Abstract
Objectives:
To assess patient compliance and treatment efficacy of preventive expansion treatment with removable Planas functional appliances using an integrated microsensor.
Materials and Methods:
Wear time (WT) and behavior of 69 patients undergoing treatment with Planas functional appliances were assessed and analysed using TheraMon microsensors (Gschladt, Hargelsberg, Austria). Patients were followed up for a period of 9 months, and visits were made every 3 months to download WT data from the microsensor and to assess wearing behavior. From individual WT graphs,10 parameters were derived to characterize compliance for each patient. Treatment efficacy was measured by eight parameters determining the level of expansion after 9 months of treatment.
Results:
Patients wore their device on average 15.8 ± 5.2 h/d. WT was unrelated to age and gender, but it was positively influenced by patient habits when keeping appliances during eating, sports, care and handling. Treatment efficacy in terms of intercanine and intermolar expansion was 4.4 ± 1.9 mm and 4.6 ± 2.0 mm for the maxilla, and 5.3 ± 2.0 mm and 4.7 ± 2.3 mm for the mandible, respectively. Efficacy was negatively affected by poor compliance (WT < 9 h/d) and by high variability of within-subject WT recordings.
Conclusions:
Perfect compliance is not necessary to achieve treatment success, but patients should exhibit sufficient wear time to allow maxillary expansion to occur. The TheraMon microsensor offers a new perspective and aid to individualize treatment prescriptions.
Keywords: Compliance, Microsensor, Functional appliances
INTRODUCTION
Early orthodontic treatment with removable appliances is intended to prevent dentofacial unbalance in the mixed dentition and to reduce the overall need for later complex orthodontic treatment with fixed appliances. Interceptive treatment is based on the principle that correction should be performed before an abnormality has fully developed.1–3 This idea was supported by King et al.4 when they focused on the perception of early treatment benefits. The use of a Planas functional device, based on the overall rehabilitation of the stomatognathic system using neuro-occlusal rehabilitation,5,6 constitutes an effective way to correct early abnormality, including maxillary and mandibular overcrowding in the mixed dentition.7
The success of early orthodontic treatment with removable appliances is highly dependent on patient compliance,8 defined as the extent to which the patient's behavior matches the practitioner's recommendations.9 Witt et al.10 described some factors that determined the patient's compliance, such as regimen, perceived comfort, patient personality, and parental attitudes, but many other influencing factors have been reported in the literature.11–14
Several methods exist to assess compliance,11,15,16 but most are subjective and tend to overestimate wear time (WT).15,17 Today, WT can be reliably measured by temperature-sensitive microsensors incorporated in the removable appliance by polymerization; the TheraMon sensor18,19 (TheraMon System; Gschladt, Hargelsberg, Austria) is widely used for its reliability and ergonomics.20
The aim of the present study was to assess patient compliance in preventive expansion treatment with removable Planas functional appliances. The primary objective was to estimate WT with TheraMon microsensors. The secondary objective was to establish how WT impacted treatment efficacy.
MATERIALS AND METHODS
Experimental Design and Study Population
This was a prospective single-center study designed to evaluate patient compliance in early orthodontic treatment with a Planas removal functional appliance. Eligible patients were recruited sequentially between January and July 2016 (6 months) among all admissions to the Orthodontics Department of University Hospital of Liege, Liege, Belgium. The inclusion criteria were (1) patients requiring maxillary and mandibular expansion (both arches) by Planas functional appliances, (2) patients with primary or mixed dentition, (3) good general health (American Society of Anesthesiologists I or II), and (4) adequate dento-oral health (ie, treated caries, absence of periodontal diseases). The exclusion criteria were: (1) mental or motor disabilities; (2) permanent dentition, and (3) previous orthodontic treatment.
Alginate impressions (Cavex Colorchange, Cavex Holland, BV, Haarlem, Netherlands), orthopantograms, lateral cephalograms (Planmeca Inc Helsinki, Finland), and extra- and intraoral photographs were performed to collect the orthodontic data. Space analyses were performed on study models using a digital caliper.
