Abstract
Background
A lack of resources has created waiting lists for many elective surgical procedures within Canada's universal health care system. Coronary artery bypass grafting (CABG) for the treatment of atherosclerotic ischemic heart disease is one of these affected surgical procedures. We studied the impact of waiting times on the quality of life of patients awaiting CABG.
Methods
A prospective cohort of 266 patients from 3 hospitals in Montreal was used. Patients who gave informed consent were followed from the time they were registered for CABG until 6 months after surgery; recruitment began in November 1993, and the last follow-up was completed in July 1995. Patient groups were classified according to the duration of the wait for CABG (≤ 97 days or >> 97 days). We measured the following outcomes: quality of life (using the Medical Outcomes Study 36-item Short Form [SF-36]), incidence of chest pain (using the New York Heart Association angina classification), frequency of symptoms (using the Cardiac Symptom Inventory) and rates of complications and death before and after surgery.
Results
There were no differences in quality of life at baseline between the 2 groups. Immediately before surgery, compared with patients who waited 97 days or less, those who waited longer had significantly reduced physical functioning (change from baseline SF-36 score 0 v. –4 respectively, p = 0.001), vitality (change from baseline score –0.1 v. –1.3, p = 0.01), social functioning (change from baseline score 0.4 v. –0.4, p = 0.03) and general health (change from baseline score 1.1 v. –1.7, p = 0.001). At 6 months after surgery, compared with patients who waited 97 days or less for CABG, those who waited longer had reduced physical functioning (change from baseline SF-36 score 4.0 v. –0.1 respectively, p = 0.001), physical role (change from baseline score 0.8 v. 0.0, p = 0.001), vitality (change from baseline score 2.2 v. 0.9, p = 0.001), mental health (change from baseline score 1.2 v. 0.0, p = 0.001) and general health (change from baseline score 1.8 v. –0.3, p = 0.001). The incidence of postoperative adverse events was significantly greater among the patients with longer waits for CABG than among those with shorter waits (32 v. 14 events respectively, p = 0.005). Longer waits before CABG were associated with an increased likelihood of not returning to work after surgery (p = 0.08): 10 (53%) of the 19 patients with longer waiting times remained employed after CABG, as compared with 17 (85%) of the 20 with shorter waiting times.
Interpretation
The significant decrease in physical and social functioning, both before and after surgery, for patients waiting more than 3 months for CABG is an important observation. Longer waiting times were also associated with increased postoperative adverse events. By decreasing waiting times for CABG, we may improve patients' quality of life and decrease the psychological morbidity associated with CABG.
Cardiovascular disease is a major cause of morbidity and death in the Western world and remains the primary cause of death in North America, with about 50 000 Canadians dying of cardiovascular disease every year. In 1990, cardiovascular disease caused 39% of all deaths in Canada, and over half of these deaths resulted from ischemic coronary artery disease (CAD).1 Because of improvements in health care and changes in patients' attitudes and behaviours, the rate of death from cardiovascular disease has decreased in recent years.2,3,4,5,6,7 As a result, the number of individuals alive with cardiovascular disease has grown, leading to an increased demand for health care services.
