACEs and health risks and risk behaviors. The odds ratios (ORs) increased in a dose-response fashion from 1.8 (95 % CI, 1.4–2.3) to 2.8 (95 % CI, 2.1–3.7) for psychological distress, 2.2 (95 % CI, 1.3–3.5) to 6.3 (95 % CI, 3.9–10.0) for suicidal ideation or self-harm, 1.4 (95 % CI, 0.9–2.2) to 1.5 (95 % CI, 1.0–2.3) for binge drinking, 1.6 (95 % CI, 1.1–2.4) to 1.7 (95 % CI, 1.2–2.6) for smoking, 1.9 (95 % CI, 0.6–2.6) to 3.7 (95 % CI, 1.3–10.6) for drug use, and 1.3 (95 % CI, 0.6–2.6) to 3.5 (95 % CI, 1.9–6.5) for STIs for 1–2 ACEs and 3+ ACEs, respectively, compared with those reporting no ACEs. Prevalence of each health outcome for different ACE category groups, 95 % CIs for the ORs and adjusted ORs (aORs), andp-values are provided in Table 2. In the adjusted models controlling for age, food insecurity, and level of schooling completed, we found significantly increased odds for psychological distress (aORs: 1.8 [1.4–2.3], 2.8 [2.1–3.7]), suicidal ideation and self-harm (aORs: 2.3 [1.4–3.7], 6.4 [4.1–10.2]), and smoking (aORs: 1.7 [1.2–2.5], 1.9 [1.3–2.9]) for 1–2 ACEs and 3+ ACEs compared to no ACEs. The aORs were significantly higher for 3+ ACEs compared to no ACEs for binge drinking (aOR: 1.6 [1.0–2.5]), drug use (aOR: 4.0 [1.4–11.9]), STIs (aOR: 3.9 [2.1–7.5]), and early pregnancy (aOR: 1.7 [1.1–2.5]). For these health risks and risk behaviors, the odds for 1–2 ACEs compared with no ACEs were not significantly higher.
Table 2.
Exposure to Adverse Childhood Experiences (ACEs) and Health Risks and Risk Behaviors Among 18-24 year olds, Honduras, 2017.
| Unadjusted Models |
Adjusted Modelsa |
|||||
|---|---|---|---|---|---|---|
| Health Risks and Risk Behaviors | Weighted % (95 % CI) | OR (95 % CI) | p-value | aOR (95 % CI) | p-value | |
| Psychological distress in the past 30 days | No ACEs (n = 585) | 37.0 (31.9, 42.1) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 51.3 (47.8, 54.8) | 1.8* (1.4, 2.3) | <0.0001 | 1.8* (1.4, 2.3) | <0.0001 | |
| 3+ ACEs (n = 1075) | 62.1 (58.8, 65.5) | 2.8* (2.1, 3.7) | <0.0001 | 2.8* (2.1, 3.7) | <0.0001 | |
| Suicide ideation or self-harm | No ACEs (n = 585) | 5.4 (3.1, 7.6) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 10.9 (8.8, 13.1) | 2.2* (1.3, 3.5) | 0.0021 | 2.3* (1.4, 3.7) | 0.0009 | |
| 3+ ACEs (n = 1075) | 26.2 (23.1, 29.3) | 6.3* (3.9, 10.0) | <0.0001 | 6.4* (4.1, 10.2) | <0.0001 | |
| Binge drinking in the past 30 days | No ACEs (n = 585) | 22.7 (15.8, 29.6) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 29.2 (24.4, 34.0) | 1.4 (0.9, 2.2) | 0.1342 | 1.5 (0.9, 2.3) | 0.0928 | |
| 3+ ACEs (n = 1075) | 30.6 (26.2, 35.0) | 1.5 (1.0, 2.3) | 0.0585 | 1.6* (1.0, 2.5) | 0.0303 | |
