Abstract
Objectives
There is limited research on sex differences in postural orientation (ie, alignment between body segments) in people with knee injury measured with a clinically applicable method. An understanding of the relationship between postural orientation and physical function may help guide decision making in rehabilitation. The aims were to evaluate (1) sex differences in visual assessment of Postural Orientation Errors (POEs) and (2) the association between POEs and objective and patient-reported physical function, in men and women with anterior cruciate ligament reconstruction (ACLR).
Methods
Twenty-four women and 29 men (mean 26.7 (SD 6.5) years) with ACLR were included. Six POEs (lower extremity and trunk) were scored from a video of five tasks with varying difficulty to compute POE scores (total and subscores). Objective physical function was evaluated with the single-leg hop for distance and side hop. Patient-reported physical function was evaluated using patient-reported outcome measures (PROMs).
Results
Women had significantly more POEs than men (median difference 5.5–25, p≤0.028). More POEs were associated with shorter hop distance and fewer side hops in women (rs= −0.425 to −0.518, p<0.038), but not in men (rs<0.301, p>0.05). No associations were found between POE scores and PROMs, in either sex (rs< –0.246, p>0.05).
Conclusions
Women with ACLR seem to have more POEs compared with men, indicating worse postural orientation. More POEs were associated with worse hop performance, suggesting that POE scores may be used as criteria for rehabilitation progression. The lack of associations between POE scores and PROMs indicate that these measures complement each other.
Keywords: anterior cruciate ligament, knee injuries, questionnaire, sports physiotherapy, gender
Key messages.
What is already known
Women have shown to have worse postural orientation at the knee, measured with 3D kinematics, compared with men.
What are the new findings
Women with anterior cruciate ligament reconstruction (ACLR) had more Postural Orientation Errors (POEs) compared with men. To help design rehabilitation programmes to improve postural orientation in patients with an ACL injury, future studies need to investigate underlying modifiable factors for POEs, for example, muscle strength and muscle activation patterns, in men and women, respectively.
POE scores were moderately to strongly associated with hop performance in women, but not in men. The POE subscale activities of daily living could be used in rehabilitation by clinicians to decide when patients can progress to more advanced exercises, such as jumping tasks.
No associations between POEs and patient-reported outcome measures (PROMs) in this study could indicate that POEs do not reflect the patient’s perceived knee function and knee quality. Assessment of POEs and PROMs may complement each other, and both could be used to evaluate a patient’s knee function during rehabilitation after ACLR.
Introduction
Clinical guidelines for rehabilitation after anterior cruciate ligament (ACL) injury suggest a goal-based approach. Specifically, progression in rehabilitation is based on evaluation of different aspects of patient-reported and objective physical function, for example, patient-reported outcome measures (PROMs), functional performance and movement quality.1 2 Postural orientation is one aspect of movement quality, defined as the ability to maintain alignment between body segments during a static or dynamic task.3 Postural orientation can be measured with either two-dimensional (2D) and 3D kinematics or visual assessment. The latter is a more feasible approach for the clinical setting. However, a systematic approach to visually assess postural orientation is needed to enable valid and reliable evaluations and to facilitate comparison between studies, but no such approach is included in current clinical guidelines.1 2 In recent cross-sectional studies, we evaluated measurement properties of a test battery for visual assessment of Postural Orientation Errors (POEs) of the lower extremity and trunk, during tasks of varying difficulty. The test battery showed good reliability and validity in patients with an ACL injury and ACL reconstruction (ACLR).4 5 Thus, visual assessment of POEs can be used to assess postural orientation during the rehabilitation of ACL injuries.
Undesirable postural orientation, for example, greater 3D knee abduction, is suggested as a risk factor for sustaining both a first and second ACL injury.6 7 Women have an increased risk of rupturing their ACL compared with men.8 Thus, it is of importance to investigate sex differences in various measures of postural orientation, to guide rehabilitation progression for men and women, respectively. A systematic review9 and recent cross-sectional study10 observed worse postural orientation, that is, greater 3D knee abduction angle, in both women with an ACL injury and healthy women, compared with men. In contrast, no sex differences were observed for visual assessment of Knee Medial-to-Foot Position (KMFP).11 However, whether sex differences are present in visual assessment of other POEs during daily and sport-specific activities in individuals with an ACL injury is unknown.
Hop performance and strength measures are often used as criteria for return to sport. However, these measures alone do not seem to provide sufficient information for a safe return to sport.12 13 A combination of measures of objective physical function (eg, movement quality, strength and hop performance) and patient-reported functions are recommended in clinical guidelines to guide progression during ACL rehabilitation, and help with the decision regarding return to sport.1 2 An understanding of the relationship between objective and patient-reported physical functions might help in better targeting the approach to rehabilitation, and possibly facilitate a safer return to sport/activity. For example, one cross-sectional study reported that quadriceps strength asymmetry was associated with greater movement asymmetry in the knee during landing, the authors, therefore, suggested that rehabilitation needs to focus on increasing quadriceps strength to improve knee biomechanics during landing.14 To our knowledge, the association between visual assessment of movement quality and other measures of objective and patient-reported physical functions has only been examined in one cohort, including people with an ACL injury or ACLR.15 16 Poorer movement quality (referred to as ‘substitution patterns’) was associated with worse patient-reported knee function and lower knee-specific activity, and worse hop performance.15 16 Although several studies have observed sex differences in various measures of physical function, for example, hop performance,10 PROMs17 18 and postural orientation (3D knee kinematics),7 9 10 there is limited research on whether associations between physical functions differ between men and women.
