Abstract
Background:
Several studies have reported that medical robot-assisted method (RA) might be superior to conventional freehand method (FH) in orthopedic surgery. Yet the results are still controversial, especially in terms of femoral neck fractures surgery. Here, 2 methods were assessed based on current evidence.
Methods:
Electronic databases including Cochrane Library, PubMed, Web of Science. and EMBASE were selected to retrieved to identify eligible studies between freehand and RAs in femoral neck fractures, with 2 reviewers independently reviewing included studies as well as collecting data.
Results:
A total of 5 studies with 331 patients were included. Results indicated that 2 surgical methods were equivalent in terms of surgical duration, Harris score, fracture healing time, fracture healing proportion and complications, while RA showed clinical benefits in radiation exposure, intraoperative bleeding, total drilling times, and screw parallelism.
Conclusions:
Current literature revealed significantly difference between 2 techniques and suggested that RA might be beneficial for patients than freehand method.
Keywords: cannulated screw, femoral neck fractures, freehand, meta-analysis, robot-assisted, systematic review
1. Introduction
As a common orthopedic trauma, femoral neck fractures may occur in any age group, especially in the middle-aged and elderly.[1] Due to high-energy trauma, young adults are also likely to suffer femoral neck fractures, yet only accounting 2% to 3%.[1,2] Surgery was increasingly advocated in most femoral neck fractures, including: in situ fixation, closed or open reduction and internal fixation, hemiarthroplasty, and total hip arthroplasty.[3] The Garden classification was selected to guide the surgical method for the femoral neck fractures and was commonly divided into 4 types.[4] Although surgical treatment was reported to be optimal, they often resulted in many complications, including avascular necrosis of the femoral head (14.3%), nonunion (9.3%), malunion (7.1%), implant failure (9.7%), and surgical site infection (5.1%), which may due to poor reduction, fixation instability, and osteoporosis.[2,5–7] Cannulated screw fixation is a standard surgical procedure for femoral neck fractures in all age-groups and accurate screw placement is consider to be essential in stable fracture fixation.[8]
Compared with FH, computer assisted orthopedic surgery developed quickly, including:
-
1.
Improvement of image-guided surgery;
-
2.
Navigation systems and peri–operative assessment devices;
-
3.
Robotics and simulation;
-
4.
Artificial intelligence, algorithms and simulation.
These developments aim to improve visibility to the surgical field, offers hitherto unavailable quantitative data, and increases geometrical accuracy when carrying out surgical procedures.[9,10] For more than 2 decades, the continuous development and functional improvement of robot-assisted method (RA) orthopedic surgery has been more accurate, minimally invasive and safe, and accepted by an increasing number of orthopedic doctors and promoted in clinical practice.[11] Yet conversely, they were still not commonplace compared to un-assisted, conventional freehand method surgery (FH)[2,9–11] as previous studies failed to prove that RA provided better clinical outcome than FH.[12–15] Up to now, meta-analysis comparing RA and FH in pedicle screws implantation in spine and total hip arthroplasty have been published and various robots, including: Renaissance, Spine Assist, ROSA, Mazor, ROBODOC, and MAKO were proved to improve the accuracy and decrease radiation time.[16–18] However, due to the rarity of the RA application in femoral neck fractures, no systematic review and meta-analysis was performed before. On the basis of previous researches, this study attempted to investigate the operation time (surgical duration), fluoroscopy frequency (radiation exposure), intraoperative bleeding, total drilling times, screw parallelism (the accuracy of screw), Harris score, fracture healing time, fracture healing proportion and complications between RA and FH techniques.
2. Materials and methods
2.1. Search strategy
This systematic review and meta-analysis conformed to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.[19] Several databases, including the Cochrane Library, PubMed, Web of Science and EMBASE, were searched for eligible articles before August 2020, comparing at least 2 techniques for the cannulated screw insertion involving femoral neck fractures. We adopted the following search strategy: containing the combinations of navigation or navigate, robot or robotic, screw or screws, hip fracture or femur fracture, or femoral neck fractures. The literature search was performed without restriction to article type, publication date or language.
2.2. Eligibility criteria
2.2.1. Types of studies
Randomized controlled trials, prospective cohort, retrospective cohort, or case-control studies of FH and RA surgery for femoral neck fracture were included in this systematic review and meta-analysis. As for other types of publication, reviews, case reports, conference, and meta-analyses will be excluded from the study.
2.2.2. Types of participants and interventions
Patients diagnosed with femur fracture or femoral neck fractures or hip fracture were included in our study. Studies assessing the effect of RA in animals or artificial femoral neck models were excluded. Interventions must be that patients in experimental groups received RA surgery for cannulated screw implantation while patients in control groups received conventional FH fixation.
2.2.3. Types of outcome
Outcomes included operation time (surgical duration), fluoroscopy frequency (radiation exposure), intraoperative bleeding, total drilling times, screw parallelism (the accuracy of screw), Harris score, fracture healing time, fracture healing proportion and complications between RA and FH were collected.
2.3. Data extraction and quality assessment
The articles’ full-text was reviewed when the titles, subtitles and abstracts were conformed to eligibility criteria. Two reviewers (Zheng and Lu) were independently responsible for articles selection and evaluating the risk of bias based on the Cochrane Handbook. Any discrepancies were compared and resolved through the senior (Qian) reviewer for a consensus. Two authors independently collected the basic and clinical information, including: first author's name, year of the publication, study type, number of patients, robot type and clinical outcomes. Additionally, postoperative complications were collected and classified through the Clavien–Dindo classification system.[20]
2.4. Ethics
As a meta-analysis; ethical approval, as well as institutional review board approval, was not applicable for the study because the included data were extracted from previously reported articles, and identification information of participants were not provided.