| Current smoking | No ACEs (n = 585) | 9.3 (6.1, 12.6) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 14.2 (11.5, 16.9) | 1.6* (1.1, 2.4) | 0.0190 | 1.7* (1.2, 2.5) | 0.0067 | |
| 3+ ACEs (n = 1075) | 15.2 (12.3, 18.2) | 1.7* (1.2, 2.6) | 0.0067 | 1.9* (1.3, 2.9) | 0.0014 | |
| Drug use in the past 30 days | No ACEs (n = 585) | 1.2 (0.6, 2.4) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 2.3 (1.2, 3.5) | 1.9 (0.6, 2.6) | 0.2452 | 2.2 (0.7, 6.8) | 0.1895 | |
| 3+ ACEs (n = 1075) | 4.5 (2.9, 6.0) | 3.7* (1.3, 10.6) | 0.0131 | 4.0* (1.4, 11.9) | 0.0113 | |
| STI | No ACEs (n = 585) | 2.2 (1.0, 3.5) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 2.8 (1.7, 3.9) | 1.3 (0.6, 2.6) | 0.5416 | 1.4 (0.7, 3.0) | 0.3213 | |
| 3+ ACEs (n = 1075) | 7.4 (5.6, 9.3) | 3.5* (1.9, 6.5) | <0.0001 | 3.9* (2.1, 7.5) | <0.0001 | |
| Early pregnancy (before age 18 years) | No ACEs (n = 585) | 34.7 (26.4, 43.0) | REF | REF | ||
| 1–2 ACEs (n = 1041) | 30.8 (26.0, 35.6) | 1.1 (0.7, 1.7) | 0.6599 | 1.3 (0.8, 2.1) | 0.2850 | |
| 3+ ACEs (n = 1075) | 36.0 (31.3, 40.7) | 1.5 (1.0, 2.2) | 0.0590 | 1.7* (1.1, 2.5) | 0.0146 | |
Note. OR = odds ratio; aOR = adjusted odds ratio; CI = confidence interval; STI = Sexually Transmitted Infection.
Indicates p < 0.05 for the p value comparing 1–2 ACEs to No ACEs and 3+ ACEs to No ACEs.
Adjusted model includes age, food insecurity, and educational attainment.
3.3. Individual ACEs and health risks and risk behaviors
We assessed the relationship between each ACE and health outcome through separate multiple logistic regressions for each ACE and health outcome individually. Results, including aORs, 95 % CIs, and p-values, are presented in Table 3. In the adjusted models, sexual violence was significantly associated with higher odds for psychological distress (aOR = 2.8 [2.1–3.7]), suicide ideation or self-harm (aOR = 4.9 [3.6–6.5]), drug use (aOR = 2.3 [1.1–4.6]), and STIs (aOR = 4.7 [3.1–7.1]), but not binge drinking (aOR = 1.2 [0.8–1.7]), smoking (aOR = 1.4 [1.0–2.0]), or early pregnancy (aOR = 1.2 [0.8–1.9]). Physical violence was associated with higher odds of all of the health risks and risk behaviors, with aORs ranging from 1.4 (1.1–1.9) for binge drinking and current smoking to 4.2 (2.3–7.7) for drug use (all aORs, 95 % CIs, and p-values in Table 3). Emotional violence was significantly associated with psychological distress (aOR = 3.7 [2.8–4.9]), suicide ideation or self-harm (aOR = 4.9 [3.7–6.6]), drug use (aOR = 2.2 [1.2–4.2]), and STIs (aOR = 3.2 [1.9–5.3]), but not binge drinking (aOR = 1.3 [0.9–2.0]), smoking (aOR = 1.2 [0.8–1.8]), or early pregnancy (aOR = 1.2 [0.8–2.1]).
Table 3.
