Abstract
Objectives:
To investigate the influence of cheek volume on facial esthetics judged by orthodontists and non-specialists.
Materials and Methods:
A 25-year-old female's natural and smiling face was captured by 3D stereophotogrammetry. Cheek volume of the 3D image was altered to different degrees three-dimensionally. For the natural and smiling face, seven groups of facial images were created: decreased grade I/II/III, increased grade I/II/III, and the original one. Thirty orthodontists and 30 nonspecialists were invited to perform esthetic evaluation of the original and transformed images using a questionnaire. Data were calculated with one-way analysis of variance (least significant difference test) and independent samples t test.
Results:
Compared to nonspecialists, orthodontists gave lower esthetic scores to the decreased grade III facial images (maximum deformation degree: 7.500 mm and 7.327 mm in natural and smiling face-oriented image groups, respectively). The decreased grade III facial images also received the highest age ranks. However, the increased grade III facial images received the lowest scores and highest age ranks from nonspecialists (maximum deformation degree: 6.994 mm and 5.300 mm in natural and smiling face-oriented image groups, respectively) (P < .01).
Conclusions:
Orthodontists and nonspecialists showed different esthetic evaluation of varied cheek volume. The influence of cheek volume in orthodontic diagnostic analysis needs further consideration.
Keywords: 3D stereophotogrammetry, Esthetics
INTRODUCTION
Enhanced esthetic appearance is consistently an objective of orthodontic treatment. Seeking a better dentofacial appearance has been reported to have a strong influence on a patients' decision to start orthodontic treatment.1–3 Patient satisfaction was shown to be associated with perceived esthetic outcome.4 The perspective of facial esthetics may vary among individuals but previous studies showed that balanced facial proportion5–7 and a harmonious dentolabial relationship at relaxed lip posture and in the full smile was generally preferred.8 It may be said that orthodontic treatment for esthetic reasons is a sign of the times and, recently, orthodontists have become more and more focused on developing treatment plans for improvement of facial esthetics.9
With the introduction of cephalometrics, normal measurements between dentofacial structures and facial soft tissues have been established in recent decades.10,11 This provided orthodontists with access to abundant information to use for concrete treatment planning and to achieve more predictable treatment outcomes. The soft tissue-oriented treatment approach has been advocated for current orthodontic practice.12 Physiologic characteristics of soft tissue changes with growth and morphologic improvements of the soft tissues produced by orthodontic treatment have been studied using cephalometrics.13 It is noteworthy that the information presented using cephalometrics is about the profile.
Recently, some patients have expressed their concerns about unpleasant soft tissue changes in the cheek area that cannot be presented by cephalometrics. They were worried about the “orthodontic face” as quoted from social media and the social network.14 The so-called “orthodontic face” features the loss of cheek volume and consequently high cheekbones. The cheek is critical when evaluating a face. Plastic surgeons believe that cheek volume is an important determinant of facial beauty and youthful appearance.11 Using a 3D imaging system, changes in the cheek were found after orthognathic surgery consisting of preoperative orthodontic treatment and maxillomandibular transverse osteodistraction.15,16 Since, the current analysis of soft tissues in orthodontics is primarily based on two-dimensional images,17–19 there is little evidence available on how cheek volume, a three-dimensional variable, might influence perception of facial esthetics in orthodontic practice.
Three-dimensional (3D) stereophotogrammetry is an innovative method for collecting clinical data. It features easy and quick data collection, noninvasive image capture, and quantified data which can be extracted as x, y, z coordinate data for future analysis.20 With images taken by 3D stereophotogrammetry and computer image processing, the dimensional transformation of cheek volume can be manipulated digitally. In this study, the influence of varied cheek volume on facial esthetics was investigated in orthodontists and nonspecialists. The purpose was to explore the potential value of including cheek volume in orthodontic diagnostic analysis.
MATERIALS AND METHODS
Ethical approval was granted by the local institutional research ethical board (WCHSIRB-ST-2016-086). 3D stereophotogrammetry (3dMDface system, 3dMD Inc., Atlanta, Ga) was used to capture both natural and smiling facial images of the model in natural head position. A 25-year-old female was chosen as the model. The inclusion criteria of the model were as follows: (1) average growth pattern; (2) no facial deformity; (3) acceptable cheek volume without discernible volume loss; and (4) no history of plastic surgery.
Cheek area was defined with four distinct facial landmarks: the outer limit as the tragus; the inner border as the nasolabial groove; the upper limit to the infraorbital margin and zygomatic arch; and the lower extended to the inferior region of the mandible.21 The trend of soft tissue deformation was assumed to satisfy the Gaussian distribution (Figure 1A):22,23
|
.
|
Figure 1.