2.5. Data analysis
Review Manager 5.3 (Cochrane Collaboration, Oxford, UK) and SPSS 19.0 software (SPSS, Inc., Chicago, IL) were used for the statistical analysis. The results were further analyzed by Chi-Squared test and Fisher exact test. Plus, P values <.05 of the 2-sided tests were defined as statistically significant. Weighted mean differences (WMD) and standardized mean differences (SMD) were used to compare continuous variables, and risk ratios (RR) was applied to compare dichotomous variables, respectively. SMD was adopted when the methods or units of outcome measurements were different. The associated 95% confidence intervals (CI) were summarized. The heterogeneity of individual studies was assessed, according to the Higgins I2 statistic (I2 > 50% was defined as a threshold). A random effects model (I2 > 50%) or a fixed effect (I2 < 50%) was selected depended on the heterogeneity between studies. Sensitivity analysis and subgroup analysis were adopted for significant heterogeneity.
3. Results
3.1. Literature search
By searching the PubMed, Web of Science, Embase, and Cochrane Library databases, 651 articles were identified as potentially relevant, with 342 excluded as duplicates. After screening of titles and abstracts, 287 articles were excluded with irrelevant topics and article type. The full-text of the remaining 34 articles were assessed and 5 articles were eligible for inclusion in the systematic review and meta-analysis. Final search results of the literature were presented in Figure 1.
Figure 1.
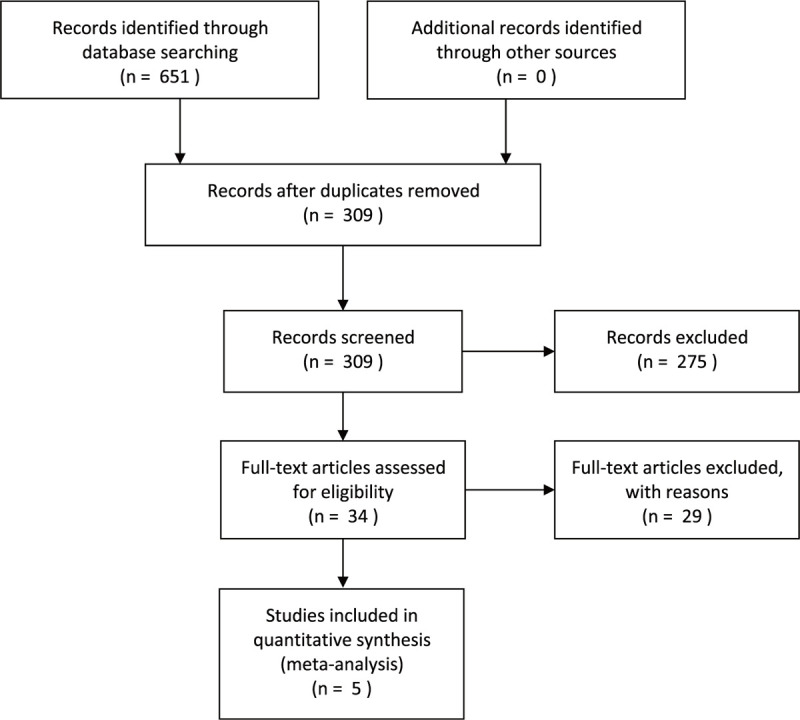
Study flow diagram.
3.2. Study characteristics and quality
Five single center studies involving 159 patients in RA groups and 172 patients in FH groups were included in this study. The average age of the participants was between 44 and 62. Injuries were caused by traffic injuries, sports injuries, slip injuries and high-level falls, and the average time from injury to surgery was between 27.55 and 151.2 hours. There were no statistically significant differences between the 2 groups in gender, age, cause of injury, fracture lateral, fracture type and time from injury to surgery (P > .05). There were 4 retrospective case–control studies[1,2,13,21] and 1 prospective study[11] that compared a series of patients. Four studies used the bi-planar robot system (TINAV/TiRobot Medical Technologies, China)[1,2,11,21] and 1 used the UR Positioning Robots (Universal Robots, Denmark).[13] All the studies selected X-ray images of patients to evaluate the accuracy of screws implantation. The mean time of followed up was 12 to 24 months, and the Harris scores and the final results of the fracture healing between 2 groups were compared. All studies were published within past 5 years. The main characteristics of the included studies are listed in Table 1.
Table 1.
Main characteristics of included studies.
| Patients | |||||
| Study | Year | Study type | RA | FH | Robot type |
| Meng et al | 2019 | retrospective | 30 | 30 | TiRobot |
| Sheng-jun et al | 2019 | prospective | 26 | 23 | TiRobot |
| Xiao-dong et al | 2019 | retrospective | 63 | 65 | TiRobot |
| Yanxiang et al | 2017 | retrospective | 20 | 36 | Universal Robots |
| Yi et al | 2016 | retrospective | 20 | 18 | TiRobot |
The Cochrane Handbook was employed to assess the risk of bias for included studies, including 6 domains: random sequence generation, allocation concealment, blinding of patients and personnel, blinding of outcome assessment, incomplete outcome data, and selective reporting risk. Three studies failed to report the random sequence generation and allocation concealment.[1,13,21] Blinding of patients and personnel was unfeasible to surgeons in the included studies and the risk of bias was judged high. The outcome assessments were reported in all articles and they were judged to low risk of bias. When it comes to the incomplete outcome, the Meng et al study was judged as high risk of bias because they failed to report intraoperative bleeding.[2] Similarly, the data of screw parallelism, fracture healing time and complications were incomplete, which might reduce the reliability of conclusion. Among them, 2 articles were published in Chinese and hence may generate other bias.[1,21] The reviewers judgments on risk of bias of each study is presented in Figure 2.
Figure 2.