Exposure to Individual ACEs and Health Risks and Risk Behaviors Among 18-24-year-olds, Honduras, 2017.
| Psychological distress |
Suicide ideation or self- harm |
Binge drinking (past 30 days |
Current smoking |
Drug use (past 30 days) |
STI | Early Pregnancy (before 18) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ACE | aOR (95 % CI) |
p | aOR (95 % CI) |
p | aOR (95 % CI) |
p | aOR (95 % CI) |
p | aOR (95 % CI) |
p | aOR (95 % CI) |
p | aOR (95 % CI) |
p |
| Sexual violence | 2.8* (2.1, 3.7) |
<0.001 | 4.9* (3.6, 6.5) |
<0.001 | 1.2 (0.8, 1.7) |
0.3639 | 1.4 (1.0, 2.0) |
0.0518 | 2.3* (1.1, 4.6) |
0.0245 | 4.7* (3.1, 7.1) |
<0.001 | 1.2 (0.8, 1.9) |
0.4342 |
| Physical violence | 2.1* (1.7, 2.5) |
<0.001 | 3.2* (2.5, 4.3) |
<0.001 | 1.4* (1.1, 1.9) |
0.0064 | 1.4* (1.1, 1.9) |
0.0091 | 4.2* (2.3, 7.7) |
<0.001 | 2.4* (1.6, 3.6) |
<0.001 | 1.5* (1.1, 2.1) |
0.0230 |
| Emotional violence | 3.7* (2.8, 4.9) |
<0.001 | 4.9* (3.7, 6.6) |
<0.001 | 1.3 (0.9, 2.0) |
0.1955 | 1.2 (0.8, 1.8) |
0.4635 | 2.2* (1.2, 4.2) |
0.0170 | 3.2* (1.9, 5.3) |
<0.001 | 1.2 (0.8, 2.1) |
0.3937 |
| Witness violence at home | 1.7* (1.3, 2.1) |
<0.001 | 2.5* (2.0, 3.3) |
<0.001 | 1.4* (1.0, 2.0) |
0.0456 | 1.0 (0.7, 1.4) |
0.9245 | 2.1* (1.1, 4.0) |
0.0195 | 2.1* (1.4, 3.3) |
0.0008 | 0.7 (0.5, 1.0) |
0.0664 |
| Witness violence in community | 2.0* (1.7, 2.5) |
<0.001 | 2.3* (1.8, 2.9) |
<0.001 | 1.4* (1.1, 1.8) |
0.0142 | 1.9* (1.4, 2.5) |
<0.001 | 2.5* (1.4, 4.5) |
0.0031 | 1.7* (1.1, 2.6) |
0.0193 | 1.7* (1.2, 2.4) |
0.0027 |
| Orphaned by one or both parents | 1.2 (0.9, 1.5) |
0.2031 | 1.4* (1.0, 2.0) |
0.0661 | 1.1 (0.7, 1.7) |
0.5644 | 1.3 (0.9, 2.0) |
0.1297 | 2.1* (1.0, 4.3) |
0.0379 | 1.6 (0.8, 3.0) |
0.1696 | 1.3 (0.9, 1.9) |
0.2424 |
| Migration by one or both parents | 1.3* (1.1, 1.6) |
0.0032 | 1.6* (1.2, 2.1) |
0.0005 | 1.0 (0.8, 1.4) |
0.8209 | 1.2 (0.9, 1.7) |
0.1478 | 1.4 (0.8, 2.7) |
0.2743 | 1.8* (1.2, 2.8) |
0.0097 | 1.0 (0.7, 1.3) |
0.9097 |
Note. ACE = Adverse Childhood Experience; aOR = adjusted odds ratio; CI = confidence interval; STI = Sexually Transmitted Infection.
Adjusted model includes age, food insecurity, and educational attainment.
Indicates p < 0.05 for the p-value.
Witnessing violence in the home was significantly associated with higher odds of psychological distress (aOR = 1.7 [1.3–2.1]), suicide ideation or self-harm (aOR = 2.5 [2.0–3.3]), binge drinking (aOR = 1.4 [1.0–2.0]), drug use (aOR = 2.1 [1.1–4.0]), and STIs (aOR = 2.1 [1.4–3.3]), but not smoking (aOR = 1.0 [0.7–1.4]) or early pregnancy (aOR = 0.7 [0.5–1.0]). Witnessing violence in the community was significantly associated with higher odds of all health risks and risk behaviors, with aORs ranging from 1.4 (1.1–1.8) for binge drinking to 2.5 (1.4–4.5) for drug use.
