Abstract
Poroid hidradenoma (PH) is a rare benign tumor that shows differentiation of the eccrine sweat gland. It occurs mainly in adults, presenting as a 0.5 to 2 cm-sized intradermal nodule, mostly on the head, extremities, trunk and neck. We report two rare cases of PH, one on the face and the other on the heel. The first patient was a 50-year-old male who had a solitary, skin-colored nodule on his right temple for 6 months. The second patient was a 67-year-old female who presented with a solitary, bean-sized, tender nodule on her left heel for 1 year. The common histological examination finding was a well-circumscribed tumor composed of solid portions and large cystic spaces in the center. The tumor cells consisted of small, monomorphic poroid cells and large cuticular cells in both cases. To our knowledge, only few cases of PH have been reported. Herein, we report two rare cases of PHs with literature review.
Keywords: Cuticular, Eccrine, Hidradenoma, Poroid
INTRODUCTION
Poroid hidradenoma (PH) is a benign neoplasm with eccrine differentiation1. Typically, PH is a solitary tender nodule with a diameter ranging from 0.5 to 2 cm. It appears skin-colored or slightly reddish, but the presence of cystic parts may confer a blue color on the lesion. It has both solid and cystic components and is restricted within the dermis2. We present rare cases of PH in two patients.
CASE REPORT
Case 1
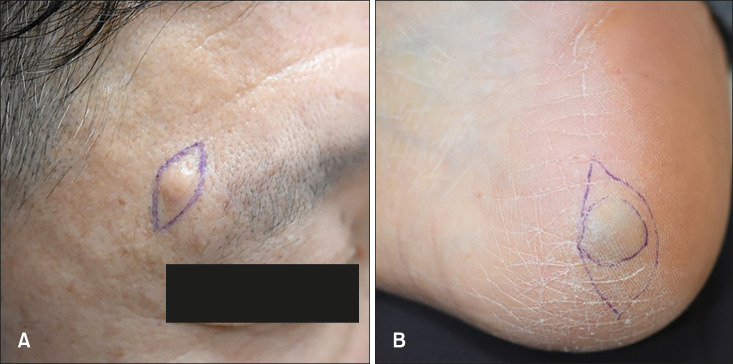
A 50-year-old male presented with a solitary skin-colored nodule on his right temple. The patient recalled first noticing the lesion 6 months before. The lesion had increased in size, but the patient did not complain of tenderness or other subjective symptoms. He had a history of nephrotic syndrome and no history of trauma in the area of the skin lesion. He had no relevant social and family histories. Physical examination revealed a bean-sized, skin-colored, indurated nodule arising from the right temple (Fig. 1A).
Fig. 1. (A) Case 1: A 50-year-old male with a solitary skin-colored nodule on the right temple. (B) Case 2: A 67-year-old female with a 1.5 cm-sized, bluish indurated nodule arising from her left heel.
Case 2
The second case was a 67-year-old female who presented with a solitary tender nodule on her left heel. The lesion had appeared 1 year prior and slowly enlarged over 3 months. The patient had a history of hypertension and no history of trauma in her skin lesion. She had no relevant social and family histories. Physical examination revealed a 1.5 cm-sized, bluish indurated nodule arising from the left heel (Fig. 1B).
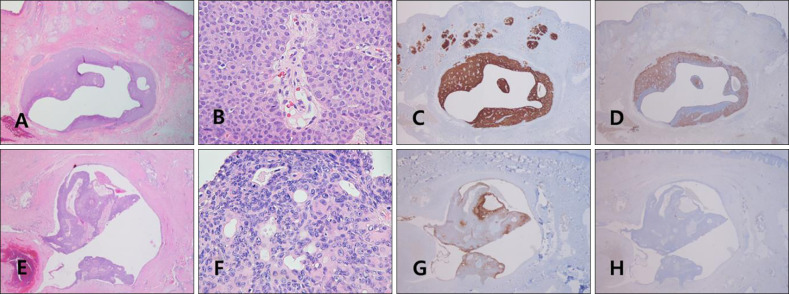
Histological examination of two specimens revealed well-circumscribed tumors composed of solid portions and large cystic spaces. Tumors were confined entirely to the dermis and no epidermal connection could be seen. Ductal lumens were filled with eosinophilic materials, They consisted of smaller monomorphic poroid cells with round-to-oval nuclei and larger cuticular cells with a pale cytoplasm in both cases (Fig. 2). In an immunohistochemical study, carcinoembryonic antigen (CEA) and epithelial membrane antigen (EMA) were both positive in the solid portions and ductal structures in the first case. In the second case, only EMA was positive (Fig. 2). We received the patient's consent form about publishing all photographic materials.
