Abstract
Objectives
We aimed to assess mobility patterns and reasons for high mobility among young women engaged in sex work within a randomised controlled trial to gauge how mobility may hinder access to health services and enhance HIV risk in a highly vulnerable population.
Setting
Participants were recruited from a clinic in Kampala, Uganda set up for women at high risk of HIV infection.
Participants
Adolescent girls and young women engaged in sex for money and/or commodities are at particular risk in countries with high HIV prevalence and high fertility rates. High mobility increases exposure to HIV risk. Women participants were eligible for the parent study if aged 15–24 years, HIV negative and engaged in sex work. For this substudy, 34 qualitative interviews were held with 14 sex workers (6 HIV positive, 8 HIV negative), 6 health worker/policy makers, 3 peer educators, 5 ‘queen mothers’ and 6 male partners
Measures
Participants used Google Maps to identify work venues at 12-month and 18-month study visits. We also conducted 34 interviews on mobility with: high-risk women, male partners, health workers and sex-worker managers. Topics included: distance, frequency and reasons for mobility. We used Python software to analyse mapping data.
Results
Interviews found in depth narratives describing lack of education and employment opportunities, violence, lack of agency, social, sexual and familial support networks and poverty as a complex web of reasons for high mobility among young sex workers.
Conclusions
Young women at high risk are highly mobile. Reasons for mobility impact access and retention to health services and research activities. Strategies to improve retention in care should be cognisant and tailored to suit mobility patterns.
Trial registration number
Keywords: HIV & AIDS, public health, qualitative research
Strengths and limitations of this study.
This study investigates behaviour of one of the most vulnerable populations to HIV, sexually transmitted infections (STIs) and unintended pregnancy in sub-Saharan Africa; young sex workers aged 15–24 years.
This study illuminates detailed factors that motivate young sex worker mobility over time and the potential relationships between mobility and high-risk sexual behaviour.
This study employed both qualitative and a mapping methodology using Google Maps to explore participants’ own descriptions of distance, frequency and reasons for mobility as well as mapped locations that highlight very high levels of mobility giving insight into options to inform better suited interventions.
The data gathered here are highly contextual and specific to the study population and environment; the findings may not translate to other regions of sub-Saharan Africa or elsewhere.
In this analysis, we have not combined the STI results with the mobility data.
Introduction
Adolescent girls and young women engaged in sex in exchange for money and/or commodities are at particular risk in countries with high HIV prevalence and high fertility rates.1–3 Young women may differentiate between commercial and transactional sex work based on stigma or relationship status.4 5 In some cases, sex work is the only source of family income, and in others, women use transactional sex to supplement income.6 Transactional sex may thus be situational or temporary, and associated with acute shortfalls in cash, need for school fees or food insecurity.7 8 Sex work is often socially stigmatising,9 whereas informal transactional sex may be socially accepted in some, situations, or contexts.10 Globally, female sex workers (FSW) of all ages are over 10 times more likely to be living with HIV than women in the general population.11 In sub-Saharan Africa in 2012, the average HIV prevalence among FSW was >35%,11 with 20%–40% of FSW entering sex work as adolescents with a mean age of entry of 16 years or younger.
In Uganda, about 12% of adolescent girls and young women report transactional sex.12–14 Young people in Uganda have an HIV prevalence of 3.7% nationally, yet younger female sex workers have about a four to seven times higher prevalence of HIV,15 16 with female sex workers over 15 years of age in Kampala reported to have between 33% and 37% HIV infection.17 18 In addition, female sex workers under 16 years of age, new to sex work are dramatically more vulnerable than older colleagues to violence, sexually transmitted infections (STIs) and HIV and poorer access to services.19–25 Yet, despite rising numbers of young female sex workers and their recognised vulnerability, there have been few interventions to date that have targeted this group.3 25
Studies in India have found that sex work-related mobility is often undertaken to maximise trade opportunity.26 In East Africa, research around mobility has highlighted that mobility both short-term and long-term was associated with higher-risk sexual behaviour, and is strongly associated with gender: the HIV risks associated with mobility are more prominent for women than for men.27
High mobility increases young female sex workers exposure to risk.27 28 Mobility can place people in situations that increase their risk of acquiring STIs, HIV and other infections.28–31 Studies have reported that mobility is associated with concurrent sexual partners which further increases risk to HIV and other STIs.32 Studies from Europe have shown that migrants diagnosed with HIV are more likely to present late for treatment and care than nationals.33 Settling into a new place also presents challenges and instability affecting finding food and medical care34; these include irregular housing status, language and cultural barriers, cost of services, a lack of youth-inclusive health policies and accessible services.27 In this paper, we report patterns of, and reasons for, young women at higher risk (YWHR) mobility and the potential links between mobility and HIV risk among YWHR participating in a randomised controlled trial (RCT) that aims to assess the effectiveness of a cognitive behavioural and structural HIV prevention intervention (the Zero Transmission (ZETRA) trial) on reducing the frequency of unprotected sex in Kampala, Uganda.