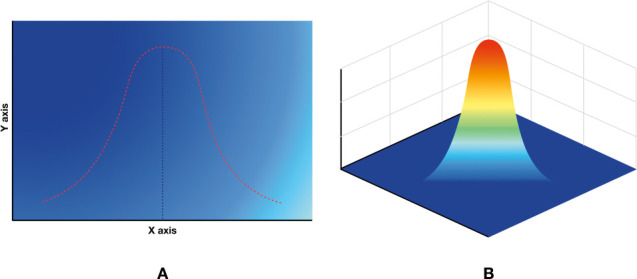
An illustration of Gaussian distribution (A); the Gaussian distribution in a 3D manner (B) in which the selected point had the largest deformation and gradually diminished around.
The point selected was deformed and then gradually diminished around, which could be viewed in accordance with the Gaussian distribution in a 3D manner (Figure 1B). The shape of the Gaussian distribution curve could be controlled based on μ and σ2, thus controlling the contour of deformation. Layers were provided to control the extent of deformation. Convex and concave parameters were presented to select the direction of deformation.
Volume transformation was within the defined cheek area. After exporting the image in .obj format in the novel software designed for this study, grid data were chosen to execute transformation. By adjusting the contours, layers, and parameters, the patterns of deformation were set as desired. A convex parameter (above the black bar) resulted in increased cheek volume, while a concave parameter (below the black bar) generated decreased cheek volume (Figure 2A). Combinations of different deformation patterns were adopted occasionally to make the transformed facial images vivid. Then, transformed 3D images were superimposed on the original to ensure the transformation was limited to the defined cheek area (Figure 2B). In this research, there were three groups of images with increased cheek volume and three groups of images with decreased cheek volume derived from the natural and smiling face. Original and transformed images were imported to the 3dMD face system to acquire images in a unified head position. Color-coded mapping was used to show the quantitative deformation (Figure 2C).24,25 All 3D facial images in this study are presented in Figures 3–7. Each set of images included views of the front, the oblique, and the profile.
Figure 2.
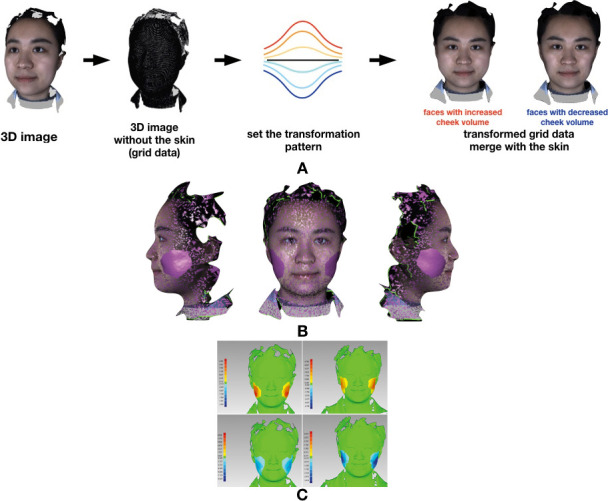
An illustration of cheek volume transformation: an original 3D facial image was shown in grid data, and then transformation of cheek volume was conducted according to varied transformation patterns (A); transformed faces were superimposed on the original to ensure the deformation was limited to the defined cheek area (B); color-coded mapping showed the measurable deformation degrees; warm-toned bar represents dimensionally convex deformation to increase cheek volume, while cold-toned bar represents dimensionally concave deformation to decrease cheek volume (mm) (C).
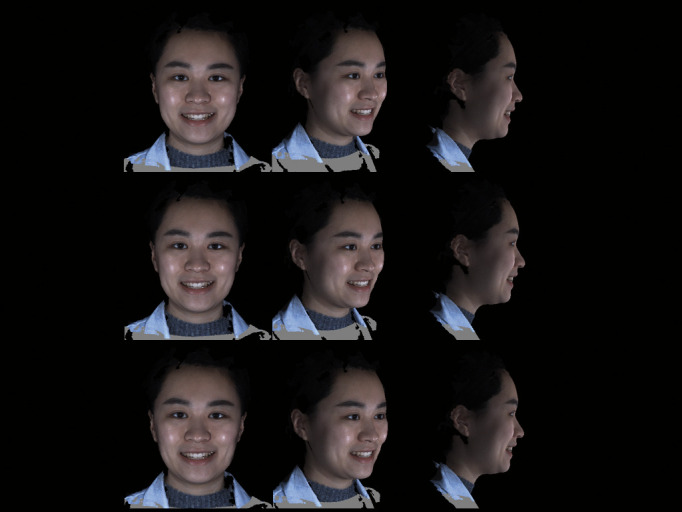
Figure 3.