Being orphaned by one or both parents was associated with higher odds of drug use (aOR = 2.1 [1.0–4.3]), but not the other outcomes in the models (aORs, 95 % CIs, and p-values in Table 2). Parental migration was associated with higher odds of psychological distress (aOR = 1.3 [1.1–1.6]), suicide behavior or self-harm (aOR = 1.6 [1.2–2.1]), and STIs (aOR = 1.8 [1.2–2.8]), and not the other health outcomes in the models (Table 3 includes aORs, 95 % CIs, and p-values).
4. Discussion
The literature on ACEs has established associations with numerous negative mental and physical health outcomes in adulthood. However, little is known about the frequency and consequences of ACEs in LMICs, with particular data gaps in Central America, including Honduras. Therefore, this study presents the first-ever national estimate of ACEs and their impacts in Honduras by examining the prevalence of ACEs, including violence victimization, witnessing violence, and parent-child separation, and potential health consequences among young adults.
Findings from this study indicate that ACEs, including violence, witnessing violence, and separation from a parent, are common among young men and women in Honduras. An estimated 77 % of 18–24-year-olds experienced at least one ACE before age 18 years. Over one third of young adults in Honduras experienced multiple forms of childhood adversity, with 43 % of females and 34 % of males experiencing three or more ACEs. These prevalence estimates are high compared to ACEs estimates in the United States which suggest about 61 % of adults in the United States experienced at least one ACE before age 18 years (Merrick et al., 2019). These estimates are more similar to findings from the Philippines, where about 75 % reported at least one ACE exposure (Ramiro et al., 2010).
Consistent with other ACEs studies (VanderEnde et al., 2016; Bellis et al., 2014), experiencing and witnessing physical violence are common forms of childhood adversity in Honduras, with 30.8 % of the population experiencing physical violence, 35.4 % witnessing physical violence in the community, and 19.7 % witnessing physical violence in the home. Health risks and risk behaviors are also common among young adults in Honduras. Results indicate moderately high prevalence of psychological distress, binge drinking, suicide ideation or self-harm, and smoking among young adults. These findings suggest a significant prevalence of mental health problems and risk behaviors in this population, regardless of ACE score. Such levels indicate a need for preventive interventions to promote mental and behavioral health to avoid future serious health problems.
There were also significant sex differences in the prevalence of health risks and risk behaviors, with mental health problems more common among females and substance misuse more common among males. These results suggest a need to tailor interventions for different populations of young adults. Preventive interventions to reduce smoking and address alcohol and drug misuse may be particularly relevant for young men in Honduras. For young women, strategies that support mental health and promote resilience are needed.
Sex differences are also evident in the prevalence of specific ACEs, with young women experiencing significantly more sexual violence, emotional violence, and witnessing physical violence in the home in childhood compared to young men. These differences in violence prevalence by sex are consistent with other ACEs and VACS studies where women generally report more victimization than men (Baglivio et al., 2014; Felitti et al., 1998). Interestingly, in contrast with studies that suggest that males experience more physical violence than females (Kilpatrick & Saunders, 1997; Stark et al., 2019), females and males experienced comparable rates of childhood physical violence in Honduras. These findings suggest unique patterns of childhood physical violence by sex in Honduras compared to other countries and contexts.
Consistent with growing evidence that supports the cumulative effects of ACEs (Felitti et al., 2019; Kalmakis & Chandler, 2015; Petruccelli et al., 2019), a dose-response relationship exists between the count of ACEs and health risks and risk behaviors in Honduras. Clear and consistent graded relationships emerged between ACEs and psychological distress, suicide ideation and self-harm, and smoking. Young adults with 3 or more ACEs were also at increased risk for binge drinking, drug use, STIs, and early pregnancy compared with those with no ACEs. These findings are consistent with those from previous research documenting a dose-response relationship between ACEs and health conditions from other countries (Merrick et al., 2019; Vanderende et al., 2016). Indeed, the consistency in patterns emphasizes the need to prevent the accumulation of ACEs to reduce risk for poor health (Centers for Disease Control & Prevention, 2019).