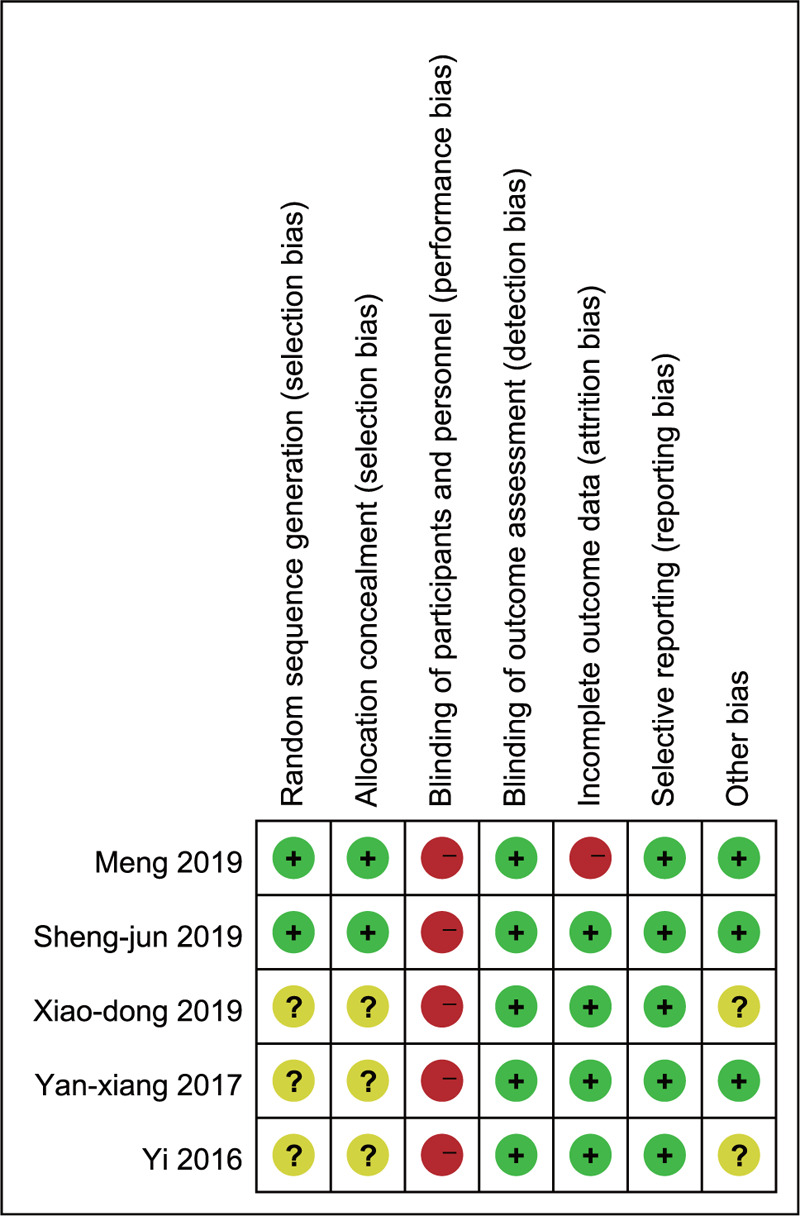
Risk of bias summary: review authors’ judgments about included studies.
3.3. Meta-analysis results
3.3.1. Surgical duration and radiation exposure
Four studies defined the duration of the operation as either starting the aseptic surgical sheet or starting the robotic system and ending at the end of the sutured incision, while 1 study collected the data of total placement time of cannulated screws (minutes).[2] Compared with the FH group, the surgical duration of the RA group was shortened in 2 studies[1,2] and prolonged in 1 study[13] while other 2 studies found no statistical significance.[11,21] The combination of these studies suggested that there were no significant difference in overall surgical duration between RA and FH screw implantation (I2 = 89%; SMD: −0.30; 95% CI, −1.01 to 0.41; P = .41) (Fig. 3). For, radiation exposure, 3 studies reported fluoroscopy frequency (number) as the intraoperative radiation exposure[1,11,13] and 2 studies provided radiation exposure time.[2,21] Results showed that the radiation exposure significantly reduced in the RA group compared with FH screw placement (I2 = 91%; SMD: −2.02; 95% CI, −2.98 to −1.06; P < .001) (Fig. 4).
Figure 3.
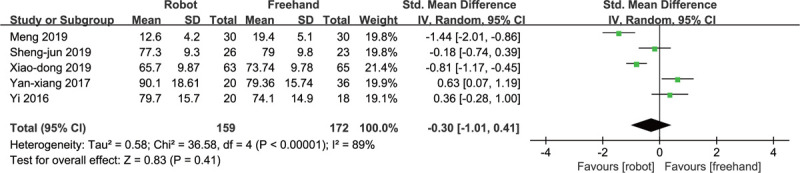
Forest plot of RA vs FH: surgical duration.
Figure 4.
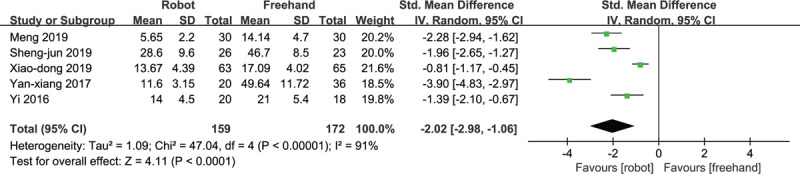
Forest plot of RA vs FH: radiation exposure.
3.3.2. Intraoperative bleeding and total drilling times
The amount of intraoperative bleeding was compared in 4 studies and they all supported that the blood loss in RA group was significantly lower than FH group (I2 = 98%; WMD: −18.29; 95% CI, −30.08 to −6.51; P = .002) (Fig. 5). For total drilling times, only 1 study compared the average drilling attempt for each screw[2] while other 4 studies compared the total times of the screw placements. There was significant difference between the 2 groups (I2 = 93%; SMD: −2.57; 95% CI, −3.70 to −1.43; P < .001) (Fig. 6).
Figure 5.
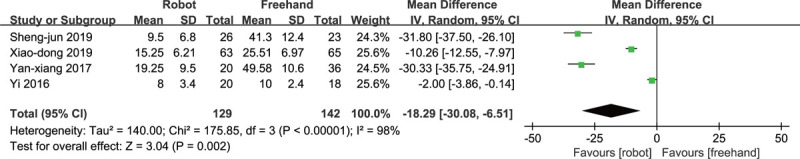
Forest plot of RA vs FH: intraoperative bleeding.
Figure 6.
