Abstract
Introduction
The lockdown period due to the coronavirus disease 2019 (COVID-19) in Spain probably had a significant emotional impact on chronic patients and hence on those who are suffering from inflammatory bowel disease (IBD) due to their high risk of emotional disorders. The aim of this study was to learn how COVID-19 influenced patients suffering from IBD during the quarantine period, focusing in particular on psychological distress through the Perceived Stress Scale-10 (PSS-10) and also the impact of the pandemic on therapeutic adherence using the Visual Analogue Scale (VAS).
Patients and methods
A prospective, single-centre and analytical observational study was carried out in the IBD unit in August 2020. Patients were contacted and interviewed by phone. A descriptive analysis was carried out and subsequently the factors associated with the loss of therapeutic adherence and higher-moderate levels of stress were analyzed through logistic regression multivariate analyses.
Results
A total of 426 patients were included with a median PSS-10 score of 12 (10–16). A higher level of stress was reported by those who were not married, women and those who experienced an increase in IBD-related symptoms. Adherence to treatment was not associated with stress based on the PSS-10 questionnaire.
Conclusions
Although the lockdown period due to the COVID-19 pandemic has probably had a significant emotional impact on Spaniards with IBD, IBD patients in general had lower PSS-10 scores.
Keywords: SARS-CoV-2, Perceived stress, Therapeutic adherence, Inflammatory bowel disease
Abstract
Introducción
El confinamiento debido a la pandemia por COVID-19 en España tuvo probablemente un importante impacto emocional en los pacientes crónicos, y por tanto en aquellos que sufren enfermedad inflamatoria intestinal (EII) debido a su riesgo incrementado de padecer desórdenes emocionales. El objetivo de este estudio es el de conocer como la COVID-19 ha influido a los pacientes con EII durante el período de cuarentena, haciendo hincapié en el nivel de estrés a través de la Escala de Estrés Percibido (PSS-10) así como en la adherencia a los tratamientos por medio de la escala visual analógica (VAS).
Pacientes y métodos
Estudio prospectivo, unicéntrico y observacional realizado en la Unidad de EII durante el mes de agosto de 2020. Los pacientes fueron entrevistados por teléfono. Se llevó a cabo un análisis descriptivo inicial, posteriormente se identificaron los factores relacionados con la pérdida de adherencia, así como con los niveles altos-moderados de estrés a través de análisis de regresión logística multivariante.
Resultados
Fueron incluidos un total de 426 pacientes con una puntuación media en la escala PSS-10 de 12 (10-16). Los niveles más altos de estrés se reportaron en aquellos pacientes que no estaban casados, las mujeres o aquellos que habían incrementado sintomatología relacionada con su EII. La adherencia al tratamiento no se asoció con el nivel de estrés basado en el cuestionario PSS-10.
Conclusiones
A pesar de que el período de cuarentena por COVID-19 haya podido tener un importante papel en el impacto emocional de la población española con EII, los pacientes con EII tuvieron en general niveles bajos según el cuestionario PSS-10.
Palabras clave: SARS-CoV-2, Estrés percibido, Adherencia terapéutica, Enfermedad inflamatoria intestinal
Introduction
The coronavirus disease 2019 (COVID-2019), caused by “Severe Acute Respiratory Syndrome Coronavirus 2” (SARS-CoV-2) and its very fast worldwide diffusion triggered that World Health Association (WHO) declared a world state of emergency on January 30th, 2020, and a pandemic on March 11th, 2020. Nowadays, in accordance with John Hopkins University data, the SARS-CoV2 has induced more than 46,600,000 of documented infections and more than 1,200,000 directly attributed deaths.1
Since the beginning of the pandemic, significant COVID-19 epicentres included China, Italy, Spain, France, South Korea, Iran, Japan and Germany among others were noticed. As these different countries passed through the stages of the outbreak, different approaches to reach COVID-19 containment were put in place with the aim of reducing human-to-human transmission.2
In Spain, one of the most affected countries at the onset of the pandemic, very strict attitudes to prevent the spread of the disease were adopted by declaring a nationwide state of alert on March 14th. From 16th March to 21st of June, a population lockdown was imposed. Hence the authorities controlled personal movements, public gatherings were cancelled, schools were closed, and so were most of private and public non-essential businesses. Similar measures were implemented as in the 2003 SARS epidemic was done.3
This situation of isolation by an unknown and potentially serious disease has been able to have an important emotional impact on the general population and probably this impact may have been greater on patients with chronic health conditions as inflammatory bowel disease (IBD). Special attention deserved patients treated with biologics or inmmunomodulators agents that have more aggressive IBD and a potential increased risk of serious infections. Some factors such as psychological distress, employment situation, patient's beliefs about medication and doctor-patient discordance have been noticed previously as some reasons of non-adherence to medication in IBD patients,4 and COVID-19 pandemic may also have had a negative influence in these factors.