TheraMon microsensors have a weight of 0.40 ± 0.01 g, a length of 13.0 ± 0.1 mm, a width of 9.0 ± 0.1 mm, and a height of 4.3 ± 0.1 mm (Figure 1). They measure the intraoral temperature at 15-minute intervals and are designed to capture data for a period of approximately 100 consecutive days. The temperatures recorded by the sensors were transferred electronically to the unloading TheraMon station and converted into WT by the TheraMon software (TheraMon software, version 2.1.0.13; Handelsagentur Gschladt, Austria) (Figure 2). The software also provided easy visualization and analysis of the data as WT daily graphs.
Figure 1.
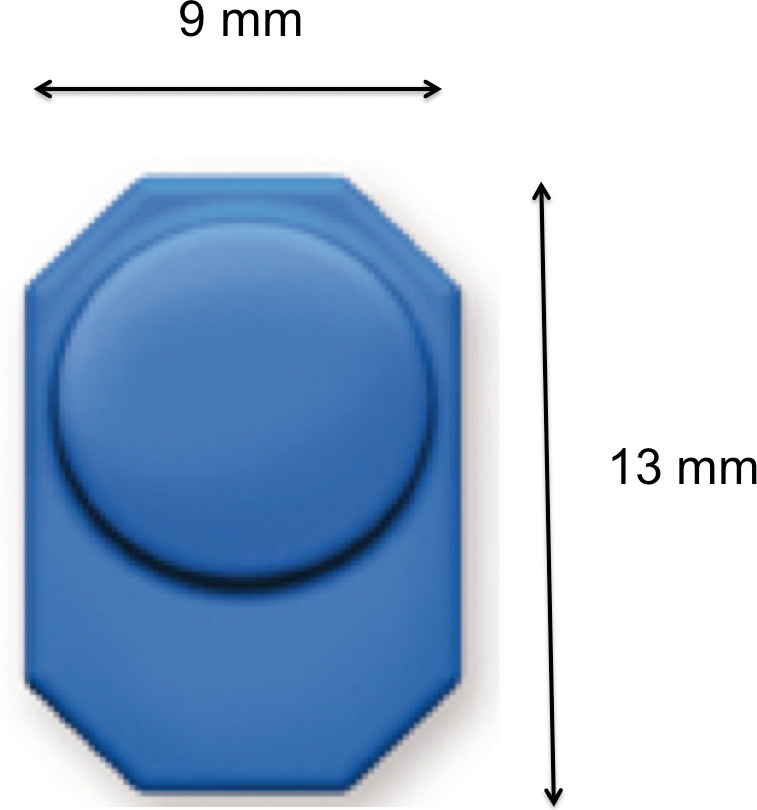
A tiny device (13 mm × 9 mm × 4.5 mm) that can be inserted in most orthodontic appliances.
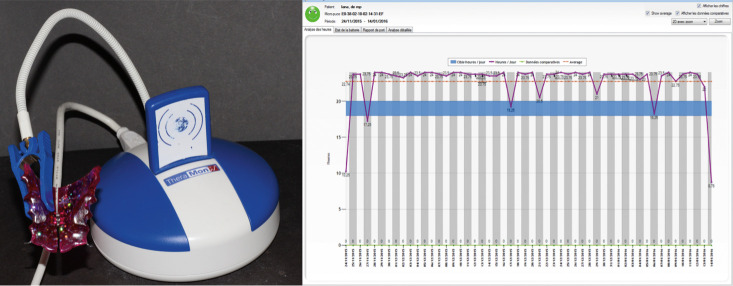
Figure 2.
Unloading TheraMon station and daily wear time values from the TheraMon microsensor software diagram (mean wear is shown by the dotted line, the blue bar signifies the prescription, and the unit of the x-axis is days).
Orthodontic Procedures
An independent Belgian laboratory produced Planas appliances for all patients. Based on alginate impressions, Planas appliances were designed as upper and lower removable resin plates with transverse expansion screws and resin tracks parallel to the Camper plane. The upper and lower plates were stabilized through raised areas between the canines and the lateral incisors and other raised areas distal to the first molar. The microsensors were fitted into the Planas appliances at the end of the process to avoid overheating (Figure 3). After placement, patients were asked to activate the transverse expansion screws every week and wear the Planas appliance 24 h/d, removing it for toothbrushing only. Patients were allowed to eat and play sports with or without the appliance. Patients were followed up for a period of 9 months and assessed at 3-month visits where data were downloaded from the device and graphically displayed as daily WT values.