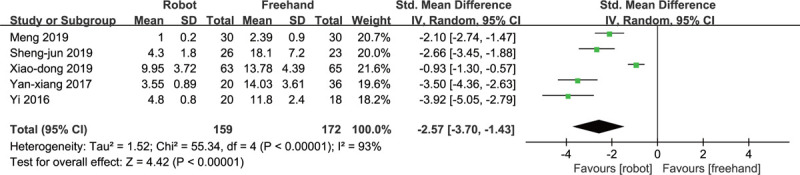
Forest plot of RA vs FH: total drilling times.
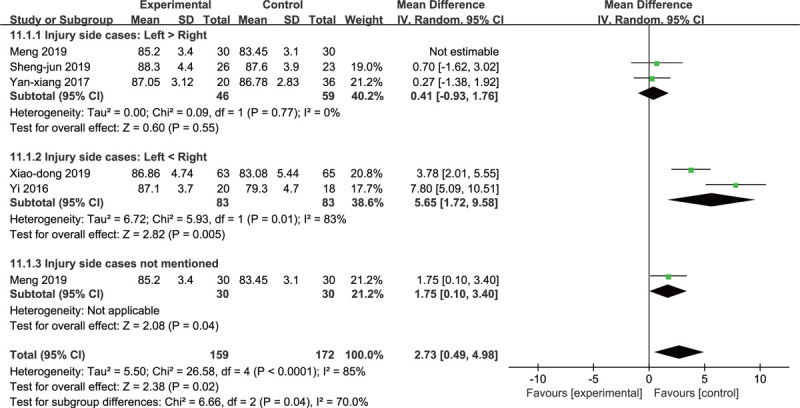
3.3.3. Screw parallelism and Harris score
Anteroposterior and lateral X-ray images of the hip joint were taken after the cannulated screw was placed and the parallelism and dispersion of the screws were measured on the plain and lateral films[2]. Only 2 studies reported the anteroposterior screw shaft angle and lateral screw shaft angle.[2,21] Results indicated that the screws inserted in the robot group have better dispersion (I2 = 100%; WMD: −1.59; 95% CI, −2.91 to −0.28; P = .02) (Fig. 7) and the differences between subgroup was low (P = .78; I2 = 0%). Sheng-jun et al reported the screw parallelism without mentioning the measure methods (robot: 24.0 ± 0.6 compared freehand: 21.5 ± 1.2, P < .001).[11] The Harris score was applied to evaluate the functional recovery after 12 months or at the last follow-up of the operation. All included patients were evaluated according to the Harris scoring standard, including: pain, function, degree of deformity, and range of motion.[22] It is also noteworthy that the combination of the results demonstrated that the Harris score was higher in the RA group (I2 = 85%; WMD: 2.73; 95% CI, 0.49–4.98; P = .02) (Fig. 8).
Figure 7.
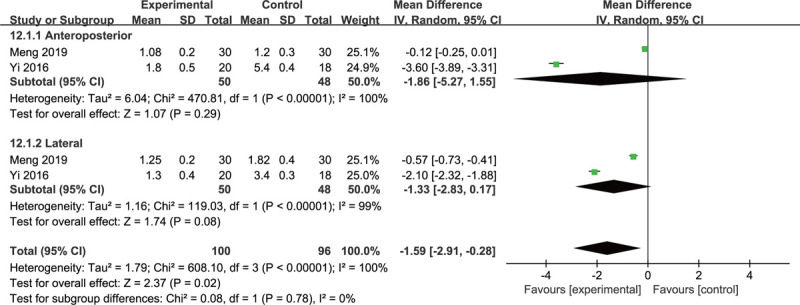
Forest plot of RA vs FH: subgroup analysis of screw parallelism according to the anteroposterior and lateral X-ray images of the hip joint.
Figure 8.
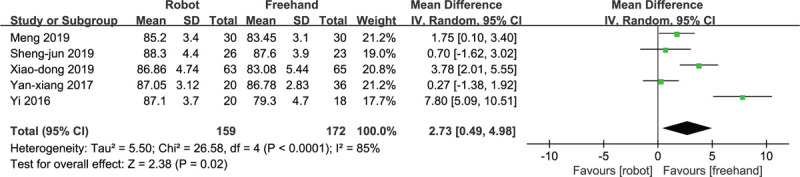
Forest plot of RA vs FH: Harris score.
3.3.4. Fracture healing time and proportion
Three studies reported the fracture healing time after the operation while the unit of time was different.[11,13,21] Results showed that no significant difference were found between the RA group and the FH group (I2 = 29%; SMD: −0.28; 95% CI, −0.61 to 0.06; P = .11) (Fig. 9). The combined results suggested that robot-assisted screw placement was not prior to freehand approach (I2 = 0%; RR: 1.02; 95% CI, 0.97–1.08; P = .43) (Fig. 10).
Figure 9.
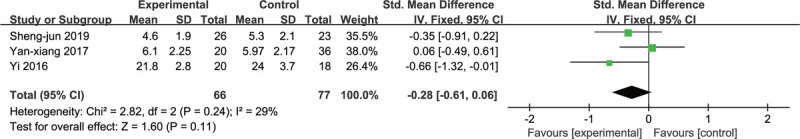
Forest plot of RA vs FH: fracture healing time.
Figure 10.
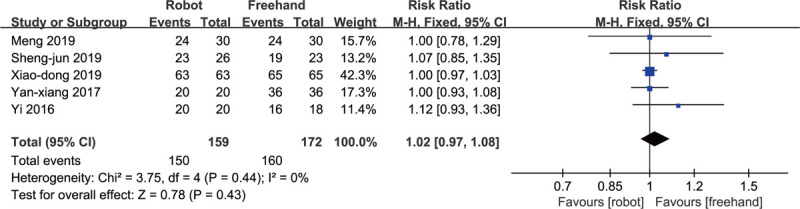
Forest plot of RA vs FH: fracture healing proportion.
