Abstract
Purpose
To assess the diagnostic value of strain ratio elastography (SRE), a semiquantitative elastosonographic method based on the displacement of the tissue from an external source (manual compression with the transducer), as compared and in combination with conventional ultrasound for the differentiation of breast lesions.
Methods
One hundred and eighty-two patients with breast lesions consecutively underwent B-mode, color Doppler US, and strain US-elastography. Each lesion was classified according to the BI-RADS lexicon by evaluating the size, the B-mode, and color Doppler features and then evaluated by SRE. Histology proven by biopsy was used as the gold standard and the patients with malignant lesions subsequently underwent operations. The diagnostic performance of each method was assessed with 2 × 2 contingency tables and ROC curve analysis. To maximize the SRE sensitivity and specificity, the SRE cut-off value was calculated using the Youden test.
Results
Histological examination revealed 66 benign and 116 malignant breast lesions. The conventional ultrasound showed sensitivity and specificity for the differentiation of benign and malignant lesions of 86.2% and 75.8%, respectively. Similar results were found for strain US-elastography with a cut-off of 2.49, with sensitivity and specificity of 89.7% and 72.7%, respectively. The association of conventional ultrasound with the SRE value increased the sensitivity (98.3%) but decreased the specificity compared with conventional US alone (63.6%).
Conclusion
Strain US-elastography can be associated with BI-RADS US examination. According to our preliminary results, it helped increase the sensitivity although it decreased the specificity. However, further multicenter studies on a larger population are warranted.
Keywords: Breast lesions, Ultrasound, Strain US-elastography, Strain ratio, BI-RADS
Introduction
Ultrasound (US) plays a crucial role as a first-line imaging diagnostic tool, as a complementary method to mammography in women aged > 40 years, for breast lesion characterization, although it suffers from operator experience dependence [1]. Furthermore, US proved to be effective not only for diagnostic purposes but also for guidance during invasive procedures [2].
With the introduction of the Breast Imaging Reporting and Data System (BI-RADS) for US [3], the terminology and criteria for describing and classifying breast lesions were standardized with good diagnostic performance.
However, despite the extensive application of this lexicon, controversies regarding some topics remain, especially the question of how to apply the subcategorization of the suggested BI-RADS. Other US techniques, such as US-elastography, were developed to improve US performance. Indeed, the European Federation of Societies for Ultrasound in Medicine and Biology (EFSUMB) and the World Federation for Ultrasound in Medicine and Biology (WFUMB) dealt with US-elastography, publishing their guidelines about physical principles, clinical indications and limitations of elastography in several fields, including breast [4–6].
US-elastography is a noninvasive ultrasonographic imaging technique that provides information on tissue elasticity and stiffness [7].
Strain US-elastography (SRE) is a semiquantitative elastosonographic method based on the displacement of the tissue from an external (manual compression with the transducer) or patient source (physiologic movements of heart and respiration, with the transducer maintained motionless with slight skin contact) and has been used for the evaluation of superficial tissues, such as the breast, prostate, testis, neck, and thyroid; however, variable results have been reported [8, 9]. Elasticity imaging by strain US-elastography provides complementary information to conventional US by adding stiffness as another measurable parameter [10].
The aim of the present study was to assess the diagnostic performance of strain US-elastography (SRE) in the differentiation of breast lesions as an adjunct tool to the BI-RADS 2013 lexicon.
Methods
A population of 182 patients with breast lesions, aged 29–85 years (median = 54.3 years), assessed with conventional US and strain US-elastography (SRE) at the Sapienza University of Rome was studied.
The study protocol was approved by the hospital’s Ethical Review Board and was conducted in accordance with the principles of the Declaration of Helsinki and its amendments. Patients were fully informed of the characteristics of the study before providing consent, and written informed consents were obtained from all subjects.
The inclusion criteria were women with one or more breast nodules at voluntary periodic screening and/or who present a palpable breast mass.
The exclusion criteria were as follows: pregnancy, lactation, neoadjuvant chemotherapy in progress or having been completed less than 2 months previously, radiotherapy in progress or having been completed less than 3 months previously, and insufficient documentation.