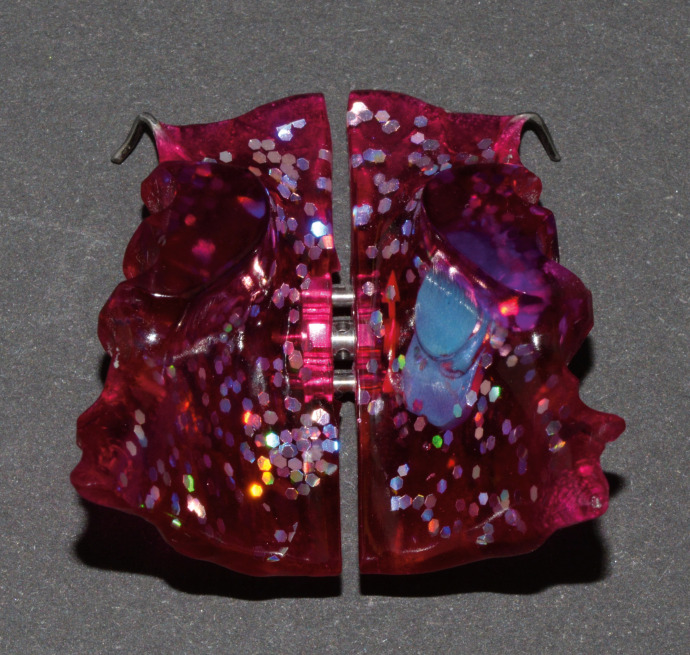
Figure 3.
Planas functional device with TheraMon microsensors.
Ten parameters were derived from the individual WT graph to characterize patient compliance: (1) number of daily WT recordings during the 9-month treatment period; (2) average daily WT values (hours); (3) standard deviation (SD) of daily WT values (hours); (4) relative dispersion of daily WT values expressed by the coefficient of variation (%), which was defined as coefficient of variation = SD/mean × 100%; (5) the area under the WT curve (hours × days); (6) area under the curve for WT > 15 h/d (hours × days); (7) persistence (duration) under the curve of WT > 15 hours (days); (8) the area under the curve for WT < 9 h/d (hours × days); (9) persistence under the curve of WT < 9 hours (days); and (10) the number of WT holidays (ie, number of days for which WT = 0). WT curves were obtained by simple linear interpolation between consecutive recordings (Figure 4).
Figure 4.
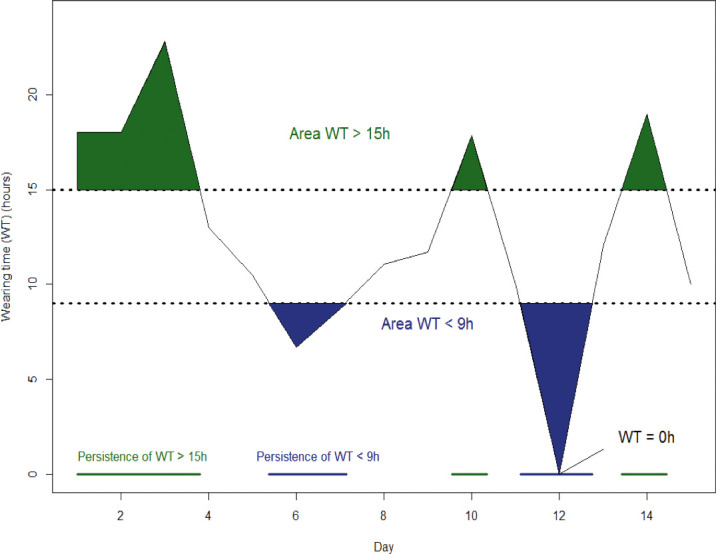
Area and persistence below 9 h/d and above 15 h/d with respect to the wear-time response curve obtained by linear interpolation between successive recordings.
Treatment efficacy was measured by eight parameters determining the level of expansion after 9 months of treatment as follows: (1) maxillary final gap opening (mm), (2) mandibular final gap opening (mm), (3) change in maxillary intercanine distance (mm), (4) change in mandibular intercanine distance (mm), (5) change in maxillary intermolar distance (mm), (6) change in mandibular intermolar distance (mm), (7) change of angulation of 16 (°), and (8) change of angulation of 26 (°).