Methods
Setting
This study was based within the Good Health for Women Project clinic in Kampala, Uganda. This was an independent clinic established in 2008 to provide HIV and other STI prevention, care and treatment to FSW, their partners and their children in a safe location. Since inception, the clinic has been a site for conducting research on the context and underlying factors of HIV risk.6 18 35–40 The clinic offered routine HIV counselling and testing, syndromic management of STIs, family planning, antenatal care, free condoms, risk reduction counselling, counselling for excessive alcohol use, tuberculosis screening and treatment, ART and co-trimoxazole/dapsone preventive therapy. Enrolled women attended quarterly visits for HIV prevention and treatment services and study visits every 6 months. This clinic generally saw about 50 sex workers per day during the time of the study. To protect the confidentiality and safety of participants, it was located in an accessible area of central Kampala not identifiable to the general public as a place frequented specifically by participants at high risk of HIV infection.
Procedures
Mapping of work venues
The first aim of this substudy was to explore the dynamics of the social and sexual networks, mobility and context of YWHR in Kampala. Work venues of our RCT participants have been mapped in two ways: qualitative and quantitative data collection using key informant interviews of four categories of participants in urban Kampala: YWHR, peer educators, sex worker managers and male partners. In-depth interviews of YWHR study participants explored where, why, how, when, how frequently and for how long they move using interview guides.
Participant enrolment
Randomised parent study
Participants were recruited from a specialised clinic in Kampala called the ‘Good Health for Women Project’ clinic described above. Women were recruited for this clinic by field workers who conducted mobilisation activities with community peer sex worker-leaders to identify sex workers from commercial hotspots who were then enrolled at the clinic irrespective of HIV status as has been described by Vandepitte et al.18 All enrolled women attended quarterly follow-up visits including comprehensive HIV prevention and treatment services described above.
Inclusion criteria for our parent randomised trial (ZETRA trial) included
HIV-negative women, aged 15–24 years, being sexually active and having engaged in any form of transactional sex at least once in the last 3 months, agreeing to participate in intervention sessions and to all study procedures and interviews planned over 18 months of follow-up.
Qualitative substudy on mobility
Participant groups were purposefully selected in order to access opinions, experiences, perceptions on the research questions around mobility from a wide range of possible angles (table 1).
Table 1.
Groups, topics and number of participants in qualitative study on mobility, 2019–2020
| Group | Topics | Number |
|
|
6 HIV positive 8 HIV negative 8 (3 PE; 5 QM) |
| Male partners of YWHR | Customers perspectives on mobility | 6 |
| Health workers | Provider perspectives on barriers to retention; possible solutions | 6 |
| Total | 34 |
YWHR, young women at higher risk.
In addition to describing work venues using text, together with a staff member, the participants used Google Maps to point out the location and improve the accuracy of the work venues’ latitude and longitude coordinates at two time points to assess change over time. An exploratory analysis using Python and Pandas library was conducted to gain a better understanding of the data aspects such as the main features of the data. Python is a programming language. Pandas stands for ‘Python Data Analysis Library’. It takes data and creates a python object with rows and columns forming a data frame that acts very similar to tables in statistical software packages like Excel and SPSS. This was then used to store the data after pre-processing. Finally, descriptive statistics were tabulated.
Community mapping of work venues identified areas sometimes termed ‘hot spots’ where HIV high-risk youth congregate. Mapping was dynamic as new ‘hotspots’ were discovered over time and new information built onto data obtained from community members and the study field team who had strong relationships with participant community members over >10 years. The interviews, lasting about 1 hour, took place in secure and private spaces at the study clinic offices with only researcher and participant present.
All interviewed participants received UgSh 20 000 (US$8.00) as compensation for their transport expenses as is current practice for all other studies at the study clinic.
Data collection and analysis
Interviewers were university-trained social scientists and research counsellors, who conducted in-depth interviews in the local language (Luganda) and had interest in the research topic. Interviews were recorded and field notes taken. Discussions were held before and during the study regarding the sensitive (illegal) nature of sex work in Uganda and how that may affect the research as well as the safety of staff and participants. The interviewers (three women; one man) had over 5 years of experience working with high-risk women and are known and trusted in the participant community.
Interview recordings and notes were transcribed and translated into English. Each audio transcript was quality controlled by the study coordinator who listened to the audio and read the transcript to add any missing information or correct any mis-typed data in the transcript. Coding was conducted using the English translation of the transcripts using NVivo V.12 for Mac by two coders based in Uganda with complete knowledge of the context and focused on descriptive thematic coding.41 Analysis focused on both a priori and emerging content, identifying the dominant and the range of explanations and comparisons across clients. Multiple interactive discussions during team meetings were held with the analysis team and senior researchers to validate data interpretation. The main codes included in the interview guides were frequency, distance and reasons for travel. The codes that emerged during analysis under reasons for mobility included lack of education and employment, violence, lack of agency, influence of social networks and poverty.