3.3.5. Complications
Three studies[11,13,21] claimed no complication after operation while 2 studies[1,2] reported a total of 15 patients with 5 complications among 188 patients. Meanwhile, no significant differences were observed between 2 groups in overall complications rate (6.45% compared with 9.47%, I2 = 37%; RR: 0.69; 95% CI, 0.27–1.73; P = .43). Based on the Clavien–Dindo classification, major complications (Clavien–Dindo grade III/IV) required surgical, endoscopic, or radiologic intervention or life-threatening complications. Since several patients behaved more than 1 complication, the unit of major and minor complications was person-time. Also, no significant difference between 2 groups were found in major complications (6.45% compared with 11.58%, I2 = 13%; RR: 0.57; 95% CI, 0.24–1.36; P = .20) (Fig. 11). The Fisher exact test were selected to analyze each complication in major complications (Table 2).
Figure 11.
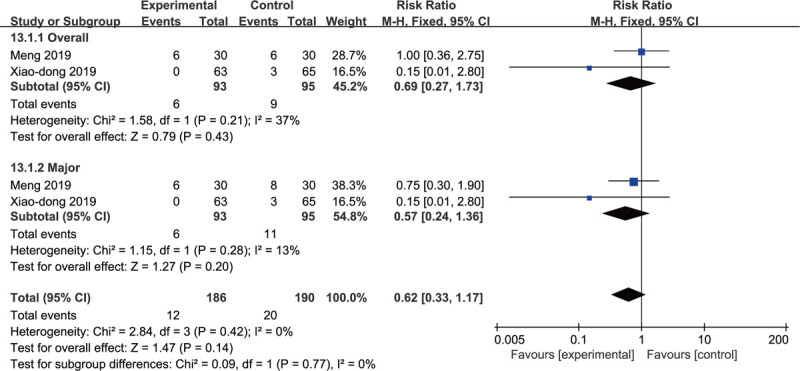
Forest plot of RA vs FH: subgroup analysis of complications according to overall (number) and major (person-time) complications.
Table 2.
Complications between robot-assisted surgery and freehand surgery.
| Complications | RA | FH | P |
| Major complications (person-time) | 6 | 11 | |
| Femoral head necrosis | 1 | 4 | .37 |
| Femoral neck shortened | 5 | 2 | .28 |
| hardware failure | 0 | 3 | .25 |
| Severe fracture | 0 | 2 | .50 |
| Minor complications (person-time) | 0 | 1 | |
| Nonunion | 0 | 1 | 1.00 |
| Total patients (number) | 6 | 9 |
3.3.6. Sensitivity analysis and subgroup analysis
In case that significant heterogeneity existed in the results of surgical duration, radiation exposure, intraoperative bleeding, total drilling times and Harris score. A sensitivity analysis was conducted by omitting 1 study in each turn and analyzed the others to estimate whether the heterogeneity was affected markedly by a single study. This analysis confirmed the stability of the results in surgical duration, radiation exposure and intraoperative bleeding. While excluded the study by Xiao-dong et al and Yi et al, the heterogeneity decreased in total drilling times (from 93–73) and Harris score (from 85–66), respectively,[1,21] which may lead by clinical heterogeneity and methodology heterogeneity. The subgroup analysis was conducted to assess the heterogeneity among studies. The proportion of Garden classification of I and II before the operation were divided into 3 groups: <30%, 30%–60%, >60%. According to the results of subgroup analysis, there was no obvious heterogeneity between studies that the proportion of Garden classification of I and II <30%, and the combined results favored robot-assisted screw placement (I2 = 0%; SMD: −3.65; 95% CI, −4.34 to −2.97; P < .001). Similarly, no obvious heterogeneity existed in the studies 30% to 60% (I2 = 15%; SMD: −2.34; 95% CI, −2.87 to −1.80; P < .001). The subgroup analysis results both showed that the RA group significantly reduced the number of total drilling times compared with the FH group the differences between subgroup was high (P = .78; I2 = 96.2%) (Fig. 12). The statistic difference of Harris score in the included studies was cut into 3 groups: injury side cases of left were more than right, injury side cases of left were less than right, and injury side cases of left and right were unknown. The results of 2 subgroups were opposed (I2 = 0%; WMD: 0.41; 95% CI, −0.93 to 1.76; P = .55 compared with I2 = 83%; WMD: −5.65; 95% CI, 1.72–9.58; P = .005) while the overall results favored RA group and the differences between subgroup was high (P = .04; I2 = 70.0%) (Fig. 13).
Figure 12.
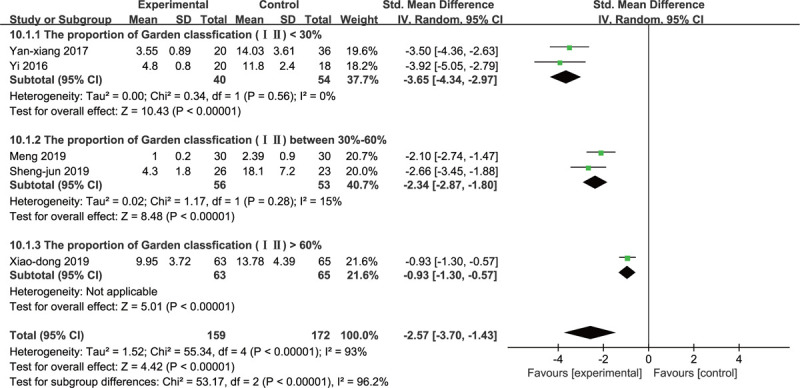
Forest plot of RA vs FH: subgroup analysis of total drilling times according to the proportion of Garden classification of I and II before the operation.
Figure 13.
Forest plot of RA vs FH: subgroup analysis of Harris score according to the injury side cases of each study.
4. Discussion and conclusions
In prior decades, the spine seems to be an appealing field to be exploited by robotic technologies.[23,24] However, the incidence of femoral neck fractures in the middle and elderly is increasing with the aggravation of the aging population and the traffic accidents while the application of robots in femoral neck fractures received less concern.[1,25] To our knowledge, this study was first attempt to conduct the systematic review and meta-analysis to compare RA and FH screw implantation in various aspects for the femoral neck fractures with the consideration of heterogeneity across included studies.[26] This meta-analysis of 4 retrospective studies and 1 prospective study including 331 patients compared the surgical duration, radiation exposure, intraoperative bleeding, total drilling times, screw parallelism, Harris score, fracture healing time, fracture healing proportion, and complications.