Original 3D images, natural face and smiling face (from top to bottom).
Figure 7.
Smiling faces with decreased cheek volume and the maximum deformation degree (from top to bottom): 1.519 mm (Decreased Grade I), 3.414 mm (Decreased Grade II), 7.327 mm (Decreased Grade III).
Figure 4.
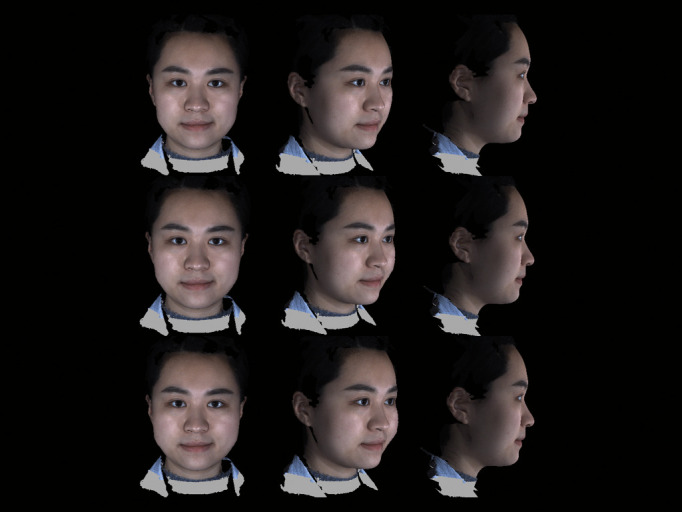
Natural faces with increased cheek volume and the maximum deformation degree (from top to bottom): 2.282 mm (Increased Grade I), 5.150 mm (Increased Grade II), 6.994 mm (Increased Grade III).
Figure 5.
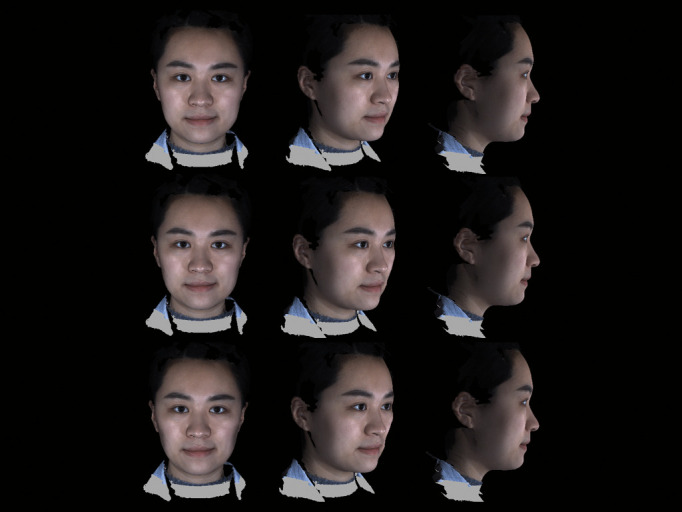
Natural face with decreased cheek volume and the maximum deformation degree (from top to bottom): 2.193 mm (Decreased Grade I), 4.480 mm (Decreased Grade II), 7.500 mm (Decreased Grade III).
Figure 6.

Smiling faces with increased cheek volume and the maximum deformation degree (from top to bottom): 1.893 mm (Increased Grade I), 4.796 mm (Increased Grade II), 5.300 mm (Increased Grade III).
A questionnaire was designed to investigate esthetic evaluation of the original and transformed facial images by orthodontists (including senior orthodontic residents) and nonspecialists who were not dentists or orthodontists. In the orthodontist group, the age of the evaluators ranged from 23 to 36 years old and the ratio of males to females was 1:2. In the nonspecialist group, the ages ranged from 17 to 52 years old and the ratio of males to females was 3:2. Within each group of natural and smiling face-oriented images, the one original image and six transformed images were presented in random order. Orthodontists and nonspecialists were asked to grade all facial images on a scale of 0 to 100, indicating the least attractive and most attractive, respectively. They were also asked to rank all images on a scale of 1 to 7 in order from the most visually youngest to the most aged.