The aims of this study were to (1) evaluate sex differences in postural orientation assessed by visual observation of POEs, and (2) determine the association between POEs and hop performance and PROMs, respectively, in men and women undergoing rehabilitation after ACLR.
Methods
Study design and patients
An invitation to participate in this cross-sectional study was sent out to all patients at the Department of Orthopaedics, Skåne University Hospital, Sweden, that had undergone an ACLR between June 2015 and March 2016 (n=165). Patients were included if they were between 18 and 39 years of age, >16 weeks postreconstruction, undergoing supervised physical therapy, and had progressed to jumping exercises with a change of direction in their rehabilitation. Patients who used crutches, had completed rehabilitation, had a medial collateral ligament injury grade 3, or other injuries or diseases overriding the knee injury symptoms were excluded.
All patients gave their written informed consent before participation. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (online supplemental appendix 1).19 Patients were not involved in this study’s design, conduct, reporting or dissemination plans.
Procedures
Data were collected during a single session at Lund University, Sweden. During data collection, patients wore their own athletic shoes, shorts and sports bra (women).
Functional tasks
Five tasks with increasing difficulty were performed according to Nae et al,4 5 in the following order: (1) single-leg mini squat (SLS), (2) stair descending (SD), (3) forward lunge (FL), (4) single-leg hop for distance (SLHD) and (5) side hop (SH). The tasks were videorecorded from a frontal view (Oqus colour video camera (2c-series), 30 Hz, V.2.12, Gothenburg, Sweden).
Postural Orientation Errors
POEs were visually assessed from the video-recordings by one physical therapist (JN). Each segment-specific POE was scored on a 3-point ordinal scale from 0 (good) to 2 (poor) with a validated, reliable scoring system (inter-rater reliability weighted Ƙ=0.31 to 0.9).4 5 The Total POE score (the score of POEs within and across tasks), the POE subscale activities of daily living (ADL) (the POE scores within the SLS, SD and FL), the POE subscale Sport (the POE scores within the SLHD and SH), segment-specific POEs across tasks (the score of a segment-specific POE across tasks), and within-task POE scores (the score of segment-specific POEs within respective hop task) were calculated to a 0–100 scale (table 1; 0 represents good postural orientation and 100 poor postural orientation).
Table 1.
The test battery of tasks and POEs assessed within each task
| Functional tasks | Ankle POE | Knee POEs | Thigh POE | Hip POE | Trunk POE | Calculation of the within-task POE score | |
| Foot pronation | Knee Medial-to-foot position | Femur medial to shank | Femoral valgus | Deviation of pelvis in any plane | Deviation of trunk in any plane | ||
| Single-leg mini squat* | X | X | X | X | X | X | |
| Stair descending* | X | X | |||||
| Forward lunge* | X | X | X | X | |||
| Single-leg hop for distance | X | X | X | X | |||
| Side hop† | X (M, L) | X (M, L) | X (M, L) | X (M) | X (M) | ||
| Segment-specific POEs across tasks | N.C. | N.C. | |||||
| POE Subscale ADL | (Sum score of single-leg mini squat, stair descending and forward lunge) | ||||||
| POE Subscale Sport | (Sum score of single-leg hop for distance and side hop) | ||||||
| Total POE score | |||||||
Calculation formulae for the within-task POE scores, segment-specific POEs across tasks and total POE score, included in the analysis.
*These tasks are only included in the Total POE score and the POE subscale ADL in this study.
†The segment-specific POEs scored in medial and lateral landings, respectively.
ADL, activities of daily living; L, lateral landing; M, medial landing; N.C, not calculated; POEs, postural orientation errors.
Hop performance
For the SLHD, hop distance was measured in centimetres from toe at take-off to heel at landing. The longest jump from three trials for the injured leg was used in the analysis. The SLHD is reliable (test-retest, intraclass correlation coeficient (ICC)2,1=0.92), and responsive to change through rehabilitation in patients with ACLR.20 The SH was measured as the number of successful hops, on the injured leg, over two parallel lines, 30 cm apart,21 during 30 s.22 The SH has shown excellent test–retest reliability in people following ACLR (ICC=0.87).22
Patient-reported outcome measures
Participants completed web-based versions of the following PROMs the week before physical testing: the Knee injury Osteoarthritis Outcome Score (KOOS),23 the ACL-Quality of Life (ACL-QoL),24 the Knee Self-Efficacy Scale (K-SES)25 and the global knee function.26 Subscales regarding knee function and knee QoL was chosen in PROMs with several subscales.
