Abstract
Objectives:
To evaluate and compare the buccolingual inclinations of maxillary and mandibular first molars in untreated children and adults.
Materials and Methods:
One hundred and thirty-eight subjects were selected and divided into three groups, as follows: (1) age 6–9 years, N = 46; (2) age 10–19 years, N = 56; and (3) age 25–35 years, N = 36. For each subject, existing cone beam computed tomography images were used, and the long axis for each maxillary and mandibular first molar was determined. The converge angles formed by the long axis of left and right maxillary first molars and by the long axis of left and right mandibular first molars were measured.
Results:
The maxillary molars exhibited buccal inclination, with the converge angle of 21.1° ± 9.5° in group 1, 17.3° ± 8.6° in group 2, and 9.3° ± 7.3° in group 3. Statistically significant differences were found between groups 1 and 3 and groups 2 and 3, but not between groups 1 and 2. The mandibular molars exhibited lingual inclination, with the converge angle of 34.9° ± 11° for group 1, 26.6° ± 9.2° for group 2, and 26.1° ± 7.7° for group 3. Statistically significant differences were found between groups 1 and 2 and groups 1 and 3, but not between groups 2 and 3.
Conclusions:
Maxillary first molars exhibited buccal inclination. Adults displayed less inclination than did children. Mandibular first molars exhibited lingual inclination. Adults displayed less inclination than did children. Some degree of curve of Wilson should be maintained at the end of orthodontic treatment to fulfill physiologic needs and stability.
Keywords: Buccolingual, Molar, Children, Adults, Inclination
INTRODUCTION
Wilson1 was the first to report the lateral inclination of the grinding teeth, the lower being inclined lingually and the upper being inclined buccally. This occlusal curve in the coronal plane has been referred to as the curve of Wilson. Monson2 reported that the occlusal curve in the coronal plane was tangent to a sphere with a 4-inch radius. This was referred to as the sphere (or curve) of Monson. Dempster et al.3 studied the arrangement of the roots of the teeth in skulls with typical dentition and confirmed the lingual inclination of the mandibular posterior teeth.
Andrews4 suggested the six keys to normal occlusion. The third key relates to crown inclination, which refers to the labiolingual or buccolingual inclination of the long axis of the crown, not to the long axis of the entire tooth. He reported a lingual inclination present in the maxillary and mandibular posterior crowns.
It has been reported that the buccolingual inclination of molar crowns changes with the growth of an individual. Marshall et al.5 found that maxillary molars erupted with a buccal crown inclination and that the first molars uprighted by 3.3°, while the maxillary second molars uprighted by 5.9°, from ages 7.5 to 26.4 years. In contrast, mandibular molars were found to erupt with lingual crown inclination, and mandibular first molars uprighted by 5.0° and mandibular second molars uprighted by 7.5°. Sayania et al.6 studied untreated longitudinal dental casts at ages 6–16 years in 47 males and 48 females. They recorded the height differences between buccal and lingual cusps for the maxillary and mandibular first molars. They reported that maxillary molars erupted with buccal crown inclination at age 6 and uprighted lingually at age 16 (by about 0.4 mm). Mandibular molars erupted with lingual crown inclination at age 6 and uprighted buccally at age 16 (by about 0.5 mm). At age 16, maxillary molars maintained some buccal crown inclination and mandibular molars maintained some lingual inclination.
The American Board of Orthodontics (ABO) evaluates clinically acceptable values for buccolingual inclination of posterior teeth by comparing height differences between buccal and lingual cusps.7 The ABO stated that “In order to establish proper occlusion in maximum intercuspation and avoid balancing interferences, there should not be a significant difference between the heights of the buccal and lingual cusps of the maxillary and mandibular molars and premolars.” The ABO quantitatively evaluates proper buccolingual inclination of posterior teeth using a step gauge, in which the lingual cusps must be within 1 mm of the straight edge.
In most previous studies, evaluation of buccolingual inclination has been limited to the crowns of teeth utilizing model casts. However, there are limitations to using models due to the variations in crown morphology.8,9 Thus, a new method that allows an unobstructed view of crown and root structure is critical in assessing inclination of tooth. With the advent of three-dimensional (3D) imaging, such as cone beam computed tomography (CBCT), practitioners can visualize and measure the true 3D anatomy of patients, which allows measurements to be made in three planes of space. Measurement of the buccolingual inclination of the tooth is best evaluated with a coronal section of the tooth via CBCT.