US evaluation of each breast lesion included conventional US and strain US-elastography (SRE), all performed using Toshiba Aplio i800 (Canon Medical System Europe BV), equipped with a multifrequency linear probe (5–10 MHz). Ultrasonographic features were evaluated according to a predefined protocol: for each lesion B-mode maximum size (in mm), the B-mode and color Doppler features, and SRE parameter (strain ratio). All lesions were assigned a BI-RADS category according to BI-RADS lexicon 2013 classification [11, 12].
Nodules ranged in size from 6 to 27 mm, with a mean size of 14.1 mm.
For each lesion, we considered the following criteria: echogenicity, margins, vascularization, posterior features, orientation, and compressibility.
For strain US-elastography with strain ratio (SRE) evaluation, the operator exercised manual compression on the tissue with the ultrasound transducer [13].
The repeated manual compression of a tissue using a hand-held US transducer, paying attention to not apply precompression [14], produces a strain (displacement) within the same tissue, providing a color-coded strain distribution map (elastogram). The probe was held perpendicularly to the skin surface, using the real-time quality indicator for optimal compression-release control. The examination was considered optimal when the screen quality indicator (multiple boxes that change color from white to red, yellow, or green) on the upper right turned green. On the elastogram (placed on the left side of the screen, side by side with the B-mode image), the breast lesion was color coded depending on its stiffness with a colorimetric scale on the screen indicating the corresponding hard and soft areas. The examination was performed on the axial and longitudinal diameter with manual placement of a ROI (region of interest) on the lesion, giving a qualitative information of its stiffness. The largest diameter of the suspicious lesion was included in the image. Subsequently, semiquantitative information such as the strain ratio, an index of the relative elasticity between a chosen ROI located in the lesion and another of approximately the same size, localized on the sonographically normal adipose tissue, adjacent to the lesion at the same depth, was assessed. There was no case excluded due to the absence of surrounding fat.
The ultrasound equipment software then calculated the strain ratio value of the tissue with the semiquantitative information.
Nodules categorized as BI-RADS 2 were monitored in a 24-month follow-up, while lesions categorized as BI-RADS 3, 4, and 5 underwent ultrasound-guided core needle biopsy using a freehand technique. Each biopsy sample was analyzed by one pathologist specialized in breast cancer diagnosis. The pathologist was blinded to the results of the US information. Subsequently, the patients with malignant lesions were operated on.
Statistical analysis
The data were analyzed using the IBM SPSS Statistics package, version 23.0 (IBM Corp., Armonk, New York, United States). We used 2 × 2 contingency tables and calculated the area under the ROC curve (AUC) to determine the diagnostic accuracy of conventional US and strain US-elastography. Positive predictive values (PPV) and negative predictive values (NPV) were calculated as well. AUROC was computed and compared using the easyROC package [15]. Cut-off values were calculated using receiver operation characteristic (ROC) and the Youden test to get the optimal value.
SE sensitivity and specificity and its result were used as the basis for data dichotomization. The Bonferroni test was carried out to compare the AUC of the different diagnostic tests and their combination. For all the statistical tests, a value of p that was less than 0.05 was considered significant.
Results
182 patients satisfied the inclusion criteria. Histology results showed 66 patients with benign (Fig. 1a, b) and 116 patients with malignant nodules (Fig. 2a, b).
Fig. 1.
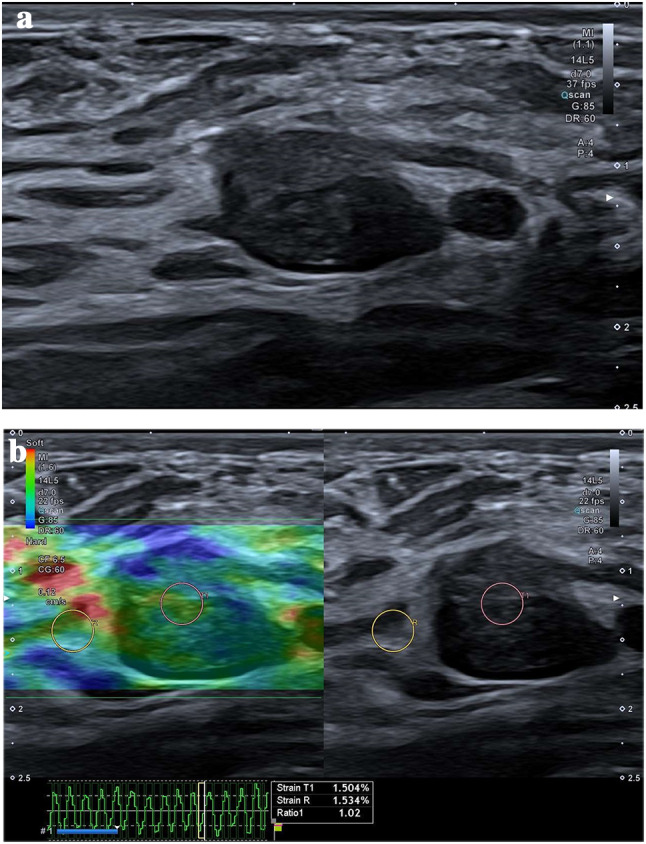
a Conventional US: oval, hypoechoic lesion with lobulated margins, classified as BI-RADS 3. Fibroadenoma was found on histological examination. b Semiquantitative US-elastography showed a strain ratio value of 1.02, suggestive of benign lesion. Fibroadenoma was found on histological examination
Fig. 2.