Therefore, the aim of this study is to know how COVID 19 has influenced to the patients suffering with IBD during the quarantine period, focusing heavily on the psychological distress and adherence to medications.
Patients and methods
Subject selection and recruitment
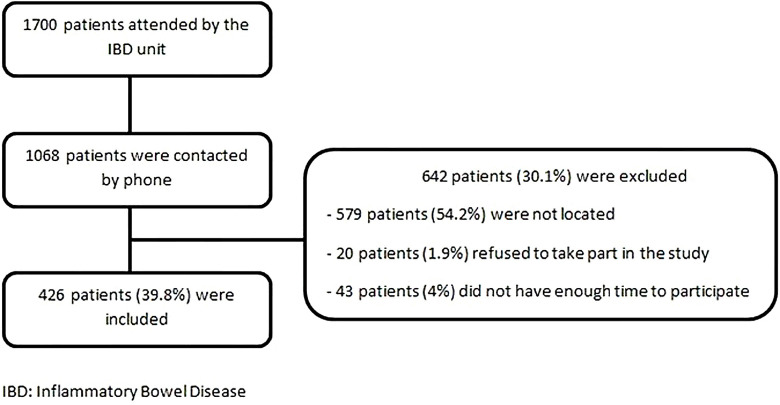
This investigation is a prospective, unicentric and analytical observational study conducted in a public large teaching Hospital integrated into the Spanish National Health System (University Hospital “Lozano Blesa”). Patients were recruited from the IBD Unit and all of them had previously been registered in ENEIDA (Nationwide study on genetic and environmental determinants of inflammatory bowel disease) database.5 During August of 2020, patients were contacted by telephone by two trained researchers not involved in the patient's medical care. Inclusion criteria were age ≥18 years old and clinic, endoscopic/imaging and histological diagnosis of Crohn's Disease (CD), Ulcerative Colitis (UC) or Indeterminate Colitis (IC) for at least 6 months. See Fig. 1 .
Figure 1.
Recruitment of study population (flow chart).
Variables
Some variables were obtained by ENEIDA database (gender, age, medical history, IBD type and treatment) and others by telephone interview (civil status, educational level, smoking habit, patient–physician relationship, employment and economic situation). During telephone interview, patients were also asked about symptoms related to IBD or COVID-19 disease.
Definition of confirmed and probable SARS-CoV-2 infection
Confirmed SARS-CoV-2 infection was defined when the patient had a positive SARS-CoV-2 CRP analysis.
Probable SARS-CoV-2 infection was defined when a person had fever with one or more symptoms of lower respiratory track and no alternative diagnosis could explain the symptoms but SARS-CoV-2 CRP analysis was not performed. This definition arises in the context of the beginning of pandemic, in which the capacity to carry out CRP in Spain was low due to lack of resources and a diagnosis by clinical criteria was chosen in patients who did not require hospitalization.
Instruments used to assess perceived stress and therapeutic adherence
The emotional impact and psychological symptoms associated with the lockdown period were evaluated using the Perceived Stress Scale-10 (PSS-10), with a range of 0–40 points. The original Perceived Stress Scale consists of 14 items with a 5-point response scale (0 = never, 1 = almost never, 2 = once in a while, 3 = often, 4 = very often).6, 7 In accordance with the guidelines from the original author, the short 10-item version can be created and obtained by reversing the scores of the four positive items (items 6, 7, 8 and 9) and then summing across all 10 items (1, 2, 3, 6, 7, 8, 9, 10, 11, and 14). This short version has previously showed a reliable and valid measure of perceived stress in Spanish population, where higher scores reflect higher levels of stress. Scores ranging from 0–13 would be considered low stress, from 14–26 moderate stress and scores from 27 to 40 high perceived stress.8
Therapeutic Adherence was measured using Visual Analogue Scale (VAS), considering an optimal therapeutic adherence ≥80% (range between 0 and 100%).9 For statistical analysis, it was considered to have therapeutic adherence if VAS ≥80% and lack of therapeutic adherence if VAS <80%.
Statistical analysis
Data were analyzed using SPSS 26.0 (SPSS Ibérica, Madrid, Spain). Clinical and demographic characteristics of the sample are presented as absolute and relative frequencies (n (%)). Perceived Stress Score is expressed with median and interquartile range (IQR). Normal distribution was assessed by Kolmogorov-Smirnov test, where p ≥ 0.05 means normality. To study the relationship of qualitative variables we used Chi-square or Fisher test. In the case of quantitative variables Student's t Test or Mann–Whitney U Test were used. A p value <0.05 was considered statistically significant. To study the level of perceived stress and its related factors, patients with severe and moderate level of stress were analyzed as part of the same group. The factors associated with the loss of therapeutic adherence and higher-moderate levels of stress were analyzed through Logistic regression multivariate analyses.