Thirty complete questionnaires from orthodontists and nonspecialists were collected in five days. SPSS (version 22.0, IBM, Armonk, NY) was used for analysis. One-way analysis of variance (least significant difference test) was used to assess statistically significant differences between images within orthodontists and nonspecialists. Raw data were adjusted by subtracting the values of the original images (scores and ranks) from values of the transformed images to coordinate the evaluation of baseline between orthodontists and nonspecialists. The independent samples t test was used to compare the evaluation results between orthodontists and non-specialists. Classification of cheek volume deformation (maximum deformation degree) is shown in Table 1. Means and standard deviations of the scores and ranks for each image were calculated (Table 2) and P < .01 was considered statistically significant.
Table 1.
Classification and the Maximum Deformation Degree
| Groups |
Natural Face (mm) |
Smiling Face (mm) |
| Decreased grade III | 7.5 | 7.327 |
| Decreased grade II | 4.48 | 3.414 |
| Decreased grade I | 2.193 | 1.519 |
| Original image | – | – |
| Increased grade I | 2.282 | 1.893 |
| Increased grade II | 5.15 | 4.796 |
| Increased grade III | 6.994 | 5.3 |
Table 2.
Means and Standard Deviations of the Scores and Ranks for Each Image Group
| Groups |
Order of Images |
Orthodontists |
Nonspecialists |
||
| Mean |
SD |
Mean |
SD |
||
| Esthetic scores for natural-face-oriented images | |||||
| Decreased grade III | 1 | 65.23 | 13.86 | 71.17 | 12.9 |
| Decreased grade II | 7 | 75.8 | 13.61 | 72.17 | 10.53 |
| Decreased grade I | 3 | 80.97 | 9.85 | 71.53 | 10.31 |
| Original image | 5 | 82.17 | 12.68 | 75.67 | 12.62 |
| Increased grade I | 4 | 75.5 | 15.28 | 73.63 | 13.83 |
| Increased grade II | 2 | 68.83 | 12.01 | 68.13 | 11.78 |
| Increased grade III | 6 | 59.07 | 12.89 | 61.03 | 14.33 |
| Esthetic scores for smiling-face-oriented images | |||||
| Decreased grade III | 1 | 72 | 13.24 | 76.1 | 12.85 |
| Decreased grade II | 7 | 78.73 | 10.93 | 74.2 | 11.04 |
| Decreased grade I | 3 | 83.77 | 8.67 | 69.53 | 11.2 |