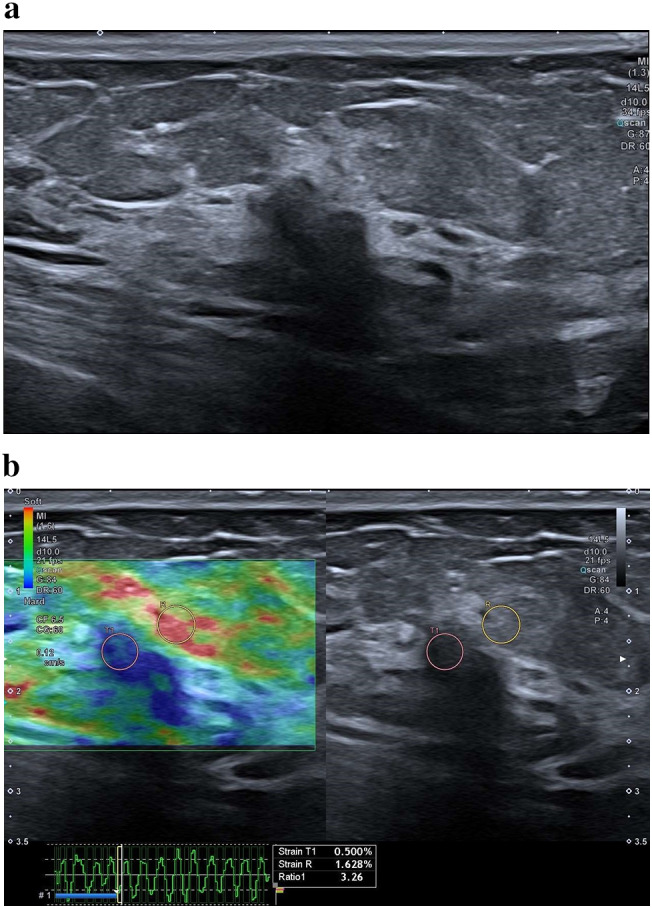
a Conventional US: markedly hypoechoic lesion with posterior attenuation and irregular margins, classified as BI-RADS 5. Invasive ductal carcinoma was found on histological examination. b Semiquantitative US-elastography showed a strain ratio value of 3.26, suggestive of malignant lesion. Invasive ductal carcinoma was found on histological examination
Seventy lesions were BI-RADS 5, of which 35 were invasive ductal carcinomas, 22 were invasive ductal carcinomas with ductal carcinomas foci in situ, 7 were ductal carcinoma in situ, 3 were invasive lobular carcinomas, and 3 were fibroadenoma.
46 lesions were BI-RADS category 4, of which 33 were invasive ductal carcinomas, 9 were lobular carcinomas, and 4 were fibroadenoma.
38 lesions were BI-RADS category 3, of which 14 were found to be invasive ductal carcinoma histologically proven, which also had associated ductal carcinomas in situ foci, while the other 24 nodules were fibroadenomas.
28 nodules were classified as BI-RADS category 2, of which 2 were found to be invasive ductal carcinoma with foci of ductal carcinomas in situ at biopsy, performed for their notable growth.
The comparison between US BI-RADS and histology are reported in Tables 1 and 2.
Table 1.