Ethical considerations
Participants had previously given their consent to be included in ENEIDA database. Moreover, this study was also approved by the Aragon Clinical Research Ethics Committee (CEICA) on July 29th 2020 (C.I. PI20/386). Patients were explained that every data that they provide was confidential and subject to anonymization. The study was carried out in accordance with recommendations of Declaration of Helsinki.
Results
Clinical and demographic characteristic of the study population
Of the 1700 patients who are under medical follow up in our IBD Unit, 1068 were contacted by phone. Finally, 426 (39.8%) patients were included in the study. Fig. 1 shows the reasons for exclusion of the patients not include.
Clinical and demographic characteristics of the patients were shown in Table 1 . During the Spanish lockdown period of the COVID-19 pandemic, most of patients have not symptoms related to their IBD (307; 72.1%). Among those who have symptoms (119; 27.9%), the most frequent was diarrhoea and abdominal pain (49; 11.5%), followed by bloody stools (25; 5.9%), increased number of stools without blood (24; 5.6%) and isolated abdominal pain (21; 4.9%).
Table 1.
Clinical and demographic characteristics of study population.
| n (%) | |
|---|---|
| Gender | |
| Women | 217 (50.9) |
| Age | |
| 18–24 | 3 (0.7) |
| 25–34 | 43 (10.1) |
| 35–44 | 86 (20.2) |
| 45–54 | 111 (26.1) |
| 55–64 | 99 (23.2) |
| 65–80 | 84 (19.7) |
| Civil status | |
| Married | 280 (65.7) |
| Divorced | 28 (6.6) |
| Single | 99 (23.2) |
| Widower | 19 (4.5) |
| Educational level | |
| None | 8 (1.9) |
| Primary studies | 91 (21.2) |
| Secondary education | 116 (27.2) |
| Superior or university studies | 211 (49.5) |
| Smoking habit | |
| Yes | 84 (19.7) |
| No | 342 (80.3) |
| Comorbidities | |
| Yes | 160 (37.6) |
| No | 266 (62.4) |
| Type of IBD | |
| UC | 249 (58.4) |
| CD | 177 (41.6) |
| IBD treatment | |
| None | 65 (15.3) |
| Corticosteroids | 6 (1.4) |
| 5-ASA | 166 (39) |
| Methotrexate | 4 (0.9) |
| Azathioprine | 51 (12) |
| Anti-TNF | 35 (8.2) |
| Vedolizumab | 7 (1.6) |
| Ustekinumab | 28 (6.6) |
| Biologic agent + other drug | 64 (15) |
| Socioeconomic level | |
| Working full time | 226 (53.1) |
| Unemployed | 67 (15.7) |
| Temporal job reduction | 9 (2.1) |
| Part-time employment | 10 (2.3) |
| Retired | 109 (25.6) |
| Student | 5 (1.2) |
CD: Crohn's Disease. IBD: inflammatory bowel disease, IC: Indeterminate Colitis. n (%): frequency (percentage), UC: Ulcerative Colitis.
Most of subjects were not diagnosed of SARS-COV-2 infection (396; 93%). However, 9 patients (2.1%) suffered confirmed infection and 21 of them (4.9%) had compatible symptoms without test confirmation. Furthermore, 356 patients (83.6%) did not have relatives or close friends infected by SARS-COV-2 whereas 50 (11.7%) of them had relatives or close friends who recovered at home, 9 (2.1%) in hospital and 11 patients (2.6%) suffered deaths in their close circle.
Regarding economic situation of included patients, most of them do not have economic difficulties (373; 87.6%) whereas 32 (7.5%) occasionally have them, 14 (3.3%) half of the year and 7 (1.6%) have economic difficulties monthly.
Finally, the majority of participants refer a very good patient–physician relationship (317; 74.4%). 93 patients (21.8%) refer a good relationship, 14 (3.3%) improvable and 2 (0.5%) of them refer bad relationship. On the other hand, the physician's view of the relationship is unknown.
Perceived stress level of IBD patients during COVID-19 lockdown in Spain
People who participated in the study had a median PSS-10 score of 12.10, 11, 12, 13, 14, 15, 16 Most of them had low level of perceived stress (265 (62.2%)) compared to those who had moderate or high level (161 (37.8%)). The answers for each question of PSS-10 scale are showed in Table 2 .
Table 2.