In this study, no statistical difference was found in surgical duration, which was consistent with previous hypothesis.[27] However, other studies reported that RA group prolonged the operation time,[14,28] which may be affected by the fact that most of the time was spent on equipment placement and debugging, image acquisition, and other noninvasive procedures, implying that the preoperative preparation time is long.[11] Another study suggested that as a new technique, the increase in RA surgical time can be partly attributed to the learning curve.[26] Extensive radiation exposure may endanger patients and medical staff, and lead to an higher cancer risk.[29,30] Plus, this study reported that the radiation exposure showed significant difference between the 2 groups. Similarly, other studies showed that the radiation exposure in the FH group was 2 to 4 times than RA group.[27,31] On the contrary, other studies reported that the duration of intraoperative radiation exposure was similar between 2 groups which might reflect a request for control of the robot system and limited confidence in the robot system's accuracy.[14,32] Consistent with previous studies, the intraoperative bleeding was less in the robot-assisted group in this study.[33,34] Yet previous studies have claimed that it can reflect the extent of the operation trauma and increase while prolong the duration of the operation.[1,33] In this study, there was no correlation between the surgical duration and the intraoperative bleeding, which may be attributed to the high heterogeneity of included studies and hence lead to false-negative. What's more, results suggested that robot can help surgeons to insert the screws accurately and reduce the total drilling times, which means less trauma and intraoperative bleeding.[11] Since the robot system provided prompts to complete the path planning, drilling positioning and guiding needle adjusting based on 2-D X-ray images while effectively ensured the safety of the operation.[11] In addition, the risk of iatrogenic fractures was reduced due to less drilling attempts and the operating platform can provide the length of the screws after inserted, which helped to complete the screw placement and reduce radiation exposure.[2] The accuracy of screw placement and Harris score were critical for patients, and showed statistical difference in this study. Despite a meta-analysis reported no differences between 2 groups,[35] it has reported that the misplacement rates range from 5% to 41% in the lumbar spine and from 3% to 55% in the thoracic spine with conventional techniques.[36] As long-duration operations predisposed the surgeon to both physical and mental exhaustion and hence decreased the accuracy while robots performed the repetitive tasks, held tools for long periods, eliminated physiological tremor and human manual errors.[17,37,38] Additionally, robots can achieve more accurate and precise movements which was close to 0 mm deviation, while improve the stability of fracture fixation.[11,26] However, the present study revealed the fact that there were no statistical difference in the fracture healing time and proportion between 2 methods. The subgroup analysis showed no difference of complications while the other 3 included studies reported no complications at the end of follow-up, which was consistent with another meta-analysis.[32] Meanwhile, the entry points suggested by the robot were checked by surgeons and hence reduced postoperative revision rate.[32,39,40] The reason may be that the patients were included for routine femoral neck fractures with clear anatomy, resulting in the lack of obvious advantages of the RA system.[31,32] As it suggested that in severe deformity spinal cases with insufficient anatomy, especially when the pedicles were deformed, the RA may be advantageous.[31,32]
Apart from the robots mentioned in this study, Japanese scholars have developed a robot to assist in femoral neck fractures reduction which can track the relative positions of bone fragments and generate an appropriate reduction path.[41] Boiadjiev et al developed a robot which had the advantage of predicting the optimal hole depth, minimized the radiation exposure and reduced the risk of capsule penetration.[42] Both methods have been well tested in the laboratory, but have not yet been applied to the clinic. Although the computer-assisted navigation systems for insertion of cannulated screws in femoral neck fractures presented better results than freehand surgery,[8,43] the robots were superior to computer-assisted navigation group.[44] Moreover, robots may be safely used to train surgical novices in a basic procedure, which is able to avoid harmful radiation and avoid causing potential risk for patients.[45]
Yet conversely, scholars pointed out that RA surgery was expensive and grassroots hospitals need a cheap auxiliary positioning device like Kirschner wire positioning device which can assist in quantitative positioning and guide the placement with high efficiency, less radiation exposure and penetration damage.[46] While another scholar claimed that robots show net cost neutrality, since they are capable to reduce inventory, eliminate surgical trays, improve workflow and surgical efficiency.[47] Besides, robot-assisted surgery required longer preoperative preparation time and placed ilium with an optical tracer, which may be harmful.[2] Meanwhile, the experience of the surgeons to conduct appropriate intraoperative planning is crucial for the robot system.[2]
Several limitations to this study are not expected to be ignored. First, there was a lack of sufficient multi-center randomized controlled studies with a large sample size and long follow-up. Second, the results demonstrated serious statistical heterogeneity, though the sensitivity analysis and subgroup analysis have shown the stability of the results. Third, may be affected by little studies used robots for femoral neck fractures, the conclusion of the present study may only represent the surgical robots for the femoral neck fractures rather than as a whole. Fourth, all of our included studies failed to focus on the effect on each type of Garden classification of femoral fracture.
This meta-analysis suggested that robot-assisted cannulated screw fixation may be superior to conventional freehand method. To be specific, 2 surgical methods were equivalent in terms of surgical duration, Harris score, fracture healing time, fracture healing proportion and complications, while robot-assisted surgery showed clinical benefits in radiation exposure, intraoperative bleeding, total drilling times and screw parallelism. In this paper, 5 robotic studies on femoral neck fracture have been included and preliminary conclusions have been obtained, the authors confirmed that there was a significant benefit to robotics for femoral neck fractures. Although robots in femoral neck fractures are not general currently, it will definitely achieve satisfactory clinical results as it develops. Thus, more well designed comparative studies are required for further validate the benefits of robots for femoral neck fractures.
Acknowledgments
The authors thanks for the data support from included studies.
Author contributions
Conceptualization: Yongshun Zheng, Jiazhao Yang, Fan Zhang, Jinsen Lu, Yeben Qian.