The KOOS subscales QoL and Functioning in Sport and Recreation (Sport/rec) were used in the analysis. KOOS is reported to be reliable (ICC2,1>0.75), valid against the Short Form-36 (SF-36), and responsive to change (effect sizes at 3 months 0.67–1.11, and 12 months 1.08–3.54).27 28
The ACL-QoL subscales ‘recreational activities and sport participation or competition’ and ‘lifestyle’ were used in the analysis. The Swedish version of the questionnaire has shown good test-retest reliability (ICC2.1=0.71–0.97), and is valid against KOOS QoL (r=0.87) and SF-36 (r=0.65–0.72).29
The K-SES subscale Present was used in the analysis. K-SES has shown good test-retest reliability (ICC=0.75) and is valid against SF-36 and KOOS.25
The global knee function is an estimation of the patients’ global knee function on a visual analogue scale from 1 (‘normal knee function’) to 100 mm (‘totally disabled’).26
Statistical analysis
This was an exploratory investigation and a secondary analysis of a dataset aimed to evaluate measurement properties of POEs,5 thus, no a priori power calculation was performed. Complete cases were used for each analysis. Normality was assessed by inspecting histograms and the Kolmogorov-Smirnov test. All variables, except body mass index (BMI), were normally distributed.
Descriptive statistics were calculated for POE scores (median (quartiles)), hop performance and PROMs (mean (SD)) and for patient characteristics, for men and women separately. Mann-Whitney U test was used to evaluate any sex differences in ordinal data (POE scores) and BMI, independent sample t-tests were used to evaluate possible sex differences in continuous data (hop performance, PROMs, age, height, mass, time since surgery) and χ2 test for nominal data (injury mechanism, injury occasion, graft type). Values of p≤0.05 were considered statistically significant.
The Spearman’s rank correlation coefficient was used to assess associations between postural orientation and hop performance and between postural orientation and PROMs. As hop performance, PROMs and postural orientation include different constructs, at most moderate associations were expected, and will thus be discussed. The following thresholds were applied: ≥0.10–0.29 represents weak correlations,≥0.3–0.49 represents moderate correlations and ≥0.5 strong correlations.30 Values of p≤0.05 were considered statistically significant.
Results
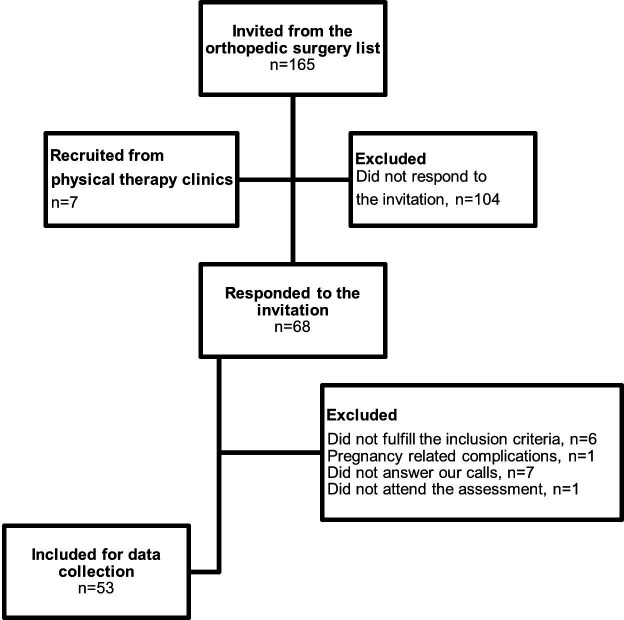
Sixty-eight of the invited 165 participants agreed to participate, and 53 patients were finally included (figure 1). There were missing data for two participants regarding POE scores, and one participant did not respond to the PROMs.
Figure 1.
Flow chart over the recruitment process.
Descriptive data
Twenty-four women (46%), and 29 men (54%), with an ACLR, were included in this study. Women were significantly shorter and lighter than men. Women sustained their injury more often during training and men during the competition. All the other characteristics did not differ between sexes (table 2).
Table 2.
Characteristics of included patients
| Men (n=29) | Women (n=24) | Mean difference (95% CI) | |
| Age* | 27.1 (6.2) | 26.3 (6.9) | −0.85 (−4.5 to 2.8) |
| Height (cm)* | 179 (6.7) | 167 (5.8) | −12.2 (−15.6 to -8.7) |
| Mass (kg)* | 80.6 (12.7) | 67.7 (9.2) | −12.9 (−19.2 to -6.7) |
| BMI† | 24.1 (23.3–26.1) | 23.5 (22.3–26.6) | P=0.211 |
| Injury occasion‡ | P=0.03 | ||
| Match, n (%) | 15 (51.7) | 4 (16.7) | |
| Training, n (%) | 9 (31) | 13 (54.2) | |
| Other, n (%) | 5 (17.2) | 7 (29.2) | |
| Injury mechanism‡ | P=0.653 | ||
| Non-contact, n (%) | 19 (65.5) | 16 (66.7) | |
| Contact, n (%) | 9 (31.0) | 8 (33.3) | |
| Do not remember, n (%) | 1 (3.4) | 0 (0.0) | |
| Time since reconstruction (weeks)* | 28.4 (6.3) | 27 (6.7) | −1.49 (-5.1 to 2.15) |
| Type of graft‡ | P=0.501 | ||
| Hamstrings, n (%) | 27 (93.1) | 22 (91.7) | |
| Patellar, n (%) | 2 (6.9) | 1 (4.2) | |
| Donated, n (%) | 0 | 1 (4.2) | |
| ACL revision surgery, n (%) | 2 (6.9) | 5 (20.9) | P=0.132 |
| Associated injuries, n (%) | 22 (75.9) | 17 (70.8) | P=0.682 |
| Bilateral ACL injury, n (%) | 2 (6.9) | 3 (12.5) | P=0.491 |
| Meniscal injury, n (%) | 10 (34.5) | 14 (58.3) | P=0.595 |
| Collateral ligament, n (%) | 7 (24.1) | 6 (25) | P=0.943 |
| Cartilage, n (%) | 8 (27.6) | 3 (12.5) | P=0.182 |
| Other, n (%) | 1 (3.4) | 2 (8.3) | P=0.448 |
| Tegner activity level before injury† | 8 (6–9) | 8 (6–9) n=23 | P=0.985 |
| Tegner activity level at test session† | 3 (2–4.5) | 3 (3–4) n=23 | P=0.962 |
*Mean (SD).