PSS-10 questionnaire answers by item.
| PSS-10 questionnaire | Answers n (%) |
|||||
|---|---|---|---|---|---|---|
| In the last month, how often have you… | 0 |
1 |
2 |
3 |
4 |
|
| Never | Almost never | Sometimes | Fairly often | Very often | ||
| 1 | Been upset because of something that happened unexpectedly? | 50 (11.7) | 233 (54.7) | 105 (24.6) | 37 (8.7) | 1 (0.2) |
| 2 | Felt that you were unable to control the important things in your life? | 40 (9.4) | 266 (62.4) | 74 (17.4) | 44 (10.3) | 2 (0.5) |
| 3 | Felt nervous and stressed? | 22 (5.2) | 85 (20) | 194 (45.5) | 120 (28.2) | 5 (1.2) |
| 4 | Felt confident about your ability to handle your personal problems? * | 4 (0.9) | 15 (3.5) | 71 (16.7) | 268 (62.9) | 68 (16) |
| 5 | Felt that things were going your way?* | 2 (0.5) | 15 (3.5) | 57 (13.4) | 271 (63.9) | 81 (19) |
| 6 | Found that you could not cope with all the things that you had to do? | 29 (6.8) | 277 (65) | 88 (20.7) | 31 (7.3) | 1 (0.2) |
| 7 | Been able to control irritations in yourlife?* | 3 (0.7) | 11 (2.6) | 87 (20.4) | 262 (61.5) | 63 (14.8) |
| 8 | Felt that you were on top of things?* | 1 (0.2) | 19 (4.5) | 79 (18.5) | 265 (62.2) | 62 (14.6) |
| 9 | Been angered because of things that happened that were outside of your control? | 32 (7.5) | 235 (55.2) | 123 (28.9) | 35 (8.2) | 1 (0.2) |
| 10 | Felt difficulties were piling up so high that you could not overcome them? | 24 (5.6) | 220 (51.6) | 153 (35.9) | 29 (6.8) | 0 (0) |
On these 4 questions the scores are changed as followed: 0 = 4, 1 = 3, 2 = 2, 3 = 1 and 4 = 0.
The level of perceived stress was more severe in woman, unmarried and among patients with active IBD (Table 3 ).
Table 3.
Factors associated with the level of Perceived Stress (PSS-10 scale) in patients with IBD.
| PSS-10 Score |
Univariate* |
Multivariate** |
||||||
|---|---|---|---|---|---|---|---|---|
| Moderate/high | Low | RR | CI (95%) | p Value | OR | CI (95%) | p Value | |
| n (%) | n (%) | |||||||
| Age | ||||||||
| ≥45 | 112 (69.6) | 182 (68.7) | 0.484 | |||||
| <45 | 49 (30.4) | 83 (31.3) | ||||||
| Gender | ||||||||
| Women | 96 (59.6) | 121 (45.7) | 1.422 | 1.107–1.928 | 0.005 | 1.590 | 1.053–2.403 | 0.028 |
| Men | 65 (40.4) | 144 (54.3) | ||||||
| Civil status | ||||||||
| Non-married | 68 (42.2) | 78 (29.4) | 1.402 | 1.103–1.783 | 0.007 | 1.746 | 1.133–2.688 | 0.011 |
| Married | 93 (57.8) | 187 (70.6) | ||||||
| Educational level | ||||||||
| Superior/university | 77 (47.8) | 134 (50.6) | 0.583 | |||||
| Elemental/none | 84 (52.2) | 131 (49.4) | ||||||
| Employment status | ||||||||
| Unemployed | 83 (51.6) | 107 (40.4) | 1.322 | 1.037–1.685 | 0.024 | 1.369 | 0.886–2.096 | 0.159 |
| Working | 78 (48.4) | 158 (59.6) | ||||||
| Smoking habit | ||||||||
| Yes | 38 (23.6) | 46 (17.4) | 0.116 | |||||
| No | 123 (76.4) | 219 (82.6) | ||||||
| Comorbidity | ||||||||
| Yes | 72 (44.7) | 88 (33.2) | 1.345 | 1.057–1.711 | 0.017 | 1.471 | 0.952–2.273 | 0.082 |
| No | 89 (55.3) | 177 (66.8) | ||||||
| Type of IBD | ||||||||
| CD | 73 (45.3) | 104 (39.2) | 0.216 | |||||
| UC | 88 (54.7) | 161 (60.8) | ||||||
| Corticosteroids treatment | ||||||||
| Yes | 4 (2.5) | 2 (0.8) | 0.142 | |||||
| No | 157 (97.5) | 263 (99.2) | ||||||
| Biologic treatment | ||||||||
| Yes | 45 (28.0) | 89 (33.6) | 0.225 | |||||
| No | 116 (72.0) | 176 (66.4) | ||||||
| Worsening IBD symptoms | ||||||||
| Yes | 62 (38.5) | 57 (21.5) | 1.616 | 1.275–2.047 | <0.001 | 2.064 | 1.322–3.222 | 0.001 |
| No | 99 (61.5) | 208 (78.5) | ||||||
| Patient–physician relationship | ||||||||
| Bad | 9 (5.6) | 7 (2.6) | 0.121 | |||||
| Good | 152 (94.4) | 258 (97.4) | ||||||
| COVID infection (confirmed or suspected) | ||||||||
| Yes | 12 (7.5) | 18 (6.8) | 0.769 | |||||
| No | 149 (92.5) | 247 (93.2) | ||||||
| Relatives or close friends affected | ||||||||
| Yes | 33 (20.5) | 37 (14.0) | 0.078 | |||||
| No | 128 (79.5) | 228 (86.0) | ||||||
| Therapeutic adherence | ||||||||
| Yes | 122 (90.4) | 216 (92.7) | 0.430 | |||||
| No | 13 (9.6) | 17 (7.3) | ||||||
IBD: inflammatory bowel disease. UC: Ulcerative Colitis. N (%): number (frequency).