| Original image | 5 | 82.83 | 11.33 | 75.7 | 13.91 |
| Increased grade I | 4 | 75.93 | 12 | 69.33 | 12.84 |
| Increased grade II | 2 | 70.63 | 10.64 | 69.07 | 13.2 |
| Increased grade III | 6 | 63.17 | 10.79 | 60.87 | 13.12 |
| Age ranks for natural-face-oriented images | |||||
| Decreased grade III | 1 | 6.13 | 1.61 | 4.1 | 2.4 |
| Decreased grade II | 7 | 4.3 | 2.1 | 3.57 | 1.87 |
| Decreased grade I | 3 | 3.67 | 1.58 | 3.97 | 1.77 |
| Original image | 5 | 2.87 | 1.28 | 2.93 | 1.86 |
| Increased grade I | 4 | 3.57 | 1.48 | 3.87 | 1.78 |
| Increased grade II | 2 | 3.33 | 1.71 | 4.4 | 1.67 |
| Increased grade III | 6 | 4.13 | 2.4 | 5.3 | 1.97 |
| Decreased grade III | 1 | 5.93 | 1.78 | 3.67 | 2.26 |
| Decreased grade II | 7 | 4.8 | 1.9 | 3.9 | 2.02 |
| Decreased grade I | 3 | 3.57 | 1.61 | 4.33 | 1.71 |
| Original image | 5 | 3.23 | 1.48 | 2.67 | 1.81 |
| Increased grade I | 4 | 3.6 | 1.5 | 4.07 | 1.78 |
| Increased grade II | 2 | 2.97 | 1.71 | 4.13 | 1.5 |
| Increased grade III | 6 | 3.9 | 2.37 | 5.23 | 2.11 |
RESULTS
Orthodontists
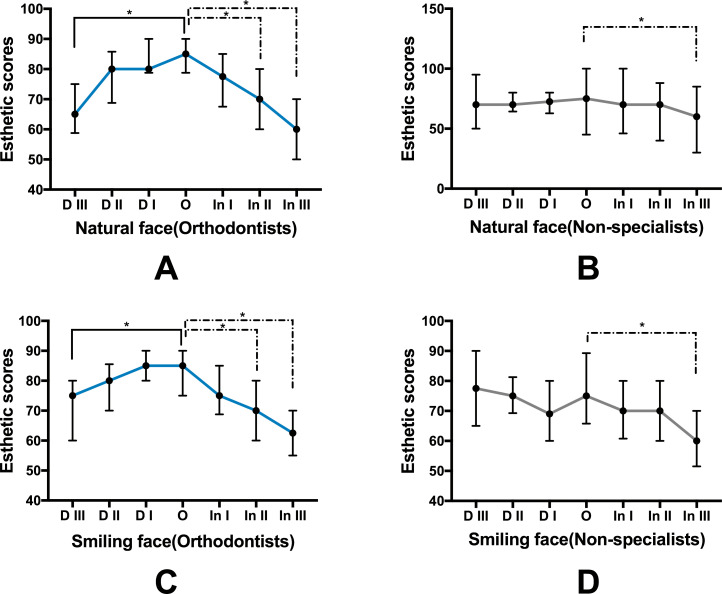
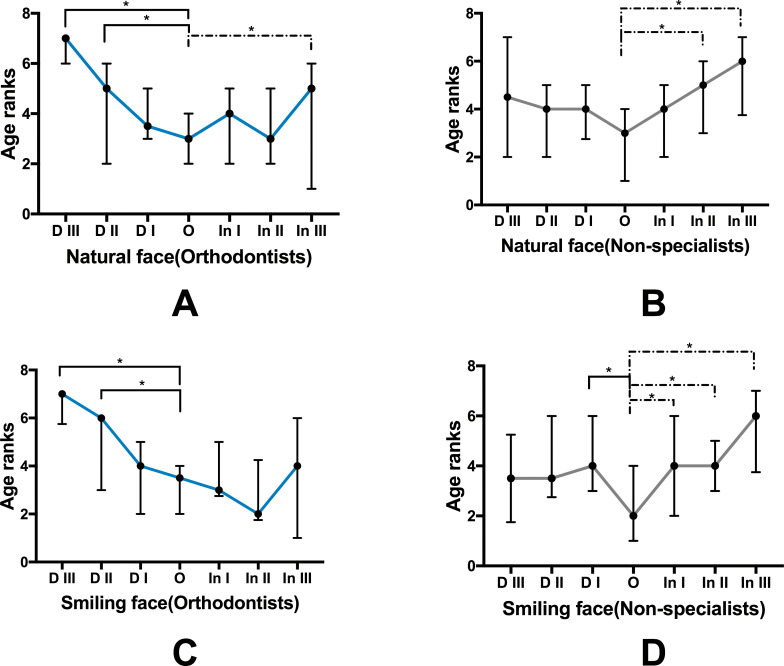
Decreased grade III images received lower esthetic scores and higher age appearance ranks (Figure 8A, 8C, 9A, 9C; P < .01). Also, decreased grade II ranked higher than other images (Figure 9A, 9C; P < .01). Increased grade II and III received lower esthetic scores (Figure 8A, 8C; P < .01).
Figure 8.
Esthetic scores for each image group (P < .01; D indicates decreased grade; In, increased grade; O, original image).
Figure 9.
Age ranks for each image group (P < .01).
Nonspecialists
Increased grade III images received lower esthetic scores and higher age appearance ranks (Figure 8B, 8D, 9B, 9D; P < .01).
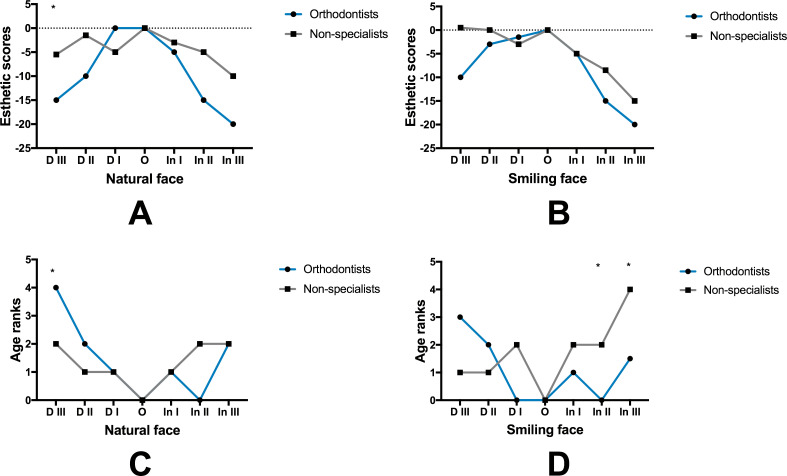
Orthodontists vs. Nonspecialists
The decreased grade III images received lower scores and higher ranks from orthodontists compared to non-specialists in the natural face-oriented image group. Nonspecialists gave increased grade II and III images higher ranks in the smiling face-oriented image group (Figure 10; P < .01).
Figure 10.