Three questions were asked to assess patient habits: (1) eating with appliances (yes/no), (2) playing sports with appliances (yes/no), and (3) preference of wearing (day or night). Care and handling were assessed by the presence of tartar (yes/no) on the appliances. The presence of parents at each visit was recorded (yes/no).
Statistical Analysis
A power calculation showed that a sample size of at least 61 patients was necessary to estimate the mean daily WT with a statistical precision of 1 hour at the 95% confidence level assuming an SD of 4 hours for the distribution of WT. The results were expressed as the mean and SD for quantitative variables and as numbers and percentages for categoric findings. The association between variables was measured by the correlation coefficient. To compare mean values before and after treatment, the Student's paired t-test was used. The effect of patient characteristics and treatment on WT values was assessed by linear regression and expressed by the regression coefficient with standard error. The eight treatment outcomes were combined by principal component analysis and summarized by two weighted scores called principal components (PC1 and PC2) used in subsequent analyses. This allowed us to obtain a simpler treatment efficacy measure to be correlated with compliance parameters. The results were considered significant at the 5% critical level (P < .05). All calculations were performed with SAS (version 9.4) SAS Institute Inc., Cary, NC, USA.
RESULTS
During the recruitment period, 69 patients (37 boys and 32 girls) were eligible to enter the study. Their mean age was 7.8 ± 1.1 years. The space analysis of the study models revealed a mean crowding of 5.7 ± 2.8 mm in the maxilla and 4.0 ± 2.6 mm in the mandible (Table 1). About 65% of patients removed appliances during lunch and 70% removed them during sports; 58% of patients preferred to wear them at night rather than during the day. Tartar on the appliances was noted in 50% of the study subjects. For 80% of patients, parents were present.
Table 1.
Patient Characteristics
| Variables |
Mean ± SD |
| Age (y) | 7.8 ± 1.1 |
| Gender, no. (%) | |
| Female | 32 (46%) |
| Male | 37 (54%) |
| Space analysis (mm) | |
| Maxilla | –5.7 ± 2.8 |
| Mandible | –4.0 ± 2.6 |
The compliance parameters could not be measured for 10 patients (dropouts, equipment failure, problems in downloading and/or reading data, outliers, and gross blunders) leaving 59 patients for the analysis. The mean number of daily recordings per patient (ie, days of monitoring) was equal to 224 ± 45. As seen in Table 2, patients wore their device on average 15.8 ± 5.2 h/d. Specifically, 12% wore their device less than 9 h, 36% between 9 hours and 15 hours, and 52% more than 15 h/d. The SD of the individual WT was 4.2 ± 1.3 h/d and the coefficient of variation was 38% ± 49%, indicating a large variability of WT within patients. On average, the area under the WT curve was 3462 ± 1255 hours × days. The area under the curve for WT < 9 hours was 40 ± 58 hours × days with a corresponding persistence of 26 ± 45 days, while the area under the curve for WT >15 hours and the corresponding persistence were 626 ± 584 hours × days and 123 ± 74 days, respectively. The number of WT holidays was 27 ± 41 days during the study period. No correlation was found between WT and age, gender, or crowding. WT was positively influenced by eating (P < .0001) and playing sports (P = .0002) with the appliance and by care and handling (P = .023). There was no difference in WT according to the preference of day or night wearing (P = .089) or the presence of the parents (P = .34). WT values were comparable during weekends and weekdays.
Table 2.
Distribution of Compliance Parameters in 59 Patients With Planas Functional Appliances With TheraMon Microsensors and Relationship (Regression Coefficient ± SE) With Treatment Outcome Obtained by the First Principal Componenta
| Parameter of Compliance |
Mean ± SD |
Coefficient ± SE |
P Value |
| No. of daily WT recordings/patient | 224 ± 45 | –0.004 ± 0.006 | .48 |
| Mean daily WT (h) | 15.8 ± 5.2 | 0.14 ± 0.050 | .0094 |
| SD daily WT (h) | 4.2 ± 1.3 | –0.35 ± 0.20 | .085 |
| Coefficient of variation daily WT (%) | 38 ± 49 | –0.033 ± 0.0095 | .0011 |
| Area under WT curve (hours × days) | 3462 ± 1255 | 0.0004 ± 0.0002 | .070 |
| Area WT > 15 h/d (hours × days) | 626 ± 584 | 0.0005 ± 0.0004 | .24 |
| Duration WT > 15 h/d (days) | 123 ± 74 | 0.0053 ± 0.0035 | .14 |
| Area WT < 9 h/d (hours × days) | 40.2 ± 57.9 | –0.013 ± 0.0041 | .0049 |
| Duration WT < 9 h/d (days) | 25.8 ± 45.2 | –0.019 ± 0.0056 | .0014 |
| No. of days WT = 0 | 26.9 ± 40.9 | –0.020 ± 0.0082 | .025 |
WT indicates wear time.