Information is limited in the literature about the values for buccolingual inclination of molars through long axis in untreated children and adults using 3D imaging. Barrera et al.10 investigated the inclination of maxillary first molars in adults using CBCT. Of the 10 normocclusion adults they evaluated, the average buccal inclination was 4.05° per side; of the 10 malocclusion adults with bilateral posterior crossbite, the average buccal inclination was only 0.2°. Using CT, Kasai and Kawamura11 reported that modern Japanese adult male skulls with relatively normal occlusion had lower first molars with an average lingual inclination of 13.3° per side; however, for the ancient (Jomon) skulls, measured inclination was only 7.4°. They suggested that the difference was due to stronger musculature of the ancient than of the modern people. More recently, Alkhatib and Chung12 investigated the degree of buccolingual inclination of maxillary and mandibular first molars in untreated adults using CBCT. They reported that maxillary first molars had an average buccal inclination of 4.9°, and mandibular first molars had a lingual inclination of 12.6°. However, the buccolingual inclinations in maxillary and mandibular molars in children have not been reported in the literature.
The purpose of this study was to evaluate and compare the buccolingual inclination of maxillary and mandibular first molars of children and adults utilizing CBCT.
MATERIALS AND METHODS
Institutional review board approval was obtained from the University of Pennsylvania prior to collecting any pre-existing CBCT information. The images were previously taken in a private practice with an I-CAT machine (Imaging Sciences International, Hatfield, Pa) with 0.3-mm voxel size. A sample of 138 untreated Caucasian subjects was selected. A CBCT image was taken as a pretreatment record on each subject. The subjects were divided into three groups: (1) age 6–9 years for the child group (21 females, 25 males), (2) age 10–19 years for the adolescent group (27 females, 29 males), and (3) age 25–35 years for the adult group (17 females, 19 males). The inclusion criteria were (1) no prior orthodontic treatment, (2) maxillary and mandibular first molars fully erupted and roots completely formed, (3) skeletal Class I (ANB 0–4°), (4) minimal dental wear, (5) less than 5 mm of crowding per arch, and (6) no missing teeth other than third molars. Subjects were excluded for the following: (1) posterior crossbite, (2) crowns or significant restorations on any first molar, (3) presence of a supernumerary tooth, or (4) craniofacial deformities or evident facial or skeletal asymmetry.
Using Dolphin Imaging (version 10.5, Dolphin Imaging & Management Solutions, Chatsworth, Calif), each image was standardized and oriented such that Frankfort-horizontal and a line connecting the inferior border of the orbital rims were parallel to the floor. The sagittal guideline of the tooth axis was defined, per the guideline of Masumoto et al.,13 as a line that passes through the midpoint of the mesio-distal crown width and the midpoint between both middle points of each the mesial and distal roots at one-third the distance from the root apex. Once the sagittal orientation was determined, the coronal cross section was obtained in a 0.5-mm slice using a section that best fit the right and left molar mesio-distal midpoints. The coronal section was used to measure tooth axes. The long axis of the tooth was defined as a line connecting the midpoint of the buccal and lingual cusp tips and the midpoint of the buccolingual width at the cervical base close to the furcation of the anatomic crown. The angles at which the right and left first molar tooth axes intersected were measured (Figures 1 and 2), which represented the inclination of both left and right molars.
Figure 1.
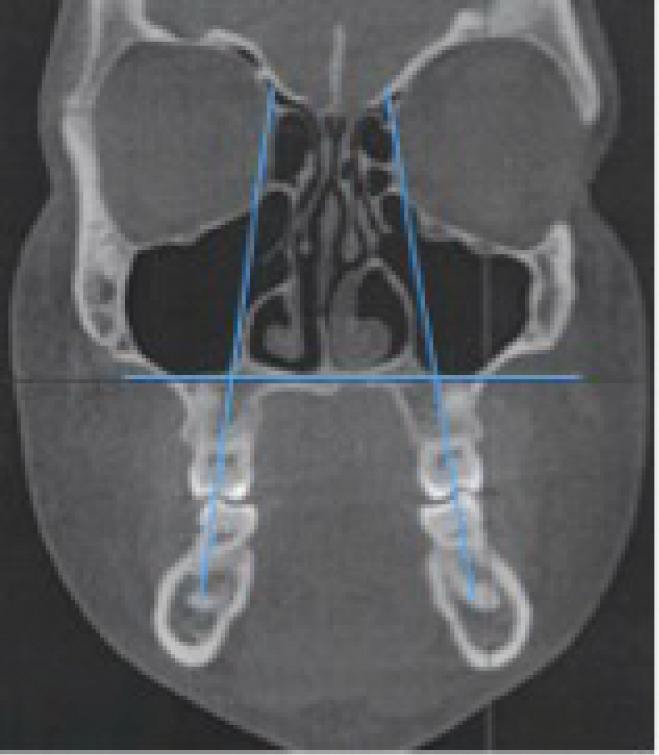
The upper angle formed by the intersection of the maxillary right and left first molar tooth axes.