Comparison between orthodontists and nonspecialists (with adjusted data, P < .01).
DISCUSSION
Dogliotti et al. reported that maxillomandibular transverse osteodistraction (MMTOD) produced facial changes in the cheek.15 Efforts have been made to predict quantitative soft tissue deformations after orthognathic surgery. However, shortcomings existed in the prediction of the final position of the lip and cheek areas.16 In an investigation of soft tissue changes after rapid maxillary expansion (RME), the largest median increase was found in cheek projection of the prepubertal group.26 Decreased grade III images was graded as less attractive and as the most aged by orthodontist evaluators. Additionally, increased grade III images were found to be the least attractive, but there was no rank difference. In nonspecialists, increased grade III images were evaluated to be the least attractive and the most aged.
Cheek volume loss was related to facial aging in a medical esthetic evaluation.27,28 This may explain why orthodontists regarded decreased grade III images as less attractive and visually more aged compared to nonspecialists.
Interestingly, the general response of the nonspecialist group was not consistent with some patients' concerns. The nonspecialist evaluators expressed lower esthetic evaluation for increased grade III images, while the patients appear to be worried about losing cheek volume. Some patients may take the initiative to collect information about treatment outcomes by using the internet. Through social media and the social network, the concept of “orthodontic face” has been deeply engraved in their mind. This could be why such patients have special concerns; patients under treatment may sometimes complain about cheek volume loss, which is unwanted for them. In many cases, they have had extraction treatment due to bimaxillary dentoalveolar protrusion. Additionally, they may have high cheekbones and retruded mandibles. Whether patients with specific types of malocclusion or maxillofacial deformity are predisposed to certain tendencies for cheek volume change after orthodontic treatment still needs further investigation.
There was feedback from some study participants that the difference among images was subtle. Error of 3dMD face system (3dMDface system, 3dMD Inc., Atlanta, Ga) has been reported to be below 1.0 mm.29 And the 3dMD stereophotogrammetry scanner has been proven as a valid and reliable tool to measure volumetric changes in facial contours of more than 5.9 mL.30 The quantitative difference was shown by the measurement of distance in this study as it was easier to perceive by color-coded mapping. The scale of distribution and variation between these groups might be refined more delicately for more potential details. The manipulation of cheek volume in this study cannot be interpreted as the reflection of treatment outcomes. It was a simulation based on observation. Precise prediction of soft tissue changes in the cheek area remains a challenge. Additionally, classic biological factors related to esthetic evaluation include sex, age, race, etc.31 Though professional experience was shown to be an influence in this study, more comprehensive information might be gained with finer categorization of the evaluators.
Arnett believed, “We only treat what we are educated to see. The more we see, the better the treatment we render our patients.”32 It is not the orthodontist's obligation to manipulate cheek volume. However, it may not be advisable to exclude factors that could possibly upgrade overall knowledge of orthodontic diagnostic analysis. Plastic surgeons have adopted a series of descriptive and subjective scales to evaluate the cheek and mid-face, such as age-related midface volume deficit (MVD), Global Aesthetic Improvement Scale (GAIS), look and feel of the midface (LAFM), and self-perception of Age (SPA).27,33 With the emergence of advanced imaging systems, more quantitative details will continue to become accessible in treatment planning through computed tomography, magnetic resonance imaging, and 3D stereophotogrammetry.34,35 The 3D facial photographic average and 3D superimposition of individual samples to the average have been investigated and the protocol for mapping human faces in three dimensions has been established.36 But, in terms of cheek volume, a protocol of diagnostic analysis is still unavailable for orthodontic practice.
CONCLUSIONS
Orthodontists and nonspecialists show different esthetic evaluations of alterations in cheek volume.
Discrepancies exist between orthodontists and nonspecialists in perception of cheek esthetics, which needs further investigation.
The value of cheek volume in orthodontic diagnostic analysis requires more consideration.