Comparison between US-BI-RADS and histology
| BENIGN | MALIGNANT | |
|---|---|---|
| BI-RADS 2 | 26/28 (93%) | 2/28 (7%) |
| BI-RADS 3 | 24/38 (63%) | 14/38 (37%) |
| BI-RADS 4 | 13/46 (28%) | 33/46 (72%) |
| BI-RADS 5 | 3/70 (4%) | 67/70 (96%) |
Table 2.
Comparison between BI-RADS and histology
| TP | FP | TN | FN | |
|---|---|---|---|---|
| US | 100 | 16 | 50 | 16 |
| SRE | 104 | 18 | 48 | 12 |
| US + SRE | 114 | 24 | 42 | 2 |
FN false negative, FP false positive, TN true negative, TP true positive
US showed sensitivity and specificity for the differentiation of benign and malignant lesions of 86.2% and 75.8%, respectively.
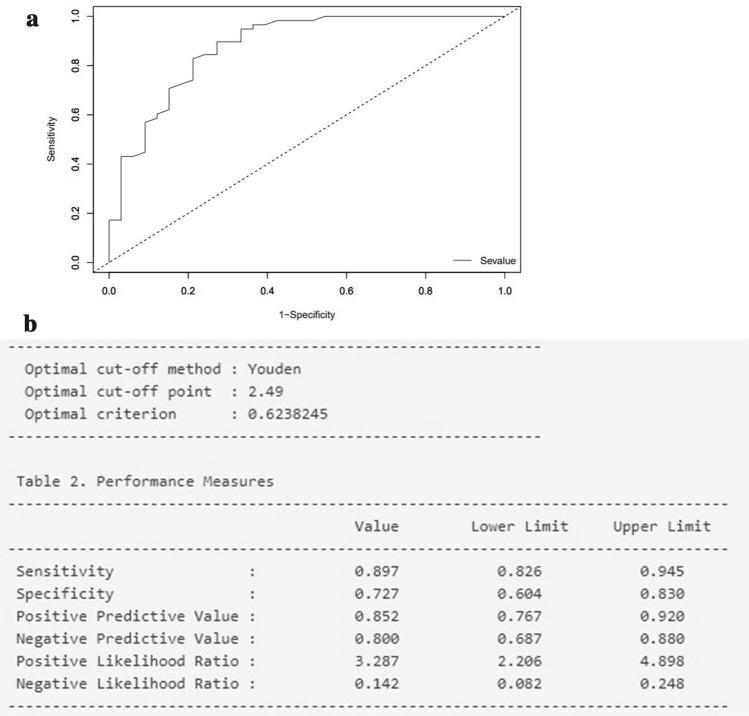
Using the Youden test, the optimal SRE cut-off turned out to be 2.49 (Fig. 3a, b) and the strain US-elastography accuracy achieved similar results as the US evaluation (sensitivity and specificity of 89.7% and 72.7%).
Fig. 3.
a ROC curve for different SRE values. b SRE cut-off using Youden test
Table 3 shows the diagnostic performance of conventional US, SRE and their combination (conventional US + SRE).
Table 3.
Accuracy of the methods and their combinations
| Parameter | Se | Sp | AUC | PPV | NPV |
|---|---|---|---|---|---|
| Conventional US | 86.2% | 75.8% | 0.810 | 86.2% | 75.8% |
| SRE | 89.7% | 72.7% | 0.812 | 85.2% | 80% |
| Conventional US + SRE | 98.3% | 63.6% | 0.810 | 82.6% | 95.5% |
Se sensitivity, Sp specificity, AUC area under curve, PPV positive predictive value, NPV negative predictive value, SRE strain US-Elastography
Table 4 shows the comparison of performances among modalities.
Table 4.
Comparison of performances among modalities
| Variable 1 | Variable 2 | ROC AUC (1) (SE) | ROC AUC (2) (SE) | Ʌ(ROC AUC) (SE) | p value* |
|---|---|---|---|---|---|
| US | SRE | 0.810 (0.044) | 0.812 (0.044) | 0.002 (0.063) | 0.973 |
| US | US + SRE | 0.810 (0.044) | 0.810 (0.043) | 0.000 (0.062) | 0.997 |
| SRE | US + SRE | 0.812 (0.044) | 0.810 (0.043) | 0.002 (0.062) | 0.970 |
US ultrasound, SRE strain ratio elastography, US + SRE ultrasound + strain ratio elastography
*p value refers to the Bonferroni test for comparison of AUCs (AUC area under curve)
The comparison between the AUCs of the two methods did not show statistically significant differences (p > 0.05) (Fig. 4). The association of the conventional evaluation with the SRE value increased the sensitivity (98.3%) but decreased the specificity compared with conventional US alone (63.6%). Benign masses showed a median strain ratio (SRE) of 2.16 (range 1.23–4.43), whereas the malignant masses had a median SRE of 3.51 (range 2–7.58). The ROC analysis demonstrated that a strain ratio value of 2.49 was the ideal cut-off point for the diagnosis of malignancies.