Coronary artery bypass grafting (CABG) is an effective treatment of CAD. It has been shown both to relieve angina in the majority of patients undergoing the procedure and to prolong life in a large proportion of patients.8,9,10 The more severe the CAD, the stronger the indication for CABG as opposed to treatment with lifestyle modification, medical treatment or angioplasty.11,12,13,14,15,16,17 Coronary artery revascularization as a treatment of CAD is common, and its popularity and use in Canada and throughout the Western world continues to rise.18 In Quebec, the number of CABG procedures increased from 2016 in 1981 to 3273 in 1987 and has risen further since then.3,6
In the United States, because of alternatives in the health care system, there is virtually no wait for coronary artery revascularization procedures. Between 1981 and 1987, there was a 108% increase in the number of CABG procedures performed there, compared with only a 39% increase in Canada. The annual population rate of CABG in the United States is about twice the Canadian rate.2,3,19 In Canada, economic constraints of an overloaded medical system have meant a lack of resources and facilities to accommodate all of the patients requiring bypass surgery. Waiting lists vary in length from 3 to 9 months. In 1980, the average waiting time for CABG at the Montreal Heart Institute was 3–4 months, and by 1990 the wait had increased to 9 months.20
In 1991, there were 13 618 CABG procedures performed in Canada, with a mean waiting time to elective surgery of 21.3 weeks. The longest waiting times occurred in Quebec, with a mean of 34 weeks.21 Long waiting times before coronary artery revascularization procedures have been associated with an increased number of cardiac events, increased mortality, increased costs and decreased quality of life.18,22,23 During long waits, patients may experience psychological distress, anxiety and depression.24,25 Such psychological effects have been found to persist after surgery.26,27,28
Priority scoring systems have been implemented in some settings to triage patients to shorter or longer waiting periods for CABG on the basis of disease severity. However, these systems have been shown to be poor predictors of clinical events and outcome.21,29,30,31 Quality of life is used as an outcome measure when studying chronic disease states, such as CAD, and when evaluating treatments that may prolong life while concurrently increasing morbidity.32,33,34 CABG may increase the life span of selected patients with CAD; however, patients remain ill with progressive chronic atherosclerosis. Symptoms may thus recur even within the first 10 years after surgery.35 The evaluation of quality of life of patients undergoing CABG is therefore essential.36,37,38,39
The rationale behind the present study is based on the strong evidence that CABG significantly improves the quality of many patients' lives by reducing angina and decreasing psychological distress. However, this improvement depends on the physical, social and psychological status of the patient before surgery, which may deteriorate as waiting times for CABG increase. We prospectively evaluated the effects of a prolonged waiting time on the quality of life of patients before and after CABG.
Methods
All patients who were registered to undergo elective CABG at 3 hospitals in Montreal (the Royal Victoria Hospital, the Montreal General Hospital and the Montreal Heart Institute) were eligible for inclusion in the study. Patients were prospectively enrolled at the time of their initial evaluation when it was decided that CABG was indicated by the treating cardiac surgeon (on the basis of angiogram, symptoms or stress test results). The treating surgeon described the study to the patient, and study personnel enrolled the patient after receiving informed consent. Patients were excluded if the CABG was performed on an emergency basis (because of unstable angina or myocardial infarction) and the patient was not on the waiting list; there was a language barrier, or physical or neuropsychological health problem that prevented adequate comprehension or prevented the interview from being properly conducted; or the patient had undergone previous angioplasty or CABG.
The recruitment period was from November 1993 to December 1994. A total of 280 patients were enrolled; 6 were excluded before follow-up (4 did not undergo surgery and 2 died during surgery). Of the 274 remaining patients, 8 were lost to follow-up before the 6-month postoperative evaluation. This left 266 patients who completed the study.
Participants were followed from the time they were enrolled until 6 months after CABG. They were interviewed at the time of their enrolment, immediately before surgery, 6 weeks after surgery and 6 months after surgery. One of 3 research assistants conducted interviews in hospital, at the patients' homes and over the telephone.
Sociodemographic data, baseline clinical characteristics and baseline clinical status of all patients were recorded at the initial interview. The baseline clinical status was based on medical history (previous cerebrovascular event or myocardial infarction) and the presence of comorbid conditions (congestive heart failure, diabetes mellitus, chronic obstructive pulmonary disease (COPD), rheumatologic disease, cancer). The New York Heart Association angina classification40 was used to evaluate the severity of angina symptoms by evaluating the patient's pain, discomfort and limitation of activities. The Cardiac Symptom Inventory39 was used to measure the frequency of 8 cardiac-related symptoms: fatigue, pain in the arm or neck, chest heaviness, breathlessness, palpitations, chest pain, edema of the extremities and chest tightness. Patients were asked to rate the frequency of these symptoms on a 4-point scale. Total scores, out of a possible 24, were standardized to scores out of 100; higher scores signified a higher frequency of symptoms. Quality of life was measured with the use of the Medical Outcomes Study 36-item Short Form (SF-36).41,42,43 This instrument measures physical functioning, physical role, vitality, pain, emotional role, social functioning, mental health and general health. It was administered at baseline, immediately before surgery, 6 weeks after surgery and 6 months after surgery.