Chi-square test.
Logistic regression multivariate analysis.
Therapeutic adherence during COVID-19 lockdown
According to our analysis, the 79.3% of patients had an optimal therapeutic adherence to IBD treatment during COVID-19 quarantine (VAS ≥ 80%). Analyzing patients who were treated with biologics agents a higher percentage of therapeutic adherence has been found. On the other hand, between those who had superior studies a lower percentage of good therapeutic adherence has been detected as showed in Table 4 . There is no significant association between patient's perceived stress score and their adherence to treatment.
Table 4.
Therapeutic adherence in patients with IBD during COVID-19 pandemic in Spain.
| Variables | Therapeutic adherence |
Univariate* |
Multivariate** |
|||||
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | RR | CI (95%) | p Value | OR | CI (95%) | p Value | |
| Age | ||||||||
| <45 years | 9 (30) | 109 (32.2) | 0.800 | |||||
| ≥45 years | 21 (70) | 229 (67.8) | ||||||
| Gender | ||||||||
| Women | 12 (40) | 174 (51.5) | 0.228 | |||||
| Men | 18 (60) | 164 (48.5) | ||||||
| Civil status | ||||||||
| Other | 15 (50) | 109 (32.2) | 1.96 | 0.995–3.893 | 0.049 | 1.713 | 0.786–3.735 | 0.176 |
| Married | 15 (50) | 229 (67.8) | ||||||
| Educational level | ||||||||
| Superior | 20 (66.7) | 159 (47.0) | 2.112 | 1.017–4.387 | 0.039 | 2.296 | 1.014–5.198 | 0.046 |
| Elemental/none | 10 (33.3) | 179 (53) | ||||||
| Employment status | ||||||||
| Working | 22 (73.3) | 187 (55.3) | 0.056 | |||||
| Unemployed | 8 (26.7) | 151 (44.7) | ||||||
| Smoking habit | ||||||||
| Yes | 4 (13.3) | 64 (18.9) | 0.449 | |||||
| No | 26 (86.7) | 274 (81.1) | ||||||
| Comorbidities | ||||||||
| Yes | 9 (30) | 127 (37.6) | 0.410 | |||||
| No | 21 (70) | 211 (62.4) | ||||||
| Type of IBD | ||||||||
| EC | 8 (26.7) | 128 (37.9) | 0.223 | |||||
| CU | 22 (73.3) | 210 (62.1) | ||||||
| Corticosteroids treatment | ||||||||
| Yes | 1 (3.3) | 5 (1.5) | 0.442 | |||||
| No | 29 (96.7) | 333 (98.5) | ||||||
| Biologic treatment | ||||||||
| No | 26 (86.7) | 208 (61.5) | 3.722 | 1.327–10.437 | 0.006 | 4.110 | 1.375–12.289 | 0.011 |
| Yes | 4 (13.3) | 130 (38.5) | ||||||
| Worsening IBD symptoms | ||||||||
| No | 20 (66.7) | 249 (73.7) | 0.407 | |||||
| Yes | 10 (33.3) | 89 (26.3) | ||||||
| COVID infection (confirmed or suspected) | ||||||||
| Yes | 6 (20) | 22 (6.5) | 3.036 | 1.354–6.806 | 0.008 | 2.592 | 0.924–7.273 | 0.070 |
| No | 24 (80) | 316 (93.5) | ||||||
| Relatives or close friends affected | ||||||||
| Yes | 4 (13.3) | 61 (18) | 0.516 | |||||
| No | 26 (86.7) | 277 (82) | ||||||
| PSS-10 score | ||||||||
| Moderate/high level | 13 (43.3) | 122 (36.1) | 0.430 | |||||
| Low level | 17 (56.7) | 216 (63.9) | ||||||
IBD: inflammatory bowel disease. UC: Ulcerative Colitis. N (%): number (frequency).
Chi-square test.
Logistic regression multivariate analysis.
Discussion
In spite of the high amount of information about IBD patients and their management that is being published since the COVID-19 pandemic outbreak, no data about the emotional impact or adherence to medications and its consequences in those patients are available. The psychological management of patients with chronic diseases is always a clinical challenge considering the usual high incidence of emotional disorders, but it is even more complex in new situations as a pandemic and a lockdown period that can trigger significant stress and have an evident impact on their quality of life and also in their disease course.10, 11
In this study including 426 IBD patients we aimed to evaluate their perceived stress situation and the adherence to treatment during the lockdown period in Spain, one of the strictest worldwide.