Fig. 4.
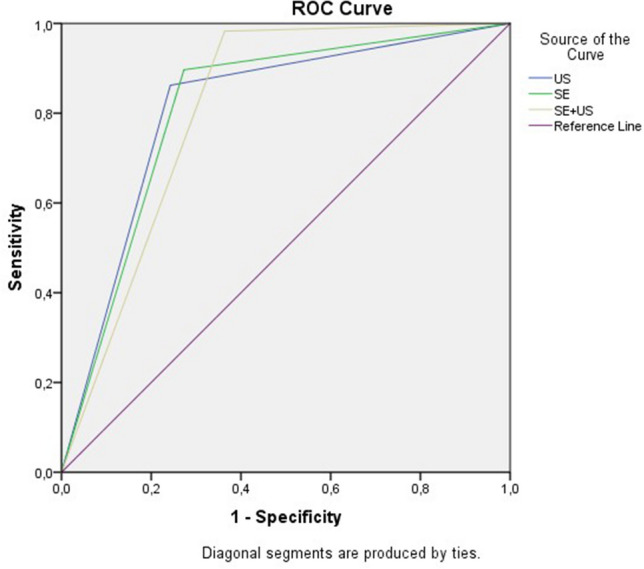
AUC of the different diagnostic tests and their combination
Discussion
The development and publication of BI-RADS began after the recognition of the need for a globally shared lexicon that would allow the sharing and clear expression of morphology, the operator’s judgment, and the strategy considered to be the best advice in the assessment of breast lesions [11].
A recent computer-guided decision-making software assisting in US morphologic analysis, S-Detect, was also introduced to improve inter-reader agreement in the assessment of breast lesions according to the BI-RADS US lexicon [16].
According to Xiao et al. [17], the use of the 2013 criteria resulted in 100% sensitivity, 17.4% specificity, 46.8% PPV, 100% NPV, and 0.867 ROC.
However, the differentiation of breast lesions is still considered challenging. Therefore, the technical developments of US-elastography opened new further prospects for the characterization of breast lesions, as already shown for characterization of lesions of the head and neck region [18, 19] with promising results, particularly for thyroid lesions despite diagnostic technological developments such as US-elastography [20–22].
Indeed, some studies suggested that strain US-elastography (SRE) can be added to the BI-RADS classification, improving the diagnostic performance of the ultrasound in the assessment of focal breast lesions [23–25].
Another study suggested that US-elastography can also be used in prognostic and treatment efficacy evaluation [26].
All these studies used the traditional form of elastography, the freehand compression SRE, which is an operator-dependent technique, with the drawback that the amount of the applied external pressure affects the tissue elasticity detected. The strain ratio, the semiquantitative approach described by Ueno et al. in 2007 [27], represents a further diagnostic aid for the evaluation of breast focal lesions. It is based on the positioning of 2 ROIs—one ROI in the lesion and a same-size reference ROI in the adjacent breast adipose tissue at the same depth as the lesion. Other studies evaluated the high sensitivity and specificity of shear wave elastography (SWE), a further elastosonographic method, in the differentiation of benign and malignant breast lesions [28]. According to EFSUMB [5] and WFUMB guidelines [6], US-elastography can be used to increase the suspicion category of lesions with no suggestive morphological features (i.e., a change from BI-RADS 3 to BI-RADS 4) and to distinguish solid lesions from cysts, whereas its use is not advised in the reduction of the category from 4 to 3. Previous efforts have described elastography’s role in improving sensitivity.
In a meta-analysis of 2,087 lesions, Sadigh et al. [29] reported for strain ratio a total sensitivity of 88% and a specificity of 83%.