Figure 2.
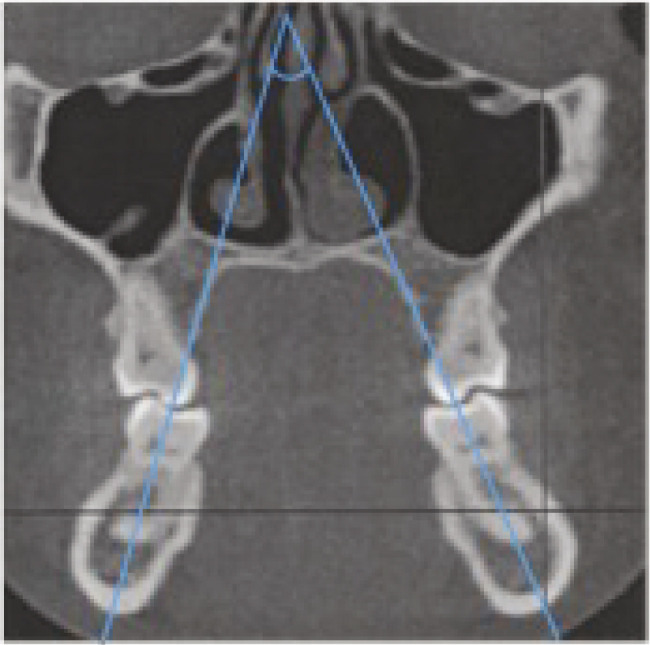
The lower angle formed by the intersection of the mandibular right and left first molar tooth axes.
All measurements were repeated after a 3-week interval by the same investigator (BY). A paired t-test was used for tooth inclination measurements to determine whether there were significant differences compared with the original measurements. An independent sample t-test was utilized to compare measurements between groups of variables, and a P-value of ≤.05 was used to assign statistical significance. The mean and standard deviation (SD) were calculated for each measurement for tooth inclination.
RESULTS
Intraexaminer testing revealed no statistical difference in repeated measurements (P > .05). Table 1 shows the mean, SD, and range of the upper and lower convergent angles of all three groups. In all groups, the maxillary molars showed buccal inclination, and mandibular molars showed lingual inclination. In addition, the mandibular molars were more lingually inclined in magnitude than the maxillary molars were buccally inclined. No statistically significant differences were noted between male and female groups (P > .05).
Table 1.
Mean, Standard Deviation (SD), and Range of the Upper Converge Angle and Lower Converge Angle of All Three Groupsa
| N |
Mean Upper Angle, ° |
Range, ° |
Mean Lower Angle, ° |
Range, ° |
|
| Group 1 (age 6–9 y) | |||||
| Female (F) | 21 | 22.9 ± 8.4 | 7–41.5 | 36.6 ± 12.1 | 20.5–57.5 |
| Male (M) | 25 | 19.6 ± 10.2 | 0–36 | 33.4 ± 10.0 | 14–51.5 |
| F/M combined | 46 | 21.1 ± 9.5 | 0–41.5 | 34.9 ± 11.0 | 14–57.5 |
| Group 2 (age 10–19 y) | |||||
| F | 27 | 18.3 ± 9.5 | 5–33 | 29.1 ± 9.9 | 13–42.5 |
| M | 29 | 16.4 ± 7.9 | 0–35 | 24.3 ± 8.0 | 7–37 |
| F/M combined | 56 | 17.3 ± 8.6 | 0–35 | 26.6 ± 9.2 | 7–42.5 |
| Group 3 (age 20–35 y) | |||||
| F | 17 | 6.8 ± 6.3 | 0–18 | 26.3 ± 8.8 | 2–40 |
| M | 19 | 11.6 ± 7.5 | 1–24.5 | 25.9 ± 6.8 | 15.5–40 |
| F/M combined | 36 | 9.3 ± 7.3 | 0–24.5 | 26.1 ± 7.7 | 2–40 |
No statistically significant difference between male and female in all groups. For F/M combined upper angle, statistically significant difference between groups 1 and 3 and groups 2 and 3, but not between groups 1 and 2. For F/M combined lower angle, statistically significant difference between groups 1 and 2 and groups 1 and 3, but not between groups 2 and 3.