We recorded the incidence of the following adverse events before, and up to 6 months after, CABG: myocardial infarction (determined by clinical ischemic pain, new appearance of Q waves or left bundle branch block, elevated creatine kinase [CK] level [to more than twice the upper limit of normal] or elevated CK-MB fraction); new unstable angina (determined by decreased threshold and increased intensity, frequency or duration of pain, and by rest pain with ST-segment elevation, ST-segment depression or T-wave inversion); hospital admission (admission for any reason; admissions were subclassified according to relation to CAD); and death (death from any cause). In addition, we reviewed the patients' charts to determine the occurrence of postoperative complications (myocardial infarction, cerebrovascular accident or stroke, or death).
Mean SF-36 scores were calculated for each study period and for each patient group. The cohort was divided into 2 groups according to the number of days' waiting from enrolment to surgery. The number of days for each group, corresponding roughly to 3 months, was determined to allow similar numbers of patients in each group for comparison of outcomes. Patients with a short waiting time were those who underwent CABG within 97 days after enrolment; those with a long waiting time underwent CABG after 97 days. Differences in the mean SF-36 scores were tested by means of one-way analysis of variance. Differences in proportions were tested by means of the χ2 test.
Results
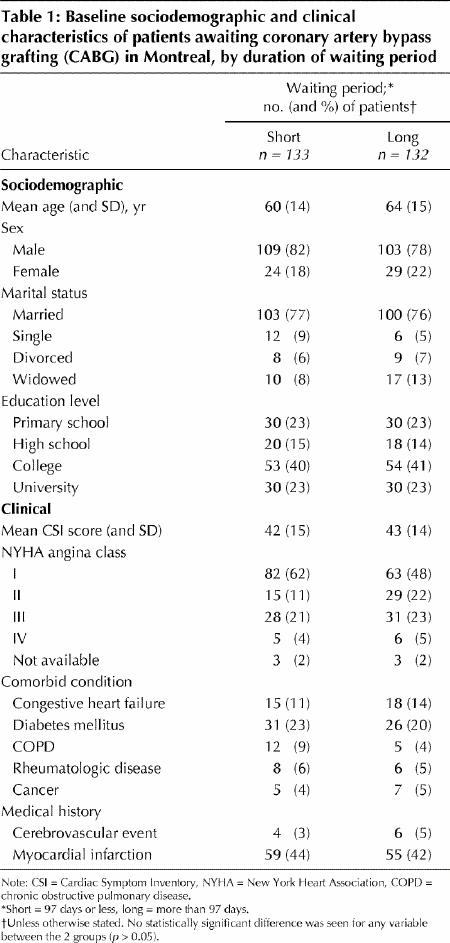
The sociodemographic characteristics of the 266 patients included in the study are presented in Table 1. The majority of the patients in both groups were men (80%), and the mean age of the participants was 62 years. The baseline clinical characteristics and severity of cardiac symptoms were similar for the 2 groups (Table 1). The comorbidity at baseline was also similar for the 2 groups. However, there was a slightly lower prevalence of COPD and diabetes in the group with a longer waiting time; this difference was not statistically significant. The frequency of cerebrovascular events and myocardial infarctions at baseline was similar for both groups.
Table 1
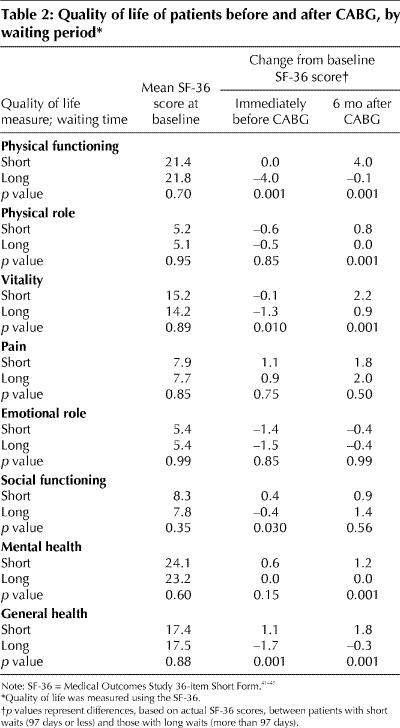
The SF-36 scores are given in Table 2. At baseline, there were no differences in the quality of life between the 2 groups. Immediately before surgery, patients who waited longer than 97 days for CABG had significantly lower scores for physical functioning (p = 0.001), vitality (p = 0.010), social functioning (p = 0.030) and general health (p = 0.001) than the patients with a shorter waiting time. At 6 months after surgery, patients who waited more than 97 days had significantly lower scores for physical functioning (p = 0.001), physical role (p = 0.001), vitality (p = 0.001), mental health (p = 0.001) and general health (p = 0.001) than patients with a shorter waiting time.