Farrokh et al. [30] reported an SR sensitivity equal to 94.4% and a specificity of 87.3% with a benign/malignant cut-off of 2.9.
Alhabshi et al. [31] reported that the strain ratio was the most useful method for the characterization of malignant lesions with a cut-off value of 5.6.
In our study, conventional ultrasound showed sensitivity and specificity for the differentiation of benign and malignant lesions of 86.2% and 75.8%, respectively.
Strain US-elastography with a 2.49 cut-off showed similar results to the US evaluation with sensitivity and specificity of 89.7% and 72.7%, respectively. The comparison between the AUCs of the two methods did not show statistically significant differences (p > 0.05). The association of conventional evaluation with the SRE value increased the sensitivity (98.3%) but decreased the specificity compared with the standard US alone (63.6%).
In conclusion, the US-elastography with strain ratio showed a high sensitivity and specificity in the differentiation of benign and malignant lesions of the breast; however, it has some limitations related to operator experience and the depth of the lesions, in addition to their size. The main limitation of our study is that our institution represents a referral center with a high prevalence of cancer in our cohort. This study confirms the results of the current literature about the use of semiquantitative elastosonography in the breast pathology. Strain US-elastography reduced false negatives in cases of malignancies showing no suspicious features in conventional US, increasing the diagnostic accuracy of ultrasound. It also allowed, with a cut-off value of 2.49, to focus on those lesions that, even if not suspected after ultrasound, present a value greater than the cut-off and should undergo biopsy.
Abbreviations
- AUC
Area under curve
- AUROC
Area under the receiver operating characteristic curve
- BI-RADS
Breast imaging, reporting and data system
- EFSUMB
European Federation of Ultrasound in Medicine and Biology
- NPV
Negative predictive value
- PPV
Positive predictive value
- ROC
Receiver operation characteristic
- ROI
Region of interest
- SRE
Strain ratio elastography
- US
Ultrasound
- WFUMB
World Federation of Ultrasound in Medicine and Biology
Funding
This work received no specific funding.
Compliance with ethical standards
Conflict of interest
Federica Pediconi lectured for Bracco, Bayer and Siemens; Vito Cantisani lectured for Bracco, Samsung and Canon. The other authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hooley RJ, Scoutt LM, Philpotts LE. Breast ultrasonography: state of the art. Radiology. 2013;268:642–659. doi: 10.1148/radiol.13121606. [DOI] [PubMed] [Google Scholar]
- 2.Carlino G, Rinaldi P, Giuliani M, Rella R, Bufi E, Padovano F, Ciardi C, Romani M, Belli P, Manfredi R. J Ultrasound. 2019;22(1):85–94. doi: 10.1007/s40477-018-0335-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park CS, Lee JH, Yim HW et al (2007) Observer agreement using the ACR Breast Imaging Reporting and Data System (BI-RADS)-ultrasound, First Edition (2003). Korean J Radiol 8(5):397–402 [DOI] [PMC free article] [PubMed]
- 4.Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Klauser AS, Sporea I, Calliada F, Cantisani V, D'Onofrio M, Drakonaki EE, Fink M, Friedrich-Rust M, Fromageau J, Havre RF, Jenssen C, Ohlinger R, Săftoiu A, Schaefer F, Dietrich CF (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: Clinical applications. Ultraschall Med 34(3):238–253 [DOI] [PubMed]
- 5.Săftoiu A, Gilja OH, Sidhu PS, Dietrich CF, Cantisani V, Amy D, Bachmann-Nielsen M, Bob F, Bojunga J, Brock M, Calliada F, Clevert DA, Correas JM, D'Onofrio M, Ewertsen C, Farrokh A, Fodor D, Fusaroli P, Havre RF, Hocke M, Ignee A, Jenssen C, Klauser AS, Kollmann C, Radzina M, Ramnarine KV, Sconfienza LM, Solomon C, Sporea I, Ștefănescu H, Tanter M, Vilmann P. The EFSUMB guidelines and recommendations for the clinical practice of elastography in non-hepatic applications: update 2018. Ultraschall Med. 2019;40(4):425–453. doi: 10.1055/a-0838-9937. [DOI] [PubMed] [Google Scholar]