Patient and public involvement
Interaction with participants’ in the study was done deliberately from the formative phase where participants shared their priorities, experiences and preferences which informed and guided the development of the research questions, measures and intervention. Participants were not directly involved in the original study design (at proposal writing phase), but they were directly engaged in recruitment of study participants and gave significant input into intervention development with regard to content and form. The current study has benefitted from two community advisory boards, one that was set up for the clinic at initiation in 2008 and one that was a youth-specific community advisory board developed for this study. The groups both met every quarter during the study implementation and provided guidance on both implementation and interpretation of study results. Two specific additional member-checking exercises were conducted in January 2021 with data collection staff and study participants. The 32-item COREC checklist was used to ensure quality of our reporting (online supplemental file 1).
bmjopen-2020-043078supp001.pdf (67.8KB, pdf)
Findings
We recruited 644 YWHR participants for the parent RCT. All participants were HIV negative at enrolment. For this substudy, we conducted 34 qualitative interviews; in addition to the 14 sex workers (6 HIV positive, 8 HIV negative), 6 health worker/policy makers, 3 peer educators, 5 ‘queen mothers’ and 6 male partners were recruited for qualitative interviews. A ‘queen mother’ is the term used by participants and can roughly translate as a sex work manager. The inclusion criteria for peer educators were: must be a sex worker who was influential in the sex worker community, knew the sex workers within her community (hot spot), has been working within the hot spot for at least a year, knew how to communicate well to participants and study staff. The median age of YWHR sample at baseline was 20.5 years, 46% of whom were 15–19 years of age. With regard to educational level, 7% of YWHR had reached A-level or beyond and about half had some primary education (table 2).
Table 2.
Average age and age range of qualitative participants 2019–2020
| Category | Average age | Range |
| Queen mothers | 39.8 | 32–53 |
| YWHR HIV negative | 20.5 | 18–24 |
| YWHR HIV positive | 22.5 | 20–24 |
| Male partners | 36.4 | 34–40 |
| HCWs | 34.2 | 23–45 |
HCWs, healthcare workers; YWHR, young women at higher risk.
Nobody refused to be interviewed.
By 15 March 2020, of the 236 participants who attended both 12-month and 18-month follow-up visits, 193 (82)% identified different work venues across these time points.
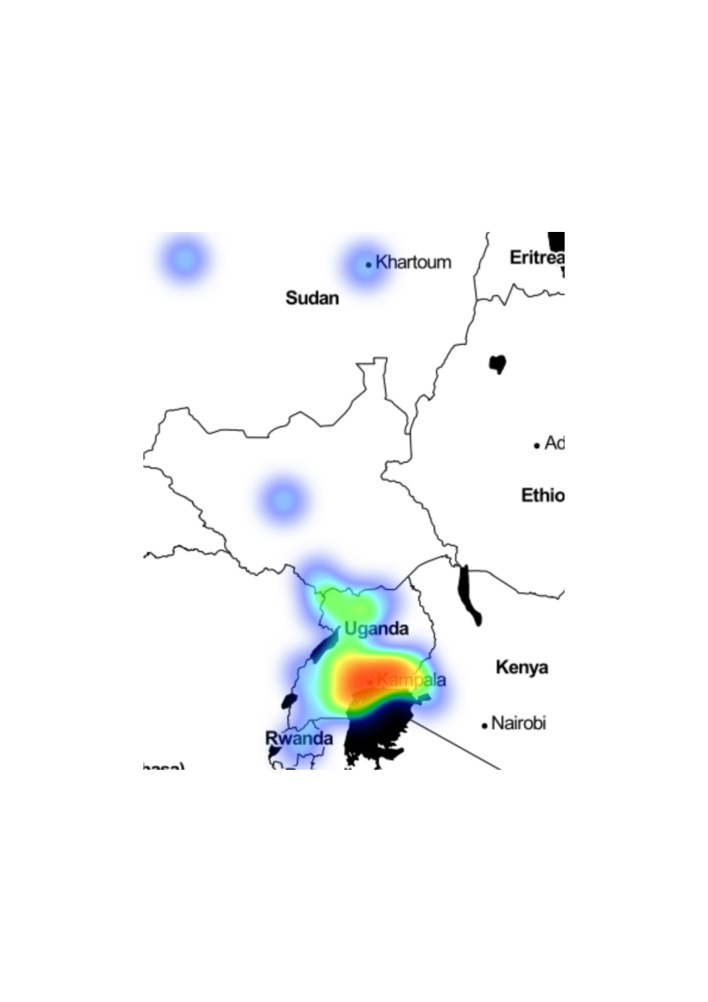
Work venues span distances from Sudan, Kenya and Rwanda, rural Uganda and Kampala. The median distance travelled was 5 km with an IQR of 4–10 in active Kampala work venues like Makindye and Bwaise, with the clinic coordinates as reference point. Most (85%) of the movement was within a radius of 15 km from Kampala. Fifteen per cent of the movements were beyond 15 km from Kampala (figure 1).
Figure 1.
Mapping data on reported work venues for young sex workers in Kampala.
More older women (aged 20–24 years) travelled farther (>15 km) compared with YWHR aged 15–19 years. Some participants described frequenting up to 12 workplaces in the previous month. Seven YWHR participants had seroconverted at their 6-month visit, three at 12 months and three at 18 months.
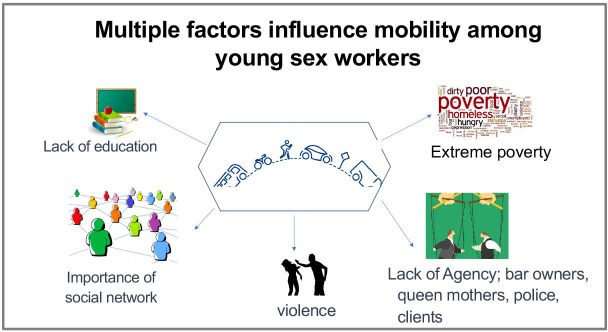
In interviews we asked YWHR (HIV positive and negative), male partners, bar managers and owners, health workers and ‘queen mothers’ reasons for high mobility. Five basic themes emerged: lack of education and employment opportunities, violence, lack of agency, social/sexual/familial networks and poverty (figure 2).