Continued exposure to childhood adversities increases the risk that health consequences will persist into adulthood, negatively impacting future health and life outcomes. These findings support the need for comprehensive interventions that target multiple forms of childhood adversity. Fortunately, there are a number of evidence-based approaches to lessen the immediate and long-term harms of ACE exposures (Centers for Disease Control & Prevention, 2019; World Health Organization, 2016). Timely access to assessment, intervention, effective care, and support for children and families exposed to ACEs can help mitigate health and behavioral consequences (Centers for Disease Control & Prevention, 2019). Early signs of psychological distress, suicide ideation, or health compromising behaviors such as illicit drug use may indicate a need for victim-centered psychological services and enhanced primary care (Centers for Disease Control & Prevention, 2019). Ultimately, primary prevention of ACEs can reduce risk and promote health. Evidence-based programs such as those highlighted in INSPIRE: Seven Strategies to End Violence Against Children (World Health Organization, 2016) highlight comprehensive, multisectoral efforts supported by the best-available evidence. INSPIRE includes evidence-based programs categorized in 7 strategies: Implementation and Enforcement of Laws, Norms and Values, Safe Environments, Parenting and Caregiver Supports, Income and Economic Strengthening, Response and Support Services, and Education and Life Skills. The programs and strategies highlighted in INSPIRE have the added value of having been implemented and/or evaluated in LMICs, making them a potential fit for the Honduran context.
Several programs in INSPIRE may fit the patterns of ACE exposures and health risks and risk behaviors noted here. Promoting social norms that protect against violence and adversity, especially for women and children, could be useful to the prevention of ACEs in Honduras (Centers for Disease Control & Prevention, 2019; Basile et al., 2016; David-Ferdon et al., 2016; Niolon et al., 2017). Given the prevalence of witnessing violence in the home or community in Honduras, such programs can address social norms supportive of violence. Bystander interventions and community-based efforts to mobilize men and boys to establish new positive social norms have been shown to reduce violence against dating partners and sexual violence perpetration (Coker et al., 2017; Miller et al., 2013). Public education campaigns can reframe the way people think and talk about ACEs and can include positive parenting programs around safe and effective discipline (Fortson, Elevens, Merrick, Gilbert, & Alexander, 2016). Legislative approaches to reduce corporal punishment can also help establish norms around safer discipline strategies in the home (Fortson et al., 2016).
The strengths of this study include the rigorous methodology and nationally representative sample, and inclusion of a broad range of questions on both ACEs and health risks and risk behaviors. Several limitations are also noted. Due to the self-report, retrospective data collection methods used in this study, it is possible that the prevalence of ACEs has been underreported. This would lead to underestimating the true strength of the association between exposure to ACEs and health outcomes. Though the ACEs measures in the present study included modules from two instruments with documented validity and reliability data, the migration questions were developed for the present study as no validated scale exists that measures parental migration. More work is needed to define the psychometric properties, validity, and reliability of the migration module. While we demonstrate differences in the burden of ACEs by gender, we are underpowered to estimate substantively meaningful differences in the associations between ACEs and health outcomes by gender. Further research is needed, in this and other settings, to estimate whether ACEs differentially impact adolescents and young adults by gender. The cross-sectional design of the study also limits the ability to establish temporality between associations. Nonetheless, restricting analysis to experiences that occurred prior to 18 years and health risks and risk behaviors in the past 30 days aids in separating the temporality of exposures and some of the outcomes measured. Additionally, because this was a secondary analysis, this study was limited to the use of variables asked about in the VACS questionnaire and therefore only able to examine ACEs that were captured with the instrument. Other ACEs that could be explored in Honduras in future studies include living with someone who is a substance user, mentally ill, or imprisoned, experiencing childhood neglect, and involvement in gang violence (Campbell, Walker, & Egede, 2016).