Table 2
The incidence of adverse events before CABG did not differ between the 2 groups. There were 13 adverse events during this period: 6 patients were admitted to hospital because of cardiac-related illness, and 4 had myocardial infarction; 1 patient, in the long-wait group, died while awaiting surgery.
The incidence of postoperative adverse events did differ significantly between the groups: 32 occurred in the group with a long waiting time, as compared with 14 in the group with a shorter waiting time (p = 0.005). The number of cerebrovascular accidents in each group was 14 and 6 respectively (p = 0.10, p = 0.07 in test for trend), and the number of myocardial infarctions was 7 and 2 respectively (p = 0.17, p = 0.09 in test for trend).
Among the patients whose employment status was known, those with a long waiting time before CABG were less likely than those with a shorter waiting time to be employed at 6 months after surgery (p = 0.08). At baseline, the proportion of people working was similar in the long- and short-wait groups: 35% (19/54) and 36% (20/55) respectively. At 6 months after surgery, 10 (53%) of the 19 patients with longer waiting times remained employed, as compared with 17 (85%) of the 20 with shorter waiting times.
Interpretation
The patients' quality of life, both before and after surgery, decreased significantly with increasing waiting times before CABG. The significant decrease in physical and social functioning and in general health that occurred in the preoperative period among patients waiting more than 97 days is alarming. This effect is compounded by the fact that these patients fared significantly worse after surgery than did the patients with a shorter waiting time. With decreased waiting times for CABG, patients' preoperative conditions could be maintained at a more optimum level and hence postoperative morbidity could be decreased.
The increase in the number of postoperative adverse events, specifcally cerebrovascular accident and myocardial infarction, with increasing waiting times is also of concern. These complications can significantly decrease quality of life and increase mortality. In addition, these postoperative complications are costly to the health care system.18
One strength of our study was the homogeneity of the patients: the 2 groups were similar in terms of age, sex, marital status, clinical characteristics, history of cerebrovascular accident and myocardial infarction, comorbid conditions and baseline quality of life. Another strength was the low dropout rate; only 14 (4.9%) of the patients did not complete the study.
Study limitations included an insufficient sample size to detect a statistically significant increase in the number of individual adverse events occurring postoperatively in patients with longer waiting times before CABG. The short follow-up period did not allow long-term evaluation of adverse events and mortality. Another major limitation was the age of the data. However, the waiting time for CABG in Quebec has not shortened since these data were collected, and in some situations it has grown longer.
An important observation in our study is the homogeneity of the patient groups with respect to disease severity and comorbidity. This indicates that these factors were not considered when the patients were placed on the waiting list for surgery. In fact, a subsequent analysis of the data in our study showed that the most significant determinant of the duration of waiting was the surgeon, followed by the institution, whereas disease severity and comorbidity were not significant determinants. This result indicates a lack of triaging and calls for the implementation of policies that would standardize the availability of surgical services and ensure proper queuing of patients with more severe disease.
Footnotes
This article has been peer reviewed.
Competing interests: None declared.
Correspondence to: Dr. John Sampalis, Department of Clinical Epidemiology, Montreal General Hospital, 1650 Cedar Ave., Montreal QC H3G 1A4; fax 514 934-8293; mcsa@musica.mcgill.ca
References
- 1.Christenson JM, Solimano AJ, Williams J, Connolly B, Monik L, Erb-Campbell H, et al. The new American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiac care: presented by the Emergency Cardiac Care Subcommittee of the Heart and Stroke Foundation of Canada. CMAJ 1993;149(5):585-90. [PMC free article] [PubMed]
- 2.Health, United States, 1988. Hyatsville (MD): National Center for Health Statistics; 1989. Pub no (PHS) 89-1232.