Figure 2.
The factors influencing mobility among young sex workers in Kampala.
Lack of education and employment options leading to mobility
With little or no education or job training, participants narrated life stories that they described as ‘failed dreams’. One participant, the 10th child in her family, described her dream as a young girl wishing to become a doctor. With insufficient money to continue her education, she had a second dream of hotel management. As this dream did not materialise, she described survival strategies that included moving from place to place performing sex work. Changing dreams led to changing locations. Another participant, the ninth child in her family, recounted her story of deciding to quit school to help her parents stop worrying about her school fees. She said: (when teachers), “chase you from school [meaning force you to leave school due to lack of school fees] and you spend a week at home”, it was very difficult on the whole family. Some YWHR mentioned stealing money as a way to survive without a job and running from one place to another not to be caught by police or by the people they stole from.
You go to a club in Wandegeya [a Kampala quarter] and meet a man who gives you 20 000/= [~6 USD] to go and buy beer… It is at that point that you get out of the club and move to another bar…You disappear… When you go to [another bar] and meet someone who gives you 10 000/= to buy beer, you also leave… By the end of the day, all you have done is cheat them of their money without much effort (YWHR, early 20s).
Some young women noted that there are educated sex workers, however, but they often work under different circumstances described as escort services that earn more money and are in less dangerous conditions.
Violence between YWHR and customers and between themselves
YWHR described situations where violence was a ‘normal’ part of their lives inflicted by customers neglecting to wear condoms. One YWHR narrating her experiences working on the Ssese Islands: “You may ask a man to wear a condom and those are automatic punches”. Other YWHR describe how regular partners find them in bars unexpectedly and beat them for that.
You may sometimes be at work and he finds you, ‘What are you doing here at night?’ he asks. He beats you up… You are definitely forced to leave that place because he has embarrassed you before your customers. (YWHR, early 20s)
Physical violence, or the threat of violence, perpetrated by boyfriends, colleagues or pimps was reported as a reason for frequent mobility; sometimes as a response to what may have been thought of as wrongdoing:
….when we steal from customers… should he find you, he can box you (Laughs heartedly)… Should he get you, he can beat you up. So, you have to be really witty. Some men have families and they budget how much they are to spend on a prostitute … say about 5000/= [~1.30 USD]… you come and take it all, you also take his phone. Should he find you, he can surely beat you up (YWHR, early 20s)
A YWHR, whose parents had both died when she was under 10 years old and who was raised by her uncle, narrated her experience of leaving that home soon after her parents died and starting sex work under 15 years of age. She described how customers in bars would often give young women too much alcohol so that they would get very drunk and then force them to have sex without payment; if the woman refused, she would either have to run or be beaten up. A second YWHR recounted the story of a friend who was sold to an overseas sex worker-dealer and broke her legs when she was thrown off a balcony.
Sometimes you might even be put in a room with twenty men and you're to sleep with all of them in one night … (young sex worker, HIV positive, early 20s)
One male partner described that some relationships between YWHR may become violent. Sex workers themselves discussed how the competition for customers and jealousy regarding success between them can lead to violence and movement.
They are so violent. They fight too much …one gets to a point where they cannot live with anyone … Alcohol and the things they use [other drugs]… fighting also causes them to move … they are drunk full-time (Male partner)
Drug use, tension and infighting among YWHR and between them and customers were all reasons for mobility.
Lack of agency in relation to mobility
Some participants noted that YWHR do not often have full control over their lives and the movement in their lives. They could be at the mercy of clients, queen mothers, whoever is providing housing, the police, bar owners or managers. One male partner noted that some bars bring a group of young women, about 10, on the weekends, take them back to rural areas on Monday, and bring a new group the following weekend.
They have to keep on moving because it’s not good when the clients get used to their faces… Clients only give good money to fresh faces… With time they go back to the places they’ve been before. They just keep on rotating [moving] (Bar owner)
Some young women work under a manager who has control over their mobility; when, where, how frequently and for how long they work in certain locations. A male partner described how negotiations take place between the manager and the venue owner regarding the young women who are brought from rural areas to work in some locations in Kampala.
It’s the boss [the pimp/queen mother] for those [girls]… they go anywhere she tells them to (Male partner)
In other situations, as sex work is illegal, law enforcement will regulate young women’s movements by coercing money out of them or forcing them to move. Some women mentioned how during seasons when police may need money, they will harass YWHR; this will be another reason for their mobility.
Sometimes the police come and search for us and they do not want you there… Like Christmas season…they round you up; we get little money and they want some of it …You run to some place where they do not know you,… (YWHR, early 20s).
How social networks and social support relate to mobility
Participants described home environments where there is no emotional, social or financial support. In some cases, YWHR have had to move from home to home or to leave school due to the death of parents. These situations can lead to mobility to escape an unstable or unhealthy setting.