†Median (quartiles) and Mann-Whitney U-test.
‡χ2 test, significant difference in match and training.
ACL, anterior cruciate ligament; BMI, body mass index.
Sex differences
Women had more POEs (ie, Total POE score, POE subscales and femoral valgus across tasks), jumped a shorter distance and performed fewer SH, compared with men (p<0.05). No sex differences were observed for any PROMs (table 3).
Table 3.
Descriptive data for POE scores, hop performance, patient-reported outcome measures for men and women separately, and differences between men and women
| POE scores | Men (n=29) | Women (n=24) | Mean difference (95% CI) | p-value |
| Total POE score* | 20.5 (14–29)† | 26 (21–33)† | NA | 0.012 |
| POE subscale ADL* | 15.5 (11–24.25)† | 25 (14.75–32.5) | NA | 0.012 |
| POE subscale sport* | 25 (12.5–34.5) | 31 (28–36)† | NA | 0.028 |
| KMFP across tasks* | 10 (0–20) | 20 (10–20)‡ | NA | 0.106 |
| Femur medial to shank across tasks* | 42 (25–65)† | 50 (42–69)‡ | NA | 0.053 |
| Femoral valgus* | 29 (17–48)† | 54 (33–58)‡ | NA | 0.001 |
| Deviation of pelvis in any plane* | 37.5 (25–50) | 50 (37.5–50)‡ | NA | 0.294 |
| Hop performance | ||||
| SLHD§ longest jump (cm) | 121 (36) | 91 (29) | −29.8 (-48.0 to -11.7) | 0.002 |
| SH§ no of hops (n) | 45 (16) | 31 (18) | −14.8 (-24.4 to -5.2) | 0.003 |
| Patient-reported outcome measures | ||||
| KOOS sport/rec§ | 58 (21.9) | 59 (24.8)† | 0.9 (-12.1 to 13.9) | 0.890 |
| KOOS QoL§ | 48 (19.8) | 50 (14.7)† | 1.8 (-8.2 to 11.7) | 0.723 |
| ACL-QoL subscale Recreational activities and sport participation§ | 38 (16.1) | 38 (20.3)† | 0.4 (-9.8 to 13.5) | 0.944 |
| ACL-QoL subscale life style§ | 48 (18.7) | 53 (17.5)† | 4.1 (-6.1 to 14.3) | 0.426 |
| K-SES subscale present§ | 6.7 (1.5) | 7.1 (1.9)† | 0.5 (-0.5 to 1.4) | 0.345 |
| Global knee function§ | 44 (21.8) | 35 (18.8)† | −9.2 (-20.5 to 2.1) | 0.115 |
*Median (quartiles) and Mann-Whitney U-test,.
†One subject did not complete all tasks/PROMs.
‡Two subjects did not complete all tasks.
§Mean (SD) and independent sample t-test.
ACL, anterior cruciate ligament; ADL, activities of daily living; KMFP, Knee Medial to Foot Position; KOOS, Knee injury and Osteoarthritis Outcome Score; K-SES, Knee Self-Efficacy Scale; NA, not applicable; POE, Postural Orientation Error; PROMs, patient-reported outcome measures; QoL, quality of life; SH, side hop; SLHD, single leg hop for distance.
Associations between postural orientation and hop performance
A higher score on the POE subscale ADL was significantly associated with shorter hop distance (−0.518, p=0.01) and fewer SH (−0.425, p=0.038), in women. No significant associations between POE scores and hop performance were observed in men. Non-significant associations above 0.3 were found between higher Total POE score and shorter hop distance in women (rs=−0.349, p=0.103), and between higher within-task, POE score for the SLHD and longer hop distance in men (rs=0.3, p=0.112) (table 4).
Table 4.