IBD patients who participated in the study had a median PSS-10 score of 12,10, 11, 12, 13, 14, 15, 16 which mean surprisingly a low stress level. Perceived Stress has been reported previously in people who had suffered from the SARS epidemic in 2003 with a median PSS score of 20,12 which means a moderate level of perceived stress. This results persisted even one year later.7 Perceived stress has also been studied during COVID-19 pandemic among Spanish healthcare professionals with evident higher levels with a median of 31.6 in those who worked in an specific COVID-19 unit.13
The fact that most of IBD patients and their relatives did not suffer the COVID-19 infection could explain their lower perceived stress scores compared with COVID-19 patients and healthcare workers. Low perceived stress scores have been noticed in healthy control population in the COVID-19 outbreak,14, 15 and also in people with other pre-existing medical conditions.11 The fact that healthy people and IBD patients have a similar perceived stress score could be explained through the good patient–physician relationship that the study population have shown. However, this fact has not been studied before and more evidence is needed.
A higher level of stress have been reported in those IBD patients who were not married, women and among patients with active IBD.
Female patients have been pointed out before as an independent risk factor to a higher perceived stress score during the pandemic related with a significantly more “perceived helplessness”, which could also explain our results.14, 15 General population with an occasional couple (single, widowed or divorced)15 have showed higher scores in the same way as our IBD patients. However, it has not been showed in healthcare workers13 probably due to the fear of spreading the infection among their cohabitants.
Definitely, many of the daily activities and the way people related have changed in recent months during pandemic, at least temporarily. This fact became more evident during the lockdown, which may have influenced the emotional sphere of patients with IBD. The limitation of movements caused a decrease in physical activity, which is supposed to improve quality of life.19 Anxiety and depression have been noticed as important factors leading to a lower quality of live and thereby a worse course of the disease, which could lead to a further worsening of IBD symptoms as could have happened during the lockdown period.16 This highlights the connection between both physical and mental sphere 17, 18 and stresses the importance of taking patient's mental health into account.
Having IBD symptoms could be an important reason for a high level of perceived stress, as our analysis has reported.19 Moreover, patients with active disease have significantly higher prevalence of mood disorders compared to those in remision19 as have been noticed in other chronic diseases.20, 21
In our study, therapeutic adherence was also evaluated during the lockdown period among IBD patients. There are several ways to evaluate the adherence to different treatments. From all of them we chose VAS, which was identified as the best tool to assess adherence in IBD.6, 9 Despite the fact that it is supposed to be done as a showed straight line from 0 to 100 where the patients should point out where their adherence level is in a face-to-face interview, it was easily done verbally through the telephone interview asking to the patient the simple question: From 0 to 100, how often do you take your IBD treatment?
On this line, most IBD patients have been probably aware that they are chronically ill, so they could be afraid that their disease or the treatments may predispose them to a worse course of SARS-CoV2 infection. That could explain the reason why patients who suffered from COVID-19 disease had lower adherence rates to medication. Furthermore, in case of being infected, immunomodulatory treatment is usually withdrawn in clinical practice.
In the same way, non-married patients had also lower adherence rates than married ones. Some authors reported that patient associations and their family contributed to reduce their fear more than their physicians,22 which could explain why non-married patients could be less adherent than others. Consequently, a good physician–patient relationship becomes more important even than in normal conditions, especially in those cases with lower family support.23
The adherence to non-biological treatment (more often oral medication) were significatively lower than adherence to biologic therapy as had been published before the pandemic outbreak.24, 25 This fact may be related to a more aggressive course of the disease, which makes the patient more aware of the importance of an adequate adherence.
Psychological distress and doctor-patient discordance were associated with higher non-adherence rates. However, in spite of the pandemic, perceived stress was not associated with a lower adherence in our cohort, probably because of the great patient–physician relationship. Therefore, it is not only important to make posology adjustments to improve therapeutic adherence, but also psychological support to the patient at the time of the visit. It is possible that non-face-to-face consultations may make this work difficult, but it is important to emphasize this aspect especially in patients with identified risk factors related to non-adherence.24
The male gender26, 27 and younth28, 29 have also been noticed as poor adherence predictors in some cohorts, although these conclusions have not been reflected in our results, probably due to the reduction of free outside time period imposed during the lockdown period that could have affected especially to younger patients. As for education, it is proven to be inversely related to adherence as has been noticed previously.30 However, due to the exceptional moment whiting this study has been done compared with those in previously published articles before the pandemic, a direct comparison of the results was not possible.29
The novelty of the study suppose an important strength. For our understanding this is the first work that studies the emotional status and its consequences in IBD patients through PSS-10 questionnaire, and the first time that it is done in these patients during the pandemic lockdown. Thus, further studies are needed to determine the impact of the pandemic in IBD patients but above all focusing in emotional aspects, which may contribute to their quality of live and therefore in their course of the disease and adherence to medications.