They don’t have parents. Some have caretakers who aren’t their biological parents; they have faced many social issues. They keep on moving from one place to another …Their needs are not met… they are out of school… (Health worker, aged 45 years)
YWHR described how they preferred to stay close to their friends, who may be emotionally replacing a family network, so that when a friend moves from one place to another they follow along and go together. One participant also explained how YWHR count on each other for safety, that they ‘have to be there for each other’. Participants have also noted that their connections to one another are similar to a business partner where if a customer requests a quality such as size or beauty, a participant may connect her associate to that customer. One health worker also mentioned peer pressure as a factor leading to mobility; ‘she might have a colleague in Bwaise who will convince her to move (there) when they talk to each other’; citing higher payment in another location.
Poverty leads to mobility
The overarching reason for why participants constantly move was financial. One participant mentioned that they travel to different towns to target market days. Other illustrations of this association included descriptions of accommodations that are daily rate lodges where one has to leave if she cannot pay for the night. Searching for bars where they could have loyal or regular, customers, leaving venues that were already claimed by other sex workers; or going to a place where customers pay higher prices were all situations connecting poverty and mobility.
The reason we kept leaving, was money. They may be buying sex workers here for 5000/= and elsewhere they are buying them at 10 000/= or 15 000/= (YWHR, early 20s)
The biggest reason we left that place was that there were colleagues that had specific customers and they would tell us to look for our customers that were dedicated and attached to us… The reason [for mobility] was to get a new place (YWHR, early 20s)
In addition to the reasons for mobility, we asked about frequency of travel and distances travelled. The farthest distances travelled included Mombasa, Mauritius, Dubai, Juba and Canada.
Reasons for participants’ mobility concentrated around the themes of lack of education and employment opportunities sometimes related to seasons including the festive season, violence, lack of agency, limited family support/social networks as well as poverty. Subthemes and connections between these themes show a complex web of drivers of mobility potentially leading to high-risk sexual behaviour.
Discussion
Our findings highlight that YWHR in Kampala are highly mobile, with multiple push and pull factors associated with mobility. We found that participants were far more mobile than we anticipated, with both greater distances, greater frequency and destinations of movement.
Access to sexual and reproductive health services: previous studies dating back to early 2000s, showed that a number of factors were associated with initiating sex work in Uganda and the region; including low levels of education, broken family systems, limited job market and low access to sexual and reproductive health services and these factors are similar to the factors we have found that influence mobility.42 43 Limited access to sexual and reproductive health for AGYW is an important factor related to the high level of unexpected pregnancies among this age group. Maternal mortality is the second largest cause of death among adolescent girls aged 15–19 years globally. Of all annual births, around 16 million are among girls in this age range; about 2 million are among girls under the age of 15 years.44 In addition, 41% of young women aged 20–24 years and nearly half of those who experienced sexual violence, were pregnant, the highest rate in sub-Saharan Africa.45 With limited education, and very high national unemployment, many young women have very few options in making enough money to feed themselves and their children. This of course is exacerbated with the current COVID-19 crisis. Often the constellation of factors leading young women into sex work are the factors that push them into steady mobility.
Violence motivates mobility: some sex worker studies conducted in sub-Saharan Africa have highlighted how migration into urban areas to sell sex has resulted in conflicts and violence with local sex workers.46 Our participants also described how they often moved in order not to compete with other women or to find a venue where they could cultivate loyal clients. Violence and fear of violence has been reported as closely intertwined with mobility, poverty, substance abuse and risk for HIV in India.47 48 Intimate partner violence (IPV) is highly associated with risk for HIV and Ugandan women and female sex workers report extremely high rates of reported IPV (45%–75% globally).17 49 50 Among Ugandan women, aged 20–24 years, 40% have experienced sexual violence.51 52 In our study, violence was reported as perpetrated by police, regular and non-regular partners, other sex workers and managers or pimps, and was a reason for mobility. The reasons were to run from a conflictual or violent situation or towards a potentially more peaceful situation. Ramesh et al demonstrated that participants who were more mobile were more likely to report violence and that sex workers reporting both mobility and violence were more likely to be infected with HIV.47 There are many studies globally reporting correlation between violence and increased risk for HIV.49 Physical, sexual and psychological violence increase susceptibility to HIV among women and girls often through a clustering of factors that include poverty, substance use, social, gender norms that weave into an intractable pattern of higher risk environment.49
Relationship between mobility and HIV prevention: the proposed pathways showing higher mobility associated with HIV risk in other studies demonstrate that female sex workers who travel more often reported less consistent condom use, have higher STI symptoms and greater perceived risk for HIV acquisition even after controlling for demographic and socioeconomic factors including violence.29 53–55 In our study, over 80% of the participants were mobile, and we do note that reasons for mobility are qualitatively related to high-risk sexual behaviour and are strong obstacles for HIV prevention behaviour including consistent adherent condom use and use of pre-exposure prophylaxis (PrEP) medication.
Limitations and strengths: our study was not originally powered to statistically measure the relationship between mobility and STI, HIV or unplanned pregnancy. We noted the high mobility on assessing the reasons for difficulty in retaining our study participants. This became a substudy and we were then able to discuss, in-depth, the frequency, distances, reasons and context surrounding our participants’ mobility.