Data curation: Yongshun Zheng.
Formal analysis: Yongshun Zheng, Jiazhao Yang.
Funding acquisition: Yeben Qian.
Investigation: Yongshun Zheng, Jinsen Lu.
Methodology: Yongshun Zheng.
Project administration: Fan Zhang, Yeben Qian.
Resources: Yongshun Zheng, Jiazhao Yang, Fan Zhang, Jinsen Lu.
Software: Yongshun Zheng, Jinsen Lu.
Supervision: Fan Zhang, Jinsen Lu, Yeben Qian.
Validation: Jiazhao Yang, Fan Zhang, Jinsen Lu, Yeben Qian.
Visualization: Yongshun Zheng, Jinsen Lu.
Writing – original draft: Yongshun Zheng.
Writing – review & editing: Jiazhao Yang, Fan Zhang, Jinsen Lu, Yeben Qian.
Footnotes
Abbreviations: CI = confidence interval, FH = freehand method, RA = robot-assisted method, RR = risk ratio, SMD = standardized mean differences, WMD = weighted mean difference.
How to cite this article: Zheng Y, Yang J, Zhang F, Lu J, Qian Y. Robot-assisted vs freehand cannulated screw placement in femoral neck fractures surgery: a systematic review and meta-analysis. Medicine. 2021;100:20(e25926).
This work was supported by the Natural Science Foundation of Anhui Province (1508085MH173, KJ2015A137).
The authors have no conflicts of interests to disclose.
All data generated or analyzed during this study are included in this published article and its supplementary information files.
RA = robot-assisted, FH = freehand.
RA = robot-assisted, FH = freehand.
References
- [1].Wang XD, Lan H, Li KN. Treatment of femoral neck fractures with cannulated screw invasive internal fixation assisted by orthopaedic surgery robot positioning system. Orthop Surg 2019;11:864–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].He M, Han W, Zhao CP, et al. Evaluation of a bi-planar robot navigation system for insertion of cannulated screws in femoral neck fractures. Orthop Surg 2019;11:373–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Florschutz AV, Langford JR, Haidukewych GJ, et al. Femoral neck fractures: current management. J Orthop Trauma 2015;29:121–9. [DOI] [PubMed] [Google Scholar]
- [4].Aggarwal A, Singh M, Aggarwal AN, et al. Assessment of interobserver variation in Garden classification and management of fresh intracapsular femoral neck fracture in adults. Chin J Traumatol 2014;17:99–102. [PubMed] [Google Scholar]
- [5].Miller BJ, Callaghan JJ, Cram P, et al. Changing trends in the treatment of femoral neck fractures: a review of the american board of orthopaedic surgery database. J Bone Joint Surg Am Vol 2014;96:e149. [DOI] [PubMed] [Google Scholar]
- [6].Slobogean GP, Sprague SA, Scott T, et al. Complications following young femoral neck fractures. Injury 2015;46:484–91. [DOI] [PubMed] [Google Scholar]
- [7].Thiele OC, Eckhardt C, Linke B, et al. Factors affecting the stability of screws in human cortical osteoporotic bone: a cadaver study. J Bone Joint Surg Br Vol 2007;89:701–5. [DOI] [PubMed] [Google Scholar]
- [8].Liebergall M, Ben-David D, Weil Y, et al. Computerized navigation for the internal fixation of femoral neck fractures. J Bone Joint Surg Am Vol 2006;88:1748–54. [DOI] [PubMed] [Google Scholar]
- [9].Nolte LP, Beutler T. Basic principles of CAOS. Injury 2004;35: Suppl 1: S-A6-16. [DOI] [PubMed] [Google Scholar]
- [10].Picard F, Deakin AH, Riches PE, et al. Computer assisted orthopaedic surgery: past, present and future. Med Eng Phys 2019;72:55–65. [DOI] [PubMed] [Google Scholar]
- [11].Duan SJ, Liu HS, Wu WC, et al. Robot-assisted percutaneous cannulated screw fixation of femoral neck fractures: preliminary clinical results. Orthop Surg 2019;11:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Verma R, Krishan S, Haendlmayer K, et al. Functional outcome of computer-assisted spinal pedicle screw placement: a systematic review and meta-analysis of 23 studies including 5992 pedicle screws. Eur Spine J 2010;19:370–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Cao Y, Zhao Y, Hu L, et al. Clinical application of computer-assisted cannulated screw internal fixation system based on error correction method for femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2017 Mar;31:257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ringel F, Stuer C, Reinke A, et al. Accuracy of robot-assisted placement of lumbar and sacral pedicle screws: a prospective randomized comparison to conventional freehand screw implantation. Spine 2012;37:E496–501. [DOI] [PubMed] [Google Scholar]
- [15].Laudato PA, Pierzchala K, Schizas C. Pedicle screw insertion accuracy using O-Arm, robotic guidance, or freehand technique: a comparative study. Spine 2018 Mar;43:E373–8. [DOI] [PubMed] [Google Scholar]
- [16].Ghasem A, Sharma A, Greif DN, et al. The arrival of robotics in spine surgery: a review of the literature. Spine 2018;43:1670–7. [DOI] [PubMed] [Google Scholar]
- [17].Joseph JR, Smith BW, Liu X, Park P. Current applications of robotics in spine surgery: a systematic review of the literature. Neurosurg Focus 2017;42:E2. [DOI] [PubMed] [Google Scholar]
- [18].Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty 2016;31:2353–63. [DOI] [PubMed] [Google Scholar]
- [19].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. [DOI] [PubMed] [Google Scholar]
- [20].Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187–96. [DOI] [PubMed] [Google Scholar]
- [21].Tong Y, Luo X, Wu G, et al. Comparative study on fixation with percutaneous cannulated screws assisted by robot navigation and conventional surgery with manual positioning for femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2016;30:685–9. [DOI] [PubMed] [Google Scholar]