- 3.Nair C, Colburn H, Maclean DR, Petrasovits A. Cardiovascular disease in Canada. Health Rep 1989;1(1). [PubMed]
- 4.Mortality, summary list of causes. Vital Statistics series. Ottawa: Statistics Canada; 1988. Cat no 84-209-XPB.
- 5.1990 World Health Statistics Annual. Geneva: World Health Organization; 1991.
- 6.Peters S, Chagani K, Paddon P, Nair C. Coronary artery bypass surgery in Canada. Health Rep 1990;2(1):9-26. [PubMed]
- 7.Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomized controlled trials by the Coronary Artery Bypass Graft Trialists Collaboration. Lancet 1994;344:563-70. [DOI] [PubMed]
- 8.Moliterno DJ, Elliott JM, Topol EJ. Clinical trials of myocardial revascularization. Curr Probl Cardiol 1995;20:121-92. [PubMed]
- 9.Guidelines and indications for coronary artery bypass graft surgery. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Coronary Artery Bypass Graft Surgery). J Am Coll Cardiol 1991;17:543-89. [PubMed]
- 10.Coronary artery surgery study (CASS): a randomized trial of coronary artery bypass surgery. Quality of life in patients randomly assigned to treatment groups. Circulation 1983;68:951-60. [DOI] [PubMed]
- 11.Anderson RP. Will the real CASS stand up? A review and perspective on the coronary artery surgery study. J Thorac Cardiovasc Surg 1986;91:698-709. [PubMed]
- 12.Frye RL, Fisher L, Schaff HV, Gersh BJ, Vlietstra RE, Mock MB. Randomized trials in coronary artery bypass surgery. Prog Cardiovasc Dis 1987;30:1-22. [DOI] [PubMed]
- 13.Califf RM, Pryor DB, Greenfield JC. Beyond randomized clinical trials: applying clinical experience in the treatment of patients with coronary artery disease. Circulation 1986;74:1192-4. [DOI] [PubMed]
- 14.Julian DG. The practical implications of the coronary artery surgery trials. Br Heart J 1985;54:343-50. [DOI] [PMC free article] [PubMed]
- 15.Katz NM. Expectations of coronary artery surgery. Am Fam Physician 1987; 35:181-94. [PubMed]
- 16.Landolt CC, Guyton RA. Lessons learned from randomized trials of coronary bypass surgery: viewpoint of the surgeon. Cardiology 1986;73:212-22. [DOI] [PubMed]
- 17.Black N, Langham S, Coshall C, Parker J. Impact of the 1991 NHS reforms on the availability and use of coronary revascularisation in the UK (1987–1995). Heart 1996;76(Suppl 4):1-30. [DOI] [PMC free article] [PubMed]
- 18.Dupuis G, Kennedy E, Perrault J. The hidden cost of delayed bypass surgery. Clin Invest Med 1990;13:C35.
- 19.Higginson LAJ, Cairns JA, Smith ER. Rates of cardiac catheterization, coronary angioplasty and coronary artery bypass surgery in Canada (1991). Can J Cardiol 1994;10:728-32. [PubMed]
- 20.Causes of death. Vital Statistics series. Ottawa: Statistics Canada; 1988. Cat no 84-208-XPB.