REFERENCES
- 1.Albino JE, Cunat JJ, Fox RN, Lewis EA, Slakter MJ, Tedesco LA. Variables discriminating individuals who seek orthodontic treatment. J Dent Res. 1981;60(9):1661–1667. doi: 10.1177/00220345810600090501. [DOI] [PubMed] [Google Scholar]
- 2.Shaw WC. Factors influencing the desire for orthodontic treatment. Eur J Orthod. 1981;3(3):151–162. doi: 10.1093/ejo/3.3.151. [DOI] [PubMed] [Google Scholar]
- 3.Tedesco LA, Albino JE, Cunat JJ, Green LJ, Lewis EA, Slakter MJ. A dental-facial attractiveness scale. Part I. Reliability and validity. Am J Orthod. 1983;83(1):38–43. doi: 10.1016/0002-9416(83)90269-5. [DOI] [PubMed] [Google Scholar]
- 4.Pacheco-Pereira C, Pereira JR, Dick BD, Perez A, Flores-Mir C. Factors associated with patient and parent satisfaction after orthodontic treatment: a systematic review. Am J Orthod Dentofacial Orthop. 2015;148(4):652–659. doi: 10.1016/j.ajodo.2015.04.039. [DOI] [PubMed] [Google Scholar]
- 5.Rhodes G. The evolutionary psychology of facial beauty. Annu Rev Psychol. 2006;57:199–226. doi: 10.1146/annurev.psych.57.102904.190208. [DOI] [PubMed] [Google Scholar]
- 6.Giddon DB. Orthodontic application of psychological and perceptual studies of facial esthetics. Semin Orthod. 1995;1(2):82–93. doi: 10.1016/s1073-8746(95)80095-6. [DOI] [PubMed] [Google Scholar]
- 7.Dahlia W, Zaidel SMA, Kiran Baig et al. Appearance of symmetry, beauty, and health in human faces. Brain Cogn. 2005;57:261–263. doi: 10.1016/j.bandc.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 8.Mack MR. Perspective of facial esthetics in dental treatment planning. J Prosthet Dent. 1996;75(2):169–176. doi: 10.1016/s0022-3913(96)90095-5. [DOI] [PubMed] [Google Scholar]
- 9.Kiekens RM, Maltha JC, van't Hof MA, Kuijpers-Jagtman AM. Objective measures as indicators for facial esthetics in white adolescents. Angle Orthod. 2006;76(4):551–556. doi: 10.1043/0003-3219(2006)076[0551:OMAIFF]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Scheideman GB, Bell WH, Legan HL, Finn RA, Reisch JS. Cephalometric analysis of dentofacial normals. Am J Orthod. 1980;78(4):404–420. doi: 10.1016/0002-9416(80)90021-4. [DOI] [PubMed] [Google Scholar]
- 11.Bergman RT. Cephalometric soft tissue facial analysis. Am J Orthod Dentofacial Orthop. 1999;116(4):373–389. doi: 10.1016/s0889-5406(99)70222-2. [DOI] [PubMed] [Google Scholar]
- 12.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics 5th ed. Maryland Heights, Mo: Mosby; 2012. [Google Scholar]
- 13.Turley PK. Evolution of esthetic considerations in orthodontics. Am J Orthod Dentofacial Orthop. 2015;148(3):374–379. doi: 10.1016/j.ajodo.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 14.Yuan J, Weipeng L, Yan Y, Shuai W, Yu L, Zhihe Z. The effects of orthodontic treatment on cheek fullness in adult women. Chin J Orthod. 2015;22(1):24–27. [Google Scholar]
- 15.Bianchi FA, Gerbino G, Corsico M, Schellino E, Barla N, Verze L. Soft, hard-tissues and pharyngeal airway volume changes following maxillomandibular transverse osteodistraction: Computed tomography and three-dimensional laser scanner evaluation. J Craniomaxillofac Surg. 2017;45:47–55. doi: 10.1016/j.jcms.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 16.Nadjmi N, Defrancq E, Mollemans W, Hemelen GV, Berge S. Quantitative validation of a computer-aided maxillofacial planning system, focusing on soft tissue deformations. Ann Maxillofac Surg. 2014;4:171–175. doi: 10.4103/2231-0746.147112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Anic-Milosevic S, Lapter-Varga M, Slaj M. Analysis of the soft tissue facial profile by means of angular measurements. Eur J Orthod. 2008;30(2):135–140. doi: 10.1093/ejo/cjm116. [DOI] [PubMed] [Google Scholar]
- 18.Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofacial Orthop. 1993;103(4):299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 19.Scavone H, Jr, Trevisan H, Jr, Garib DG, Ferreira FV. Facial profile evaluation in Japanese-Brazilian adults with normal occlusions and well-balanced faces. Am J Orthod Dentofacial Orthop. 2006;129(6):e721–725. doi: 10.1016/j.ajodo.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 20.Nord F, Ferjencik R, Seifert B, et al. The 3dMD photogrammetric photo system in cranio-maxillofacial surgery: Validation of interexaminer variations and perceptions. J Craniomaxillofac Surg. 2015;43(9):1798–1803. doi: 10.1016/j.jcms.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 21.Papel ID, Frodel JL, Holt GR, Larrabee WF, Nachlas NE, Park SS, Sykes JM. Facial Plastic and Reconstructive Surgery 4th ed. Stuttgart, Germany: Thieme; 2016. [Google Scholar]