Since this is the first nationally representative study of ACEs in Honduras, further research to more deeply establish these relationships could provide additional information to the field. These findings can serve as baseline data on the prevalence of ACEs and can provide information to examine the drivers and contexts of ACEs among female and male youth in Honduras. It may also be important to explore the mechanisms driving these ACEs, specifically in Honduras, in order to design targeted, evidence-based interventions and policy strategies. Future analyses may also explore additional risk behaviors that have been shown to be associated with childhood trauma like violence perpetration or re-victimization later in life (Stroem, Aakvaag, & Wentzel-Larsen, 2019; Swedo et al., 2019).
In conclusion, a majority of adolescents and young adults in Honduras have experienced ACEs, and are at elevated risk for poor health. The high prevalence of ACEs and associated health risks and risk behaviors in this population support the need for early intervention and prevention strategies in order to avoid the accumulation of traumatic experiences and protect youth from the harmful impacts of ACEs. This study provides compelling evidence to inform future interventions and prevention efforts to decrease the prevalence of ACEs and ultimately mitigate the resulting burden of disease in Honduras.
Acknowledgments
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
CDC disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Baglivio MT, Epps N, Swartz K, Huq MS, Sheer A, & Hardt NS (2014). The prevalence of adverse childhood experiences (ACE) in the lives of juvenile offenders. Journal of Juvenile Justice, 3, 1–23. [Google Scholar]
- Basile KC, DeGue S, Jones K, Freire K, Dills J, Smith SG, et al. (2016). STOP SV: A technical package to prevent sexual violence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Bellis MA, Hughes K, Leckenby N, Jones L, Baban A, Kachaeva M, et al. (2014). Adverse childhood experiences and associations with health-harming behaviours in young adults: Surveys in eight eastern European countries. Bulletin of the World Health Organization, 92, 641–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg LA, & Carranza M (2018). Organized criminal violence and territorial control: Evidence from northern Honduras. Journal of Peace Research, 55, 566–581. [Google Scholar]
- Broidy L., & Agnew R (1997). Gender and crime: A general strain theory perspective. The Journal of Research in Crime and Delinquency, 34, 275–306. [Google Scholar]
- Campbell JA, Walker RJ, & Egede LE (2016). Associations between adverse childhood experiences, high-risk behaviors, and morbidity in adulthood. American Journal of Preventive Medicine, 50, 344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavanaugh CE, Petra H, & Martins SS (2015). Gender-specific profiles of adverse childhood experiences, past year mental and substance use disorders, and their associations among a national sample of adults in the United States. Social Psychiatry and Psychiatric Epidemiology, 50, 1257–1266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2017). Critical elements of interviewer training for engaging children and adolescents in global violence research: Best practices and lessons learned from the violence against children survey. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Preventing adverse childhood experiences: Leveraging the best available evidence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Coker AL, Bush HM, Cook-Craig PG, DeGue SA, Clear ER, Brancato CJ, et al. (2017). RCT testing bystander effectiveness to reduce violence. American Journal of Preventive Medicine, 52, 566–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David-Ferdon C, Vivolo-Kantor AM, Dahlberg LL, Marshall KJ, Rainford N, & Hall JE (2016). A comprehensive technical package for the prevention of youth violence and associated risk behaviors. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Dube SR, Fairweather D, Pearson WS, Felitti VJ, Anda RF, & Croft JB (2009). Cumulative childhood stress and autoimmune diseases in adults. Psychosomatic Medicine, 71, 243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duke NN, Pettingell SL, McMorris BJ, & Borowsky IW (2010). Adolescent violence perpetration: Associations with multiple types of adverse childhood experiences. Pediatrics, 125, 778–786. [DOI] [PubMed] [Google Scholar]