- [22].Laklouk MA, Hosny GA. Hinged distraction of the hip joint in the treatment of Perthes disease: evaluation at skeletal maturity. J Pediatr Orthop Part B 2012;21:386–93. [DOI] [PubMed] [Google Scholar]
- [23].Johnson N. Imaging, navigation, and robotics in spine surgery. Spine 2016;41: Suppl 7: S32. [DOI] [PubMed] [Google Scholar]
- [24].Ringel F, Villard J, Ryang YM, et al. Navigation, robotics, and intraoperative imaging in spinal surgery. Adv Tech Standards Neurosurg 2014;41:03–22. [DOI] [PubMed] [Google Scholar]
- [25].Thorngren KG, Hommel A, Norrman PO, et al. Epidemiology of femoral neck fractures. Injury 2002;33: Suppl 3: C1–7. [DOI] [PubMed] [Google Scholar]
- [26].Gao S, Lv Z, Fang H. Robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis of randomized controlled trials. Eur Spine J 2018;27:921–30. [DOI] [PubMed] [Google Scholar]
- [27].Hyun SJ, Kim KJ, Jahng TA, et al. Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine 2017;42:353–8. [DOI] [PubMed] [Google Scholar]
- [28].Kim HJ, Jung WI, Chang BS, et al. A prospective, randomized, controlled trial of robot-assisted vs freehand pedicle screw fixation in spine surgery. Int J Med Robot 2017;13: doi: 10.1002/rcs.1779. Epub 2016 Sep 27. [DOI] [PubMed] [Google Scholar]
- [29].Mastrangelo G, Fedeli U, Fadda E, et al. Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med 2005;55:498–500. [DOI] [PubMed] [Google Scholar]
- [30].Perisinakis K, Damilakis J, Theocharopoulos N, et al. Patient exposure and associated radiation risks from fluoroscopically guided vertebroplasty or kyphoplasty. Radiology 2004;232:701–7. [DOI] [PubMed] [Google Scholar]
- [31].Roser F, Tatagiba M, Maier G. Spinal robotics: current applications and future perspectives. Neurosurgery 2013;72: Suppl 1: 12–8. [DOI] [PubMed] [Google Scholar]
- [32].Yu L, Chen X, Margalit A, et al. Robot-assisted vs freehand pedicle screw fixation in spine surgery - a systematic review and a meta-analysis of comparative studies. Int J Med Robot 2018;14:e1892. [DOI] [PubMed] [Google Scholar]
- [33].Long T, Li KN, Gao JH, et al. Comparative study of percutaneous sacroiliac screw with or without TiRobot assistance for treating pelvic posterior ring fractures. Orthop Surg 2019;11:386–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Matanes E, Boulus S, Lauterbach R, et al. Robotic laparoendoscopic single-site compared with robotic multi-port sacrocolpopexy for apical compartment prolapse. Am J Obstet Gynecol 2020;222:358.e1–e11. [DOI] [PubMed] [Google Scholar]
- [35].Liu H, Chen W, Wang Z, et al. Comparison of the accuracy between robot-assisted and conventional freehand pedicle screw placement: a systematic review and meta-analysis. Int J Comput Assist Radiol Surg 2016;11:2273–81. [DOI] [PubMed] [Google Scholar]
- [36].Mason A, Paulsen R, Babuska JM, et al. The accuracy of pedicle screw placement using intraoperative image guidance systems. J Neurosurg Spine 2014;20:196–203. [DOI] [PubMed] [Google Scholar]
- [37].Overley SC, Cho SK, Mehta AI, et al. Navigation and robotics in spinal surgery: where are we now? Neurosurgery 2017;80:S86–99. [DOI] [PubMed] [Google Scholar]
- [38].Fan Y, Du JP, Liu JJ, et al. Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: an updated meta-analysis. Medicine (Baltimore) 2018;97:e10970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Lonjon N, Chan-Seng E, Costalat V, et al. Robot-assisted spine surgery: feasibility study through a prospective case-matched analysis. Eur Spine J 2016;25:947–55. [DOI] [PubMed] [Google Scholar]
- [40].Schatlo B, Molliqaj G, Cuvinciuc V, et al. Safety and accuracy of robot-assisted versus fluoroscopy-guided pedicle screw insertion for degenerative diseases of the lumbar spine: a matched cohort comparison. J Neurosurg Spine 2014;20:636–43. [DOI] [PubMed] [Google Scholar]
- [41].Joung S, Kamon H, Liao H, et al. A robot assisted hip fracture reduction with a navigation system. Medical image computing and computer-assisted intervention: MICCAI International Conference on Medical Image Computing and Computer-Assisted Intervention 2008;11(Pt 2):501–8. [DOI] [PubMed] [Google Scholar]
- [42].Boiadjiev T, Kastelov R, Boiadjiev G, et al. Automatic bone drilling by femoral head structure detection. Biotechnol Biotechnol Equip 2017;32:785–94. [Google Scholar]
- [43].Muller MC, Belei P, Pennekamp PH, et al. Three-dimensional computer-assisted navigation for the placement of cannulated hip screws. A pilot study. Int Orthop 2012;36:1463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Wang JQ, Zhao CP, Su YG, et al. Computer-assisted navigation systems for insertion of cannulated screws in femoral neck fractures: a comparison of bi-planar robot navigation with optoelectronic navigation in a Synbone hip model trial. Chin Med J 2011;124:3906–11. [PubMed] [Google Scholar]
- [45].Nousiainen MT, Omoto DM, Zingg PO, et al. Training femoral neck screw insertion skills to surgical trainees: computer-assisted surgery versus conventional fluoroscopic technique. J Orthop Trauma 2013;27:87–92. [DOI] [PubMed] [Google Scholar]
- [46].Du GH, Jiang JS, Fu G, et al. Auxiliary positioning of a new positioning device in internal fixation of femoral neck fracture with cannulated screws. Chin J Tissue Eng Res 2020;24:2855–60. [Google Scholar]
- [47].Lonner JH, Fillingham YA. Pros and Cons: a balanced view of robotics in knee arthroplasty. J Arthroplasty 2018;33:2007–13. [DOI] [PubMed] [Google Scholar]