As seen in Table 3, after the 9-month treatment period, intercanine and intermolar expansion reached 4.4 ± 1.9 mm and 4.6 ± 2.0 mm for the maxilla and 5.3 ± 2.0 mm and 4.7 ± 2.3 mm for the mandible, respectively. The final maxillary and mandibular gap openings were 5.5 ± 1.8 (>5 mm for 61% of the patients) and 5.3 ± 1.8 mm (>5 mm for 50% of the patients). The changes of angulation at 16° and 26° were also significant. As most treatment outcomes were highly correlated, they were linearly combined by principal component analysis and reduced to two weighted components (PC1 and PC2), which explained approximately 70% (49% for PC1 and 21% for PC2) of the total variability. Since weights associated with each outcome in PC1 were positive, PC1 was viewed as an averaged global efficacy score with high (low) values indicating high (low) efficacy. In PC2, weights were negative for maxillary features and positive for mandibular features, representing a contrast between maxilla and mandible. As seen in Table 2, PC1 (global efficacy score) increased with mean daily WT (P = .0094) but decreased with WT variability measured by the coefficient of variation (P = .0011), area (P = .0049) and persistence of WT <9 hours (P = .0014), and with WT holidays (P = .025). Interestingly, the area and persistence of WT values >15 hours did not influence treatment outcome. No association was found between compliance parameters and the second principal component.
Table 3.
Characteristics and Parameters of Treatment Efficacy Between Baseline and After 9 Months
| Parameters of Treatment Efficacy |
Mean ± SD |
P Value |
| Maxillary final gap opening (mm) | 5.5 ± 1.8 | |
| Mandible final gap opening (mm) | 5.3 ± 1.8 | |
| Change in maxillary intercanine distance (mm) | 4.4 ± 1.9 | <.0001 |
| Change in mandible intercanine distance (mm) | 4.6 ± 2.0 | <.0001 |
| Change in maxillary intermolar distance (mm) | 5.3 ± 2.0 | <.0001 |
| Change in mandible intermolar distance (mm) | 4.7 ± 2.3 | <.0001 |
| Change in 16° angle | 5.4 ± 3.5 | <.0001 |
| Change in 26° angle | 5.7 ± 3.6 | <.0001 |
DISCUSSION
The objective of the study was to assess patient compliance in early orthodontic treatment by Planas removal appliance. The TheraMon sensor is the most recent wear time microsensor electronic device developed to measure the wear time of removable orthodontic appliances. It demonstrated an intuitive and easy utilization according to previous studies.19–21 The TheraMon microsensors provided an objective, reliable and accurate assessment of patient compliance.
In this study, over half of the patients wore their device at least 15 h/day with moderate variability and almost no WT gaps. Schott et al.22 analyzed patient behavior and concluded that it was quite heterogeneous and that some patients wore their appliances on one day and not on the other.
Most previously published studies assessing patient wear times did not reach 12 h/day.22–25 While WT in the current study was lower compared to the 24 h/day prescription, on average, patients demonstrated better behavior than in previous studies. However, in terms of percentage of WT with respect to the orthodontist's prescription, the results matched those of Sahm et al.,16 namely that 50 to 60% of the WT prescription was applied by the patient. This finding demonstrated that an overstated prescription of WT is necessary to reach an adequate WT.
Wearing removal appliances during lunch and sporting activities was low. The design of Planas appliances, based on the prescription of Planas, required only raised indexed areas between the canines and the lateral incisors and distal of the first molar without Adam's clasps; this design could explain the results obtained. Considering that WT was positively influenced by eating (P < .0001) and playing sports (P = .0002) with the appliances, it would be necessary to use a perfect system of stabilization for removal appliances, e.g., Adam's clasp on molars, to enhance WT during lunch and sports.