- Dunne MP, Zolotor AJ, Runyan DK, Andreva-Miller I, Choo WY, Dunne SK, et al. (2009). ISPCAN Child Abuse Screening Tools Retrospective version (ICAST-R): Delphi study and field testing in seven countries. Child Abuse & Neglect, 33, 815–825. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Wiliamson DF, Spitz AM, Edwards V, et al. (2019). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventative Medicine, 56, 774–786. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventative Medicine, 14, 245–258. [DOI] [PubMed] [Google Scholar]
- Fellmeth G, Rose-Clarke K, Zhao C, Busert LK, Zheng Y, Massazza A, et al. (2018). Health impacts of parental migration on left-behind children and adolescents: A systematic review and meta-analysis. Lancet, 392, 2567–2582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelhor D, Hamby SL, Ormrod R, & Turner H (2005). The juvenile victimization questionnaire: Reliability, validity, and national norms. Child Abuse & Neglect, 29, 383–412. [DOI] [PubMed] [Google Scholar]
- Fortson BL, Klevens J, Merrick MT, Gilbert LK, & Alexander SP (2016). Preventing child abuse and neglect: A technical package for policy, norm, and programmatic activities. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Government of Honduras. (2019). Sub-secretariat of security in prevention, secretariat of security. Honduras violence against children survey, 2017. Tegucigalpa, Honduras. [Google Scholar]
- Hansen-Nord NS, Skar M, Kjaerulf F, Almendarez J, Bahr S, Sosa O, et al. (2014). Social capital and violence in poor urban areas of Honduras. Aggression and Violent Behavior, 19, 643–648. [Google Scholar]
- Hillis S, Mercy J, Amobi A, & Kress H (2016). Global prevalence of past-year violence against children: A systematic review and minimum estimates. Pediatrics, 137. e20154079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. (2017). The effect of multiple adverse childhood experiences on health: Systematic review and meta-analysis. The Lancet Public Health, 2, 356–366. [DOI] [PubMed] [Google Scholar]
- Kalmakis KA, & Chandler GE (2015). Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners, 27, 457–465. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-LT, et al. (2002). Short screening scales to monitor population prevalences and trends in nonspecific psychological distress. Psychological Medicine, 32, 959–976. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Heeringa S, Lakoma MD, Petukhova M, Rupp AE, Schoenbaum M, et al. (2008). Individual and societal effects of mental disorders on earning in the United States: results from the national comorbidity survey replication. The American Journal of Psychiatry, 165, 703–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, & Saunders BE (1997). Prevalence and consequences of child victimization: Results from the National Survey of Adolescents: Final report. Washington, DC: US Department of Justice, Office of Justice Programs. [Google Scholar]
- Landa-Blanco M, Cheon H, Flores LGR, Spohn C, & Katz CM (2020). Violence in Honduras from 2008 to 2018. Injury Prevention, 26, 191–193. [DOI] [PubMed] [Google Scholar]
- Lanier P, Maguire-Jack K, Lombardi B, Frey J, & Rose RA (2018). Adverse childhood experiences and child health outcomes: Comparing cumulative risk and latent class approaches. Maternal and Child Health Journal, 22, 288–297. [DOI] [PubMed] [Google Scholar]
- Leban L, & Gibson CL (2020). The role of gender in the relationship between adverse childhood experiences and delinquency and substance use in adolescence. Journal of Criminal Justice, 66, Article 101637. [Google Scholar]
- Merrick MT, Ford DC, Ports KA, Guinn AS, Chen J, Klevens J, et al. (2019). Vital signs: Estimated proportion of adult health problems attributable to adverse childhood experience and implications for prevention – 25 states, 2015-2017. Morbidity and Mortality Weekly Report, 68, 999–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E, Tancredi DJ, McCauley HL, Decker MR, Virata MCD, Anderson HA, et al. (2013). One-year follow-up of a coach-delivered dating violence prevention program: A cluster randomized controlled trial. American Journal of Preventive Medicine, 45, 108–112. [DOI] [PubMed] [Google Scholar]