Table 1 also shows that, for maxillary first molars, group 1 (age 6–9 years) combined male and female had a mean of 21.1° ± 9.5°, group 2 had a mean of 17.3° ± 8.6°, and group 3 had a mean of 9.3° ± 7.3°. The differences among these three groups were statistically significantly different between groups 1 and 3 and groups 2 and 3, but not between groups 1 and 2. For mandibular first molars, group 1 had 34.9° ± 11°, group 2 had 26.6° ± 9.2°, and group 3 had 26.1° ± 7.7°. The differences between these three groups were significant between groups 1 and 2 and groups 1 and 3, but not between groups 2 and 3.
DISCUSSION
The advantages of using CBCT are the ability to visualize the whole tooth in order to avoid the uncertainty that results from using dental casts with uneven cuspal wear or irregular tooth morphology. Determining the tooth axis for the upper molars poses specific challenges due to the frequent divergence between the upper molar roots. Barrera et al.10 used a line connecting the central groove to the furcation for the molar axis, which was similar to the method used in this study. Kasai and Kawamura11 defined the long axis to pass through the mid-point at one-half of the crown width and the mid-point at one-third of the distance from the root apex. This accounts for the potential of apical dilacerations but not anomalous root morphology or whole root divergence. Mitra and Ravi14 measured the maxillary molar inclinations using CT; however, only the buccal roots were measured. Shewinvanakitkul et al.15 measured the long axis of the lower first molars to be a line from the central groove to the middle of the root apices. Using the whole root without factoring in dilacerations may have skewed the results. Using the whole crown with the aid of 3D imaging, as was done in the current study, likely provided the most accurate assessment of long axis determination for upper and lower molars.
The results illustrated that the maxillary and mandibular molars were more upright in adults than in children, which was in support of the findings of Marshall et al.5 and Sayania et al.6 It is important to know that at the adult age, normally the maxillary molars still exhibited some buccal inclination, and mandibular molars still exhibited some lingual inclination, which was in agreement with the findings of Berrera et al.10 and Alkhatib and Chung.11
Weinstein et al.16 reported that each unit of the dentition was in equilibrium with its surroundings at any instant. The surroundings can include adjacent teeth, the tongue, the buccolabial musculature, the bone, and the intervening periodontal ligament. The time it takes for the uprighting to occur can be described as the fourth dimension of the equilibrium theory, which Weinstein proposed. Brodie17 and Moyers18 referred to the dimension of time as a contributor to the equilibrium of teeth. Brodie17 stated that as the primary teeth begin to erupt and as the alveolar process is formed to accompany them, the contact is broken between the cheek and lips on one side and the tongue on the other side. Moyers18 stated that a change in muscular environment around a tooth will cause the tooth to move through the bone until it is again in balance.
During analysis of the coronal cuts in the current study, a clear trend was observed that the mandibular basal bone inclination frequently aligned with the lingual inclination of the lower molars. Kohakura et al.19 reported that CT scans on male Asiatic Indians showed a similar relationship between the tooth axis and the bone axis, in which the lower first molar averaged 10.18° ± 4.8° of lingual inclination and the bone inclination averaged 8.35° ± 5.2°. It would be interesting to further pursue the relationship between molar inclination and bone inclination in untreated adults.
Dawson20 presented two reasons for the existence of the curve of Wilson. The first was for optimal resistance to loading, whereby buccolingual inclination of the posterior teeth paralleled the inward pull and orientation of the internal pterygoid muscle contraction to produce the greatest resistance to masticatory forces. The second was that the inward inclination of the occlusal table allowed open access to food as it was being chewed, facilitating the masticatory process. Nanda21 stated that a small curve of Wilson between the buccal segments allowed for proper occlusal function, but that “an accentuated curve would result in balancing interferences, especially in the second molar area.” It is important to determine an appropriate amount of buccolingual tooth inclination for adequate function and to quantify it so that treatment goals are well supported by evidence. Given the orientation of anatomic structures described by Dawson,20 it would be expected that the bone inclination would also be oriented this way for optimal masticatory loading as well. Okeson22 explained that the curve of Wilson exists to ensure the most effective use of cuspal contacts while avoiding nonfunctional contacts known as balancing interferences.