Spearman’s rank correlation coefficient (rs) between postural orientation scores and hop performance during the single-leg hop for distance and side hop, in men and women separately
| POE scores | Hop performance | |||||||
| Single-leg hop for distance Longest jump injured leg (cm) |
Side hop No of hops, injured leg (n) |
|||||||
| Men, n=29 | Women, n=24 | Men, n=29 | Women, n=24 | |||||
| rs | p-value | rs | p-value | rs | p-value | rs | p-value | |
| Total POE score | −0.024* | 0.903 | −0.349* | 0.103 | −0.178* | 0.364 | −0.267* | 0.219 |
| POE Subscale ADL | −0.013* | 0.946 | −0.518 | 0.010 | −0.204* | 0.297 | −0.425 | 0.038 |
| POE Subscale Sport | −0.067 | 0.732 | −0.144* | 0.511 | −0.079 | 0.685 | −0.106* | 0.629 |
| Within-task POE score Single-leg hop for distance | 0.301 | 0.112 | −0.120 | 0.577 | NA | |||
| Within-task POE score side hop | NA | −0.177 | 0.359 | −0.048* | 0.827 | |||
r values ≥0.3 are indicated in bold.
*One subject did not complete all tasks.
ADL, activities of daily living; NA, not applicable; POE, postural orientation error; rs, Spearman’s rank correlation coefficient.;
Associations between postural orientation and PROMs
Associations were below 0.3 between POE scores and PROMs, for both men and women (rs=0.0001 to −0.235, p>0.22) (table 5).
Table 5.
Spearman’s rank correlation coefficient (rs) between different postural orientation scores and patient-reported outcome measures separately in men and women
| PROMs | POE scores | |||||
| Total POE score | POE subscale ADL | POE subscale sport | ||||
| rs | P value | rs | P value | rs | P value | |
| KOOS sport/rec | ||||||
| Men (n=29) | −0.179* | 0.68 | 0.0001* | 0.999 | −0.235 | 0.22 |
| Women (n=22) | −0.093 | 0.363 | −0.148 | 0.5 | −0.145 | 0.52 |
| KOOS QoL | ||||||
| Men (n=29) | 0.022* | 0.912 | 0.092* | 0.643 | 0.007 | 0.972 |
| Women (n=23) | 0.120* | 0.594 | −0.014 | 0.949 | 0.184 | 0.412 |
| ACL-QoL subscale Sport† | ||||||
| Men (n=29) | −0.112* | 0.572 | −0.019* | 0.922 | −0.124 | 0.523 |
| Women (n=23) | 0.092* | 0.685 | 0.019 | 0.932 | 0.054 | 0.812 |
| ACL-QoL subscale Life style | ||||||
| Men (n=29) | 0.020* | 0.918 | 0.032* | 0.874 | 0.013 | 0.947 |
| Women (n=22) | 0.216 | 0.335 | 0.057 | 0.796 | 0.142 | 0.53 |
| K-SES subscale Present | ||||||
| Men (n=29) | 0.045* | 0.82 | 0.066a | 0.74 | 0.037 | 0.85 |
| Women (n=22) | 0.046 | 0.839 | 0.021 | 0.925 | −0.145 | 0.52 |
| Global knee function | ||||||
| Men (n=29) | −0.086* | 0.665 | −0.099* | 0.615 | −0.096 | 0.622 |
| Women (n=23) | −0.177* | 0.431 | 0.081 | 0.712 | −0.246* | 0.27 |
*One subject did not complete all tasks.
†ACL-QoL subscale Recreational activities and sport participation.
ACL, anterior cruciate ligament; ADL, activities of daily living; KOOS, Knee injury and Osteoarthritis Outcome Score; K-SES, Knee Self-Efficacy Scale; POE, postural orientation error; PROMs, patient-reported outcome measures; QoL, quality of life; rs, Spearman’s rank.
Discussion
We found that women with ACLR displayed more POEs than men, indicating worse postural orientation and that POE scores were moderately to strongly associated with hop performance in women, but not in men. We found no association between POE scores and PROMs in either sex.
Women with ACLR exhibited more POEs than men in Total POE score, POE subscales and the segment-specific POE femoral valgus. This is consistent with previous studies on sex differences in movement quality, that is, that women have more landing errors31 32 and greater knee abduction,7 9 10 indicating worse movement quality than men. The Landing Error Scoring System (LESS) is a test battery in which movement patterns of the trunk, hip, knee and ankle are visually assessed and scored during the drop jump. Higher LESS scores have been reported in healthy women, and in women with an ACL injury, compared with men.31 32 Because POEs were assessed in multiple tasks using postural orientation as a separate entity, compared with the LESS during one task using different constructs (eg, postural orientation, stance width, and stiff landing), our findings indicate that postural orientation more generally differs between sexes. Kinematic studies, using 3D analysis, have also reported that women have increased knee abduction compared with men, in both healthy9 and populations with ACL injury.7 10 Our findings and those previously reported, suggests that rehabilitation after ACLR, particularly in women, should have a strong focus on improving postural orientation.
There could be several possible modifiable and non-modifiable underlying factors for sex differences in postural orientation, but these are not well explored. One likely anthropometric, non-modifiable, factor is pelvic width. Women have a wider pelvis normalised to height than men,33 and it has been reported that a wider pelvic width to femoral length ratio is associated with greater knee valgus during an SLS.34 However, another study reported that pelvic width to femoral length ratio, in women, was not related to 3D hip adduction during running.35 We did not measure pelvic width in our study. However, pelvic width could explain more femoral valgus POEs in women than men, as one of the reference points for femoral valgus POE is placed on the pelvis. A possible modifiable factor for sex differences in postural orientation could be sensorimotor function. Cronström et al reported that lower knee muscle strength and lower muscle activation of the trunk was associated with increased 3D knee abduction in women, but not in men.10 While there is some understanding of the sex differences and modifiable factors associated with knee abduction (one aspect of postural orientation),9 36 further studies are needed to investigate underlying modifiable factors for other POEs, for example, muscle strength and muscle activation patterns, in men and women. Such information may help design rehabilitation programmes aimed at improving postural orientation in men and women after an ACL injury.