- Moser CON, & McIlwaine C (2006). Latin American urban violence as a development concern: Towards a framework for violence reduction. World Development, 34, 89–112. [Google Scholar]
- Nguyen KH, Kress H, Villaveces A, & Massetti GM (2019). Sampling design and methodology of the violence against children and youth surveys. Injury Prevention, 25, 321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niolon PH, Kearns M, Dills J, Rambo K, Irving S, Armstead T, et al. (2017). Preventing intimate partner violence across the lifespan: A technical package of programs, policies, and practices. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Nurius PS, Green S, Logan-Greene P, Longhi D, & Song C (2016). Stress pathways to health inequalities: Embedding ACEs within social and behavioral contexts. International Public Health Journal, 8, 241–256. [PMC free article] [PubMed] [Google Scholar]
- Pereda N, Gallardo-Pujol D, & Guilera G (2018). Good practices in the assessment of victimization: The Spanish adaptation of the juvenile victimization questionnaire. Psychology of Violence, 8, 76–86. [Google Scholar]
- Petruccelli K, Davis J, & Berman T (2019). Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse & Neglect, 97, Article 104127. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, & Wilkinson G (2000). Gender differences in depression: Critical review. The British Journal of Psychiatry, 177, 486–492. [DOI] [PubMed] [Google Scholar]
- Ramiro LS, Madrid BJ, & Brown DW (2010). Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse & Neglect, 34, 842–855. [DOI] [PubMed] [Google Scholar]
- Ransford C, Decker RB, Cruz GM, Sanchez F, & Slutkin G (2017). El modelo Cure Violence: Reduccion de la violencia en San Pedro Sula (Honduras). Revista CIDOB d’Avers Internacionals, 116, 179–204. [Google Scholar]
- Reisner SL, Falb KL, & Mimiaga MJ (2011). Early life traumatic stressors and the mediating role of PTSD in incident HIV infection among US men, comparisons by sexual orientation and race/ethnicity: Results from the NESARC, 2004–2005. Journal of Acquired Immune Deficiency Syndromes, 57, 340–350. [DOI] [PubMed] [Google Scholar]
- Secretaría de Salud [Honduras], Instituto Nacional de Estadistica (INE) e ICF International. (2013). Encuesta Nacional de Salud y Demografia 2011-2012. Tegucigalpa, Honduras. [Google Scholar]
- Solberg MA, & Peters RM (2019). Adverse childhood experiences in non-westernized nations: Implications for immigrant and refugee health. Journal of Immigrant and Minority Health, 22, 145–155. [DOI] [PubMed] [Google Scholar]
- Stark L, Seff I, Hoover A, Gordon R, Ligiero D, & Massetti G (2019). Sex and age effects in past-year experiences of violence amongst adolescents in five countries. PLoS One, 14. e0219073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroem IF, Aakvaag HF, & Wentzel-Larsen T (2019). Characteristics of different types of childhood violence and the risk of revictimization. Violence Against Women, 25, 1696–1716. [DOI] [PubMed] [Google Scholar]
- Swedo EA, Sumner SA, Hillis SD, Aluzimbi G, Apondi R, Atuchukwu VO, et al. (2019). Prevalence of violence victimization and perpetration among persons aged 13-23 years – Four Sub-Saharan African Countries, 2013-2015. Morbidity and Mortality Weekly Report, 68, 350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank in Honduras (October 2019). Retrieved from https://worldbank.org/en/country/honduras.
- United Nations General Assembly. (2015). Transforming our world: The 2030 Agenda for Sustainable Development.
- VanderEnde K, Chiang L, Mercy J, Shawa M, Hamela J, Maksud N, et al. (2018). Adverse childhood experiences and HIV sexual risk-taking behaviors among young adults in Malawi. Journal of Interpersonal Violence, 33, 1710–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2016). INSPIRE: Seven strategies for ending violence against children. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Yacoub S, Sergio A, & Padgett-Moncada D (2006). Violence related injuries, deaths and disabilities in the capital of Honduras. Injury, 37, 428–434. [DOI] [PubMed] [Google Scholar]
- Zolotor AJ, Runyan DK, Dunne MP, Jain D, Péturs HR, Ramirez C, et al. (2009). ISPCAN child abuse screening tool children’s version (ICAST-C): Instrument development and multi-national pilot testing. Child Abuse & Neglect, 33, 833–841. [DOI] [PubMed] [Google Scholar]