No significant difference was found between genders as in previously published studies.15,23,25 Further, age was not identified as a significant determinant that influenced the compliance. The literature is controversial on this point. According to Tsomos et al.,25 large-scale studies are required to investigate the correlation between age and compliance.
Surprisingly, a 24 h/day WT prescription was not necessary to achieve perfect treatment efficacy; WT persistence of at least 15 h/day did not influence treatment outcome. Finally, the prescription should be adjusted to avoid WT overestimation, keeping in mind that patients wore their appliance 50–60% of the recommendation. A weak equation that consists of equilibrating an adequate wear time and the reality of the patient compliance needs to be addressed. In the present study, 9 h/day was the threshold; wearing the appliance below this limit turned out to be useless. Interestingly, the presence of the parents during the appointment did not enhance WT.
CONCLUSIONS
TheraMon microsensors offer new perspectives to assess compliance and to individualize treatment prescriptions.
On average, patients wore their appliance 15.8 h/d though 24 h/d was prescribed.
Age, gender, and presence of parents at visits did not modify compliance.
Perfect compliance was not necessary to achieve treatment efficacy.
ACKNOWLEDGMENTS
The authors are much indebted to their mentor Michel Limme, emeritus professor in orthodontics, and to Nathalie Maes for her help in data analysis.
REFERENCES
- 1.Deshayes MJ. Dentofacial orthopedics to treat facial asymmetries before six years of age. How to balance craniofacial growth and enhance temporomandibular function [in French] Orthod Fr. 2010;81:189–207. doi: 10.1051/orthodfr/2010021. [DOI] [PubMed] [Google Scholar]
- 2.Salvadori A, Cannoni P. Use and construction of the andresen activator [in French] Rev Orthop Dento Faciale. 1991;25:489–496. [PubMed] [Google Scholar]
- 3.Tausche E, Luck O, Harzer W. Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need. Eur J Orthod. 2004;26:237–244. doi: 10.1093/ejo/26.3.237. [DOI] [PubMed] [Google Scholar]
- 4.King GJ, Wheeler TT, McGorray SP, Aiosa LS, Bloom RM, Taylor MG. Orthodontists' perceptions of the impact of phase 1 treatment for class ii malocclusion on phase 2 needs. J Dent Res. 1999;78:1745–1753. doi: 10.1177/00220345990780111201. [DOI] [PubMed] [Google Scholar]
- 5.Canalda K. Homage to Pedro Planas [in French] Actual Odontostomatol (Paris) 1990;(172):561–568. [PubMed] [Google Scholar]
- 6.Planas P. Gothic arch and neuro occlusal rehabilitation [in French] Orthod Fr. 1965;36:235–244. [PubMed] [Google Scholar]
- 7.Limme M. Interception in the primary dentition: mastication and neuro-occlusal rehabilitation in French] Orthod Fr. 2006;77:113–135. doi: 10.1051/orthodfr/200677113. [DOI] [PubMed] [Google Scholar]
- 8.Casutt C, Pancherz H, Gawora M, Ruf S. Success rate and efficiency of activator treatment. Eur J Orthod. 2007;29(6):614–621. doi: 10.1093/ejo/cjm066. [DOI] [PubMed] [Google Scholar]
- 9.Witt E, Bartsch A, Sahm G. The wear-timing measuring device in orthodontics–cui bono? Reflections on the state-of-the-art in wear-timing measurement and compliance research in orthodontics [in German] J Orofac Orthop. 1991;52:117–125. doi: 10.1007/BF02173243. [DOI] [PubMed] [Google Scholar]
- 10.Witt E, Bartsch A, Sahm G, Schneider S. The determinants of wear behavior in treatment with removable orthodontic appliances [in German] J Orofac Orthop. 1992;53:322–329. doi: 10.1007/BF02311848. [DOI] [PubMed] [Google Scholar]