PSS-10 could offer some advantages from the others in this specific situation because it is only focused in the perceived stress during a month, which could be more specific. Moreover, it was used in patients after the epidemic of SARS in 2003, that gives it a stronger value.12
Moreover, despite the fact that it was a telephone interview, it is important to take into account that it allowed us to answer all the questions that were necessary for the patient to complete this form correctly, which is not possible in an online questionnaire.
A potential limitation of our study due to telephone contact with patients is the rate of patients not located. In this line it was not possible to extent the questionnaire to all the IBD unit patients. Furthermore, despite the fact that the interviewer was never their regular doctor, telephone interview instead of an online questionnaire could be a negative fact, so that patients may have not felt free to answer what they really felt. The fact that there was not a study in IBD population which studied the emotional status and adherence through the same tools before the pandemic to compare, the results cannot be attributed exclusively to the lockdown period. Another limitation is the specific period of time during which the survey is applied, without subsequent monitoring. However, this study constitutes a beginning for further follow-up.29
Conclusion
To conclude, although the lockdown period due to COVID-19 pandemic has probably had an important emotional impact on Spanish population, IBD patients had a lower perceived stress, and also most of them had an optimal therapeutic adherence.
Conflicts of interest
None declared.
References
- 1.Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khosrawipour V., Lau H., Khosrawipour T., Kocbach P., Ichii H., Bania J., et al. Failure in initial stage containment of global COVID-19 epicenters. J Med Virol. 2020;92:863–867. doi: 10.1002/jmv.25883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith W., DO F. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27 doi: 10.1093/jtm/taaa020. taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson C.A., Clatworthy J., Robinson A., Horne R. Factors associated with non-adherence to oral medication for inflammatory bowel disease: a systematic review. Am J Gastroenterol [Internet] 2010;105:525–539. doi: 10.1038/ajg.2009.685. [DOI] [PubMed] [Google Scholar]
- 5.Zabana Y., Panés J., Nos P., Gomollón F., Esteve M., García-Sánchez V., et al. The ENEIDA registry (Nationwide study on genetic and environmental determinants of inflammatory bowel disease) by GETECCU: design, monitoring and functions. Gastroenterol Hepatol [Internet] 2020 doi: 10.1016/j.gastrohep.2020.05.007. [DOI] [PubMed] [Google Scholar]
- 6.Nau D.P., Steinke D.T., Williams L.K., Austin R., Lafata J.E., Divine G., et al. Adherence analysis using visual analog scale versus claims-based estimation. Ann Pharmacother. 2007;41:1792–1797. doi: 10.1345/aph.1K264. [DOI] [PubMed] [Google Scholar]
- 7.Lee A.M., Wong J.G.W.S., McAlonan G.M., Cheung V., Cheung C., Sham P.C., et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52:233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- 8.Trujillo H.M., González-Cabrera J.M. Psychometric properties of the Spanish version of the Perceived Stress Scale (PSS) Psicol Conductual. 2007;15:457–477. [Google Scholar]
- 9.Severs M., Zuithoff P.N.P.A., Mangen M.J.J., Van Der Valk M.E., Siersema P.D., Fidder H.H., et al. Assessing self-reported medication adherence in inflammatory bowel disease: a comparison of tools. Inflamm Bowel Dis. 2016;22:2158–2164. doi: 10.1097/MIB.0000000000000853. [DOI] [PubMed] [Google Scholar]
- 10.Wong J.J., Sceats L., Dehghan M., Wren A.A., Sellers Z.M., Limketkai B.N., et al. Depression and health care use in patients with inflammatory bowel disease. J Crohn's Colitis. 2019;13:19–26. doi: 10.1093/ecco-jcc/jjy145. [DOI] [PubMed] [Google Scholar]
- 11.Pedrozo-Pupo J.C., Campo-Arias A. Depression, perceived stress related to COVID, post-traumatic stress, and insomnia among asthma and COPD patients during the COVID-19 pandemic. Chron Respir Dis. 2020;17:8–10. doi: 10.1177/1479973120962800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chua S.E., Cheung V., McAlonan G.M., Cheung C., Wong J.W.S., Cheung E.P.T., et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry. 2004;49:385–390. doi: 10.1177/070674370404900607. [DOI] [PubMed] [Google Scholar]
- 13.Ruiz-Fernández M.D., Ramos-Pichardo J.D., Ibáñez-Masero O., Cabrera-Troya J., Carmona-Rega M.I., Ortega-Galán Á.M. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs [Internet] 2020;29:4321–4330. doi: 10.1111/jocn.15469. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0889159120306188. [DOI] [PubMed] [Google Scholar]