Fig. 2. (A~D) Case 1. (E~H) Case 2. (A) A well-circumscribed tumor composed of solid and cystic components in the mid-dermis and no epidermal connection could be seen (H&E, ×40). (B) Ductal structures are lined by cuticular cells and some poroid cells could be observed (H&E, ×200). (C) A tumor showed positive for epithelial membrane antigen (EMA; ×40). (D) A tumor showed positive for carcinoembryonic antigen (CEA; ×40). (E) A tumor composed of soild and cystic components with no epidermal connection (H&E, ×40). (F) Poroid cells and cuticular cells were mixed in the solid portion of tumors and ductal lumens were filled with eosinophilic materials (H&E, ×200). (G) A tumor showed positive for EMA (×40). (H) A tumor showed negative for CEA (×40).
DISCUSSION
PH is a form of hidradenoma with eccrine differentiation according to the WHO classifications of skin tumors1. The age of onset ranges widely, with a peak incidence in the seventh decade of life3. No sex or ethnic predilection was reported. The most predominant site of involvement is the head and neck region, followed by the axilla, trunk, and extremities4. Miller et al.1 reported the systematic reviews of PH, which occur more commonly in male, in the head and neck region or limbs. Considering that these neoplasms can be generally asymptomatic or accompanied by mild tenderness, the incidence of PHs might be underestimated in the literature5.
Hidradenomas have traditionally been considered to exhibit eccrine differentiation based on histochemical and electron microscopic features2. However, recently, subclassification of hidradenomas into two groups, those with apocrine differentiation (known as clear cell hidradenoma) and those exhibiting eccrine differentiation (known as PH), was suggetsted6. The former accounts for 95% of all hidradenomas and is composed of clear, polygonal, and mucinous cells with apocrine differentiation. The latter neoplasm, which constitutes 5% of hidradenomas, is characterized by a single or multilobulated dermal nodule with no connection to the epidermis and consists of two cell types, poroid and cuticular cells with eccrine differentiation.
Histopathological examination revealed that PH presents solid and cystic components, and tumor cells restricted to the dermis7. The tumor is composed of two types of cells, poroid and cuticular cells. Poroid cells are uniform, small cuboidal cells with an oval-to-round nuclei. Cuticular cells have an abundant eosinophilic cytoplasm with a larger nucleus that shows occasional multinucleation. The cystic spaces are considered as eccrine dilated ducts containing eccrine secretory fluid.
In immunohistochemical studies, epithelial markers such as EMA and cytokeratin are considered related to the cells of the dermal sweat ducts5. EMA demonstrates eccrine differentiation7. CEA, a sensitive marker of cutaneous adnexal tumors, can also be positive.
The distribution of the lesions varied between the tumor groups. In our literature review, PHs are mostly predominant in the trunk and are not found on the plantar aspect of the foot (Table 1)2. A second patient with PH in the plantar area of the foot will be the rare case worldwide.
Table 1. The locations of patients with poroid hidradenoma worldwide including our cases.
| Site of the lesion | Number (%) |
|---|---|
| Trunk | 21 (33) |
| Upper limb | 13 (21) |
| Palm | 0 (0) |
| Lower limb | 11 (17) |
| Plantar aspect of foot (our case) | 1 (1) |
| Head and neck (our case) | 12 (19) |
| Another site | 4 (6) |
PHs are mostly covered with intact skin; however, approximately 15% of these neoplasms demonstrate ulceration at presentation due to direct trauma or abrasion to the mass2. PHs can have a bluish aspect, probably due to the Tyndall effect of the cystic components within the tumors5. This confounds the clinician in distinguishing between PH, angioma, melanoma and nevus.
The differential diagnosis of PH includes other poromas (hidroacanthoma simplex, dermal duct tumor, eccrine poroma) and apocrine hidradenomas8. Hidroacanthoma simplex is characterized by nests of round cells within normal epidermal cells. Dermal duct tumor is same histopathologic features, but located in the dermis. Eccrine poroma is clear margin between normal epidermal keratinocytes and cuboidal cells with dark nuclei protrudes into the underlying dermis. Apocrine hidradenomas are characterized by mucinous, polygonal and clear cells, and decapitation secretion into the ducts with apocrine differentiation8. In addition, some benign subcutaneous neoplasms such as fibroma, fibrolipoma, dermatofibroma, hemangioma, pyogenic granuloma, epidermal cyst, and basal cell epithelioma might be confused with this neoplasm8. Therefore, histological examination with a skin biopsy is crucial for the diagnosis of PH.