- 11.Bartsch A, Witt E, Sahm G, Schneider S. Correlates of objective patient compliance with removable appliance wear. Am J Orthod Dentofacial Orthop. 1993;104:378–386. doi: 10.1016/S0889-5406(05)81337-X. [DOI] [PubMed] [Google Scholar]
- 12.Mortensen MG, Kiyak HA, Omnell L. Patient and parent understanding of informed consent in orthodontics. Am J Orthod Dentofacial Orthop. 2003;124:541–550. doi: 10.1016/s0889-5406(03)00639-5. [DOI] [PubMed] [Google Scholar]
- 13.Pratt MC, Kluemper GT, Lindstrom AF. Patient compliance with orthodontic retainers in the postretention phase. Am J Orthod Dentofacial Orthop. 2011;140:196–201. doi: 10.1016/j.ajodo.2010.02.035. [DOI] [PubMed] [Google Scholar]
- 14.Sergl HG, Klages U, Zentner A. Functional and social discomfort during orthodontic treatment—effects on compliance and prediction of patients; adaptation by personality variables. Eur J Orthod. 2000;22:307–315. doi: 10.1093/ejo/22.3.307. [DOI] [PubMed] [Google Scholar]
- 15.Bos A, Kleverlaan CJ, Hoogstraten J, Prahl-Andersen B, Kuitert R. Comparing subjective and objective measures of headgear compliance. Am J Orthod Dentofacial Orthop. 2007;132:801–805. doi: 10.1016/j.ajodo.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 16.Sahm G, Bartsch A, Witt E. Micro-electronic monitoring of functional appliance wear. Eur J Orthod. 1990;12:297–301. doi: 10.1093/ejo/12.3.297. [DOI] [PubMed] [Google Scholar]
- 17.Meyer-Gutknecht H, Fritz U, Schott TC. Methods to evaluate compliance of patients with removable appliances-survey results. J Orofac Orthop. 2014;75:144–153. doi: 10.1007/s00056-013-0202-8. [DOI] [PubMed] [Google Scholar]
- 18.Schott TC, Goz G. Wearing times of orthodontic devices as measured by the theramon microsensor. J Orofac Orthop. 2011;72:103–110. doi: 10.1007/s00056-011-0014-7. [DOI] [PubMed] [Google Scholar]
- 19.Schott TC, Ludwig B, Glasl BA, Lisson JA. A microsensor for monitoring removable-appliance wear. J Clin Orthod. 2011;45:518–520. quiz 516. [PubMed] [Google Scholar]
- 20.Schott TC, Goz G. Applicative characteristics of new microelectronic sensors smart retainer(r) and theramon(r) for measuring wear time. J Orofac Orthop. 2010;71:339–347. doi: 10.1007/s00056-010-1019-3. [DOI] [PubMed] [Google Scholar]
- 21.Schott TC, Schrey S, Walter J, Glasl BA, Ludwig B. Questionnaire study of electronic wear-time tracking as experienced by patients and parents during treatment with removable orthodontic appliances. J Orofac Orthop. 2013;74:217–225. doi: 10.1007/s00056-013-0143-2. [DOI] [PubMed] [Google Scholar]
- 22.Schott TC, Ludwig B. Microelectronic wear-time documentation of removable orthodontic devices detects heterogeneous wear behavior and individualizes treatment planning. Am J Orthod Dentofacial Orthop. 2014;146:155–160. doi: 10.1016/j.ajodo.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 23.Schafer K, Ludwig B, Meyer-Gutknecht H, Schott TC. Quantifying patient adherence during active orthodontic treatment with removable appliances using microelectronic wear-time documentation. Eur J Orthod. 2015;37:73–80. doi: 10.1093/ejo/cju012. [DOI] [PubMed] [Google Scholar]
- 24.Schott TC, Fritz U, Meyer-Gutknecht H. Maxillary expansion therapy with plates featuring a transverse screw: Implications of patient compliance with wear-time and screw activation requirements. J Orofac Orthop. 2014;75:107–117. doi: 10.1007/s00056-013-0197-1. [DOI] [PubMed] [Google Scholar]
- 25.Tsomos G, Ludwig B, Grossen J, Pazera P, Gkantidis N. Objective assessment of patient compliance with removable orthodontic appliances: a cross-sectional cohort study. Angle Orthod. 2014;84:56–61. doi: 10.2319/042313-315.1. [DOI] [PMC free article] [PubMed] [Google Scholar]