To our knowledge, our study is the first to report associations between postural orientation and hop performance in men and women, separately. The association between more POEs and shorter hop distance and fewer SH in women suggests improving postural orientation might contribute to improved hop performance. Such associations were not found in men indicating that other factors are important for hop performance in men. Only one previous study has reported that worse movement quality (visually assessed ‘substitution patterns’) was associated with worse hop performance in patients with an ACL injury or ACLR.16 However, in that study, men and women were not analysed separately, and the score includes different constructs (eg, postural orientation and body weight distribution), limiting the ability to compare findings between studies.
The only significant associations observed were between the POE subscale ADL and the hop tasks in women. However, it cannot be ruled out that a larger sample size could have resulted in more significant associations for both men and women. One possible explanation may be that good postural orientation during ADL tasks is a requirement for hop performance, indicating that good postural orientation in ADL tasks should be obtained before progression to jumping tasks in rehabilitation after ACLR. This reasoning is in line with practice guidelines for ACL injury treatment, that is, that progression from phase 1 (the acute postoperative phase) to phase 2 (initiating jumping tasks) occurs when the patient can perform phase 1 exercises with good movement quality.1 2 Using the POE subscale ADL may help clinicians decide when patients can progress to more advanced exercises, such as jumping tasks. However, future longitudinal studies are needed to investigate the responsiveness of POE scores during different phases of rehabilitation before specific POE scores can be suggested as criteria for progression in rehabilitation.
The moderate association (although non-significant) between higher within-task POE score for the SLHD and longer hop distance in men showed the reverse relationship compared with women, indicating that a greater hop distance increases the demands on postural orientation in men. A cross-sectional study reported that men with ACL injury had worse movement quality, in terms of reduced 3D hip abduction, during a drop-jump despite having a normal physical function (strength and hop LSI ≥90%), compared with healthy controls.37 The authors suggested that kinematic analysis, in addition to muscle strength and hop performance, could provide further insight into the decision of return to sport.37 Further studies could evaluate whether a visual assessment of POEs could be a valuable tool for such kinematic analysis. A prospective study suggests that altered neuromuscular control at the hip and knee during landing tasks is a risk factor for reinjury.6 Whether more POEs when achieving good hop performance could constitute a risk factor for a future injury needs to be further studied.
The lack of associations between POE scores and PROMs could indicate that POEs do not reflect the patient’s perceived knee function and knee quality. Assessment of POEs and PROMs may complement each other and provide a more complete picture about the patient’s knee function, as suggested in rehabilitation practice and return to sport guidelines.1 Inconsistent findings are reported in cross-sectional studies in patients with lower extremity injury or disorder, where some observed no association between aspects of movement quality and PROMs.38 39 In contrast, others noted that worse movement quality was associated with worse PROMs.15 16 Longitudinal studies indicate that aspects of movement quality, that is, landing asymmetry in knee and trunk flexion,40 and worse ‘substitution patterns’,15 were associated with worse future PROMs.15 40 The predictive ability of POE scores to determine future PROMs is a subject for further study.
Strengths and limitations
This study is the first to investigate sex differences in a test battery for the visual assessment of POEs as a separate entity. Visual assessment of POEs has shown good validity and reliability in previous studies,4 5 indicating that it is clinically feasible. Systematic reviews suggest that hop performance and muscle strength as criteria for return to sport may not be sufficient to identify those at risk of reinjury.12 13 Further studies could evaluate whether a clinical assessment of visual assessment of POEs, in addition to muscle strength and hop performance, would add value to the criteria for progressing rehabilitation and determining return to sport.
Our exploratory study was the first step to investigate sex differences in POEs, and despite the moderate sample size, significant differences were observed between men and women, except for the segment-specific POE scores across tasks (KMFP, femur medial to shank, and deviation of pelvis in any plane). Possible confounding factors, such as height and mass, were not adjusted due to the sample size. Thus, this study’s results need to be interpreted with caution, and a larger sample is needed to verify the result and adjust for possible confounding factors. The present study was a secondary analysis from a study where the primary aim was to evaluate the measurement properties of POEs.5 Therefore, we had no predefined hypothesis on sex differences. Consequently, this was an advantage for the aim of this study because sex was unlikely to be subject to assessor bias.
Conclusions
We observed more POEs in women compared with men, indicating worse postural orientation in women. The association between more POE scores and worse hop performance suggests that POE scores may be used as criteria for rehabilitation progression. The lack of associations observed between POE scores and PROMs indicate that these measures complement each other.
Acknowledgments
The authors want to acknowledge Kay Crossley for her contribution to this study’s initial design, Axel Ström for statistical advice, and Lund University Humanities Lab for providing a test facility for data collection.