A potential link between buccolingual inclination of molars and vertical facial type has been studied, but the results are scattered and inconsistent. For example, Janson et al.23 reported that there was no statistical variation between low and high angle subjects in mandibular posterior tooth inclination but that maxillary molars had greater buccal inclination in high angle subjects. Conversely, Tsunori et al.24 found that short facial types had more lingual inclination of molars in the mandible.
Andrews25 reported a large range of values for buccolingual inclination for maxillary and mandibular first molar crowns in a sample of normal untreated patients. The current study also showed wide ranges. With such a wide range present in untreated subjects, there may be other factors influencing tooth inclination. There are currently various prescriptions available to clinicians to treat patients, yet the idea of a “one prescription fits all” approach to treatment is often employed because of its simplicity. However, care must be exercised regarding how much torque is expressed to achieve successful treatment outcomes. Dellinger26 wrote that “if full-sized unbent arch wires are placed in the mouth and are allowed to totally work out, that the results could be erratic, inconsistent, and clinically unacceptable.” Germane et al.8 and Ross et al.9 also argued that no fully expressed straight wire appliance could be expected to be correct for all patients. Thus, it is reasonable that, as is the case with treatment goals, choice of prescription, or the degree to which torque is expressed, may need to be tailored to individual patients.
Orthodontic philosophies have varied in their handling of the presence of an occlusal curvature and molar torque. Andrews27 explained, in his Six Elements philosophy, that “each crown must be inclined so that the occlusal surface can interface and function optimally with the teeth in the opposing arch.” McNamara et al.28 suggested that one of the goals of orthodontic treatment should be to flatten the occlusal plane and level the curve of Wilson. Conversely, Dawson20 stated that when the curve of Wilson is made too flat, ease of masticatory function may be impaired. The current results showed that in untreated children and adults, the curve of Wilson is present naturally. It would be logical to consider maintaining some degree of a curve of Wilson after orthodontic treatment to be consistent with the physiologic needs of masticatory function and to encourage stability of treatment.
CONCLUSIONS
Based on this study examining data from untreated children and adults, the following conclusions can be made:
Maxillary first molars exhibited buccal inclination. The adults displayed less inclination than did the children.
Mandibular first molars exhibited lingual inclination. The adults displayed less inclination than did the children.
Some degree of curve of Wilson should be maintained at the end of orthodontic treatment to fulfill physiologic needs and stability.
ACKNOWLEDGMENTS
The authors thank Drs Normand Boucher, Ashish Gurav, and Amirtha Hariharan for their help.
REFERENCES
- 1.Wilson GH. A Manual of Dental Prosthetics. Philadelphia, Pa: Lea & Febiger; 1911. [Google Scholar]
- 2.Monson GS. Applied mechanics to the theory of mandibular movements. Dent Cosmos. 1932;74:1039–1053. [Google Scholar]
- 3.Dempster WT, Adams WJ, Dubbles RA. Arrangement in the jaws of the roots of the teeth. JADA. 1963;67:779–797. doi: 10.14219/jada.archive.1963.0364. [DOI] [PubMed] [Google Scholar]
- 4.Andrews LF. The six keys to normal occlusion. Am J Orthod. 1972;62:296–309. doi: 10.1016/s0002-9416(72)90268-0. [DOI] [PubMed] [Google Scholar]
- 5.Marshall S, Dawson D, Southard KA, Lee AN, Casco JS, Southard TE. Transverse molar movements during growth. Am J Orthod Dentofacial Orthop. 2003;124:615–624. doi: 10.1016/s0889-5406(03)00630-9. [DOI] [PubMed] [Google Scholar]
- 6.Sayania B, Merchant M, Josephs P, Chung C-H. Changes in the buccolingual inclination of first molars with growth in untreated subjects—a longitudinal study. Angle Orthod. 2017;87:681–687. doi: 10.2319/120716-878.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Casko JS, Vaden JL, Kokich VG, et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am J Orthod Dentofacial Orthop. 1998;114:589–599. doi: 10.1016/s0889-5406(98)70179-9. [DOI] [PubMed] [Google Scholar]