To improve our understanding of the dynamic and complex nature of movement, sexual behaviour and the relationships between populations and disease transmission, Cassels et al proposed a network-dyadic conceptual model to interpret previous studies and inform the development of services and research.56 They propose that the transmission of HIV is dependent on movement and people’s behaviour which is influenced by the connecting of local subepidemics, and the effects on both sending and receiving communities.56 We propose that the intricate, dynamic and complex nature of relationships between both formal and informal sex work, poverty, substance use, family members, friends/colleagues and queen mother relationship networks, violence and mobility are constantly changing and impacting on each other in different and convoluted ways. How public health intervention development and implementation features into the complex interactions of the lives of participants is complex, delicate and the greater understanding we acquire into how mobility impacts on our ability to intervene the more effective these interventions will likely become. Study retention strategies and healthcare services should be informed by a more comprehensive and nuanced understanding of the complicated and tenuous lives of participants and services, and interventions should be tailored to suit mobility patterns. Peers, bar/lodge managers who have influence on YWHR lives and mobility should be involved in research activities if retention of YWHR is to be attained. We must build a mindful PrEP intervention appreciating that our beneficiaries are constantly on the move. This may look very different from a traditional clinic-based service that expects all clients to come on a regular basis for follow-up visits. A mobile clinic, conducted within active work venues, has been piloted to assess its feasibility for reducing the transport burden on highly mobile participants and increasing retention in care. We have attempted to understand whether and how mobility influences the effectiveness of HIV prevention services specifically with YWHR and the utility of identifying appropriate approaches and methods, inclusive of mobile populations, which are desperately needed at this critical moment in the HIV epidemic.27
Supplementary Material
Footnotes
Contributors: RK conceived of the study. EM and DB conducted the geography data analysis and provided input on study design and study procedures. MM, a female research counsellor, participated in data collection. FK, MM and MN oversaw data collection. RK was primarily responsible for qualitative data analysis, with input from JS. All authors were involved in member-check. RK composed the first draft of the manuscript. All authors provided input and approved of the final submission.
Funding: This study was supported by the National Institutes of Mental Health (R01MH109337), PI: RK. All authors are independent from the funders and had full access to all of the data. All authors take responsibility for the integrity of the data and accuracy of the data analysis.
Map disclaimer: The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the 'Methods' section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This research was approved by the Uganda Virus Research Institute (#GC/127/16/08/527) and the Ugandan National Council for Science and Technology (UNCST) (#HS1886). We have written informed consent for all participants and have, as confirmed by the Uganda National Council of Science and Technology, confirmed all those who are under 18 as ‘emancipated minors’. The UNCST has approved this study under the regulations as such.
References
- 1.Idele P, Gillespie A, Porth T, et al. Epidemiology of HIV and AIDS among adolescents: current status, inequities, and data gaps. J Acquir Immune Defic Syndr 2014;66:S144–53. 10.1097/QAI.0000000000000176 [DOI] [PubMed] [Google Scholar]
- 2.Stover J, Rosen J, Kasedde S, et al. The impact and cost of the HIV/AIDS investment framework for adolescents. J Acquir Immune Defic Syndr 2014;66:S170–5. 10.1097/QAI.0000000000000174 [DOI] [PubMed] [Google Scholar]
- 3.Busza J, Mtetwa S, Mapfumo R, et al. Underage and underserved: reaching young women who sell sex in Zimbabwe. AIDS Care 2016;28:14–20. 10.1080/09540121.2016.1176673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hunter M. The materiality of everyday sex: thinking beyond “prostitution”. Afr Stud 2002;61:99–120. 10.1080/00020180220140091 [DOI] [Google Scholar]
- 5.MacPherson EE, Sadalaki J, Njoloma M, et al. Transactional sex and HIV: understanding the gendered structural drivers of HIV in fishing communities in Southern Malawi. J Int AIDS Soc 2012;15:1–9. 10.7448/IAS.15.3.17364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mbonye M, Nakamanya S, Nalukenge W, et al. 'It is like a tomato stall where someone can pick what he likes': structure and practices of female sex work in Kampala, Uganda. BMC Public Health 2013;13:741. 10.1186/1471-2458-13-741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miller CL, Bangsberg DR, Tuller DM, et al. Food insecurity and sexual risk in an HIV endemic community in Uganda. AIDS Behav 2011;15:1512–9. 10.1007/s10461-010-9693-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wamoyi J, Ranganathan M, Kyegombe N, et al. Improving the measurement of transactional sex in sub-Saharan Africa: a critical review. J Acquir Immune Defic Syndr 2019;80:367. 10.1097/QAI.0000000000001928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bantebya G, Muhanguzi FK, Watson C. Adolescent girls in the balance: changes and continuity in social norms and practices around marriage and education in Uganda. Kampala, Uganda: ODI, 2014. [Google Scholar]