Footnotes
Twitter: @nae_jenny
Contributors: JN, MWC and EA planned the study. JN and AC collected the data. JN performed the visual assessments and data analysis. JN drafted the manuscript, and all the other authors revised the manuscript. All authors read and approved the final version of the manuscript.
Funding: This study was funded by the Governmental funding of clinical research within the National Health Services (ALF).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data will only be available on reasonable request due to the Swedish Ethical committee. Email the corresponding author, jenny.almqvist_nae@med.lu.se, to request the relevant data.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study was approved by The Regional Ethical Review Board, Lund, Sweden (2015/581).
References
- 1.van Melick N, van Cingel REH, Brooijmans F, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med 2016;50:1506–15. 10.1136/bjsports-2015-095898 [DOI] [PubMed] [Google Scholar]
- 2.Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol 2019;33:33–47. 10.1016/j.berh.2019.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horak FB. Postural orientation and equilibrium: what do we need to know about neural control of balance to prevent falls? Age Ageing 2006;35 Suppl 2:ii7–11. 10.1093/ageing/afl077 [DOI] [PubMed] [Google Scholar]
- 4.Nae J, Creaby MW, Nilsson G, et al. Measurement properties of a test battery to assess postural orientation during functional tasks in patients undergoing anterior cruciate ligament injury rehabilitation. J Orthop Sports Phys Ther 2017;47:863–73. 10.2519/jospt.2017.7270 [DOI] [PubMed] [Google Scholar]
- 5.Nae J, Creaby MW, Ageberg E. Extended version of a test battery for visual assessment of postural orientation errors: face validity, internal consistency, and reliability. Phys Ther 2020;100:1542–56. 10.1093/ptj/pzaa092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med 2010;38:1968–78. 10.1177/0363546510376053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med 2005;33:492–501. 10.1177/0363546504269591 [DOI] [PubMed] [Google Scholar]
- 8.Montalvo AM, Schneider DK, Yut L, et al. "What's my risk of sustaining an ACL injury while playing sports?" A systematic review with meta-analysis. Br J Sports Med 2019;53:1003–12. 10.1136/bjsports-2016-096274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cronström A, Creaby MW, Nae J, et al. Gender differences in knee abduction during weight-bearing activities: a systematic review and meta-analysis. Gait Posture 2016;49:315–28. 10.1016/j.gaitpost.2016.07.107 [DOI] [PubMed] [Google Scholar]
- 10.Cronström A, Ageberg E, Franettovich Smith MM, et al. Factors affecting knee abduction during weight-bearing activities in individuals with anterior cruciate ligament reconstruction. Phys Ther Sport 2019;38:8–15. 10.1016/j.ptsp.2019.04.006 [DOI] [PubMed] [Google Scholar]
- 11.Cronström A, Ageberg E. Association between sensory function and medio-lateral knee position during functional tasks in patients with anterior cruciate ligament injury. BMC Musculoskelet Disord 2014;15:430. 10.1186/1471-2474-15-430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Webster KE, Hewett TE. What is the evidence for and validity of Return-to-Sport testing after anterior cruciate ligament reconstruction surgery? A systematic review and meta-analysis. Sports Med 2019;49:917–29. 10.1007/s40279-019-01093-x [DOI] [PubMed] [Google Scholar]
- 13.Losciale JM, Bullock G, Cromwell C, et al. Hop testing lacks strong association with key outcome variables after primary anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 2020;48:511–22. 10.1177/0363546519838794 [DOI] [PubMed] [Google Scholar]
- 14.Palmieri-Smith RM, Lepley LK. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am J Sports Med 2015;43:1662–9. 10.1177/0363546515578252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Flosadottir V, Roos EM, Ageberg E. Muscle function is associated with future patient-reported outcomes in young adults with ACL injury. BMJ Open Sport Exerc Med 2016;2:e000154. 10.1136/bmjsem-2016-000154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Trulsson A, Roos EM, Ageberg E, et al. Relationships between postural orientation and self reported function, hop performance and muscle power in subjects with anterior cruciate ligament injury. BMC Musculoskelet Disord 2010;11:143. 10.1186/1471-2474-11-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ageberg E, Forssblad M, Herbertsson P, et al. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. Am J Sports Med 2010;38:1334–42. 10.1177/0363546510361218 [DOI] [PubMed] [Google Scholar]
- 18.Tan SHS, Lau BPH, Khin LW, et al. The importance of patient sex in the outcomes of anterior cruciate ligament reconstructions: a systematic review and meta-analysis. Am J Sports Med 2016;44:242–54. 10.1177/0363546515573008 [DOI] [PubMed] [Google Scholar]
- 19.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Epidemiology 2007;18:805–35. 10.1097/EDE.0b013e3181577511 [DOI] [PubMed] [Google Scholar]