PH is treated with total excision of the lesion, which is usually curative. These neoplasms are considered benign, because the risk of malignant transformation is less than 1%9. Furthermore, the prognosis of PH is relatively good, and recurrence has rarely been reported2. Our patients had no complications or recurrence 3 months after the excision.
Until now, only few cases of PHs have been reported. Since 1990, rare cases of PHs have been reported in the literature and only 3 case reports have been published in Korea (Table 2)10,11,12. In these reports, the clinical features of patients were similar with those of our patients, except the anatomical sites (thigh, shin, back). Herein, we report two rare cases of PHs.
Table 2. Previous reported cases of poroid hidradenomas in Korean literature.
| Case no. | Age (yr)/sex | Trauma history | Duration (yr) | Clinical feature | Site | Author |
|---|---|---|---|---|---|---|
| 1 | 51/Female | - | 1 | A solitary bluish nodule | Right thigh | Park et al. (2005)10 |
| 2 | 55/Female | - | 3 | A solitary bluish nodule | Left shin | Kim et al. (2007)11 |
| 3 | 79/Female | - | 1 | A solitary reddish to bluish nodule | Back | Kim et al. (2015)12 |
| Our case 1 | 50/Male | - | 0.5 | A solitary skin-colored nodule | Right temple | |
| Our case 2 | 67/Female | - | 1 | A solitary bluish nodule | Left heel |
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
FUNDING SOURCE: None.
DATA SHARING STATEMENT
Research data are not shared.
References
- 1.Miller R, Ieremia E, Birch J, Chan J. Poroid hidradenoma in the hand: a case report and systematic review. J Cutan Pathol. 2018;45:696–700. doi: 10.1111/cup.13282. [DOI] [PubMed] [Google Scholar]
- 2.Whitmore RM, Anderson CJ, Piper T. Poroid hidradenoma. A case presentation. J Am Podiatr Med Assoc. 1998;88:510–513. doi: 10.7547/87507315-88-10-510. [DOI] [PubMed] [Google Scholar]
- 3.Delfino S, Toto V, Brunetti B, Di Marino MP, Baldi A, Persichetti P. Poroid hidradenoma: a case report. In Vivo. 2007;21:905–907. [PubMed] [Google Scholar]
- 4.Ueno T, Mitsuishi T, Kawana S. Poroid hidradenoma: a case report with review of Japanese published work. J Dermatol. 2007;34:495–497. doi: 10.1111/j.1346-8138.2007.00319.x. [DOI] [PubMed] [Google Scholar]
- 5.Liu HN, Chang YT, Chen CC, Huang CH. Histopathological and immunohistochemical studies of poroid hidradenoma. Arch Dermatol Res. 2006;297:319–323. doi: 10.1007/s00403-005-0606-4. [DOI] [PubMed] [Google Scholar]
- 6.Nandeesh BN, Rajalakshmi T. A study of histopathologic spectrum of nodular hidradenoma. Am J Dermatopathol. 2012;34:461–470. doi: 10.1097/DAD.0b013e31821a4d33. [DOI] [PubMed] [Google Scholar]
- 7.Requena L, Sánchez M. Poroid hidradenoma: a light microscopic and immunohistochemical study. Cutis. 1992;50:43–46. [PubMed] [Google Scholar]
- 8.Battistella M, Langbein L, Peltre B, Cribier B. From hidroacanthoma simplex to poroid hidradenoma: clinicopathologic and immunohistochemic study of poroid neoplasms and reappraisal of their histogenesis. Am J Dermatopathol. 2010;32:459–468. doi: 10.1097/DAD.0b013e3181bc91ff. [DOI] [PubMed] [Google Scholar]
- 9.Chiu HH, Lan CC, Wu CS, Chen GS, Tsai KB, Chen PH. A single lesion showing features of pigmented eccrine poroma and poroid hidradenoma. J Cutan Pathol. 2008;35:861–865. doi: 10.1111/j.1600-0560.2007.00909.x. [DOI] [PubMed] [Google Scholar]
- 10.Park KT, Ahn YS, Kim JS, Yu HJ, Park YW. A case of poroid hidradenoma. Korean J Dermatol. 2005;43:1142–1144. [Google Scholar]
- 11.Kim DH, Song JY, Choi KC, Chung BS. A case of poroid hidradenoma. Korean J Dermatol. 2007;45:1109–1111. [Google Scholar]
- 12.Kim DJ, Baek JH, Lee DY, Lee SK, Kim MS, Lee UH, et al. A case of poroid hidradenoma. Korean J Dermatol. 2015;53:230–234. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Research data are not shared.