- 8.Germane N, Bentley BE, Isaacson RJ. Three biologic variables modifying faciolingual tooth angulation by straight-wire appliances. Am J Orthod Dentofacial Orthop. 1989;96:312–319. doi: 10.1016/0889-5406(89)90350-8. [DOI] [PubMed] [Google Scholar]
- 9.Ross VA, Isaacson RJ, Germane N, Rubenstein LK. Influence of vertical growth pattern on faciolingual inclinations and treatment mechanics. Am J Orthod Dentofacial Orthop. 1990;98:422–429. doi: 10.1016/S0889-5406(05)81651-8. [DOI] [PubMed] [Google Scholar]
- 10.Barrera JM, Llamas JM, Espinar E, Sáenz Ramírez C, Paredes V, Pérez-Varela JC. Wilson maxillary curve analyzed by CBCT. A study on normocclusion and malocclusion individuals. Med Oral Patol Oral Cir Bucal. 2013;18:547–552. doi: 10.4317/medoral.18291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kasai K, Kawamura A. Correlation between buccolingual inclination and wear of mandibular teeth in ancient and modern Japanese. Arch Oral Biol. 2001;46:269–273. doi: 10.1016/s0003-9969(00)00106-0. [DOI] [PubMed] [Google Scholar]
- 12.Alkhatib R, Chung C-H. Buccolingual inclination of first molars in untreated adults: a CBCT study. Angle Orthod. 2017;87:598–602. doi: 10.2319/110116-786.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Masumoto T, Hayashi I, Kawamura A, Tanaka K, Kasai K. Relationships among facial type, buccolingual molar inclination, and cortical bone thickness of the mandible. Eur J Orthod. 2001;23:15–23. doi: 10.1093/ejo/23.1.15. [DOI] [PubMed] [Google Scholar]
- 14.Mitra S, Ravi MS. Evaluation of buccolingual inclination of posterior teeth in different facial patterns using computed tomography. Ind J Dent Res. 2011;22:376–380. doi: 10.4103/0970-9290.87056. [DOI] [PubMed] [Google Scholar]
- 15.Shewinvanakitkul W, Hans MG, Narendran S, Palomo MJ. Measuring buccolingual inclination of mandibular canines and first molars using CBCT. Orthod Craniofac Res. 2011;14:168–174. doi: 10.1111/j.1601-6343.2011.01518.x. [DOI] [PubMed] [Google Scholar]
- 16.Weinstein S, Haack DC, Morris LY, Snyder BB, Attaway HE. On an equilibrium theory of tooth position. Angle Orthod. 1963;33:1–26. [Google Scholar]
- 17.Brodie AG. The fourth dimension in orthodontics. Angle Orthod. 1954;24:15–30. [Google Scholar]
- 18.Moyers RE. Handbook of Orthodontics. Chicago, Ill: The Year Book Publishers; 1958. [Google Scholar]
- 19.Kohakura S, Kasia K, Ohno I, Kanazawa E. Relationship between maxillofacial morphology and morphological characteristics of vertical sections of the mandible obtained by CT scanning. J Nihon Univ School Dent. 1997;39:71–77. doi: 10.2334/josnusd1959.39.71. [DOI] [PubMed] [Google Scholar]
- 20.Dawson PE. Functional Occlusion: From TMJ to Smile Design. St Louis, Mo: Mosby; 2007. [Google Scholar]
- 21.Nanda R. Biomechanics and Esthetic Strategies in Clinical Orthodontics. St Louis, Mo: Elsevier Saunders; 2005. [Google Scholar]
- 22.Okeson JP. Management of Temporomandibular Disorders and Occlusion, 7th ed. St Louis, Mo: Elsevier Saunders; 2012. [Google Scholar]
- 23.Janson G, Bombonatti R, Cruz KS, Hassunuma CY, Del Santo M., Jr Buccolingual inclinations of posterior teeth in subjects with different facial patterns. Am J Orthod Dentofacial Orthop. 2004;125:316–322. doi: 10.1016/j.ajodo.2003.03.010. [DOI] [PubMed] [Google Scholar]
- 24.Tsunori M, Masamitsu M, Kasai K. Relationship between facial types and tooth and bone characteristics of the mandible obtained by CT scanning. Angle Orthod. 1998;68:557–562. doi: 10.1043/0003-3219(1998)068<0557:RBFTAT>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.Andrews LF. Straight Wire: The Concept and the Appliance. San Diego, Calif: L. A. Wells; 1989. [Google Scholar]
- 26.Dellinger EL. A scientific assessment of the straight-wire appliance. Am J Orthod. 1978;73:290–299. doi: 10.1016/0002-9416(78)90135-5. [DOI] [PubMed] [Google Scholar]
- 27.Andrews LF, Andrews WA. The six elements of orofacial harmony. Andrews J. 2000;1:13–22. [Google Scholar]
- 28.McNamara JA, Brudon WL, Kokich VG. Orthodontics and Dentofacial Orthopedics. Ann Arbor, Mich: Needham; 2001. [Google Scholar]