- 22.Wang L, Zhang H, He K, Chang Y, Yang X. Active contours driven by multi-feature Gaussian distribution fitting energy with application to vessel segmentation. PLoS One. 2015;10(11):e0143105. doi: 10.1371/journal.pone.0143105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Biktashev VN. A simple mathematical model of gradual Darwinian evolution: emergence of a Gaussian trait distribution in adaptation along a fitness gradient. J Math Biol. 2014;68(5):1225–1248. doi: 10.1007/s00285-013-0669-3. [DOI] [PubMed] [Google Scholar]
- 24.Hyoung-Seon Baik S-YK. Facial soft-tissue changes in skeletal Class III orthognathic surgery patients analyzed with 3-dimensional laser scanning. Am J Orthod Dentofacial Orthop. 2010;138:167–178. doi: 10.1016/j.ajodo.2010.02.022. [DOI] [PubMed] [Google Scholar]
- 25.Meulstee J, Liebregts J, Xi T, et al. A new 3D approach to evaluate facial profile changes following BSSO. J Craniomaxillofac Surg. 2015;43:1994–1999. doi: 10.1016/j.jcms.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 26.Glaser DA, Kenkel JM, Paradkar-Mitragotri D, Murphy DK, Romagnano L, Drinkwater A. Duration of effect by injection volume and facial subregion for a volumizing hyaluronic acid filler in treating midface volume deficit. Dermatol Surg. 2015;41(8):942–949. doi: 10.1097/DSS.0000000000000416. [DOI] [PubMed] [Google Scholar]
- 27.Jang MS, Kim HY, Dhong HJ, Chung SK, Hong SD, Cho HJ. An analysis of Asian midfacial fat thickness according to age group using computed tomography. J Plast Reconstr Aesthet Surg. 2015;68(3):344–350. doi: 10.1016/j.bjps.2014.10.037. [DOI] [PubMed] [Google Scholar]
- 28.Torun GS. Soft tissue changes in the orofacial region after rapid maxillary expansion: A cone beam computed tomography study. J Orofac Orthop. 2017;78:193–200. doi: 10.1007/s00056-016-0074-9. [DOI] [PubMed] [Google Scholar]
- 29.Nord F, Ferjencik R, Seifert B, et al. The 3dMD photogrammetric photo system in cranio-maxillofacial surgery: Validation of interexaminer variations and perceptions. J Craniomaxillofac Surg. 2015;43:1798. doi: 10.1016/j.jcms.2015.08.017. [DOI] [PubMed] [Google Scholar]
- 30.van der Meer WJ, Dijkstra PU, Visser A, Vissink A, Ren Y. Reliability and validity of measurements of facial swelling with a stereophotogrammetry optical three-dimensional scanner. Br J Oral Maxillofac Surg. 2014;52(10):922–927. doi: 10.1016/j.bjoms.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 31.Liew S, Wu WT, Chan HH, et al. Consensus on changing trends, attitudes, and concepts of Asian beauty. Aesth Plast Surg. 2016;40:193–201. doi: 10.1007/s00266-015-0562-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Arnett GW, Bergman RT. Facial keys to orthodontic diagnosis and treatment planning. Part I. Am J Orthod Dentofacial Orthop. 1993;103(4):299–312. doi: 10.1016/0889-5406(93)70010-L. [DOI] [PubMed] [Google Scholar]
- 33.Few J, Cox SE, Paradkar-Mitragotri D, Murphy DK. A multicenter, single-blind randomized, controlled study of a volumizing hyaluronic acid filler for midface volume deficit: patient-reported outcomes at 2 years. Aesthet Surg J. 2015;35(5):589–599. doi: 10.1093/asj/sjv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fontdevila J, Serra-Renom JM, Raigosa M, et al. Assessing the long-term viability of facial fat grafts: an objective measure using computed tomography. Aesthet Surg J. 2008;28(4):380–386. doi: 10.1016/j.asj.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Mailey B, Baker JL, Hosseini A, et al. Evaluation of facial volume changes after rejuvenation surgery using a 3-dimensional camera. Aesthet Surg J. 2016;36(4):379–387. doi: 10.1093/asj/sjv226. [DOI] [PubMed] [Google Scholar]
- 36.Nanda V, Gutman B, Bar E, et al. Quantitative analysis of 3-dimensional facial soft tissue photographic images: technical methods and clinical application. Prog Orthod. 2015;16:21. doi: 10.1186/s40510-015-0082-0. [DOI] [PMC free article] [PubMed] [Google Scholar]