- 10.Stoebenau K, Heise L, Wamoyi J, et al. Revisiting the understanding of “transactional sex” in sub-Saharan Africa: a review and synthesis of the literature. Soc Sci Med 2016;168:186–97. 10.1016/j.socscimed.2016.09.023 [DOI] [PubMed] [Google Scholar]
- 11.Baral S, Beyrer C, Muessig K, et al. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis 2012;12:538–49. 10.1016/S1473-3099(12)70066-X [DOI] [PubMed] [Google Scholar]
- 12.Walker D, Pereznieto P, Bantebya G. Sexual exploitation of adolescent girls in Uganda: the drivers, consequences and responses to the ‘sugar daddy’ phenomenon. Kampala, Uganda: ODI, 2014. [Google Scholar]
- 13.Bakeera-Kitaka S, Nabukeera-Barungi N, Nöstlinger C, et al. Sexual risk reduction needs of adolescents living with HIV in a clinical care setting. AIDS Care 2008;20:426–33. 10.1080/09540120701867099 [DOI] [PubMed] [Google Scholar]
- 14.Lowenthal ED, Bakeera-Kitaka S, Marukutira T, et al. Perinatally acquired HIV infection in adolescents from sub-Saharan Africa: a review of emerging challenges. Lancet Infect Dis 2014;14:627–39. 10.1016/S1473-3099(13)70363-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MOH . Uganda AIDS indicator survey 2011. Kampala, Uganda and Calverton, Maryland, USA, 2012. [Google Scholar]
- 16.MOH . The crane survey report. Kampala, Uganda: MOH, 2009. [Google Scholar]
- 17.Hladik W, Baughman AL, Serwadda D, et al. Burden and characteristics of HIV infection among female sex workers in Kampala, Uganda - a respondent-driven sampling survey. BMC Public Health 2017;17:565. 10.1186/s12889-017-4428-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vandepitte J, Bukenya J, Weiss HA, et al. HIV and other sexually transmitted infections in a cohort of women involved in high-risk sexual behavior in Kampala, Uganda. Sex Transm Dis 2011;38:316–23. [PMC free article] [PubMed] [Google Scholar]
- 19.Goldenberg S, Silverman J, Engstrom D, et al. “Right here is the gateway”: mobility, sex work entry and HIV risk along the Mexico-U.S. Border. Int Migr 2014;52:26–40. 10.1111/imig.12104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goldenberg SM, Chettiar J, Simo A, et al. Early sex work initiation independently elevates odds of HIV infection and police arrest among adult sex workers in a Canadian setting. J Acquir Immune Defic Syndr 2014;65:122–8. 10.1097/QAI.0b013e3182a98ee6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldenberg SM, Rangel G, Vera A, et al. Exploring the impact of underage sex work among female sex workers in two Mexico-US border cities. AIDS Behav 2012;16:969–81. 10.1007/s10461-011-0063-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Odinokova V, Rusakova M, Urada LA, et al. Police sexual coercion and its association with risky sex work and substance use behaviors among female sex workers in St. Petersburg and Orenburg, Russia. Int J Drug Policy 2014;25:96–104. 10.1016/j.drugpo.2013.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rocha-Jimenez T, Brouwer KC, Silverman JG. Exploring the context and implementation of public health regulations governing sex work: a qualitative study with migrant sex workers in Guatemala. J Immigr Minor Health 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Servin AE, Brouwer KC, Gordon L, et al. Vulnerability factors and pathways leading to Underage entry into sex work in two Mexican-US border cities. J Appl Res Child 2015;6. [PMC free article] [PubMed] [Google Scholar]
- 25.Silverman JG. Adolescent female sex workers: invisibility, violence and HIV. Arch Dis Child 2011;96:478–81. 10.1136/adc.2009.178715 [DOI] [PubMed] [Google Scholar]
- 26.Saggurti N, Verma RK, Modugu HR. Patterns of migration/mobility and HIV risk among female sex workers. Andhra Pradesh Population Council, 2007. [Google Scholar]
- 27.Camlin CS, Cassels S, Seeley J. Bringing population mobility into focus to achieve HIV prevention goals. J Int AIDS Soc 2018;21:e25136. 10.1002/jia2.25136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Camlin CS, Akullian A, Neilands TB, et al. Gendered dimensions of population mobility associated with HIV across three epidemics in rural Eastern Africa. Health Place 2019;57:339–51. 10.1016/j.healthplace.2019.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kishamawe C, Vissers DCJ, Urassa M, et al. Mobility and HIV in Tanzanian couples: both mobile persons and their partners show increased risk. AIDS 2006;20:601–8. 10.1097/01.aids.0000210615.83330.b2 [DOI] [PubMed] [Google Scholar]
- 30.McGrath N, Eaton JW, Newell M-L, et al. Migration, sexual behaviour, and HIV risk: a general population cohort in rural South Africa. Lancet HIV 2015;2:e252–9. 10.1016/S2352-3018(15)00045-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Camlin CS, El Ayadi AM, Kwena ZA, et al. High mobility and HIV prevalence among female market traders in East Africa in 2014. J Acquir Immune Defic Syndr 2017;74:e121–8. 10.1097/QAI.0000000000001252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Camlin CS, Akullian A, Neilands TB, et al. Population mobility associated with higher risk sexual behaviour in eastern African communities participating in a universal testing and treatment trial. J Int AIDS Soc 2018;21:e25115. 10.1002/jia2.25115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hernando V, Alvárez-del Arco D, Alejos B, et al. HIV infection in migrant populations in the European Union and European economic area in 2007-2012: an epidemic on the move. J Acquir Immune Defic Syndr 2015;70:204–11. 10.1097/QAI.0000000000000717 [DOI] [PubMed] [Google Scholar]