- 6.Barr RG, Nakashima K, Amy D, et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: breast. Ultrasound Med Biol. 2015;41(5):1148–1160. doi: 10.1016/j.ultrasmedbio.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 7.Prado-Costa R, Rebelo J, Monteiro-Barroso J, Preto AS. Ultrasound elastography: compression elastography and shear-wave elastography in the assessment of tendon injury. Insights Imaging. 2018;9:791–814. doi: 10.1007/s13244-018-0642-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cantisani V, Bertolotto M, Weskott HP, Romanini L, Grazhdani H, Passamonti M, Drudi FM, Malpassini F, Isidori A, Meloni FM, Calliada F, D’Ambrosio F. Growing indications for CEUS: The kidney, testis, lymph nodes, thyroid, prostate, and small bowel. Eur J Radiol. 2015;84(9):1675–1684. doi: 10.1016/j.ejrad.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Pozza C, Gianfrilli D, Fattorini G, et al. Diagnostic value of qualitative and strain ratio elastography in the differential diagnosis of non-palpable testicular lesions. Andrology. 2016;4(6):1193–1203. doi: 10.1111/andr.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kamaya A, Machtaler S, Safari Sanjani S, Nikoozadeh A, Graham Sommer F, Pierre Khuri-Yakub BT, et al. New technologies in clinical ultrasound. Semin Roentgenol. 2013;48:214–223. doi: 10.1053/j.ro.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 11.D’Orsi CJ, Sickles EA, Mendelson EB, Morris EA, et al. ACR BI-RADS® Atlas, breast imaging reporting and data system. Reston: American College of Radiology; 2013. [Google Scholar]
- 12.Mendelson EB, Böhm-Vélez M, Berg WA et al (2013) ACR BI-RADS® Ultrasound. In: ACR BI-RADS® atlas, breast imaging reporting and data system. American College of Radiology, Reston
- 13.Ophir J, Cespedes I, Ponnekanti H, Yazdi Y, Li X. Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging. 1991;13:111–134. doi: 10.1177/016173469101300201. [DOI] [PubMed] [Google Scholar]
- 14.Barr RG, Zhang J et al (2012) Effects of precompression on elasticity imaging of the breast development of a clinically useful semiquantitative method of precompression assessment. Ultrasound Med 31:895–902 (PubMed) [DOI] [PubMed]
- 15.Goksuluk D, Korkmaz S, Zararsiz G, et al. easyROC: an interactive web-tool for ROC curve analysis using R language environment. R J. 2016;8:213–230. doi: 10.32614/RJ-2016-042. [DOI] [Google Scholar]
- 16.Bartolotta TV, Orlando AAM, Di Vittorio ML, et al. S-Detect characterization of focal solid breast lesions: a prospective analysis of inter-reader agreement for US BI-RADS descriptors. J Ultrasound. 2020 doi: 10.1007/s40477-020-00476-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao X, Jiang Q, Wu H, Guan X, Qin W, Luo B. Diagnosis of sub-centimetre breast lesions: combining BI-RADS-US with strain elastography and contrast-enhanced ultrasound—a preliminary study in China. Eur Radiol. 2017;27:2443–2450. doi: 10.1007/s00330-016-4628-4. [DOI] [PubMed] [Google Scholar]
- 18.Suh CH, Choi YJ, Baek JH, Lee JH. The diagnostic performance of shear wave elastography for malignant cervical lymph nodes: a systematic review and meta-analysis. Eur Radiol. 2017;27(1):222–230. doi: 10.1007/s00330-016-4378-3. [DOI] [PubMed] [Google Scholar]
- 19.Cantisani V, Grazhdani H, Ricci P, et al. Q-elastosonography of solid thyroid nodules: assessment of diagnostic efficacy and interobserver variability in a large patient cohort. Eur Radiol. 2014;24:143–150. doi: 10.1007/s00330-013-2991-y. [DOI] [PubMed] [Google Scholar]