- 14.Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., et al. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav Immun [Internet] 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0889159120306188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pedrozo-Pupo J.C., Pedrozo-Cortés M.J., Campo-Arias A. Perceived stress associated with COVID-19 epidemic in Colombia: an online survey. Cad Saude Publica. 2020;36 doi: 10.1590/0102-311x00090520. [DOI] [PubMed] [Google Scholar]
- 16.Farrokhyar F., Marshall J.K., Easterbrook B., Irvine J.E. Functional gastrointestinal disorders and mood disorders in patients with inactive inflammatory bowel disease: Prevalence and impact on health. Inflamm Bowel Dis [Internet] 2006;12:38–46. doi: 10.1097/01.mib.0000195391.49762.89. Available from: https://academic.oup.com/ibdjournal/article/12/1/38-46/4676626. [DOI] [PubMed] [Google Scholar]
- 17.Schoultz M., Beattie M., Gorely T., Leung J. Assessment of causal link between psychological factors and symptom exacerbation in inflammatory bowel disease: a systematic review utilising Bradford Hill criteria and meta-analysis of prospective cohort studies. Syst Rev. 2020;9 doi: 10.1186/s13643-020-01426-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abegunde A.T., Muhammad B.H., Ali T. Preventive health measures in inflammatory bowel disease. World J Gastroenterol. 2016;22:7625–7644. doi: 10.3748/wjg.v22.i34.7625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Neuendorf R., Harding A., Stello N., Hanes D., Wahbeh H. Depression and anxiety in patients with Inflammatory Bowel Disease: a systematic review. J Psychosom Res [Internet] 2016;87:70–80. doi: 10.1016/j.jpsychores.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell A.J., Chan M., Bhatti H., Halton M., Grassi L., Johansen C., et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 21.Marrie R.A., Reingold S., Cohen J., Stuve O., Trojano M., Sorensen P.S., et al. The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Mult Scler J. 2015;21:305–317. doi: 10.1177/1352458514564487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.D’Amico F., Rahier J.-F., Leone S., Peyrin-Biroulet L., Danese S. Views of patients with inflammatory bowel disease on the COVID-19 pandemic: a global survey. Lancet Gastroenterol Hepatol [Internet] 2020;5:631–632. doi: 10.1016/S2468-1253(20)30151-5. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2468125320301515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lenti M.V., Selinger C.P. Medication non-adherence in adult patients affected by inflammatory bowel disease: a critical review and update of the determining factors, consequences and possible interventions. Expert Rev Gastroenterol Hepatol [Internet] 2017;11:215–226. doi: 10.1080/17474124.2017.1284587. [DOI] [PubMed] [Google Scholar]
- 24.Ribaldone D.G., Vernero M., Saracco G.M., Pellicano R., Finocchiaro F., Caviglia G.P., et al. The adherence to the therapy in inflammatory bowel disease: beyond the number of the tablets. Scand J Gastroenterol [Internet] 2018;53:141–146. doi: 10.1080/00365521.2017.1405070. [DOI] [PubMed] [Google Scholar]
- 25.Bager P., Julsgaard M., Vestergaard T., Christensen L.A., Dahlerup J.F. Adherence and quality of care in IBD. Scand J Gastroenterol. 2016;51:1326–1331. doi: 10.1080/00365521.2016.1195870. [DOI] [PubMed] [Google Scholar]
- 26.Kane S.V., Cohen R.D., Aikens J.E., Hanauer S.B. Prevalence of nonadherence with maintenance mesalamine in quiescent ulcerative colitis. Am J Gastroenterol. 2001;96:2929–2933. doi: 10.1111/j.1572-0241.2001.04683.x. [DOI] [PubMed] [Google Scholar]
- 27.Mantzaris G.J., Roussos A., Kalantzis C., Koilakou S., Raptis N., Kalantzis N. How adherent to treatment with azathioprine are patients with Crohn's disease in long-term remission? Inflamm Bowel Dis. 2007;13:446–450. doi: 10.1002/ibd.20041. [DOI] [PubMed] [Google Scholar]
- 28.Mackner L.M., Crandall W. V. Oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2005;11:1006–1012. doi: 10.1097/01.mib.0000186409.15392.54. [DOI] [PubMed] [Google Scholar]
- 29.Bruna-Barranco I., Lué A., Gargallo-Puyuelo C.J., Arroyo M.T., Alfambra E., Montero J., et al. Young age and tobacco use are predictors of lower medication adherence in inflammatory bowel disease. Eur J Gastroenterol Hepatol. 2019;31:948–953. doi: 10.1097/MEG.0000000000001436. [DOI] [PubMed] [Google Scholar]
- 30.Červený P., Bortlík M., Kuběna A., Vlček J., Lakatos P.L., Lukáš M. Nonadherence in inflammatory bowel disease: results of factor analysis. Inflamm Bowel Dis. 2007;13:1244–1249. doi: 10.1002/ibd.20189. [DOI] [PubMed] [Google Scholar]