- 20.Reid A, Birmingham TB, Stratford PW, et al. Hop testing provides a reliable and valid outcome measure during rehabilitation after anterior cruciate ligament reconstruction. Phys Ther 2007;87:337–49. 10.2522/ptj.20060143 [DOI] [PubMed] [Google Scholar]
- 21.Itoh H, Kurosaka M, Yoshiya S, et al. Evaluation of functional deficits determined by four different hop tests in patients with anterior cruciate ligament deficiency. Knee Surg Sports Traumatol Arthrosc 1998;6:241–5. 10.1007/s001670050106 [DOI] [PubMed] [Google Scholar]
- 22.Gustavsson A, Neeter C, Thomeé P, et al. A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2006;14:778–88. 10.1007/s00167-006-0045-6 [DOI] [PubMed] [Google Scholar]
- 23.Roos EM, Lohmander LS. The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003;1:64. 10.1186/1477-7525-1-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mohtadi N. Development and validation of the quality of life outcome measure (questionnaire) for chronic anterior cruciate ligament deficiency. Am J Sports Med 1998;26:350–9. 10.1177/03635465980260030201 [DOI] [PubMed] [Google Scholar]
- 25.Thomeé P, Währborg P, Börjesson M, et al. A new instrument for measuring self-efficacy in patients with an anterior cruciate ligament injury. Scand J Med Sci Sports 2006;16:181–7. 10.1111/j.1600-0838.2005.00472.x [DOI] [PubMed] [Google Scholar]
- 26.Kostogiannis I, Ageberg E, Neuman P, et al. Activity level and subjective knee function 15 years after anterior cruciate ligament injury: a prospective, longitudinal study of nonreconstructed patients. Am J Sports Med 2007;35:1135–43. 10.1177/0363546507299238 [DOI] [PubMed] [Google Scholar]
- 27.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes 2003;1:17. 10.1186/1477-7525-1-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roos EM, Roos HP, Ekdahl C, et al. Knee injury and Osteoarthritis Outcome Score (KOOS)--validation of a Swedish version. Scand J Med Sci Sports 1998;8:439–48. 10.1111/j.1600-0838.1998.tb00465.x [DOI] [PubMed] [Google Scholar]
- 29.Kvist J. Översättning, validitets och reliabilitetstestning AV ACL‐QOL frågeformulär Om livskvalitet efter främre korsbandsskada. Svensk Idrottsmedicinsl förenings Vårmöte. Örebro, Sweden, 2006. [Google Scholar]
- 30.Cohen J. Statistical power analysis for the behavioral sciences. 2nd edition. New Jersey: Lawrence Erlbaum Associates, Inc, 1988. [Google Scholar]
- 31.Padua DA, Marshall SW, Boling MC, et al. The landing error scoring system (less) is a valid and reliable clinical assessment tool of jump-landing biomechanics: the JUMP-ACL study. Am J Sports Med 2009;37:1996–2002. 10.1177/0363546509343200 [DOI] [PubMed] [Google Scholar]
- 32.Kuenze CM, Trigsted S, Lisee C, et al. Sex differences on the landing error scoring system among individuals with anterior cruciate ligament reconstruction. J Athl Train 2018;53:837–43. 10.4085/1062-6050-459-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ro DH, Lee DY, Moon G, et al. Sex differences in knee joint loading: cross-sectional study in geriatric population. J Orthop Res 2017;35:1283–9. 10.1002/jor.23374 [DOI] [PubMed] [Google Scholar]
- 34.Pantano KJ, White SC, Gilchrist LA, et al. Differences in peak knee valgus angles between individuals with high and low Q-angles during a single limb squat. Clin Biomech 2005;20:966–72. 10.1016/j.clinbiomech.2005.05.008 [DOI] [PubMed] [Google Scholar]
- 35.Baggaley M, Noehren B, Clasey JL, et al. Frontal plane kinematics of the hip during running: are they related to hip anatomy and strength? Gait Posture 2015;42:505–10. 10.1016/j.gaitpost.2015.07.064 [DOI] [PubMed] [Google Scholar]
- 36.Cronström A, Creaby MW, Nae J, et al. Modifiable factors associated with knee abduction during weight-bearing activities: a systematic review and meta-analysis. Sports Med 2016;46:1647–62. 10.1007/s40279-016-0519-8 [DOI] [PubMed] [Google Scholar]
- 37.Norouzi S, Esfandiarpour F, Mehdizadeh S, et al. Lower extremity kinematic analysis in male athletes with unilateral anterior cruciate reconstruction in a jump-landing task and its association with return to sport criteria. BMC Musculoskelet Disord 2019;20:492. 10.1186/s12891-019-2893-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Casartelli NC, Maffiuletti NA, Brunner R, et al. Clinical rating of Movement-Pattern quality in patients with femoroacetabular impingement syndrome: a methodological study. J Orthop Sports Phys Ther 2018;48:260–9. 10.2519/jospt.2018.7840 [DOI] [PubMed] [Google Scholar]
- 39.Naili JE, Esbjörnsson A-C, Iversen MD, et al. The impact of symptomatic knee osteoarthritis on overall gait pattern deviations and its association with performance-based measures and patient-reported outcomes. Knee 2017;24:536–46. 10.1016/j.knee.2017.02.006 [DOI] [PubMed] [Google Scholar]
- 40.Ithurburn MP, Paterno MV, Ford KR, et al. Young athletes after anterior cruciate ligament reconstruction with Single-Leg landing asymmetries at the time of return to sport demonstrate decreased knee function 2 years later. Am J Sports Med 2017;45:2604–13. 10.1177/0363546517708996 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will only be available on reasonable request due to the Swedish Ethical committee. Email the corresponding author, jenny.almqvist_nae@med.lu.se, to request the relevant data.