- 34.Cassels S, Camlin CS, Seeley J. One step ahead: timing and sexual networks in population mobility and HIV prevention and care. J Int AIDS Soc 2018;21:e25140. 10.1002/jia2.25140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vandepitte J, Weiss HA, Bukenya J, et al. Alcohol use, Mycoplasma genitalium, and other STIs associated with HIV incidence among women at high risk in Kampala, Uganda. J Acquir Immune Defic Syndr 2013;62:119–26. 10.1097/QAI.0b013e3182777167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vandepitte J, Muller E, Bukenya J, et al. Prevalence and correlates of Mycoplasma genitalium infection among female sex workers in Kampala, Uganda. J Infect Dis 2012;205:289–96. 10.1093/infdis/jir733 [DOI] [PubMed] [Google Scholar]
- 37.Vandepitte J, Weiss HA, Kyakuwa N, et al. Natural history of mycoplasma genitalium infection in a cohort of female sex workers in Kampala, Uganda. Sex Transm Dis 2013;40:422–7. 10.1097/OLQ.0b013e31828bfccf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bukenya J, Vandepitte J, Kwikiriza M, et al. Condom use among female sex workers in Uganda. AIDS Care 2013;25:767–74. 10.1080/09540121.2012.748863 [DOI] [PubMed] [Google Scholar]
- 39.Francis SC, Baisley K, Lees SS, et al. Vaginal practices among women at high risk of HIV infection in Uganda and Tanzania: recorded behaviour from a daily pictorial diary. PLoS One 2013;8:e59085. 10.1371/journal.pone.0059085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mbonye M, Nalukenge W, Nakamanya S, et al. Gender inequity in the lives of women involved in sex work in Kampala, Uganda. J Int AIDS Soc 2012;15:1–9. 10.7448/IAS.15.3.17365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyatzis R. Transforming qualitative information: thematic analysis and code development. SAGE Publications, Inc, 1998. [Google Scholar]
- 42.MOH . Adolescent health policy guidelines and service standards for Uganda. Uganda: MOH, 2011. [Google Scholar]
- 43.MOH . Adolescent sexual and reproductive health: a job Aide 2012, 2012. [Google Scholar]
- 44.WHO . Adolescent pregnancy, 2020. Available: https://www.who.int/newsroom/fact-sheets/detail/adolescent-pregnancy [Accessed 8 Apr 2020].
- 45.UNFPA . Adolescents and young people in Sub-Saharan Africa opportunities and challenges. Johannesburg: UNFPA, 2012. [Google Scholar]
- 46.Chiyaka T, Mushati P, Hensen B, et al. Reaching young women who sell sex: methods and results of social mapping to describe and identify young women for DREAMS impact evaluation in Zimbabwe. PLoS One 2018;13:e0194301. 10.1371/journal.pone.0194301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ramesh S, Ganju D, Mahapatra B, et al. Relationship between mobility, violence and HIV/STI among female sex workers in Andhra Pradesh, India. BMC Public Health 2012;12:764. 10.1186/1471-2458-12-764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Saggurti N, Jain AK, Sebastian MP. Indicators of mobility, socio-economic vulnerabilities and HIV risk behaviours among mobile female sex workers in India. AIDS Behav 2012;16:952–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.STRIVE . Addressing the structural drivers of HIV: a STRIVE synthesis London school of hygiene & tropical medicine, 2019. [Google Scholar]
- 50.Roberts ST, Haberer J, Celum C, et al. Intimate partner violence and adherence to HIV pre-exposure prophylaxis (PrEP) in African women in HIV serodiscordant relationships: a prospective cohort study. J Acquir Immune Defic Syndr 2016;73:313–22. 10.1097/QAI.0000000000001093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Amegbor PM, Pascoe L. Variations in emotional, sexual, and physical intimate partner violence among women in Uganda: a multilevel analysis. J Interpers Violence 2019:088626051983942. 10.1177/0886260519839429 [DOI] [PubMed] [Google Scholar]
- 52.Cabral A, M Baeten J, Ngure K, et al. Intimate partner violence and self-reported pre-exposure prophylaxis interruptions among HIV-negative partners in HIV serodiscordant couples in Kenya and Uganda. J Acquir Immune Defic Syndr 2018;77:154–9. 10.1097/QAI.0000000000001574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saggurti N, Verma RK, Modugu HR, et al. Patterns of migration/mobility and HIV risk among female sex workers: Andhra Pradesh 2007–08. New Delhi, India: Population Council, 2008. [Google Scholar]
- 54.Saggurti N, Jain AK, Sebastian MP, et al. Indicators of mobility, socio-economic vulnerabilities and HIV risk behaviours among mobile female sex workers in India. AIDS Behav 2012;16:952–9. 10.1007/s10461-011-9937-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Camlin CS, Hosegood V, Newell M-L, et al. Gender, migration and HIV in rural KwaZulu-Natal, South Africa. PLoS One 2010;5:e11539. 10.1371/journal.pone.0011539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cassels S, Jenness SM, Khanna AS. Conceptual framework and research methods for migration and HIV transmission dynamics. AIDS Behav 2014;18:2302–13. 10.1007/s10461-013-0665-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-043078supp001.pdf (67.8KB, pdf)
Data Availability Statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.