- 20.Cantisani V, David E, Grazhdani H, Rubini A, Radzina M, Dietrich CF, Durante C, Lamartina L, Grani G, Valeria A, Bosco D, Di Gioia C, Frattaroli FM, D'Andrea V, De Vito C, Fresilli D, D'Ambrosio F, Giacomelli L, Catalano C (2019) Ultraschall Med 40(4):495–503. 10.1055/a-0853-1821[Epub 2019 May 28. Prospective Evaluation of Semiquantitative Strain Ratio and Quantitative 2D Ultrasound Shear Wave Elastography (SWE) in Association with TIRADS Classification for Thyroid Nodule Characterization] [DOI] [PubMed]
- 21.Cantisani V, Grazhdani H, Drakonaki E, D'Andrea V, Di Segni M, Kaleshi E, Calliada F, Catalano C, Redler A, Brunese L, Drudi FM, Fumarola A, Carbotta G, Frattaroli F, Di Leo N, Ciccariello M, Caratozzolo M, D'Ambrosio F (2015) Int J Endocrinol 2015:908575. 10.1155/2015/908575(Epub 2015 Apr 14. Strain US Elastography for the Characterization of Thyroid Nodules: Advantages and Limitation) [DOI] [PMC free article] [PubMed]
- 22.Fresilli D, Grani G, De Pascali ML, Alagna G, Tassone E, Ramundo V, Ascoli V, Bosco D, Biffoni M, Bononi M, D'Andrea V, Frattaroli F, Giacomelli L, Solskaya Y, Polti G, Pacini P, Guiban O, Gallo Curcio R, Caratozzolo M, Cantisani V. J Ultrasound. 2020;23(2):169–174. doi: 10.1007/s40477-020-00453-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tan M, Teh HS, Mancer JF, Poh WT. Improving B mode ultrasound evaluation of breast lesions with real-time ultrasound elastography–a clinical approach. Breast. 2008;17(3):252–257. doi: 10.1016/j.breast.2007.10.015. [DOI] [PubMed] [Google Scholar]
- 24.Chiorean A, Duma MM, Dudea SM, Iancu A, et al. Real-time ultrasound elastography of the breast: state of the art. Med Ultrasonography. 2008;10:73–82. [Google Scholar]
- 25.Cantisani V, David E, Barr RG et al (2020) US-elastography for breast lesion characterization: prospective comparison of US BIRADS, strain elastography and shear wave elastography [published online ahead of print, 2020 Apr 24]. US-Elastografie zur Charakterisierung von Brustläsionen: Prospektiver Vergleich von US-BI-RADS, Strain-Elastografie und Scherwellen-Elastografie [published online ahead of print, 2020 Apr 24]. Ultraschall Med. 10.1055/a-1134-4937 [DOI] [PubMed]
- 26.Nakashima K, Moriya T. Comprehensive ultrasound diagnosis for intraductal spread of primary breast cancer. Breast Cancer. 2013;20(1):3–12. doi: 10.1007/s12282-011-0326-x. [DOI] [PubMed] [Google Scholar]
- 27.Ueno E, Umemoto T, Bando H, Tohno E, Waki K, Matsumura T (2007) New quantitative method in breast elastography: fat lesion ratio (FLR). In: Radiological society of North America 2007 scientific assembly and annual meeting, 25–30 November, Chicago, IL. http://archive.rsna.org/2007/5015476.html
- 28.Chen L, He J, Liu G, et al. Diagnostic performances of shear-wave elastography for identification of malignant breast lesions: a meta-analysis. Jpn J Radiol. 2014;32:592–599. doi: 10.1007/s11604-014-0349-2. [DOI] [PubMed] [Google Scholar]
- 29.Sadigh G, Carlos RC, Neal CH, Dwamena BA. Accuracy of quantitative ultrasound elastography for differentiation of malignant and benign breast abnormalities: a meta-analysis. Breast Cancer Res Treat. 2012;134(3):923–931. doi: 10.1007/s10549-012-2020-x. [DOI] [PubMed] [Google Scholar]
- 30.Farrokh A, Wojcinski S, Degenhardt F (2011) Diagnostic value of strain ratio measurement in the differentiation of malignant and benign breast lesions. Ultraschall Med 32:400–405 (PubMed) [DOI] [PubMed]
- 31.Alhabshi SM, Rahmat K, Abdul Halim N, Aziz S, Radhika S, Gan GC, Vijayananthan A, Westerhout CJ, Mohd-Shah MN, Jaszle S, Harlina Mohd Latar N, Muhammad R. Semi-quantitative and qualitative assessment of breast ultrasound elastography in differentiating between malignant and benign lesions. Ultrasound Med Biol. 2013;39(4):568–578. doi: 10.1016/j.ultrasmedbio.2012.10.016. [DOI] [PubMed] [Google Scholar]