- 21.Jackson NW, Doogue MP, Elliott JM. Priority points and cardiac events while waiting for coronary bypass surgery. Heart 1999;81:367-73. [DOI] [PMC free article] [PubMed]
- 22.Naylor CD, Sykora K, Jaglal SB, Jefferson S. Waiting for coronary artery bypass surgery: population-based study of 8517 consecutive patients in Ontario, Canada. Lancet 1995;346:1605-9. [DOI] [PubMed]
- 23.Bryant B, Mayou R. Prediction of outcome after coronary artery surgery. J Psychosom Res 1989;33:419-27. [DOI] [PubMed]
- 24.Horgan D, Davies B, Hunt D, Westlake GW, Mullerworth M. Psychiatric aspects of coronary artery surgery. Med J Aust 1984;141:587-90. [PubMed]
- 25.Peduzzi P, Hultgren H, Thomsen J, Detre K. Ten-year effect of medical and surgical therapy on quality of life: Veterans Administration Cooperative Study of Coronary Artery Surgery. Am J Cardiol 1987;59:1017-23. [DOI] [PubMed]
- 26.Bass C. Psychosocial outcome after coronary artery bypass surgery. Br J Psychiatry 1984;145:526-32. [PubMed]
- 27.Magni G, Unger HP, Valfre C, Polesel E, Cesari F, Rizzardo R, et al. Psychosocial outcome one year after heart surgery. A prospective study. Arch Intern Med 1987;147:473-7. [PubMed]
- 28.Agnew TM, Whitlock RM, Neutze JM, Kerr AR. Waiting lists for coronary artery surgery: Can they be better organised? N Z Med J 1994;107:211-5. [PubMed]
- 29.Seddon ME, French JK, Amos DJ, Ramanathan K, McLaughlin SC, White HD. Waiting times and prioritization for coronary artery bypass surgery in New Zealand. Heart 1999;81:586-92. [DOI] [PMC free article] [PubMed]
- 30.Doogue M, Brett C, Elliott JM. Life and death on the waiting list for coronary bypass surgery. N Z Med J 1997;110:26-30. [PubMed]
- 31.Troidl H, Spitzer WO, McPeck B, Mulder DS, McKneally MS. Principles and practice of research strategies for surgical investigators. Berlin: Springer-Verlag; 1986. p. 63-4.
- 32.Wood-Dauphinee S, Troidl H. Assessing quality of life in surgical studies. Theor Surg 1989;4:35-44.
- 33.Margolese RG. The place of psychosocial studies in medicine and surgery. J Chronic Dis 1987;40:627-8. [DOI] [PubMed]
- 34.Varnauskas E. Survival, myocardial infarction, and employment status in a prospective randomized study of coronary bypass surgery. Circulation 1985;72 (6 Pt 2):V90-101. [PubMed]
- 35.Scheidt S. Ischemic heart disease: a patient-specific therapeutic approach with emphasis on quality of life considerations. Am Heart J 1987;114(1 Pt 2):251-7. [DOI] [PubMed]
- 36.Kaplan RM. Health-related quality of life in cardiovascular disease. J Consult Clin Psychol 1988;56:382-92. [DOI] [PubMed]
- 37.Wenger NK, Mattson ME, Furberg CD, Elinson J, editors. Assessment of quality of life in clinical trials of cardiovascular therapies. New York: Le Jacq; 1984. p. 908-14. [DOI] [PubMed]
- 38.Fletcher AE, Hunt BM, Bulpitt CJ. Evaluation of quality of life in clinical trials of cardiovascular disease. Br J Clin Pharmacol 1986;21:173S-81S. [DOI] [PubMed]
- 39.Frasure-Smith N. The psychological outcomes of coronary bypass surgery. A study of patient and spouse adjustment during the first post-surgical year. Final report to the National Health Research and Development Program. Ottawa: National Health Research and Development Program, Health Canada; 1988. Report no 6605-2021-44.
- 40.Criteria Committee of the New York Heart Association. Nomenclature and criteria for the diagnosis of diseases of the heart and great vessels. 9th ed. Boston: Little Brown; 1994. p. 253-6.
- 41.Tarlov AR, Ware JE Jr, Greenfield S, Nelson EC, Perrin E, Zubkoff M. The Medical Outcomes Study. An application of methods for monitoring the results of medical care. JAMA 1989;262:925-30. [DOI] [PubMed]
- 42.Stewart AL, Hays RD, Ware JE Jr. The MOS short-form general health survey. Reliability and validity in a patient population. Med Care 1988;26:724-35. [DOI] [PubMed]
- 43.Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, et al. Functional status and well-being of patients with chronic conditions. JAMA 1989;262:907-13. [PubMed]


